Abstract
Electrodiagnostic studies are used to anatomically localize nerve injuries. These tests help differentiate between cervical radiculopathies, brachial plexopathies, and peripheral nerve injuries. They also help to identify or rule out other underlying neurological diseases and disorders. In this case report, a 22-year-old male swimmer presented with left finger extensor weakness following pull-up exercises. Left wrist extension remained intact. Electrodiagnostic testing revealed a severe but incomplete posterior interosseous neuropathy. Magnetic resonance imaging confirmed inflammation of the nerve in the forearm. Posterior interosseous neuropathy is an uncommon but well-studied condition. Typically, this condition presents with weakness in finger and thumb extension with preserved wrist extension as the extensor carpi radialis longus is innervated proximal to the site of nerve compression in most cases. It is important to understand the anatomic course and distribution of the radial nerve in order to make an accurate diagnosis. Once the anatomy is understood, electrodiagnostic testing may be used to identify the location of nerve injury and exclude other disorders.
Keywords: posterior interosseous nerve, nerve injury, electromyography (EMG), electrodiagnostics, finger extension weakness
Introduction
Posterior interosseous neuropathy (PIN) injury can occur at any point along the course of the nerve. The etiology of nerve impairment may include trauma [5], brachial neuritis [15], mass lesions [30], repetitive overuse, and systemic diseases including diabetes and rheumatoid arthritis [31]. Other less common disorders such as motor neuron disease, multifocal motor neuropathy, hereditary brachial plexopathy, and monomelic amyoptrophy can also cause sudden weakness [12].
Posterior interosseous neuropathy is an entrapment of the deep branch of the radial nerve in the forearm. The deep branch of the radial nerve is primarily a motor nerve, and compression of this nerve may lead to weakness in finger and thumb extension without sensory abnormalities. PIN injury is uncommon and occurs less frequently than median and ulnar neuropathies in the upper extremity [7]. It accounts for less than 0.7% of all upper limb peripheral nerve compression syndromes [10].
Clinically PIN entrapment can be difficult to distinguish from lateral epicondylitis, radial nerve injury, radial tunnel syndrome, cervical radiculopathy, and brachial plexopathy based on physical exam alone and therefore diagnosis may be difficult to make. In considering the diagnosis it is important to understand the anatomical course of the radial nerve. Electrodiagnostic studies are useful in localizing the nerve injury to the posterior interosseous nerve excluding other disorders. Electrodiagnostic studies are also useful to determine severity of injury and predict prognosis.
Case Report
A 22-year-old left-handed male presented with left finger weakness. Three months prior to presentation, he had completed his swimming season and had returned to the gym to exercise. He was doing pull-ups when he noticed a tightness and discomfort at the lateral side of his left elbow. The next day he could not extend his arm secondary to pain and tightness. The pain improved after several days; however, he began to notice weakness with left finger extension. On presentation, 3 months after onset, he reported mild pain at the left elbow and weakness with finger extension. He denied any loss of sensation, numbness, or tingling. He denied any neck pain or shoulder weakness. A review of systems was otherwise normal. His past medical history was significant for left shoulder laxity in 2005 for which he underwent arthroscopic capsular plication and bursectomy in 2006.
On physical exam, inspection revealed mild asymmetry with subtle muscle atrophy in the left posterior forearm. His cervical spine demonstrated full painless cervical range of motion with no exacerbation in the left upper extremity symptoms. Spurling’s maneuver was negative bilaterally. Examination of the left shoulder revealed full painless range of motion without any signs of shoulder impingement. There was mild tenderness on palpation a few centimeters distal to the left lateral epicondyle. There was no laxity or instability noted at the left elbow. Strength examination revealed 2/5 strength with extension of the second, third, fourth, and fifth digits at the metacarpophalangeal (MCP) joints on the left and 3+/5 strength with left thumb extension. The remainder of his strength exam including left wrist flexion and extension, forearm pronation and supination, and finger flexion was 5/5 in both upper extremities. Sensation was intact to light touch and pinprick throughout the upper extremities. Reflexes were present and symmetric in the upper extremities. Hoffman’s sign was negative bilaterally.
Electromyographic and nerve conductions studies were performed 6 months after the onset of symptoms. Motor nerve conduction studies demonstrated slowed left radial motor conduction velocity across the elbow, prolonged distal latency, and reduced amplitude at the forearm and the spiral groove when compared to the right radial nerve (Table 1). Motor conduction studies of the median and ulnar nerves were normal. Sensory nerve conduction studies, including the left superficial radial sensory nerve, were normal (Table 2). All F waves were within normal limits.
