Abstract
Introduction:
In this study, we aimed to examine, in Thailand, the impact on smokers’ reported awareness of and their cognitive and behavioral reactions following the change from text-only to pictorial warnings printed on cigarette packs. We also sought to explore differences by type of cigarette smoked (roll-your-own [RYO] vs. factory-made [FM] cigarettes).
Methods:
Data came from the International Tobacco Control Southeast Asia Survey, conducted in Thailand and Malaysia, where a representative sample of 2,000 adult smokers from each country were recruited and followed up. We analyzed data from one wave before (Wave 1) and two waves after the implementation of the new pictorial warnings (two sets introduced at Waves 2 and 3, respectively) in Thailand, with Malaysia, having text-only warnings, serving as a control.
Results:
Following the warning label change in Thailand, smokers’ reported awareness and their cognitive and behavioral reactions increased markedly, with the cognitive and behavioral effects sustained at the next follow-up. By contrast, no significant change was observed in Malaysia over the same period. Compared to smokers who smoke any FM cigarettes, smokers of only RYO cigarettes reported a lower salience but greater cognitive reactions to the new pictorial warnings.
Conclusions:
The new Thai pictorial health warning labels have led to a greater impact than the text-only warning labels, and refreshing the pictorial images may have helped sustain effects. This finding provides strong support for introducing pictorial warning labels in low- and middle-income countries, where the benefits may be even greater, given the lower literacy rates and generally lower levels of readily available health information on the risks of smoking.
INTRODUCTION
Tobacco products are required to carry health warnings because tobacco is a highly addictive product that kills about half of its long-term users (Doll, Peto, Boreham, & Sutherland, 2004). The high reach at the population level and the high frequency of exposure at the individual level make health warnings a very cost-effective tool for communicating the health risks of smoking to consumers. The World Health Organization Framework Convention on Tobacco Control requires ratifying countries to mandate health warnings on cigarette products and recommends the use of pictorial warnings. The guidelines for Article 11 state that warnings should cover at least 50% of the top of the front and back of the pack and may include pictorial images. These guidelines were shaped by evidence from studies conducted over the past decade demonstrating that pictorial health warnings are more effective than text-only warnings (see recent review by Hammond, 2011).
Much of the evidence on the effectiveness of pictorial health warning labels on cigarette packages is based on findings from studies conducted in Western well-educated populations (Borland, Wilson, et al., 2009; Hammond, 2011). Past research has established that warning labels will have an impact if they can generate emotionally charged responses—either cognitive and/or behavioral (Borland, Yong, et al., 2009; Hammond, 2011). Mere awareness in frequency of noticing and/or reading warnings is not associated with subsequent quitting activity unless it first leads to such reactions (Borland, Yong, et al., 2009). Because pack warnings have the capacity to be seen many times per day, they only need to be attended to on a minority of occasions to have effects. Indeed, research studies have consistently found that reported frequency of avoiding warnings is positively associated with cognitive and behavioral responses that predict subsequent quitting activity (Borland, Yong, et al., 2009; Hammond, 2011).
The limited evidence that has been published suggests that the effects of health warnings are similar in developing countries. For instance, an experimental study found that showing smokers pictorial warnings covering 40% of the front and 60% of the back of pack (proposed for use in Malaysia) had greater positive impact than the text-only warnings that appeared only on the side of packs used at the time (Fathelrahman et al., 2010). Similarly, an experimental study in China found that adult smokers were more likely to rate pictorial warnings to be more effective than text-only warnings in motivating smoking cessation and in preventing smoking among youth (Fong et al., 2010). This is complemented by two cross-sectional population studies. The first study, which made use of some of the Malaysian data used here, found cognitive and behavioral reactions to text-only warnings were related to interest in quitting (Fathelrahman et al., 2009). The second study conducted in Brazil, Uruguay, and Mexico found that health warnings with pictorial images had greater cognitive impacts than text-only warnings, particularly among smokers with low education attainment (Thrasher et al., 2010). Stronger inferences are possible from longitudinal quasiexperimental studies, that is, those that employ cohort designs, comparing one country before and after a change in policy with another country during that same time period where there has been no change in that policy (IARC, 2008). To date, no such studies have been published on the effects of pictorial warnings in low- and middle-income countries (LMICs).
This article reports on the first quasiexperimental study of the impact of pictorial warnings in LMICs. We analyzed the longitudinal data collected between 2005 and 2008 from the International Tobacco Control Southeast Asia (ITC-SEA) Project conducted in Thailand and Malaysia to evaluate the introduction of pictorial warnings on cigarette packaging in Thailand. From March 25, 2005, just after the collection of the first wave of data, Thailand introduced larger pictorial warnings (50% on the front and back top panel of cigarette packs) to replace the smaller text-only warnings (33% on the front and back of the pack) introduced in 1997.
