Abstract
Background
Two-part proximal humerus fractures are common orthopedic injuries for which surgical intervention is often indicated. Choosing a fixation device remains a topic of debate.
Purpose
The purpose of this study is to compare two methods of fixation for two-part proximal humerus fractures, locking plate (LP) with screws versus intramedullary nailing (IMN), with respect to alignment, healing, patient outcomes, and complications. To our knowledge, a direct comparison of these two devices in treating two-part proximal humerus fractures has never before been studied. We hope that our results will help surgeons assess the utility of LP versus IMN.
Methods
A retrospective chart review was performed on 24 cases of displaced two-part surgical neck fractures of the humerus. Twelve shoulders were treated using IMN fixation and 12 others were fixated with LP. Data collected included sociodemographic, operative details, and postoperative care and function.
Results
Radiographic comparison of fixation demonstrated an average neck-shaft angle of 124° and 120° in the IMN group and LP group, respectively. Adjusted postoperative 6-month follow-up range of motion was 134° of forward elevation in the IMN group and 141 in the LP group. The differences in range of motion and in complication rates were not found to be significant.
Conclusions
Our results suggest that either LP fixation or IMN fixation for a two-part proximal humerus fracture provides acceptable fixation and results in a similar range of shoulder motion. Although complication rates were low and insignificant between the two groups, a trend toward increased complications in the IMN group is noted.
Keywords: two-part proximal humerus fracture, locking plate, intramedullary nail, outcomes of proximal humerus fractures
Introduction
Despite being a common orthopedic injury (4–5 % of all fractures) [8], management of proximal humerus fractures remains a topic of debate. Treatment is guided by multiple factors including displacement of fracture fragments, the baseline functional status of the patient, hand dominance, and age [17, 20]. Non-operative treatment is the standard of care for non- or minimally displaced proximal humerus fractures, yielding generally good outcomes [6, 12, 20]. Significantly displaced fractures may be treated operatively using a variety of fixation techniques which include percutaneous pinning, locking plate (LP) and screw fixation, intramedullary nailing (IMN), tension band, hemiarthroplasty, or a combination of techniques, with varying degrees of success [17]. The complex peri-articular anatomy and poor bone quality about the proximal humerus make stable fixation a challenging endeavor.
Open reduction and internal fixation (ORIF) with LP and closed reduction with IMN are two of the most common methods of adequately stabilizing Neer [11] two-part proximal humerus fractures. Although acute proximal humerus fractures treated with IMN have shown good results, post-IMN rotator cuff complications have led a trend toward LP fixation as this technique avoids surgical violation of the rotator cuff tendons [13]. Additionally, LP fixation has become increasingly popular due to its enhanced biomechanical properties in those with compromised bone quality [17]. LPs provide a mechanical advantage in comminuted fractures of the metaphysis, particularly in patients with osteopenia or osteoporosis [17]. Indications for LP fixation continue to evolve as long-term outcomes become available. Complications of LP fixation include screw perforation and loosening, plate failure, infection, and varus malalignment with resultant subacromial impingement [3].
IM nailing is a less invasive technique that allows for better preservation of the soft tissue envelope and blood supply to the bony fragments with acceptable bony alignment. However, drawbacks of IMN include increased comminution during placement, inability to achieve adequate compression and stability, shoulder pain and stiffness, rotator cuff dysfunction, and back out of proximal screws [13]. Malalignment with the use of IM nails for two-part fractures of the proximal humerus has been reported in the literature, similar to other metaphyseal fractures such as distal femur or proximal tibia fractures [5, 10, 15].
A recent paper [19] compared IMN to LP in two-part fractures and found similar 1-year outcomes, but literature comparing these two techniques is limited. Therefore, the purpose of this study was to compare the two most common fracture fixation devices—IM nails and LP and screws—in treating two-part proximal humerus fractures. Our null hypothesis was that there would be no clinical, functional, or radiographic differences in patients treated with either device.
