Abstract
Posterior cruciate ligament (PCL) reconstructions are challenging surgeries. Recent advances have included double-bundle PCL, arthroscopic inlay, and all-inside techniques. This technical note presents an anatomic, single-bundle, all-inside PCL reconstruction with an anterior tibialis allograft GraftLink construct. The surgery was performed with FlipCutter guide pins and ACL TightRope RT. The case involved a 22-year-old woman with an isolated grade 3 PCL tear that had failed nonoperative treatment. The technique described is minimally invasive.
Posterior cruciate ligament (PCL) reconstructions are challenging surgeries. Recent advances have included double-bundle PCL, arthroscopic inlay, and all-inside techniques.1-4 Clinical results with single- and double-bundle reconstructions have been similar despite biomechanical studies reporting improved stability with double-bundle reconstructions. One study has shown better clinical results with an arthroscopic double-bundle tibial inlay construct.3
The development of the GraftLink (Arthrex, Naples, FL) for second-generation anterior cruciate ligament (ACL) reconstruction has allowed an anatomic, single-bundle, all-inside technique that is showing excellent early results with good cosmesis and decreased pain.5 These advances are possible because of the next-generation instrumentation, including the FlipCutter and TightRope RT. This study describes the first use of a GraftLink construct for an anatomic, single-bundle, all-inside technique for a PCL reconstruction with similar use of next-generation instrumentation.
Case
A 22-year-old woman injured her right knee in a motor vehicle accident. She was a belted driver who collided with a tree after avoiding a deer, and the airbags deployed. The patient hit her knee on the dashboard. She was initially evaluated at a Level I Trauma Center, and head, chest, and abdominal injuries were ruled out. She had right knee and shin pain. Twelve days after her injury, she was evaluated by my orthopaedic partner, and radiographs yielded negative results. Physical examination showed positive posterior drawer and quadriceps active tests. Magnetic resonance imaging was performed, which showed an isolated midsubstance PCL tear, moderate effusion, and an anterolateral tibial bone bruise. Because the patient had an isolated PCL tear, she was treated initially nonoperatively, and a course of physical therapy was initiated. She went to physical therapy for 9 weeks and performed her home exercise program routinely. She was counseled that she was at increased risk of patellofemoral and medial compartment osteoarthritis. She wore a knee brace and used nonsteroidal anti-inflammatory drugs. Seven months after surgery, she began noting instability and discomfort over the medial and lateral aspects of her knee. She was referred 26 months after her injury. She noted instability with activities of daily living; pain over the medial, lateral, patellar, and popliteal aspects of the knee; and swelling. Prolonged walking, standing, and stair climbing were difficult. Her knee examination showed a small effusion, 3+ posterior drawer, 2+ posterior sag, and a positive active quadriceps test. She had a 2+ Lachman test with a firm endpoint, negative pivot shift, and no evidence of medial or posterolateral laxity. She had mild quadriceps weakness and full range of motion. Repeat radiographs showed normal results, and magnetic resonance imaging was not repeated. She was diagnosed with an isolated PCL tear that had failed optimal nonoperative treatment, and a PCL reconstruction was recommended.
Surgical Technique
The reconstruction technique is shown in Video 1. A GraftLink construct was prepared with an anterior tibialis allograft from LifeNet treated with Allowash (LifeNet Health and Allowash XG, Virginia Beach, VA). The anterior tibialis had a doubled diameter of 8.5 mm and was 290 mm long. The graft was tripled, and the posts of the graft preparation board were set at 80 mm. The graft was prepared as outlined by Lubowitz et al.5 The graft was tensioned and had a length of 90 mm. The normal intra-articular distance of the PCL is 30 to 38 mm.6,7 The planned interosseous distance in the femur was 25 mm, and the planned interosseous distance in the tibia was 40 mm (Fig 1). Therefore the graft would not bottom out in the sockets. The graft diameter was 10 mm with the tripled graft. This graft diameter is similar to that of other described PCL reconstruction techniques.1,3,4,8
Fig 1.

GraftLink construct of anterior tibialis allograft tripled, 10 mm in diameter. The graft length was 90 mm. The tibial end of the graft with the insertion depth of 40 mm is shown on the left; the intra-articular portion of the graft measured 30 mm; and the femoral end of the graft, shown on the right, was marked at 20 mm. The graft was tensioned at 15 lb for 20 minutes.