Thailand was the second country in the region, after Singapore, to adopt pictorial health warnings on tobacco packaging. In an attempt to evaluate the new warnings in Thailand, Silpasuwan et al. (2008) in March 2005 conducted a cohort study in five regions of Thailand, including Bangkok, where they collected baseline data from 1,637 Thai workers working in 22 workplaces, but this data were collected partway through rollout, a time that warnings can have had much of their initial impact (Borland & Hill, 1997). They followed the cohort up a year later, only 37% were successfully recontacted. They found a significant increase in positive attitudes toward quitting related to reported exposure to the new pictorial warnings. However, there was no significant gain in knowledge about the health risks of smoking. In addition, they found an unexpected decline in intention to quit smoking following reported exposure, but the reason for this was unclear. Given the above-mentioned methodological problems and a lack of capacity to control for possible confounding factors, no firm conclusions can be drawn from this study. The dataset we have allows us to overcome some of the main limitations of that study. Further, it provides us with the opportunity to explore the effects on smokers of hand-rolled or roll-your-own (RYO) cigarettes. It is unclear whether the new warnings would have different impacts on smokers who smoke RYO cigarettes versus factory-made (FM) cigarettes in Thailand. Previous research in Thailand using data collected in early 2005 found 58% of smokers used RYO sometimes, with 33% using it exclusively (Young et al., 2008). RYO tobacco is mostly a product of informal economy (i.e., not FM), bought from roadside vendors rather than commercially manufactured products (Young et al., 2008). That study found that exclusive RYO smokers were less aware of health warnings but there was no knowledge deficit, suggesting that health risk information was getting through to them as well (Young et al., 2008). Until July 2007 no warning was required, but since then one out of two designated pictorial health warning labels in black and white is also required on manufactured RYO products (Sangthong, Wichaidit, & Ketchoo, 2011; Termsirikulchai, Benjakul, Kengganpanich, Theskayan, & Nakju, 2008). Given that few Thai RYO smokers use manufactured RYO tobacco (Dalvey Group, 2004), exposure to these warnings is likely to be limited.
In Malaysia, the health warning labels were text-only printed on the side of cigarette packs, first introduced in 1979. The warning carried a single text-only message: “Warning by the Malaysian government; smoking is hazardous to health.” The warning labels remained unchanged over the study period, thus, allowing Malaysia to serve as a control. Malaysian smokers predominantly smoke FM cigarettes, estimated at 83% (Young et al., 2008).
This study aimed to (a) examine the impact on adult smokers’ reported awareness of warnings and their cognitive and behavioral reactions following the change from text-only to pictorial warnings that appear on cigarette packages in Thailand and (b) explore whether the impact of the new Thai warnings was moderated by the type of cigarette smoked (RYO vs. FM).
METHODS
Sample and Sampling Design
Data were drawn from the ITC-SEA Survey, a cohort survey of nationally representative samples of adult smokers in Thailand and Malaysia. Details on the conceptual framework and its methodology have been published elsewhere (Fong et al., 2006; Thompson et al., 2006). Respondents were adult smokers (≥18 years old) who reported having smoked at least 100 cigarettes in their lifetime and who had smoked at least once in the past 30 days. Respondents were surveyed using face-to-face interviews and were recruited from households using a stratified multistage sampling design. The primary strata consisted of Bangkok and four regions (North, Northeast, Central, and South) in Thailand, and six zones of Malaysia. In Thailand, respondents were selected from Bangkok and two provinces in each of Thailand’s four regions (Chiang Mai, Phrae, Nakhon Ratchasima, Nong Khai, Nakhon Pathom, Samut Sakhon, Nakhon Si Thammarat, and Songkhla). In Malaysia, respondents were drawn from one state in each of the country’s six geographic zones (Kedah, Selangor, Johore, Terengganu, Sabah, and Sarawak) at Wave 1, and a seventh state, Penang, was added in Wave 2. The samples and waves they participated in are reported in Table 1.
Table 1.