Materials and Methods
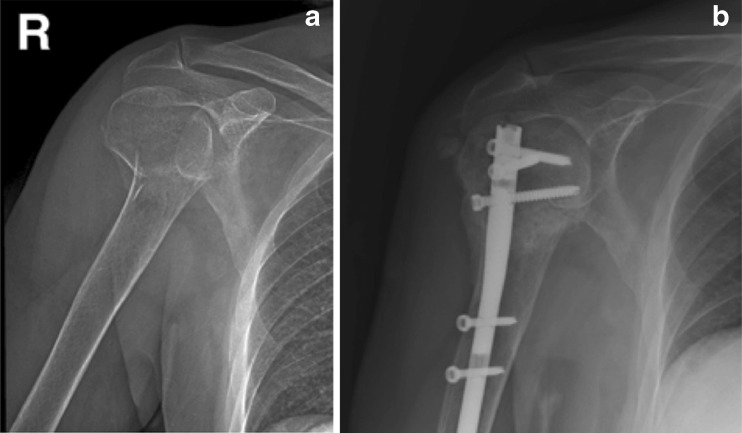
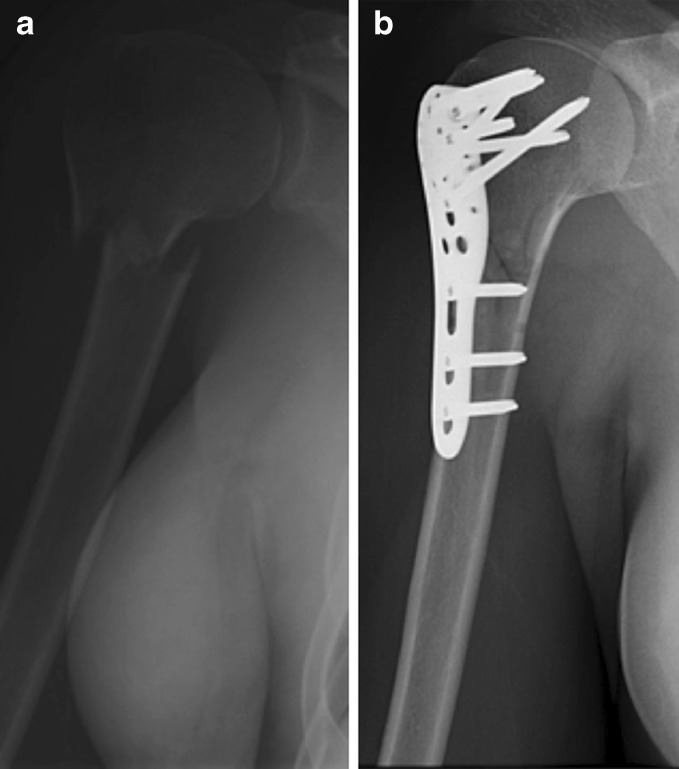
We retrospectively identified 26 shoulders, in 25 patients, with Neer two-part proximal humerus fractures that were treated with either IMN fixation or LP fixation by a single trauma-trained surgeon over a 7-year period. Medical records and radiographs were reviewed with institutional review board approval. Two patients treated with IMN fixation were lost to follow-up. Eleven patients (five male, six female) with 12 fractures and a mean age of 60 years (range, 37–83) were treated with IMN fixation. (Stryker, Mahwah, NJ; Accumed, Trenton, NJ) (Fig. 1). One patient sustained identical contralateral fractures 2 years apart; each fracture was considered separately. Mechanism of injury in this group included 10 falls from a standing height and 2 motor vehicle accidents (MVA) (Table 1). The remaining 12 patients (2 male and 10 female) with a mean age of 59 years (range, 21–81) were treated with a pre-contoured LP and screw construct. (Synthes, Paoli, PA) (Fig. 2). These patients had similar fracture patterns, injury mechanisms, and demographic parameters. Mechanism of injury included 11 falls from standing height and 1 MVA (Table 1).
Fig. 1.