Table 1.
Motor nerve conduction studies
| Site | NR | Onset (ms) | Normal onset (ms) | O-P amp (mV) | Normal O-P amp | Site 1 | Site 2 | Delta-O (ms) | Dist (cm) | Vel (m/s) | Normal Vel (m/s) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Left median motor (Abd Poll Brev), 31°C | |||||||||||
| Wrist | 3.0 | <3.6 | 11.5 | >4 | Pron Ter | Wrist | 4.7 | 29.0 | 62 | >50.0 | |
| Pron Ter | 7.7 | 11.4 | |||||||||
| Left radial (surface) motor (Ext Ind Prop), 31.1°C | |||||||||||
| Forearm | 3.6 | 2.2 | Sp Groove | Forearm | 4.4 | 20.5 | 47 | ||||
| Sp Groove | 8.0 | 2.1 | |||||||||
| Right radial (surface) motor (Ext Ind Prop), 31°C | |||||||||||
| Forearm | 2.7 | 4.8 | Sp Groove | Forearm | 2.8 | 18.0 | 64 | ||||
| Sp Groove | 5.5 | 4.4 | Sp Groove | Sp Groove | 0.0 | 0.0 | |||||
| Left ulnar segment motor (Abd Dig Minimi), 30.7°C | |||||||||||
| Wrist | 3.1 | <3.6 | 9.2 | >3 | Abv FCU | Wrist | 3.8 | 23.0 | 61 | >50 | |
| Abv FCU | 6.9 | 9.1 | Abv Uln Grv | Abv FCU | 2.0 | 12.0 | 60 | >50 | |||
| Abv Uln Grv | 8.9 | 8.5 | |||||||||
NR nerve, O-P onset to peak, Dist distance, Vel velocity, Abd Poll Brev abductor pollicis brevis, Ext Ind Prop extensor indicis proprius, Abd Dig Minimi abductor digiti minimi, Pron Ter pronator teres, Sp Groove spiral groove, Abv FCU above flexor carpi ulnaris, Abv Uln Grv above ulnar groove
Table 2.
Sensory nerve conduction studies
| Site | NR | Onset (ms) | Normal onset (ms) | O-P Amp (μV) | Normal O-P amp | Site 1 | Site 2 | Delta-O (ms) | Dist (cm) | Vel (m/s) | Normal Vel (m/s) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Left median D2 sensory (2nd digit), 30.4°C | |||||||||||
| Wrist | 2.7 | < 3.2 | 56.4 | > 10 | |||||||
| Left superficial radial sensory (FWS), 30.7°C | |||||||||||
| Forearm | 1.8 | 41.9 | > 10 | Forearm | FWS | 1.8 | 11.0 | 61 | >45 | ||
| Right superficial radial sensory (FWS), 31.7°C | |||||||||||
| Forearm | 1.5 | 34.7 | > 10 | Forearm | FWS | 1.5 | 10.0 | 67 | >45 | ||
| Left ulnar sensory (5th digit), 30.1°C | |||||||||||
| Wrist | 2.5 | < 3.2 | 46.6 | > 10 | Wrist | 5th digit | 2.5 | 0.0 | |||
NR nerve, O-P Amp onset to peak amplitude, Dist distance, Vel velocity, Norm Vel normal velocity, FWS first web space
Electromyographic needle examination (Table 3) revealed severely abnormal spontaneous activity in the form of positive sharp waves and fibrillations, discrete recruitment pattern, and decreased recruitment interval in posterior interosseous innervated muscles tested [the left extensor indicis proprius (EIP) and the extensor digitorum communis (EDC)]. The left extensor carpi radialis brevis (ECRB), which studies have shown can be innervated by either the posterior interosseous nerve or the radial nerve [9], also showed moderately abnormal spontaneous activity and a decreased recruitment pattern. The radially innervated brachioradialis was normal. These findings demonstrate denervation of the left posterior interosseous innervated muscles with sparing of radial innervated muscles and a preserved superficial sensory radial nerve. We felt that these findings were most consistent with a diagnosis of severe but incomplete left posterior interosseous neuropathy.
Table 3.