Characteristics of All Respondents Included in the Study
| Characteristic | Malaysia (n = 3,220) | Thailand (n = 3,067) | Testa | |||||
|---|---|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | χ2 | df | p value | ||
| Sex | Men | 3121 | 96.9 | 2815 | 91.8 | 28.49 | 1 | <.001 |
| Women | 99 | 3.1 | 252 | 8.2 | ||||
| Age | 18–24 | 609 | 18.9 | 234 | 7.6 | 246.88 | 3 | <.001 |
| 25–39 | 1109 | 34.4 | 799 | 26.1 | ||||
| 40–54 | 996 | 30.9 | 1198 | 39.1 | ||||
| 55+ | 506 | 15.7 | 836 | 27.2 | ||||
| Mean (SD) | 39.2 (14.6) | 45.9 (14.6) | 39.23 | 1, 49 | <.001 | |||
| Urban vs. rural | Rural | 1025 | 31.8 | 1937 | 63.2 | 4.62 | 1 | .032 |
| Urban | 2195 | 68.2 | 1130 | 36.8 | ||||
| Income | Low | 872 | 27.1 | 1006 | 32.8 | 37.73 | 3 | <.001 |
| Moderate | 910 | 28.3 | 996 | 32.5 | ||||
| High | 971 | 30.2 | 1008 | 32.9 | ||||
| Not reported | 467 | 14.5 | 57 | 1.8 | ||||
| Education | Secondary/more | 1928 | 59.9 | 499 | 16.3 | 117.28b | 1, 49 | <.001 |
| Less than secondary | 1292 | 40.1 | 2568 | 83.7 | ||||
| Ethnicity | Minor group | 837 | 26.0 | 46 | 1.5 | 126.28 | 1 | <.001 |
| Major group | 2383 | 74.0 | 3021 | 98.5 | ||||
| Smoking frequency | Nondaily smoker | 71 | 2.2 | 185 | 6.0 | 60.08 | 1 | <.001 |
| Daily smoker | 3149 | 97.8 | 2882 | 94.0 | ||||
| Cigarettes smoked per day | 0–10 | 1501 | 46.6 | 1714 | 55.9 | 29.28 | 3 | <.001 |
| 11–20 | 1512 | 47.0 | 1141 | 37.2 | ||||
| 21–30 | 122 | 3.8 | 141 | 4.6 | ||||
| 31+ | 85 | 2.6 | 71 | 2.3 | ||||
| Mean (SD) | 13.6 (8.2) | 12.7 (8.4) | 3.57 | 1, 49 | .065 | |||
| FM vs. RYO | FM | 2679 | 83.2 | 1458 | 47.5 | 85.27 | 2 | <.001 |
| Both | 286 | 8.9 | 618 | 20.2 | ||||
| RYO | 255 | 7.9 | 991 | 32.3 | ||||
| Cohort | Wave 1 (2005) | 1892 | 58.8 | 1989 | 64.8 | |||
| Wave 2 (2006/2007) | 640 | 19.9 | 499 | 16.3 | 1.48 | 2 | .476 | |
| Wave 3 (2008) | 688 | 21.4 | 579 | 18.9 | ||||
Note. FM = factory-made cigarettes; RYO = roll-your-own cigarettes.
aResults are unweighted but the survey design was accounted for in the analysis. All tests are the Rao–Scott χ2 test unless otherwise indicated.
bPearson χ2 statistic corrected for the survey design and converted into an F-statistic.
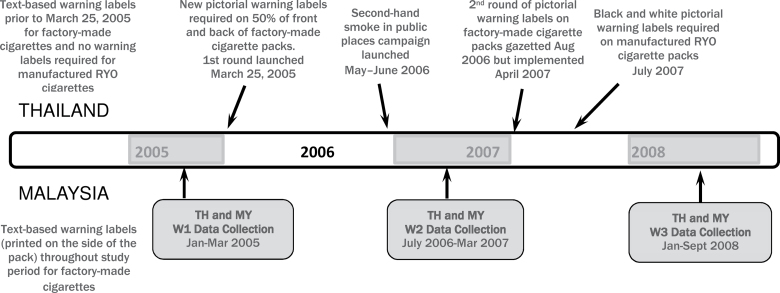
Wave 1 was conducted from January to March 2005 in both countries, Wave 2 from July to September 2006 in Thailand, about 14–18 months after the new warnings were introduced, and in Malaysia from August 2006 to March 2007. Wave 3 was conducted from January to March 2008 in Thailand, about 11 months after the second round of pictorial warnings came into effect, and from March to September 2008 in Malaysia (see Figure 1). The retention rate from Waves 1 to 2 was 78% in Thailand, but only 50% in Bangkok. The retention rate was 44% in Malaysia, where the recontact fieldwork proved to be much more difficult, due mainly to inaccessibility or other failure to recontact rather than refusal. Retention rates for Waves 2–3 were 83% and 59% for Thailand and Malaysia, respectively. In order to minimize the effect of attrition, those lost to follow-up were replenished using the same sampling procedure as used at baseline.
Figure 1.
Timeline of data collection in Thailand (TH) and Malaysia (MY) for each wave and key events related to health warning policy changes and passive smoking media campaign in Thailand.
Survey Interviewing
The survey fieldwork was conducted by trained interviewers in each of the two countries. In Thailand, the survey interviewing was conducted in Thai by staff of the Institute for Population and Social Research, Mahidol University. In Malaysia, the survey interviewing was conducted in Malay (or in English if preferred) by staff of Universiti Sains Malaysia with assistance from the Malaysian Statistics Department and Ministry of Health. The length of the survey interview was approximately 50–60min in both countries. All aspects of the training and survey interviewing protocol were standardized across both countries to the extent possible.
Measures
Demographic Measures
In addition to measures of gender and age, ethnicity was measured in accordance with the census categories in each country and was used as a binary variable in these analyses (majority group vs. minority group). Education was measured using standard categories in each country, and combined for analysis into a dichotomized variable: those without secondary education and those with at least secondary education.
Smoking-Relevant Variables
These consisted of cigarettes smoked per day, smoking frequency (daily vs. nondaily), and whether the smoker smoked exclusively FM cigarettes, smoked exclusively RYO cigarettes, or smoked a mix of RYO and FM cigarettes.