An 85-year-old male who sustained a two-part proximal humerus fracture. The patient underwent IM nail fixation of the fracture. a AP view of the two-part proximal humerus fracture prior to IM nail fixation. b 6-month follow-up AP view following intramedullary nail fixation of a right-sided two-part proximal humerus fracture depicted in Fig. 2a
Table 1.
Patient data: intramedullary nail (top) and locking plate (bottom)
| Number | Age (years) | Length of F/U (months) | Sex | Complication type | FE (°) | Anglea (°) | MOI |
|---|---|---|---|---|---|---|---|
| IM nail | |||||||
| 1 | 75 | 7 | F | Painful hardware | 140 | 110 | Fall |
| 2 | 50 | 46 | M | HO | 160 | 130 | Fall |
| 3 | 42 | 8 | M | 160 | 128 | Fall | |
| 4 | 48 | 12 | M | 120 | 125 | MVA | |
| 5 | 78 | 12 | M | 110 | 128 | Fall | |
| 6 | 83 | 12 | M | HO | 130 | 136 | Fall |
| 7 | 37 | 12 | F | 160 | 120 | MVA | |
| 8 | 75b | 28 | F | HO | 100 | 118 | Fall |
| 9 | 77b | 3 | F | 60 | 124 | Fall | |
| 10 | 72 | 3 | F | 120 | 122 | Fall | |
| 11 | 40 | 9 | F | Painful hardware | 130 | 120 | Fall |
| 12 | 45 | 3 | F | 60 | 122 | Fall | |
| Avg | 60 | 13 | 121 | 124 | |||
| Locking plate | |||||||
| 1 | 81 | 12 | F | 140 | 120 | Fall | |
| 2 | 60 | 6 | F | 160 | 130 | Fall | |
| 3 | 61 | 11 | M | Screw penetration | 130 | 110 | Fall |
| 4 | 21 | 18 | F | 160 | 126 | MVA | |
| 5 | 61 | 12 | F | 180 | 120 | Fall | |
| 6 | 81 | 12 | F | Osteonecrosis | 90 | 112 | Fall |
| 7 | 53 | 12 | F | 140 | 138 | Fall | |
| 8 | 80 | 14 | M | Screw penetration | 140 | 112 | Fall |
| 9 | 68 | 13 | F | Screw penetration | 120 | 115 | Fall |
| 10 | 37 | 25 | F | 175 | 132 | Fall | |
| 11 | 53 | 26 | F | 90 | 106 | Fall | |
| 12 | 50 | 15 | F | 170 | 122 | Fall | |
| Avg | 59 | 15 | 141 | 120 |
aAngle refers to the neck-shaft angle of the humerus
bSame patient, different shoulder 2 years apart
FE forward elevation, MOI mechanism of injury, HO heterotopic ossification
Fig. 2.
A 27-year-old female s/p a fall on an outstretched hand. The patient underwent ORIF with a locking plate. a The two-part proximal humerus fracture prior to locking plate fixation. b The two-part fracture following fixation with a locking plate
IM nailing was performed in the beach chair position, with the affected limb draped free. Initial reduction was achieved closed or with the aid of percutaneously placed Steinman pins used as joy sticks. An anterolateral subacromial approach was used, with care taken to split the deltoid at the junction of the anterior third and posterior two thirds, and to protect the supraspinatus tendon. A starting point just lateral to the articular margin was made and over-reamed. A short (180 mm)-length nail was placed across the fracture and fixed with a minimum of three screws proximally and one distal locking bolt, all placed through stab incisions via a targeting jig. Biplanar fluoroscopy confirmed placement of all implants and the fracture reduction.
