Abstract
There is growing evidence that anatomic placement of the femoral tunnel in anterior cruciate ligament reconstruction confers biomechanical advantages over the traditional tunnel position. The anteromedial portal technique for anatomic anterior cruciate ligament reconstruction has many well-described technical challenges. This article describes the translateral all-inside technique, which produces anatomic femoral tunnel placement using direct measurement of the medial wall of the lateral femoral condyle and outside-in drilling. All work is carried out through the lateral portal with all viewing through the medial portal. Thus there is no need for an accessory medial portal or hyperflexion of the knee during femoral socket preparation. A single quadrupled hamstring graft is used with cortical fixation at both the femoral and tibial tunnels.
Transtibial drilling remains the most popular method for creating the femoral tunnel in anterior cruciate ligament (ACL) reconstruction. With this technique, femoral socket placement is dictated by the tibial tunnel, which invariably results in a relatively vertical position of the graft. Although this technique has had good early clinical outcomes, the procedure has been shown to be nonanatomic.1,2 This fails to restore normal knee kinematics,3,4 which in turn may lead to early-onset osteoarthritis.5
An alternative technique for femoral tunnel preparation is anteromedial (AM) portal drilling, in which independent drilling of the femoral and tibial tunnels is performed.6 This approach requires an exact appreciation of the intra-articular bony anatomy, particularly on the medial face of the lateral femoral condyle, to define tunnel placement. This can be difficult to establish using traditional lateral portal arthroscopic viewing, where the femoral intercondylar and bifurcate ridges are not readily identified. Furthermore, use of the clock-face reference can lead to a high or anterior placement of the graft.7
Recently, the concept of “anatomic” or “footprint” ACL reconstruction has been introduced. This has been shown to confer a biomechanical advantage over nonanatomic reconstruction.3 In its current form, anatomic femoral preparation makes use of an accessory medial portal,8-10 which allows simultaneous medial viewing and preparation of the femoral tunnel. Although this improves visualization of and access to the femoral tunnel entry position, it can be technically challenging because of problems such as instrument crowding and hyperflexion.11,12 The translateral technique, first published by us in July 2012,13 simplifies the process, with all work being carried out with the knee flexed to 90° and with no requirement for an accessory medial portal. This technical note describes the translateral all-inside technique. This has all the advantages of the original technique while also preserving the gracilis tendon as a secondary stabilizer or for use as a further graft in multiligament surgery (Table 1).
Table 1.
Indications, Contraindications, Tips, Pearls, Pitfalls, Key Points, and Limitations of Translateral All-Inside Technique for ACL Reconstruction
| Indications |
| ACL deficiency requiring reconstruction, especially when performed as part of multiligament reconstruction. |
| Contraindications |
| Contraindications for any surgical technique for ACL reconstruction. |
| Advantages |
| Directly measured anatomic placement of femoral tunnel without pitfalls of creating accessory medial portal. |
| Single semitendinosus hamstring harvest. |
| Gracilis preserved as secondary stabilizer or for use as further graft. |
| Cortical fixation at both tibial and femoral sites. |
| Tips and pearls |
| The lateral portal should be placed as close to the patellar tendon as possible to allow easy passage of the translateral instruments. |
| The femoral anatomic midbundle point is halfway along a line from the deep articular margin to the shallow articular margin. This corresponds to the bifurcate ridge. |
| The height of the center of the femoral tunnel is 2 mm plus the radius of the femoral tunnel above the low articular margin. |
| The femoral jig is set at 110°. |
| The tibial jig is set at 70°. |
| The femoral socket is drilled to a depth of 20 mm. |
| The graft is marked 20 mm from the femoral end. When this mark passes beyond the mouth of the socket, the button will have been pulled free of the lateral femoral cortex. |
| Pitfalls and risks |
| It is important to identify and harvest only the semitendinosus. The technique can be performed with a quadrupled gracilis tendon, but graft size is less reliable. |
| In cases of inadequate graft size, a quadrupled semitendinosus and gracilis tendon can be used. This is termed a mega-GraftLink. |
| When one is retrieving the suture loops through the AM portal, they may become looped, making graft passage impossible. To avoid this, one should withdraw 1 end of each of the loops and form a snare at the end of the suture so that they cannot become intertwined. |
| Key points |
| RF ablation of the medial wall of the lateral femoral condyle is vital to preserve the bony landmarks. |
| During femoral preparation, all work is carried out through the lateral portal. All viewing is through the medial portal. |
| The knee is flexed to 90° throughout. |
| Limitations |
| Graft preparation can be more time-consuming than traditional whipstitching. |
Technique
The translateral technique requires special instruments. These instruments have been designed by the senior author to navigate around the distal aspect of the lateral femoral condyle while avoiding impingement on the patellar tendon medially. They include a specially shaped Opes radiofrequency (RF) probe (Arthrex, Naples, FL) for soft-tissue debridement, a modified curette, a curved dual-function marking and measuring device (Fig 1), and an anatomic aiming arm for a retrograde drill. These specific translateral tools are manufactured by Arthrex. The author uses the FlipCutter (Arthrex) to create a “retrosocket” by outside-in drilling, as has been described by other authors, including Lubowitz et al.14
Fig 1.