Needle electromyography
| Side | Muscle | Nerve | Root | Ins Act | Fibs | PSW | Fascic | Amp | Dur | Configuration | Rec Pat | Rec Int |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Left | Abd Poll Brev | Median | C8–T1 | 0 | 0 | 0 | 0 | Nml | Nml | Di/triphasic | Full | Nml |
| Left | 1st Dor Int | Ulnar | C8–T1 | 0 | 0 | 0 | 0 | Nml | Nml | Di/triphasic | Full | Nml |
| Left | Flex Car Rad | Median | C6–C7 | 0 | 0 | 0 | 0 | Nml | Nml | Di/triphasic | Full | Nml |
| Left | Triceps (Lat Hd) | Radial | C6–C7 | 0 | 0 | 0 | 0 | Nml | Nml | Di/triphasic | Full | Nml |
| Left | Biceps | Musculocutaneous | C5–C6 | 0 | 0 | 0 | 0 | Nml | Nml | Di/triphasic | Full | Nml |
| Left | Deltoid (Mid) | Axillary | C5–C6 | 0 | 0 | 0 | 0 | Nml | Nml | Di/triphasic | Full | Nml |
| Left | Flex Poll Long | Median (Ant Int) | C7–C8 | 0 | 0 | 0 | 0 | Nml | Nml | Di/triphasic | Full | Nml |
| Left | Ext Indicis | Radial (Post Int) | C7–C8 | 2+ | 3+ | 0 | 0 | Nml | Nml | Di/triphasic | Discrete | Dec |
| Left | Ext Car Rad | Radial | C6–C7 | 2+ | 2+ | 0 | 0 | Nml | Nml | Di/triphasic | Dec | Nml |
| Left | Ext Dig Com | Radial (Post Int) | C7–C8 | 2+ | 3+ | 0 | 0 | Nml | Nml | Di/triphasic | Discrete | Dec |
| Left | Brachio Rad | Radial | C5–C6 | 0 | 0 | 0 | 0 | Nml | Nml | Di/triphasic | Full | Nml |
Abd Poll Brev abductor pollicis brevis, 1st Dor Int first dorsal interosseous, Flex Car Rad flexor carpi radialis, Flex Poll Lon flexor pollicis longus, Ext Indicis extensor indicis proprius, Ext Car Rad extensor carpi radialis brevis, Ext Dig Com extensor digitorum communis, BracioRad brachioradialis, Ins Act insertional activity, Fibs fibrillations, PSW positive sharp waves, Fasic fasciculations, Amp amplitude, Dur duration, Rec Pat recruitment pattern, Rec Int recruitment interval
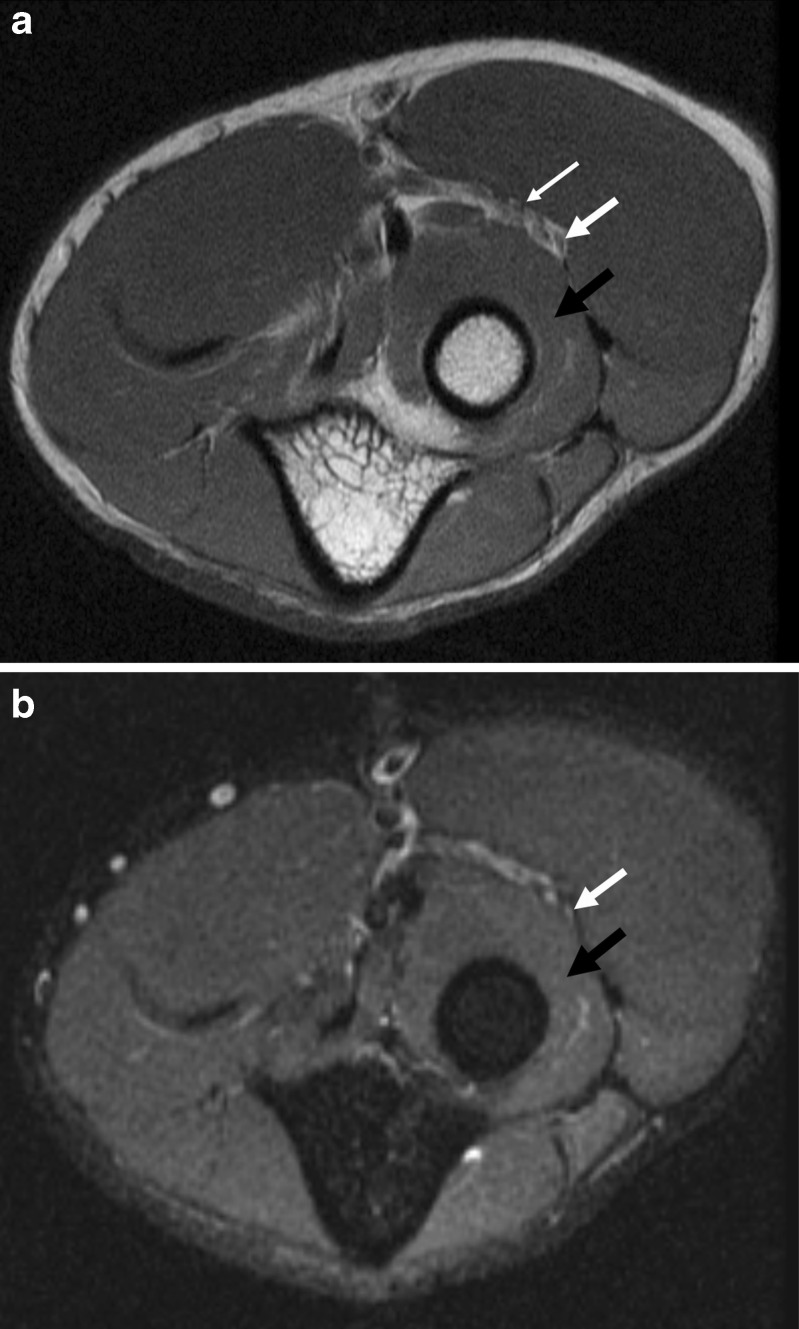
Standard AP and lateral radiographs of the left elbow were negative for an osseous or articular abnormality. Magnetic resonance image (MRI) of the left elbow (Fig. 1a, b) demonstrated signal hyperintensity in the posterior interosseous nerve, consistent with neuritis. No mass lesion was seen to compress the posterior interossoeous nerve. There was normal signal intensity in the supinator muscle, with no evidence of a denervation effect.
Fig. 1.