Patients who underwent fixation using pre-contoured LP were also placed in the beach chair position. A delto-pectoral approach was used, and fragment mobilization was achieved directly using Kirschner wires. In all cases, the humeral head was elevated and reduced through a lateral cortical window, followed by grafting of the defect with either cancellous chips or calcium phosphate cement. The plate was applied to the lateral aspect of the humeral shaft, just lateral to the bicipital groove. All proximal locking screws were placed in a unicortical fashion through an external guide and confirmed to be within the humeral head with intra-operative fluoroscopy. A minimum of five screws was used in the humeral head to achieve fixation. Antero–postero views, with internal and external rotation of the humerus, and axillary views 90° to each other were used to visualize screw placement. The distal shaft screws were placed bicortically and were a combination of locked and non-locked screws depending on the bone quality. The number of screws utilized within the proximal and distal segments was at the discretion of the treating surgeon. The non-absorbable sutures were tied down to the plate following plate and screw placement.
After surgery, all patients were treated with a similar postoperative protocol. Patients were placed in an arm sling for the first 6 weeks. Isometric deltoid, biceps, and triceps strengthening out of the sling were started on the first postoperative day. Passive range of motion exercises were started at the second week postoperatively and continued for 4–6 weeks until radiographic evidence of fracture healing was apparent, and then, active range of motion with a formal physiotherapy program was begun.
Charts were reviewed for injury and sociodemographic data. The hospital record was reviewed, and the operative details were recorded. Pre-operative radiographs were reviewed and measured for displacement and angulation; postoperative radiographs were reviewed for alignment, healing, and presence of osteonecrosis. Range of shoulder motion was measured with a goniometer, functional outcomes were recorded, and the treating surgeon recorded the development of complications. All patients were followed until there was evidence of radiographic healing of the fracture.
Unanticipated radiographic findings such as calcific tendonitis, heterotopic ossification within the deltoid, and osteonecrosis of the humeral head identified after surgical fixation were considered complications. Secondary surgery to revise or remove hardware was also considered a complication. Fracture malreduction was defined as a neck-shaft angle less than 120°.
Statistical analyses comparing complications, forward elevation, and neck-shaft angle were performed using an unpaired Student's t test.
Results
The quality of reductions and the achievement of overhead forward arm elevation were similar between the groups. Painful hardware and heterotopic ossification at the nail insertion site were noted in a few patients in the IM nail group. Screw penetration was the predominate complication occasionally noted in the LP group (Table 1). The mean length of follow-up in both groups was over 12 months (Table 1). At latest follow-up, the average forward elevation in the IMN group was 121° (range, 60–160) compared with a mean of 141° (range, 90–180) in the LP group. Three patients within the IMN group had less than 6 months of follow-up, two of whom had significant restriction of forward elevation (<60°). When the three IMN patients with less than 6 months of follow-up were excluded from analysis, the adjusted average forward elevation in the IMN group was 134°. While the forward elevation was found to be greater in patients following fixation with a LP as compared to IM nailing even after adjustment for minimum 6-month follow-up, the difference in forward elevation between the two groups was not found to be statistically significant in either (p = 0.14, unadjusted; p = 0.58, adjusted).
In both the IMN and LP groups, all fractures were united on radiographs by 3-month follow-up. The neck-shaft angle measured on radiographs at healing was 124° in the IMN group and 120° in the LP group. The difference between neck-shaft angles in the two groups was not found to be significant (p = 0.34).
Forty-two percent of the patients in the IMN group had a (five shoulders in five patients) complication. Two patients in the IMN group (16.6 %) developed calcification within the deltoid muscle, which resulted in minimal discomfort. One patient (8.3 %) developed a painful heterotopic ossification within the subacromial space, and painful hardware in the proximal shoulder developed in two patients (16.6 %). The LP group had a 33 % (four shoulders in four patients) complication rate including screw penetration (three patients) and osteonecrosis (one patient). One patient (8.3 %) in the LP group developed an asymptomatic osteonecrosis. Three patients (25 %) in the LP group had hardware penetration of the articular surface, two of which required hardware removal. The difference in complication rate was not significant.