An examination of the knee with the patient under anesthesia was performed. She was stable to varus and valgus in full extension and 30° of flexion. She had a 2+ Lachman with a firm endpoint and a negative pivot-shift test. The posterior sag was 2+, and posterior drawer was 3+. A negative dial test at 30° and 90° was noted. There was slightly more laxity with posterolateral compared with posteromedial drawer tests, and she had full range of motion. A well-padded tourniquet was placed, and an Acufex thigh holder (Smith & Nephew Endoscopy, Andover, MA) was used.
Standard anteromedial (AM), anterolateral, and posteromedial arthroscopic portals were created. An arthroscopic evaluation was performed, and there were some early chondral changes in the medial and patellofemoral compartments. The menisci were intact. There was no evidence of medial or lateral laxity. The PCL was absent in its midsubstance, and there was an empty medial wall sign. The ACL had significant sag. The PCL remnants were excised with a motorized shaver and radiofrequency device, with care taken to maintain the femoral and tibial footprints. An 8.25 × 7-cm cannula (Arthrex) was used in the posteromedial portal, and the PCL fossa was cleared so that the PCL insertion could be well visualized; 30° and 70° arthroscopes were used throughout the case.
A C-arm was used at the beginning of the case to ensure that a good lateral view of the knee could be obtained. The knee was placed in 90° of flexion. The Arthrex Anatomic Contour PCL guide was placed in the PCL sulcus in the center of the PCL footprint (Fig 2). A 10.5-mm FlipCutter was advanced to the posterior aspect of the tibia with arthroscopic and fluoroscopic visualization (Fig 3). The 10.5-mm FlipCutter was used in retrograde fashion to make a socket. The guide pin sleeve had been tapped into the tibia to maintain a 7-mm bone bridge. The tibial tunnel length was 45 mm with a 7-mm bone bridge. The FlipCutter was then removed, and an Arthrex TigerStick was passed through the guide pin sleeve, grasped with a suture grasper, and pulled out through the AM arthroscopic portal.
Fig 2.
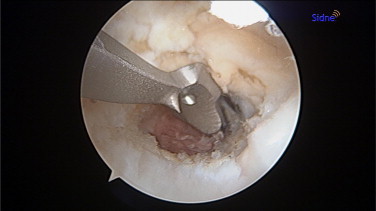
Arthroscopic view of right knee with 70° arthroscope, with Anatomic Contour PCL guide in center of PCL tibial footprint.
Fig 3.

Fluoroscopic view of right knee with 10.5-mm FlipCutter creating tibial socket. The Anatomic Contour PCL guide protects the popliteal neurovascular structures.
The 10.5-mm FlipCutter was used from the more distal aspect of the medial femoral condyle externally to make an outside-in angle for the socket. The FlipCutter aimer was then referenced 8 mm from the edge of the articular surface in the middle of the PCL footprint, leaving a 2-mm bone bridge from the anterior articular surface of the medial femoral condyle (Fig 4). The guide pin sleeve was tapped 7 mm into the femur. The femoral tunnel length was 22 mm, leaving a 7-mm bone bridge. The posterior aspect of the socket was chamfered with a rasp, and a shaver and radiofrequency device cleared the socket of debris (Fig 5). A FiberStick was passed into the socket and retrieved through the AM portal.
Fig 4.
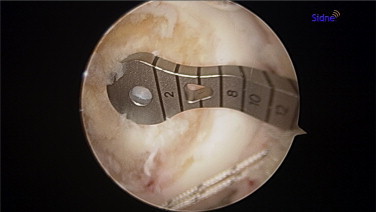
Arthroscopic view of medial femoral condyle in right knee with 30° arthroscope. The PCL guide for the FlipCutter is in the middle of the PCL femoral footprint.
Fig 5.

Arthroscopic view of medial femoral condyle in right knee with 30° arthroscope. A rasp was used to chamfer the proximal aspect of the femoral tunnel.