Axial fast spin echo (a) and inversion recovery (b) images of the left elbow demonstrate increased signal intensity in the posterior interosseous nerve (thick white arrow), without mass compression of the nerve. The superficial branch of the radial nerve (thin white arrow) has a normal signal and morphology. The supinator muscle has a normal signal, without evidence of a denervation effect (black arrow)
The patient completed 2 months of physical therapy. At 1 year post-initial injury, he reported full range of motion of his left wrist and fingers and an 85% improvement in his finger strength. He denied any limitations in daily activities. He continues to perform home strengthening exercises for his left upper extremity.
Discussion
Posterior interosseous nerve entrapment syndrome is rare. It accounts for less than 0.7% of all upper limb peripheral nerve compression syndromes [10] and has an annual incidence estimated to be 0.003% [7, 13]. In 25% of patients, PINS occurs following trauma (such as forearm fractures and crush injuries) and 15% may be iatrogenic following the reduction of a radial fracture, or release of the common extensor origin for treatment of lateral epicondylitis [18, 32]. The remaining cases develop spontaneously.
It is important to understand the radial nerve’s anatomic course and distribution in order to properly diagnose a radial nerve entrapment syndrome. The radial nerve is the largest nerve in the upper extremity, and it has a long and tortuous course. It arises as an extension from the posterior cord of the brachial plexus. It contains fibers from C5–T1 as they travel through the superior, middle, and inferior trunks of the brachial plexus to the posterior cord. In the upper arm, the radial nerve lies medial to the humerus and innervates the three heads of the triceps (lateral, long, and medial) and the anconeus. As it descends it gives off three sensory branches: the posterior cutaneous nerve of the arm, the lower lateral cutaneous nerve of the arm, and the posterior cutaneous nerve of the forearm. The radial nerve then passes through the lateral and medial heads of the triceps and follows the spiral groove of the humerus. It pierces the lateral intermuscular septum below the insertion of the deltoid to enter the anterior compartment of the arm approximately 5–12 cm proximal to the elbow [7].