Discussion
While various methods for proximal humerus fracture fixation exist, most of which are fragment specific, to our knowledge, the literature does not document a direct comparison of IMN to LP and screw fixation in treating Neer two-part proximal humerus fractures with devices available in the USA. Putti et al. [14] reported findings on the comparison of these two methods for the fixation of humeral shaft fractures, and while they found similar functional outcomes at 24-month follow-up on the American Shoulder and Elbow Surgeons (ASES) scale (45.2 with IMN and 45.1 with locking plate), their results demonstrated a significant difference in complication rate. Among their 34 patients, there was a 50 % complication rate in the IMN group compared to 17 % in the LP group. The high complication rate in the IMN group made IMN less attractive to surgeons who regularly treat proximal humerus fractures. However, the study did not account for severity of the injury when creating each cohort. By examining more simple two-part fracture patterns, our study aimed to determine whether the findings from Putti et al. were implant or fracture related.
One of our study's shortcomings was that we used forward elevation as our primary measurement of clinical outcome. As the cohorts were retrospectively identified, other values such as internal rotation, external rotation, and abduction were not charted in entirety and were thus left out of our comparison. We therefore used forward elevation as a surrogate for functional outcome. Forward elevation is a component of the ASES scale commonly used to assess function after upper extremity trauma. Other validated outcome measures such as the Constant score, DASH, or UCLA Shoulder score could also be used to assess functional outcomes, but those scores were not documented in the medical records, nor could they be reconstructed from the data. Our findings suggest that those treated with IMN have a greater limitation in range of motion. However, when compared to LP, this difference was not statistically significant (p = 0.14, p (adjusted) = 0.58).
Another shortcoming of our paper was the relatively small number of patients in each cohort. We were unable to perform a multivariate regression analysis to analyze other factors that may predispose patients to malreduction. Although Neer two-part proximal humerus fractures are common injuries, those requiring surgical fixation are much less common. This study sought to compare two different surgical fixation techniques between homogenous groups with respect to the injury pattern. Thus, our study population is not very large.
Popescu et al. [13] and Sudkamp et al. [17] reported on non-comparative range of motion outcomes following proximal humerus fractures treated with IMN and locking plate, respectively [13, 17]. Patients treated with IMN were found to have an average forward elevation of 135° at 12 months of follow-up [13], while a similar study [4] found an average forward elevation of 147.3° at 24 months of follow-up. Patients treated with ORIF and locking plate had an average forward elevation of 132 ± 35° at 12 month follow-up [17]. These outcomes are similar to those found in our study after adjustment for patients with less than 6 months follow-up. These findings suggest that the ultimate range of motion may differ by several degrees and may not make a difference in overall functional outcome.
Trepat et al. [19] compared LP and IMN in two-part proximal humerus fractures and found similar outcome scores using the UCLA score, Constant score, and Oxford score. They found no differences in the functional outcome of humeral head fracture treatment using either an angular stable plate or an angular stable antegrade nail. However, approach-related complications have been appearing more frequently in the LP group. Trepat et al. postulated that this is probably due to increased surgical approach requiring more soft tissue dissection and that maybe with a minimally invasive technique, particularly in two-part fractures, this complication could be avoided. They found no difference in range of motion with FE of 130 in the IMN group and 131 in the LP group. They reported an average neck-shaft angle of 121 in the IMN group and 125 in the LP group after surgical fixation.
Konrad et al. [9] compared LP and IMN in three-part fractures and found similar outcome scores and results. The majority of their complications were secondary to surgical technique in which screw penetration into the joint was not recognized during surgery. They concluded that surgical technique is more critical than implant selection.
Our study found that decreased range of motion is related to the length of follow-up. After matching for age, sex, and fracture pattern, the large disparity in length of follow-up dramatically alters the average range of motion of the two treatment groups. However, with similar follow-up and postoperative physical therapy regimens, the difference in range of motion between the two groups becomes unremarkable.