Antismoking Information or Advertising
Respondents were asked whether, in the last 6 months, they noticed (Yes/No) any antismoking information or advertising from TV, radio, billboard, newspaper, and so forth and Yes responses were summed to form a composite measure of awareness of antismoking information other than from warning labels.
Warning-Label Effectiveness Measures
Warning label salience (noticing and reading the labels closely) was assessed using two questions: “In the last month, how often, if at all, have you noticed the health warnings on cigarette packages?” and “In the last month, how often, if at all, have you read or looked closely at the health warnings on cigarette packages?” The response options for both were “Never,” “Once in a while,” “Often,” and “Very often.” Cognitive reactions to labels (thoughts about the harms of smoking and thoughts about quitting) were assessed using the following two questions: “To what extent, if at all, do the health warnings make you think about the health risks (health danger) of smoking?” and “To what extent, if at all, do the health warnings on cigarette packs make you more likely to quit smoking?” with response options “Not at all,” “A little,” “Somewhat,” and “A lot.” Behavioral reactions to labels (forgoing of cigarettes and avoidance) were assessed by asking: “In the last month, have the health warnings stopped you from having a cigarette when you were about to smoke one?” with response options “Never,” “Once,” “A few times,” and “Many times” and “In the last month, have you made any effort to avoid looking at or thinking about the health warnings?” (Yes/No).
Data Analysis
In order to test whether the introduction of pictorial warning labels in Thailand increased salience of the labels (noticing and reading) and psychological reactions to the labels (thinking about the risks, avoiding labels, increasing the likelihood of quitting, and forgoing a cigarette), the proportion of respondents responding in the affirmative for each measure was estimated for each of the three waves. Significant increases were expected in Thailand between Waves 1 and 2, due to the introduction of pictorial warning labels while no changes were expected in Malaysia. Logistic regression, estimated using generalized estimated equations (GEEs), was used to test whether outcome measures changed significantly over time and whether the changes differed by country. In other words, these models tested the country × time interaction effect, where a statistically significant interaction effect would indicate that the change in one country over time differed from the change in the other country. All models controlled both time-invariant covariates and time-varying covariates. Time-invariant covariates were sex, age group, urban/rural residence, income, education, ethnicity, and cohort/wave of recruitment, whereas time-varying covariates were daily/nondaily smoking status, cigarettes smoked per day, and exclusive use of RYO cigarettes. Additional analyses were conducted using only the Thai data to explore whether exclusive use of RYO cigarettes moderated the effects found.
The analysis was conducted using SUDAAN version 10.0.1 in order to account for both the multistage sampling design used in the ITC-SEA Project and for the longitudinal nature of the data. Analyses were conducted using weighted and unweighted data for all models, with no significant differences observed between weighted and unweighted analyses. Results are presented for weighted analyses, with standard errors and model coefficients adjusted accordingly.
RESULTS
Sample Characteristics
As seen in Table 1, there were more female, older, and rural respondents in the Thai sample than in the Malaysian sample. Thai respondents were less educated, more likely to be nondaily smokers, and not heavy smokers. Malaysian respondents were more reluctant to provide income information. The majority of Malaysian respondents smoked FM cigarettes, whereas about a third of the Thais were exclusive RYO users.
Impact of the New Warnings in Thailand
The descriptive results showing the change over time in reactions to the warning labels among Thai and Malaysian smokers are presented in Table 2. The results of the GEE analyses revealed that, as hypothesized, there was a significant country by time interaction effect for all label effectiveness measures (all ps < .001). The relevant statistics are presented in Table 3. Following the introduction of the new larger and pictorial Thai warnings (just after Wave 1), reported salience and the cognitive and behavioral reactions to the warnings all showed a significant increase from Waves 1 to 2 among the Thai smokers; but the same measures generally showed no change over the same period among the Malaysian smokers. The effects for all measures were generally sustained in Thailand by Wave 3 (about 18 months later) with further significant increases for quit-related thoughts and avoidance behavior. No significant changes occurred between Waves 2 and 3 for any of these measures in Malaysia.
Table 2.