In the anterior compartment of the arm, the radial nerve lies lateral to the humerus and innervates the brachioradialis, the extensor carpi radialis longus (ECRL), and the often the ECRB (alternatively, the ECRB may be innervated by the PIN). It then enters the radial tunnel, which is a potential space formed by the capitellum of the humerus and radiocapitellar joint posteriorly, the brachialis muscle medially, and the brachioradialis and ECRB muscles anteriorly and laterally [21, 23, 24]. The radial tunnel is approximately 5 cm long [32], it encompasses the space between where the radial nerve pierces the lateral intermuscular septum of the arm and where the PIN pierces the proximal edge of the supinator [1]. Alternatively some authors believe that the radial tunnel extends to the distal border of the supinator [21]. In the proximal forearm, the radial nerve divides into its two terminal branches: the superficial radial and the posterior interosseous nerves. The point of bifurcation is varied. Studies have shown that it occurs within an area of 3 cm proximal or distal to the elbow and therefore the split is not always in the radial tunnel [14].
The superficial radial nerve is a purely sensory nerve which runs under the brachioradialis in the forearm. It innervates the skin of the proximal two thirds of the extensor surface of the thumb, index, and middle fingers, and one half of the ring finger as well as the dorsum of the hand.
The deep terminal branch of the radial nerve is the posterior interosseous nerve. It innervates and then pierces the supinator muscle through the arcade of Frohse, a fibrous ring at the proximal edge of the supinator. At the distal end of the supinator, it divides into two branches [21]. The medial branch (also known as the recurrent branch) innervates the superficial layer of extensor muscles (the extensor carpi ulnaris, EDC, extensor digiti minimi and at times the ECRB). The lateral branch (also called the descending branch), innervates the deep muscle layer (the extensor pollicis longus and brevis, abductor pollicis longus (APL) and the EIP) [28]. Innervation of the ECRB and the supinator may arise from the radial nerve proper or from the proximal part of the posterior interosseous nerve prior to piercing the supinator muscle and often proximal to compression of the nerve [2, 8]. Studies have shown that the ECRB muscle may be innervated by the radial nerve, the PIN, or the superficial radial nerve. In a study of 30 cadavers, Kirici et al. showed that the ERCB was innervated by the PIN in 47% of the cadavers and the remaining 53% were innervated by the radial nerve [11].
Prior to entering the supinator muscle, the PIN also provides recurrent sensory branches to the annular ligament, the anterior radial humeral joint, and the periosteum of the lateral epicondyle [12, 16]. Distal to the tunnel, the PIN carries sensory fibers to the ligaments and joints of the wrist, the interosseous membrane of the forearm, and the periosteum of the radius [24].
The radial nerve or more distally the PIN and its branches can be compressed at any point along its course. The most common site for compression of the radial nerve/PIN in the forearm occurs at the radial tunnel [20]. In the radial tunnel, there are five potential sites of compression of the radial/posterior interosseous nerve [10]. The first site is the fibrous bands at the proximal edge of the ECRB. The second site is at the thickened fascial tissue superficial to the radiocapitellar joint between the brachialis and brachioradialis. The third site is at the leash of Henry (arterial branches that arise from the recurrent radial artery and cross over the PIN). The fourth site is at the arcade of Frohse (the proximal superior portion of the supinator), and the fifth site is at the distal edge of the supinator [10].
PIN compression is most commonly associated with tendinous hypertrophy of the arcade of Frohse [27]. Vascular compression by the leash of Henry has also been reported although it is rare [6]. Compression of the posterior interosseous nerve in the forearm can lead to two distinct syndromes: radial tunnel syndrome (RTS) and PIN syndrome. Many believe that these two syndromes represent a spectrum of disorders with varying degrees of compression of the PIN [20].
Radial tunnel syndrome is somewhat of a controversial diagnosis which has varied definitions. It is believed to be caused by irritation of the distal radial nerve or PIN (depending on where the nerve bifurcates) secondary to compression by muscles in the forearm which make up the radial tunnel. Some describe it as a compression of the nerve at the lateral intermuscular septum of the arm, proximal to the supinator muscle. Others describe it as a compression of the nerve at either the radiocapitellar joint, the fibrous bands at the radial head, or at the ECRB [3, 25]. In contrast, posterior interosseous neuropathy is a rare yet well-described and accepted syndrome.
Clinically RTS and PIN syndrome present differently. Patients with PIN syndrome typically present with loss of motor function. Rather than weakness, patients with RTS present with lateral proximal forearm pain typically worse with activity. Clinically the diagnosis of RTS may be extremely difficult to distinguish from lateral epicondylitis. In lateral epicondylitis, the focal point of tenderness is at the insertion of the extensor carpi radialis brevis at the lateral epicondyle. In RTS, pain is characteristically located 3–4 cm distal to the lateral epicondyle in the area of the radial tunnel [7]. Electrodiagnostic studies in RTS are often unrevealing [4, 7], as can be seen in cases of mild neuropraxia. In these cases nerve conduction velocities, distal latencies, and needle EMG may be normal.