Our results found that the percentage of complications was greater in the IMN group than the locking plate group. This difference was not statistically significant and was limited by our small cohorts. Results from two separate studies found a 34 % complication rate among 187 patients treated with a locking proximal humerus plate [18] as compared to a 51.3 % complication rate in 115 patients treated with IMN [13]. These complication rates are similar to those found in our comparison of IMN vs. LP of 42 and 33 %, respectively. The difference in complication rates was not specific to the location of the fracture in the humerus as IMN was also found to have a greater complication rate when compared to locking plate in the treatment of humeral shaft fractures (51 vs. 17 %)[16]. One of the most common complications reported with IMN was back out of the nail [7, 11] which caused 44 % of the total number of complications in one study [7]. Brunner et al. [2] reported primary screw perforation through the glenohumeral articular joint surface as the most common complication following fixation of proximal humerus fractures with a locking plate, and secondary screw perforation was noted as the second most common complication at 23 % of all complications. Our findings are consistent with the literature as 75 % of complications in the LP group were intraarticular screw perforation.
Varus malreduction is a complication reported in both types of fixation. Agudelo et al. [1] found that among 73 patients treated with a locking plate, 30.4 % of those with a neck-shaft angle less than 120° developed loss of fixation as compared to only 11 % in patients with a postoperative neck-shaft angle greater than 120° [1]. This suggests that varus malreduction is a risk factor for loss of fixation and should be carefully assessed during surgery. Popescu et al. [13] reported a mean postoperative neck-shaft angle of 123° in proximal humerus fractures treated with IMN while Agudelo et al. [1] reported a mean angle of 130°. We obtained acceptable calcar reduction, which we found to be inherent in obtaining an acceptable neck-shaft angle. Comminution is more likely to result in varus collapse, although we did not observe this in our cohort of patients because they did not have much calcar comminution. Our study demonstrated that both IMN and LP fixation methods yielded no significant difference in postoperative neck-shaft angle with 124° and 120° in the IMN and LP group, respectively (p = 0.34). Both treatments resulted in neck-shaft angles that were at or greater than 120°, which proved that varus malreduction can be avoided and is not attributed to the type of implant used.
There are multiple factors that are considered when deciding on a method of fixation for proximal humerus fractures. While our analysis of these two methods is limited by sample size, our results suggest a trend toward greater complication rates following IMN fixation. Although this difference is not statistically significant, evidence drawn from across multiple studies indicates that IMN treatment continually results in greater complication rates when compared to ORIF with locking plate in the treatment of proximal humerus fractures. The common complication found in locking plate fixation was primary screw perforation, resulting from incorrect surgical technique and fracture compression [11, 18]. Complications following IMN fixation included screw back out [7, 11], which is a result of the implant itself. Skill and comfort of the surgeon play a significant factor in the decision to use one method of fixation over the other.
In conclusion, both IM nailing and ORIF with locking plate are viable options for treatment of displaced two-part proximal humerus fractures that require operative stabilization. Restricted shoulder range of motion as evidenced by decreased forward elevation following IM nailing may be related to violation of the rotator cuff musculature and may not be a result of the IM nail itself. Future investigation with a large, randomized study may provide greater insight into which factors in a patient's fracture and operative considerations affect their ultimate outcome.
Acknowledgments
Disclosures
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a significant conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Footnotes
Level of Evidence: Level III-2 (retrospective cohort study): Therapeutic Study
This work was performed at the New York University Hospital for Joint Diseases.