Reactions to Warning Labels Over Time, by Country and by Type of Cigarette Smoked (Thailand Only)
| Country | Wave 1 | Wave 2 | Wave 3 | |
|---|---|---|---|---|
| % (SE) | % (SE) | % (SE) | ||
| Salience | ||||
| Notice | TH | 62.4 (2.40) | 70.1 (2.15) | 73.7 (1.87) |
| MY | 57.2 (4.15) | 50.9 (3.36) | 54.1 (3.44) | |
| Any FM | 74.6 (1.83) | 83.8 (1.37) | 88.4 (1.44) | |
| RYO only | 35.6 (4.48) | 54.7 (2.08) | 58.3 (1.77) | |
| Read | TH | 45.5 (2.01) | 53.6 (1.91) | 50.1 (1.73) |
| MY | 38.6 (3.89) | 38.0 (3.27) | 35.6 (2.58) | |
| Any FM | 55.4 (2.00) | 66.6 (2.02) | 63.1 (1.97) | |
| RYO only | 23.2 (4.02) | 39.1 (1.80) | 36.5 (2.21) | |
| Cognitive | ||||
| Think risk | TH | 30.9 (2.14) | 45.5 (1.83) | 48.3 (2.16) |
| MY | 7.6 (1.33) | 6.8 (0.93) | 5.0 (1.13) | |
| Any FM | 33.7 (1.98) | 45.5 (2.11) | 45.5 (2.53) | |
| RYO only | 24.6 (3.69) | 45.5 (2.55) | 51.2 (3.22) | |
| Think quit | TH | 27.9 (2.37) | 38.0 (1.56) | 42.0 (2.19) |
| MY | 10.6 (1.30) | 7.2 (1.12) | 5.6 (0.98) | |
| Any FM | 30.1 (2.53) | 34.7 (1.88) | 38.5 (2.61) | |
| RYO only | 23.0 (3.14) | 41.7 (2.05) | 45.7 (2.52) | |
| Behavioral | ||||
| Forgo | TH | 42.2 (1.82) | 51.0 (1.83) | 51.0 (1.77) |
| MY | 43.0 (2.58) | 30.0 (2.91) | 21.6 (2.18) | |
| Any FM | 46.2 (1.79) | 50.5 (1.84) | 49.7 (2.08) | |
| RYO only | 33.2 (3.96) | 51.6 (2.85) | 52.4 (2.39) | |
| Avoid | TH | 33.0 (1.37) | 45.5 (0.94) | 49.1 (1.38) |
| MY | 18.2 (2.68) | 15.4 (1.89) | 10.5 (1.92) | |
| Any FM | 36.1 (1.47) | 51.3 (1.30) | 53.8 (1.58) | |
| RYO only | 25.9 (3.04) | 39.0 (1.54) | 44.1 (1.71) | |
Note. FM = factory-made cigarettes; MY = Malaysia; RYO = roll-your-own cigarettes; TH = Thailand. FM and RYO estimates are for Thailand only.
Table 3.
Results of the GEE Analyses Testing the Baseline Country Differences,the Change Over Time for Each Country, and the Country × Time Interaction forLabel-Relevant Outcome Variables
| Salience | Cognitive | Behavioral | ||||
|---|---|---|---|---|---|---|
| Notice | Read | Risk | Quit | Forgo | Avoid | |
| Baseline differences | ||||||
| Thailand vs. Malaysia | 1.77** | 1.51* | 4.80*** | 2.22*** | 0.84 | 2.81*** |
| Change over time | ||||||
| Waves 2 vs. 1 | ||||||
| Thailand | 1.96*** | 1.79*** | 1.91*** | 1.61*** | 1.54*** | 1.91*** |
| Malaysia | 0.80 | 0.96 | 0.88 | 0.63 | 0.59** | 0.94 |
| Waves 3 vs. 2 | ||||||
| Thailand | 1.41** | 0.98 | 1.29* | 1.30** | 1.17* | 1.35*** |
| Malaysia | 1.28 | 1.02 | 0.90 | 0.92 | 0.79 | 0.77 |
| Waves 3 vs. 1 | ||||||
| Thailand | 2.77*** | 1.75*** | 2.47*** | 2.10*** | 1.80*** | 2.58*** |
| Malaysia | 1.02 | 0.98 | 0.79 | 0.58* | 0.47*** | 0.72 |
| Change over time × country interaction | ||||||
| Waves 2 vs. 1 | ||||||
| Thailand vs. Malaysia | 2.46*** | 1.86* | 2.16* | 2.56** | 2.59*** | 2.04** |
| Waves 3 vs. 2 | ||||||
| Thailand vs. Malaysia | 1.10 | 0.96 | 1.44 | 1.42 | 1.49* | 1.74 |
| Waves 3 vs. 1 | ||||||
| Thailand vs. Malaysia | 2.71*** | 1.79* | 3.12*** | 3.63*** | 3.86*** | 3.56** |
Note. FM = factory-made cigarettes; GEE = generalized estimated equation; RYO = roll-your-own cigarettes. All figures in the table are odds ratios adjusted for age, sex, cohort, urban/rural, income, education, ethnicity, smoking frequency, cigarettes smoked per day, and type of products smoked (RYO only vs. any FM).
*p < .05; **p < .01; ***p < .001; p values were adjusted for multiple comparisons using the Benjamini–Hochberg method to control the false discovery rate (Benjamini & Hochberg, 1995).