PIN syndrome occurs when there is compression of the PIN outside of the radial tunnel. Entrapment of the nerve is actually very rare [28]. Patients present with weakness of finger and thumb extension at the MCP joint [24]. Extension at the interphalangeal joints is preserved as the interossei and lumbrical muscles are intact. The wrist may deviate radially as the ECU is involved while the ECRL (and often the ECRB) are spared. Thumb abduction may also be weak as the APL is involved [24]. Partial PIN lesions are seen when isolated branches of the PIN are compressed. No sensory loss is typically observed.
PIN syndrome was first described in an orchestral conductor in 1905 by Guillain and Courtellemont [19]. It was hypothesized that the trauma to the nerve was caused by repetitive alternation of pronation and supination. It has been shown that the posterior interosseous nerve is displaced during supination and pronation. In supination the PIN moves laterally away from the midline which produces lengthening of the nerve [17]. If the supinator muscle is tight, it can passively compress the PIN in pronation [17]. A study by Werner et al. showed pressures of 40–50 mmHg compressing the PIN during passive stretch of the supinator. During active contraction of the supinator, the pressure increased four times [29]. It has been postulated that elbow flexion with forearm pronation may compress the brachioradialis and generate high pressures over the supinator muscle [9]. This is particularly interesting as this case of PIN occurred in a patient utilizing this position while doing pull-ups.
PIN lesions may also occur as a result of trauma, most often the result of Monteggia fractures where the proximal ulna is fractured and the radial head dislocates posteriorly [5]. Traumatic PIN injuries have also been described in case reports after intravenous cannulation of the forearm and penetrating injuries to the forearm [22, 28]. Space-occupying lesions in the forearm such as tumors, hematomas, fibromas, and ganglion cysts may also lead to PIN injury. Lipomas are the most common benign tumor associated with PIN injury [30]. Rheumatoid synovitis of the elbow joint may also cause posterior interosseous nerve palsy by compressing the nerve against the arcade of Frohse [31]. Prolonged compression with the use of a forearm orthosis has also been associated with PIN syndrome [26].
The diagnosis of PIN syndrome may be difficult to make on clinical examination alone. In this case electrodiagnostic testing assisted in making the diagnosis. Motor nerve conduction studies demonstrated slowed left radial motor conduction velocity across the elbow, prolonged distal latency, and reduced amplitude when compared to the right. The reduced amplitude of the left radial motor nerve may be secondary to axonal loss. Amplitudes may also be reduced with neuropraxic injuries (i.e., conduction block or when there is temporal dispersion). The slowing of the radial nerve conduction velocity may be secondary to demyelination. Motor nerve slowing can also occur with axonal dropout. Electromyographic needle examination helped to further localize the injury and rule out a lesion at the brachial plexus. A posterior cord brachial plexopathy was also ruled out based on normal findings in the deltoid and triceps. Brachial neuritis must also be considered in the differential diagnosis. In this case the patient did not have several of the classic antecedent symptoms often associated with brachial neuritis such as cold or flu-like symptoms, history of prior immunization or surgery, or severe pain followed by weakness. This patient did have pain preceding his weakness, though his pain lasted only a few days. Patients with brachial neuritis typically have pain that lasts 1–2 weeks. The pain distribution was atypical for brachial neuritis which usually occurs in the shoulder/neck region. In addition, electrodiagnostic testing in brachial neuritis often reveals denervation in asymptomatic muscles. In this case needle exam revealed evidence of denervation in PIN innervated muscles including the left EIP and left EDC. The abnormal findings found in the left ECRB may represent a known variation in the innervation of the ECRB muscle. This however may be an idiopathic brachial neuritis. The value of MRI is to exclude mass compression of the nerve. MRI may show increased signal consistent with neuritis or the presence of denervation in the affected muscle, which may manifest as signal hyperintensity in the acute phase, and fatty atrophy in the chronic phase.