References
- 1.Agudelo J, Schürmann M, Stahel P, Helwig P, Morgan SJ, Zechel W, et al. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21(10):676–681. doi: 10.1097/BOT.0b013e31815bb09d. [DOI] [PubMed] [Google Scholar]
- 2.Brunner F, Sommer C, Bahrs C, Heuwinkel R, Hafner C, Rillmann P, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009;23(3):163–172. doi: 10.1097/BOT.0b013e3181920e5b. [DOI] [PubMed] [Google Scholar]
- 3.Egol KA, Ong CC, Walsh M, Jazrawi LM, Tejwani NC, Zuckerman JD. Early complications in proximal humerus fractures (OTA Types 11) treated with locked plates. J Orthop Trauma. 2008;22(3):159–164. doi: 10.1097/BOT.0b013e318169ef2a. [DOI] [PubMed] [Google Scholar]
- 4.Esser RD. Treatment of three- and four-part fractures of the proximal humerus with a modified cloverleaf plate. J Orthop Trauma. 1994;8(1):15–22. doi: 10.1097/00005131-199402000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop Relat Res. 1995;315:25–33. [PubMed] [Google Scholar]
- 6.Handoll H, Brealey S, Rangan A, Torgerson D, Dennis L, Armstrong A, et al. Protocol for the ProFHER (PROximal Fracture of the Humerus: Evaluation by Randomisation) trial: a pragmatic multi-centre randomised controlled trial of surgical versus non-surgical treatment for proximal fracture of the humerus in adults. BMC Musculoskelet Disord. 2009;10:140. doi: 10.1186/1471-2474-10-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawkins RJ, Bell RH, Gurr K. The three-part fracture of the proximal part of the humerus. Operative treatment. J Bone Joint Surg Am. 1986;68(9):1410–1414. [PubMed] [Google Scholar]
- 8.Horak J, Nilsson BE. Epidemiology of fracture of the upper end of the humerus. Clin Orthop Relat Res. 1975;112:250–253. doi: 10.1097/00003086-197510000-00032. [DOI] [PubMed] [Google Scholar]
- 9.Konrad G, Audigé L, Lambert S, Hertel R, Südkamp NP. Similar outcomes for nail versus plate fixation of three-part proximal humeral fractures. Clin Orthop Relat Res. 2012;470(2):602–609. doi: 10.1007/s11999-011-2056-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koval KJ, Clapper MF, Brumback RJ, Ellison PS, Poka A, Bathon GH, Burgess AR. Complications of reamed intramedullary nailing of the tibia. J Orthop Trauma. 1991;5(2):184–189. doi: 10.1097/00005131-199105020-00011. [DOI] [PubMed] [Google Scholar]
- 11.Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- 12.Osman N, Touam C, Masmejean E, Asfazadourian H, Alnot JY. Results of non-operative and operative treatment of humeral shaft fractures. A series of 104 cases. Chir Main. 1998;17(3):195–206. doi: 10.1016/s0753-9053(98)80039-2. [DOI] [PubMed] [Google Scholar]
- 13.Popescu D, Fernandez-Valencia JA, Rios M, Cuñé J, Domingo A, Prat S. Internal fixation of proximal humerus fractures using the T2-proximal humeral nail. Arch Orthop Trauma Surg. 2009;129(9):1239–1244. doi: 10.1007/s00402-008-0789-1. [DOI] [PubMed] [Google Scholar]
- 14.Putti AB, Uppin RB, Putti BB. Locked intramedullary nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong). 2009;17(2):139–141. doi: 10.1177/230949900901700202. [DOI] [PubMed] [Google Scholar]
- 15.Russell TA, Mir HR, Stoneback J, Cohen J, Downs B. Avoidance of malreduction of proximal femoral shaft fractures with the use of a minimally invasive nail insertion technique (MINIT) J Orthop Trauma. 2008;22(6):391–398. doi: 10.1097/BOT.0b013e31817713fe. [DOI] [PubMed] [Google Scholar]
- 16.Savoie FH, Geissler WB, Vander Griend RA. Open reduction and internal fixation of three-part fractures of the proximal humerus. Orthopedics. 1989;12(1):65–70. doi: 10.3928/0147-7447-19890101-09. [DOI] [PubMed] [Google Scholar]
- 17.Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91(6):1320–1328. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 18.Tanner MW, Cofield RH. Prosthetic arthroplasty for fractures and fracture-dislocations of the proximal humerus. Clin Orthop Relat Res. 1983;179:116–128. doi: 10.1097/00003086-198310000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Trepat AD, Popescu D, Fernández-Valencia JA, Cuñé J, Rios M, Prat S. Comparative study between locking plates versus proximal humeral nail for the treatment of 2-part proximal humeral fractures. Eur J Orthop Surg Traumatol. 2012. (In press)
- 20.Zyto K. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury. 1998;29(5):349–352. doi: 10.1016/S0020-1383(97)00211-8. [DOI] [PubMed] [Google Scholar]