Moderating Effect of Type of Cigarette Smoked Among Thai Smokers
The descriptive results revealed that there were baseline differences in effectiveness measures by type of cigarette smoked (see Table 2). The results of the GEE analyses (see Table 4) revealed that at baseline (Wave 1) Thai smokers who used any FM cigarettes were more likely to notice (OR = 4.25, 95% CI: 2.92–6.17, < .001) and read the warnings (OR = 3.74, 95% CI: 2.24–6.14, p < .001) than those who smoked exclusively RYO cigarettes. At baseline, Thai FM users were also more likely to say that warning labels made them think about the health risks of smoking (OR = 1.64, 95% CI: 1.18–2.72, p < .01) and that warnings made them more likely to quit smoking (OR = 1.74, 95% CI: 1.19–2.46, p < .01) than those who smoked exclusively RYO. A significant interaction by type of cigarette smoked was found for the two cognitive measures (risk and quit-related thoughts, see Table 4) but not for the two measures of warning salience. Thai exclusive RYO users showed a significantly greater increase in warning-induced risks and quit-related thoughts between Waves 1 and 3 compared to their FM counterparts.
Table 4.
Results of the GEE Analyses Showing the Baseline Differences, the Change Over Time for Each Type of Cigarette Used, and the Type × Time Interaction for Cognitive Responses to Warning Labels in Thailand
| Cognitive | ||
|---|---|---|
| Risk | Quit | |
| Baseline differences | ||
| Any FM vs. RYO only | 1.64** | 1.74*** |
| Change over time | ||
| Waves 2 vs. 1 | ||
| Any FM | 1.75*** | 1.33* |
| RYO only | 2.36*** | 2.26*** |
| Waves 3 vs. 2 | ||
| Any FM | 1.03 | 1.23* |
| RYO only | 1.38* | 1.26* |
| Waves 3 vs. 1 | ||
| Any FM | 1.80*** | 1.63*** |
| RYO only | 3.26*** | 2.84*** |
| Change over time × type interaction | ||
| Waves 2 vs. 1—any FM vs. RYO only | 0.74 | 0.59** |
| Waves 3 vs. 2—any FM vs. RYO only | 0.74 | 0.98 |
| Waves 3 vs. 1—any FM vs. RYO only | 0.55* | 0.58** |
Note. FM = factory-made cigarettes; GEE = generalized estimated equation; RYO = roll-your-own cigarettes. All figures in the table are odds ratios adjusted for age, sex, cohort, urban/rural, income, education, ethnicity, smoking frequency, and cigarettes smoked per day.
*p < .05; **p < .01; ***p < .001; p values were adjusted for multiple comparisons using the Benjamini–Hochberg method to control the false discovery rate.
We also explored whether some of the effects found above could be confounded by the effects of noticing other health risk information about smoking by adding it as a covariate into the GEE models and the results were essentially unchanged, that is, the significant effect for quit-related thoughts remained (results not shown).
DISCUSSION
The new pictorial Thai health warnings, which are larger and contain pictorial images (see Figure 2), covering 50% of the front and back top panel of the packs, were more effective than its old smaller text-only warnings (covering 33.3% of the front and back of cigarette packs). Both the new pictorial, and the old text-only, Thai warnings were more effective than the much smaller, text-only warnings printed on the side of the packs in Malaysia. The effects of the new Thai warnings were sustained 3 years after their implementation. Furthermore, the impact of the new Thai warnings may be even greater on those who smoked only RYO cigarettes as compared to those who smoked at least some FM cigarettes.
Figure 2.
First and second rounds of Thai pictorial warning labels mandated for factory-made cigarette packs.
Note. The last two labels of the second round printed in black and white color designated for commercially produced roll-your-own cigarette packs. Reproduced with permission from the Ministry of Public Health, Thailand.
An important limitation of the study is that we cannot empirically differentiate between the effects of change itself and the effects of the warnings being larger and pictorial as the Malaysian warnings were unchanged. There is little doubt that some of the effects, at least in the first postchange survey represent novelty effects, although the new warnings had been in place for over 1 year at that time, so at least some of the novelty should have worn off. There are a number of reasons for believing that some of the initial effect and also at least some of the sustained effects are due to the stronger characteristics of the new Thai warnings. First, experimental studies consistently show larger and pictorial warnings to be more effective (Hammond, 2011). Second, novelty effects would be expected to have greater effects on salience measures than on subsequent reactions. We found the new set of pictorial warnings not only had greater impact on upstream variable like overall salience (i.e., being noticed or read closely more frequently), they also stimulated even greater changes in downstream cognitive and behavioral reactions, which have been shown previously to be important predictors of subsequent quitting activity (Borland, Yong, et al., 2009; Hammond, 2011). Third, some of the effects were even stronger nearly 3 years after implementation than they were a year or so after. The sustained effects of the new Thai warnings are consistent with international evidence that pictorial warnings suffer less wearout compared to text-only warnings (Hammond, 2011). The updating of the Thai pictorial warnings in February 2007 (between Waves 2 and 3) could also have helped to sustain the effects by reducing habituation and stimulating further cognitive and behavioral reactions as evident by the significant increase in quit-related thoughts and avoidance behavior from Waves 2 to 3. By contrast, the overall trend of the effects of the small warnings in Malaysia shows a decline over the same study period where the warnings did not change. This finding underscores the need for periodical updating of the warnings to prevent wear-out.