In summary, PIN entrapment syndrome is rare. The case described here involves PIN entrapment at the level of the supinator in a 22-year-old male doing pull-ups. Although PIN is often caused by trauma or mass lesions, it may also occur spontaneously and is thought to be secondary to the edema of adjacent structures caused by repetitive movements [32]. While idiopathic brachial neuritis cannot be excluded, we felt that this patient’s posterior interosseous neuropathy was more likely related to physical activity and that rest and modification of activities eventually led to recovery. Conservative treatment consisting of activity modification, splinting, physical therapy, anti-inflammatory medication, and/or corticosteroid injections are recommended initially when no identifiable cause is seen on imaging studies. If there is no improvement in 6 months, spontaneous recovery is less likely and surgery is recommended. Typically all five potential sites of compression (the fibrous bands at the proximal edge of the ECRB, the thickened fascial tissue superficial to the radiocapitellar joint between the brachialis and brachioradialis, the Leash of Henry, the arcade of Frohse, and the distal edge of the supinator) are released [7].
Electrodiagnostic testing was used to anatomically localize the level of the nerve injury. This case demonstrates the importance of understanding the anatomical course of a nerve. Once the anatomy is understood, electrodiagnostic testing can be used to accurately identify the location of the lesion.
Disclosures
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of this case, that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Akuthota V, Herring SA. Nerve and vascular injuries in sports medicine. New York: Springer; 2009. pp. 79–81. [Google Scholar]
- 2.Bayramoglu M. Entrapment neuropathies of the upper extremity. Neuroanatomy. 2004;3:18–24. [Google Scholar]
- 3.Braddom, RL. Physical medicine and rehabilitation. Elsevier Science, Saunders, 3rd Edition, Philadelphia. 2007: 211–212.
- 4.Brown, WF, Bolton CF, Aminoff MJ. Neuromuscular function and Disease. Basic, clinical, and electrodiagnostic aspects. Volume 1. Elsevier Science, Saunders, Philadelphia. 2002: 924–926.
- 5.Cho CH, Lee KJ, Min BW. Tardy posterior interosseous nerve palsy resulting from residual dislocation of the radial head in a Monteggia fracture: a case report. Journal of Medical Case Reports. 2009;3:9300. doi: 10.1186/1752-1947-3-9300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho TK, Kim JM, Bak KH, Kim CH. Posterior interosseous nerve (PIN) syndrome caused by anomalous vascular leash. J Korean Neurosurgery. 2005;37:293–295. [Google Scholar]
- 7.Dang AC, Rodner CM. Unusual compression neuropathies of the forearm, part II: median nerve. J Hand Surg. 2009;34A:1915–1920. doi: 10.1016/j.jhsa.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 8.Dhall U, Kanta S. Variations in the nerve supply to extensor carpi radialis brevis. J Ant Soc India. 2001;50(2):134–136. [Google Scholar]
- 9.Dickerman RD, Stevens QEJ, Cohen AJ, Jaikumar S. Radial tunnel syndrome in an elite power athlete: a case of direct compressive neuropathy. Journal of the Peripheral Nervous System. 2002;4:229–232. doi: 10.1046/j.1529-8027.2002.02030.x. [DOI] [PubMed] [Google Scholar]
- 10.Hazani R, Engineer NJ, Mowlavi A, Neumeister M, Lee A, Wilhelmi BJ. Anatomic landmarks for the radial tunnel. Eplasty. 2004;8:377–382. [PMC free article] [PubMed] [Google Scholar]
- 11.Kirichi Y, Irmak MK. Investigation of two possible compression sites of the deep branch of the radial nerve and the nerve supply of the extensor carpi radialis brevis muscle. Neurol Med Chir (Tokyo) 2004;44:14–19. doi: 10.2176/nmc.44.14. [DOI] [PubMed] [Google Scholar]
- 12.Kromberg AJ, Pestronk A. Chronic motor neuropathies: diagnosis, therapy, and pathogenesis. Annals of Neurology. 1995;37(1):43–50. doi: 10.1002/ana.410370706. [DOI] [PubMed] [Google Scholar]