The femoral and tibial ends of the graft were marked with the desired depth of insertion, 20 and 40 mm, respectively. The tibial end of the graft with the TightRope RT was first advanced into the AM portal with the TigerStick from the tibial tunnel; then the button was flipped on the anterior tibial cortex and the graft partially seated. The femoral portion of the graft was then passed into the femoral socket with the FiberStick, advanced 22 mm to the depth of the socket, and the button was flipped. The femoral portion of the graft was fully tensioned. Because the anterolateral bundle of the PCL was being reconstructed, the knee was flexed 90° with an anterior drawer force, and the tibial end of the graft was fully tensioned (Fig 6). This negated the previously noted sag in the ACL, and the posterior drawer was negative. The knee had full range of motion, and excellent tension was maintained on both the PCL and ACL to both visualization and probing. The fluoroscopic views showed satisfactory positioning of the TightRope RT titanium buttons (Fig 7).
Fig 6.
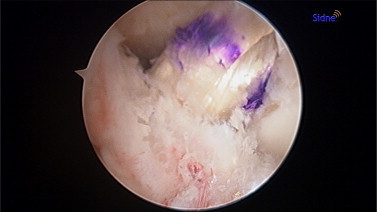
An arthroscopic view of the right knee with a 30° arthroscope shows the anterior tibialis allograft GraftLink construct. The ACL posterior sag noted before the reconstruction has resolved.
Fig 7.
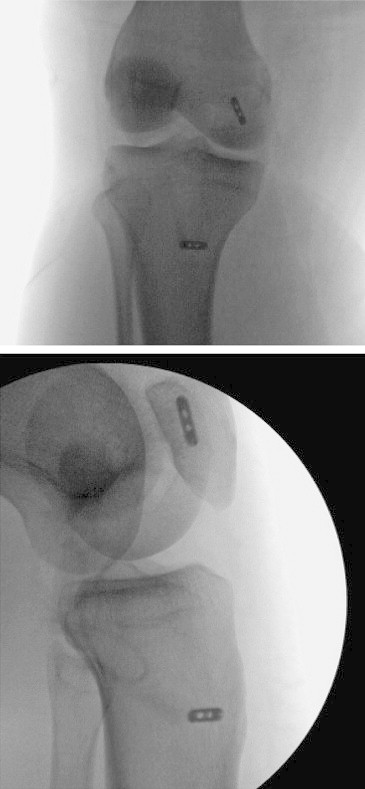
Fluoroscopic anteroposterior and lateral views of right knee with TightRope RTs securing PCL GraftLink construct.
Good cosmesis was achieved by use of 2 anterior and posteromedial portals. There were 1-cm incisions on the medial femoral condyle and the proximal-medial tibia for the creation of the femoral and tibial tunnels, respectively, for the FlipCutter and guide pin sleeves.
A standard PCL rehabilitation protocol was used, with a brace locked in extension for 1 week and then gradual mobilization. The patient had a femoral nerve catheter for the first 3 days after surgery and took narcotics for the first 2 weeks after surgery. She reports marked improvement in stability compared with preoperatively. Table 1 shows key points of the described technique.
Table 1.
Key Points
| Technique/Device | Advantage |
|---|---|
| GraftLink construct | Control graft length and diameter |
| Easy to insert compared with grafts with bone | |
| FlipCutter | Creates retrograde sockets, safer for tibia |
| Socket with consistent 7-mm bone bridge | |
| Available in multiple diameters | |
| Tibial socket | FlipCutter advanced away from popliteal neurovascular structures |
| Femoral socket | Outside-in technique decreases critical corner |
| TightRope RT | Infinite tensioning of femoral and tibial ends of graft |
Discussion
This article describes, for the first time, a PCL reconstruction that uses a GraftLink soft-tissue graft. The graft in this case was 10 mm, and the size could be larger with the use of larger-diameter soft-tissue grafts. The soft-tissue graft passed easily from the AM portal into both the tibial and femoral tunnels. The bone plug of an arthroscopic tibial inlay construct can be challenging to pass and fully seat and requires enlargement of the AM portal.