A second potential confound is that the observed effects in Thailand could be due at least in part to the major antismoking campaign on passive smoking launched from May to June 2006 (just before our Wave 2 data collection) to educate the public about the harm of secondhand smoke and encourage smokers to not smoke in front of nonsmokers in public places in Thailand. Given that this campaign was not closely related to health warning labels at all, we think confounding from it is very unlikely and the similarity of our findings to those in other countries strengthens the case that the observed onset effects are due to the changed warnings. A third limitation is that sociodemographic differences across the two studied samples along with the higher attrition rate of the Malaysian sample might affect our results but given that key demographic variables were controlled for in all our models and the use of GEE that allows anyone with at least one datapoint to be included, thus maximizing the number of cases available for analysis, our results are unlikely to be affected by any sample differences. One other limitation of this study lies with the fact that it is impossible to determine the relative contributions, and possible interactions, of the various novel elements of the warnings, that is, enhanced text warnings, information on toxic substances and carcinogens, the quitline number (1600), and the new pictorial images. All we can say at this point is that the package of changes has produced marked increases in quitting-related thoughts and microbehavior such as forgoing a cigarette, which are known to predict subsequent quitting activity (Borland, Yong, et al., 2009).
The stronger impact of the new Thai warnings among those who smoke exclusively RYO cigarettes is an intriguing one and somewhat unexpected because no warning labels were required to be displayed on RYO tobacco products until mid-2007 (after our Wave 2 but before Wave 3). At Wave 3, only 2.0% of the exclusive RYO respondents reported that their brand of tobacco products had a health warning label, confirming that the majority of the hand-rolled tobacco comes from the informal economy where no warning labels are required. For this group, any exposure to the warning labels would be incidental via those around them who smoke FM cigarettes or via exposure to discarded packs with warning labels. The evidence in this study suggests that while RYO smokers in Thailand noticed and/or read the new warnings considerably less often compared to their FM counterparts, the psychological reactions of those who reported noticing the new warnings were either as strong or even stronger. This could be due to several factors. One possibility is that the predominantly rural respondents who smoke RYO cigarettes (Young et al., 2008) are finding the messages in pictorial form much easier to process compared to the previously text-based warnings and that these messages are finally getting through to them, consistent with the fact that this group had a lower baseline to start with. A second possibility is that this group of smokers are just more receptive of health messages particularly those espoused by health or government authority compared to those who tend to smoke FM cigarettes. The effect is not due to differential interest in quitting, as it remained when we controlled for this. We also explored the possibility that RYO respondents might be more likely to confuse health risk information from other sources with those from warnings on the tobacco product packaging. However, when we controlled for this potential confounder in our analyses, the greater cognitive reactions among RYO smokers remained, discounting this explanation. On the whole, we think the RYO smokers looked to the manufactured product for information, and cigarette packs are prevalent enough, and the warnings large enough, for them to have effects without having to own them. Future study will explore whether this is the case or not.
A major strength of this study is the use of a longitudinal quasiexperimental design, a comprehensive set of measures covering both upstream (i.e., label salience) and downstream variables (i.e., cognitive and behavioral reactions). Thus, we can be certain that there were changes in reactions and these effects were almost certainly due to the new warnings, given the failure to find effects in the Malaysian sample who were not exposed, and the persistence of the effects when controlling for those potential alternative explanations that we could control for.
In summary, Thailand’s new pictorial health warnings have greater impact than the text-only warning labels they replaced and when refreshed, they help to reduce wear-out. The impact of the new pictorial warnings may be even greater for those who smoke only hand-rolled cigarettes even though they are less frequently exposed to warning labels on a day-to-day basis. Pictorial images enhance the effectiveness of health warning labels by increasing the overall salience of warnings, including making them more salient to other smokers and stimulating greater cognitive and behavioral responses that are predictive of cessation activity. This study provides strong support for introducing pictorial warning labels in LMICs, where the benefits may be even greater given the lower literacy rates and generally lower levels of readily available health information on the risks of smoking.
FUNDING
The research reported in this article was supported by grants P01 CA138389, P50 CA111236 and R01 CA100362 (Roswell Park Transdisciplinary Tobacco Use Research Center) from the U.S. National Cancer Institute, Canadian Institutes for Health Research (57897 and 79551), Thai Health Promotion Foundation, and the Malaysian Ministry of Health.
DECLARATION OF INTERESTS
None declared.
ACKNOWLEDGMENTS
We would like to thank Prof. Dr. Prakit Vathesatogkit for providing useful background details on the Thai health warning policy changes, A/Prof. Naowarut Charoenca for providing details about the Thai antismoking passive smoking campaign, Dr. Charamporn Holumyong for her helpful comments to the earlier drafts of the article and also acknowledge the contribution of the other members of the ITC project team.
Ethics committee approval: The study protocol was cleared for ethics by the Institutional Review Boards or Research Ethics Boards of the University of Waterloo (Canada), Roswell Park Cancer Institute (United States), Universiti Sains Malaysia (Malaysia), Mahidol University (Thailand), and The Cancer Council Victoria (Australia).