- 13.Latinovic R, Gulliford MC, Hughes RAC. Incidence of common compressive neuropathies in primary care. J Neurol Neurosurg Psychiatry. 2006;77:263–265. doi: 10.1136/jnnp.2005.066696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loh YC, Lam WL, Stanley JK, Soames RW. A new clinical test for radial tunnel syndrome: the rule of nine test: a cadaveric study. J Orthop Surg (Hong Kong) 2004;12(1):83–86. doi: 10.1177/230949900401200115. [DOI] [PubMed] [Google Scholar]
- 15.McCarty EC, Tsairis P, Warten RF. Brachial neuritis. Clinical Orthopedics and Related Research. 1999;368:37–42. doi: 10.1097/00003086-199911000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Miclan A, Ozge A, Sahin G, Saracoglu M, Kuyurtar F. The role of electrophysiologic tests in the early diagnosis of posterior interosseous neuropathy in patients thought to have lateral epicondylitis. Acta Orthop Traumatol Turc. 2004;38(5):326–329. [PubMed] [Google Scholar]
- 17.Molina AEP, Bout C, Oberline C, Nzeusseu A, Vanwijk R. The posterior interosseous nerve and the radial tunnel syndrome: an anatomical study. International Orthopaedics. 1998;22:102–106. doi: 10.1007/s002640050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Monteiro E, Moura A, Barros F, Carvalho P. Lipoma causing a posterior interosseous nerve syndrome. European Journal Plastic Surgery. 2002;25:35–37. doi: 10.1007/s00238-001-0335-7. [DOI] [Google Scholar]
- 19.Mulholland RC. Non-traumatic progressive paralysis of the posterior interosseous nerve. Journal of Bone and Joint Surgery. 1966;48B(4):781–785. [PubMed] [Google Scholar]
- 20.Planchier KD, Peterson RK, Steichen JB. Compressive neuropathies and tendinopathies in the athletic elbow and wrist. Clin Sports Med. 1996;15(2):331–71. [PubMed] [Google Scholar]
- 21.Prasartritha T, Prasert L, Rohanakit A. A study of the posterior interosseous nerve (PIN) and the radial tunnel in 30 Thai cadavers. The Journal of Hand Surgery. 1993;18A:107–12. doi: 10.1016/0363-5023(93)90253-Y. [DOI] [PubMed] [Google Scholar]
- 22.Ragoonwansi R, Kirkpatrick NW, Moss ALH. Posterior interosseous nerve palsy after intravenous cannulation of the forearm. Journal of the Royal Society of Medicine. 1999;92:411. doi: 10.1177/014107689909200810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. Journal of Bone and Joint Surgery. 1972;54B(3):499–508. [PubMed] [Google Scholar]
- 24.Rosenbaum R. Disputed radial tunnel syndrome. Muscle and Nerve. 1999;22:960–967. doi: 10.1002/(SICI)1097-4598(199907)22:7<960::AID-MUS26>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 25.Russel SM. Examination of peripheral nerve injuries: an anatomical approach. New York: Thieme Medical Publishers; 2006. pp. 62–64. [Google Scholar]
- 26.Siegel IM. Dorsal interrosseous nerve compression syndrome from the use of a Canadian crutch. Muscle Nerve. 1988;11(12):1273–1274. [PubMed] [Google Scholar]
- 27.Spinner M. The arcade of Frohse and its relationship to posterior interosseous nerve paralysis. The Journal of Bone and Joint Surgery. 1968;50B:809–812. [PubMed] [Google Scholar]
- 28.Sunderamoorthy D, Chaudhury M. An uncommon peripheral nerve injury after penetrating injury to the forearm: the importance of clinical examination. Emerg Med Journal. 2003;20:565–566. doi: 10.1136/emj.20.6.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Werner CO, Haeffner F, Rosen I. Direct recording of local pressure in the radial tunnel during passive stretch and active contraction of the supinator muscle. Archives of Orthopaedic and Traumatic Surgery. 1980;96:299–301. doi: 10.1007/BF00432870. [DOI] [PubMed] [Google Scholar]
- 30.Werner CO. Paralysis of the posterior interosseous nerve caused by tumour: brief report. The Journal of Bone and Joint Surgery. 1987;69 B(4):670–671. doi: 10.1302/0301-620X.69B4.3038920. [DOI] [PubMed] [Google Scholar]
- 31.White SH, Goodfellow JW, Mowat A. Posterior interosseous nerve palsy in rheumatoid arthritis. J Bone Joint Surg Br. 1988;70B(3):468–471. doi: 10.1302/0301-620X.70B3.3372573. [DOI] [PubMed] [Google Scholar]
- 32.Vreiling C, Robinson PH, Geertzen JHB. Posterior interosseous nerve syndrome: literature review and report of 14 cases. Eur J Plast Surg. 1998;21:196–202. doi: 10.1007/s002380050068. [DOI] [Google Scholar]