The use of the FlipCutter improves the safety of creating the tibial tunnel by drilling away from the popliteal neurovascular structures. The Arthrex Anatomic Contour PCL guide acts as a guide for the FlipCutter, and its width and shape prevent advancement of the FlipCutter too far posteriorly. Fluoroscopic guidance to correctly place the Anatomic Contour PCL guide is recommended, and this provides additional safety while one is advancing the FlipCutter. The use of the guide pin sleeve with the FlipCutter creates a consistent 7-mm bone bridge from the anterior tibial cortex and facilitates advancement of the passing suture. The long tibial tunnel helps avoid bottoming out of the graft, which was 45 mm in this case. The guide pin sleeve allows a 7-mm bone bridge for the femoral socket as well.
The FlipCutter enhances the creation of the femoral socket. Inside-out femoral tunnels and sockets create a “critical corner” for the femoral portion of the graft.6 The PCL aiming guide allows the creation of an anatomic socket within the femoral footprint. The outside aiming arm of the FlipCutter can be used in an outside-in fashion, decreasing the acute angle of the graft.
The TightRope RTs allowed easy graft passage and socket insertion. Moreover, they allowed infinite tensioning of the 2 ends of the graft in any degree of flexion. The normal tibial anterior step-off was created, and the posterior sag and drawer were negated. The TightRope RTs could be easily revised if graft failure occurred, and they would not interfere with future surgeries. The minimally invasive nature of the surgery yields excellent cosmesis and decreased pain. The patient was routinely discharged as an outpatient.
The described technique risks bottoming out of the graft if the graft is too long. Because the patient was short, I used a PCL intra-articular length of 30 mm. Because the femoral interosseous distance was 22 mm and the tibial interosseous distance was 45 mm, the 90-mm graft link did not bottom out, and excellent graft tension was achieved. In summary, the technique is an anatomic, single-bundle, all-inside PCL reconstruction that uses a graft-link construct, with second-generation FlipCutter guide pins and TightRope RT graft tensioning and fixation devices.
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
PCL reconstruction with anterior tibialis allograft graft-link construct using an all-inside technique. The femoral and tibial sockets were created with Arthrex FlipCutters. The femoral and tibial ends of the graft were fixed with Arthrex TightRope RT anchors that allowed infinite tensioning of the graft.
References
- 1.Bovid K.M., Salata M.J., Vander Have K.L., Sekiya J.K. Arthroscopic posterior cruciate ligament reconstruction in a skeletally immature patient: A new technique with case report. Arthroscopy. 2010;26:563–570. doi: 10.1016/j.arthro.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 2.Boyd J, ed. All-inside PCL reconstruction surgical technique. Arthrex Surgical Techniques. Naples, FL: Arthrex, Inc.; 2012.
- 3.Kim S.J., Kim T.E., Jo S.B., Kung Y.P. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am. 2009;91:2543–2549. doi: 10.2106/JBJS.H.01819. [DOI] [PubMed] [Google Scholar]
- 4.Campbell R.B., Jordan S.S., Sekiya J.K. Arthroscopic tibial inlay for posterior cruciate ligament reconstruction. Arthroscopy. 2007;23:1356.e1–1356.e4. doi: 10.1016/j.arthro.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 5.Lubowitz J.H., Amhad C.H., Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Matava M.J., Ellis E., Gruber B. Surgical treatment of posterior cruciate ligament tears: An evolving technique. J Am Acad Orthop Surg. 2009;17:435–446. doi: 10.5435/00124635-200907000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Voos J.E., Mauro C.S., Wente T., Warren R.F., Wickiewicz T.L. Posterior cruciate ligament: Anatomy, biomechanics, and outcomes. Am J Sports Med. 2012;40:222–231. doi: 10.1177/0363546511416316. [DOI] [PubMed] [Google Scholar]
- 8.Thiele R.A., Campbell R.B., Amendola A., Sekiya J.K. Biomechanical comparison of figure-of-8 versus cylindrical tibial inlay constructs for arthroscopic posterior cruciate ligament reconstruction. Arthroscopy. 2010;26:977–983. doi: 10.1016/j.arthro.2009.11.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PCL reconstruction with anterior tibialis allograft graft-link construct using an all-inside technique. The femoral and tibial sockets were created with Arthrex FlipCutters. The femoral and tibial ends of the graft were fixed with Arthrex TightRope RT anchors that allowed infinite tensioning of the graft.