REFERENCES
- Benjamini Y., Hochberg Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, 57, 289–300 Retrieved from http://www.jstor.org/pss/2346101 [Google Scholar]
- Borland R., Hill D. (1997). Initial impact of the new Australian tobacco health warnings on knowledge and beliefs. Tobacco Control, 6, 317–325. 10.1136/tc.6.4.317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R., Wilson N., Fong G. T., Hammond D., Cummings K. M., Yong H. H, … McNeill A. (2009). Impact of graphic and text warnings on cigarette packs: findings from four countries over five years. Tobacco Control, 18, 358–364. 10.1136/tc.2008.028043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R., Yong H. H., Wilson N., Fong G. T., Hastings G., Cummings K. M, … McNeill A. (2009). How reactions to cigarette packet health warnings influence quitting: Findings from the ITC Four-Country survey. Addiction, 104, 669–675. 10.1111/j.1360-0443.2009.02508.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalvey Group (2004). Amazing Thailand. Tobacco Journal International, . Retrieved from http://lists.essential.org/pipermail/intl-tobacco/2004q3/001120.html [Google Scholar]
- Doll R., Peto R., Boreham J., Sutherland I. (2004). Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ, 328, 1519. 10.1136/bmj.38142.554479.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fathelrahman A. I., Omar M., Awang R., Borland R., Fong G. T., Hammond D, … Zain Z. (2009). Smokers’ responses toward cigarette pack warning labels in predicting quit intention, stage of change, and self-efficacy. Nicotine & Tobacco Research, 11, 248–253. 10.1093/ntr/ntn029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fathelrahman A. I., Omar M., Awang R., Cummings K. M., Borland R., Shalihin S. A. (2010). Impact of the new Malaysian cigarette pack warnings on smokers’ awareness of health risks and interest in quitting smoking. International Journal of Environmental Research and Public Health, 7, 4089–4099. 10.3390/ijerph7114089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong G. T., Cummings K. M., Borland R., Hastings G., Hyland A., Giovino G. A, … Thompson M. E. (2006). The conceptual framework of the International Tobacco Control (ITC) Policy Evaluation Project. Tobacco Control, 15, (Suppl. III)iii3–iii11. 10.1136/tc.2005.015438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong G. T., Hyland A., Jiang Y., Li Q., Quah A. C. K., Driezen P., … for the ITC China project team. (2010). Perceptions of tobacco health warnings in China compared with picture and text-only health warnings from other countries: An experimental study. Tobacco Control, 19, (Suppl. 2)i69–i77 Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2976466/?tool=pubmed [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D. (2011). Health warning messages on tobacco products: A review. Tobacco Control, 20, 327–337.10.1136/tc.2010.03763 [DOI] [PubMed] [Google Scholar]
- IARC. (Ed.). (2008). Methods for evaluating tobacco control policies, Lyon, France: Author; [Google Scholar]
- Sangthong R., Wichaidit W., Ketchoo C. (2012). Current situation and future challenges of tobacco control policy in Thailand. Tobacco Control, . 10.1136/tc.2011.043331 [DOI] [PubMed] [Google Scholar]
- Silpasuwan P., Yaowaluk N., Viwatwongkasem C., Satitvipawee P., Sirichotiratana N., Sujirarat D. (2008). Potential effectiveness of health warning labels among employees in Thailand. Journal of the Medical Association of Thailand, 91, 551–558 Retrieved from http://jmat.mat.or.th/index.php/jmat/article/view/525/504 [PubMed] [Google Scholar]
- Termsirikulchai L., Benjakul S., Kengganpanich M., Theskayan N., Nakju S. (2008). Thailand tobacco control country profile, Bangkok, Thailand: Mahidol University; Retrieved from http://www.trc.or.th/en/publication/ [Google Scholar]
- Thompson M. E., Fong G. T., Hastings G., Boudreau C., Driezen P., Hyland A, … Laux F. L. (2006). Methods of the International Tobacco Control (ITC) Four Country Survey. Tobacco Control, 15, (Suppl. III)iii12–iii18. 10.1136/tc.2005.013870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrasher J., Villalobos V., Szklo A., Fong G. T., Perez C., Sebrie E, … Bianco E. (2010). Assessing the impact of cigarette package health warning labels: a cross-country comparison in Brazil, Uruguay and Mexico. Salud Publica de Mexico, 52(Suplemento 2), 1–10 Retrieved from http://www.scielosp.org/pdf/spm/v52s2/a16v52s2.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young D., Yong H. H., Borland R., Ross H., Sirirassamee B., Foong K, … Fong G. T. (2008). Prevalence and correlates of roll-your-own smoking in Thailand and Malaysia: Findings of the ITC-South East Asia Survey. Nicotine & Tobacco Research, 10, 907–915. 10.1080/14622200802027172 [DOI] [PubMed] [Google Scholar]