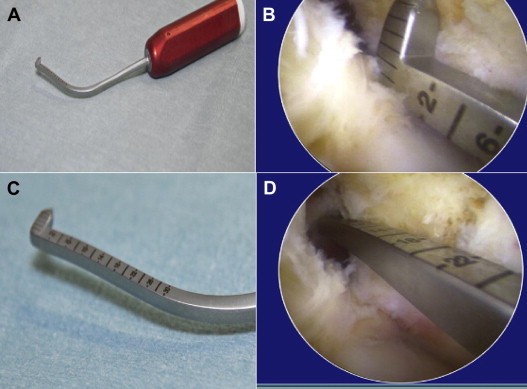
(A) Curved marking/measuring device. This instrument allows direct measurement of the medial wall of the lateral femoral condyle and anatomic positioning of the femoral tunnel. (B) Measuring from low position: the view is of the medial wall of the lateral femoral condyle of the left knee from the AM portal with the knee at 90° of flexion. The height of the center of the femoral tunnel is 2 mm plus the radius of the tunnel above the low articular margin. (C) Close-up of measuring arm. (D) Measuring deep to shallow or front to back of notch. The anatomic or midbundle position is halfway from the deep to the shallow articular cartilage. Again, the view is from the AM portal at 90° of flexion.
The patient is positioned supine with the knee flexed to 90°. A side support and footrest are used. A thigh tourniquet is used throughout. A modified anterolateral (AL) portal (Fig 2) is used, which is positioned slightly lower and more medial than the traditional high AL portal position. A 30° side-viewing arthroscope is inserted through the modified AL portal. A standard AM portal is then made under direct vision. Routine arthroscopic assessment is undertaken and appropriate surgery carried out to address any chondral or meniscal pathology.
Fig 2.
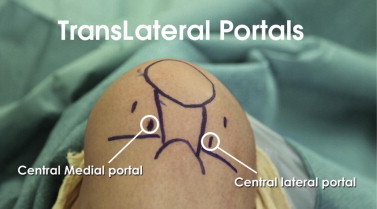
Translateral portal positions. This shows the left knee at 90° of flexion with traditional and translateral portals. The translateral portals are noticeably lower and more central than the traditional portals.
A single semitendinosus tendon is harvested through a curved incision over the pes anserinus. The tendon is loaded onto 2 adjustable suspensory devices (ACL TightRope RT; Arthrex) and quadrupled to make a GraftLink (Arthrex) (Fig 3).15 In the first-generation translateral technique, both the semitendinosus and gracilis tendons were harvested. The tendons were doubled to create a traditional 4-strand graft and secured to a single TightRope at the femoral end. The arthroscope is then swapped to the AM portal for the remainder of femoral preparation. The knee remains flexed to 90° with no hyperflexion required throughout the procedure.
Fig 3.

Quadrupled semitendinosus tendon with 2 ACL TightRopes, forming a modified GraftLink construct. A single semitendinosus tendon is harvested through a curved incision over the pes anserinus. The tendon is loaded onto 2 adjustable suspensory TightRope RT devices and quadrupled to form the modified GraftLink construct.
The medial wall of the lateral femoral condyle is prepared with the curved RF probe. The use of RF is essential to allow soft-tissue debridement while preserving the footprint of the native ACL and facilitating identification of the bony anatomic landmarks, namely the bifurcate and intercondylar ridges.
The curved marking device (Fig 1) is then inserted through the lateral portal to determine and mark the center of the ACL footprint. Figure 4 shows the anatomic footprint with the relevant measurements annotated. Two measurements are made; the first is made by use of the long axis of the measuring tool that measures from deep to shallow with the center of the ACL footprint at the midpoint,16 which corresponds to the bifurcate ridge. A second measurement is then made using the calibrated tip that determines the height of the center of the footprint from the low position. The measuring/marking device has a sharp tip, which allows the surgeon to mark the correct femoral tunnel position. Figure 5 shows the arthroscopic view during direct measurement of the medial wall of the lateral femoral condyle. A calibrated RF device, the Arthrex Caliblator, has recently been developed to permit simultaneous soft-tissue clearance and marking, significantly facilitating this process (Fig 6).
Fig 4.
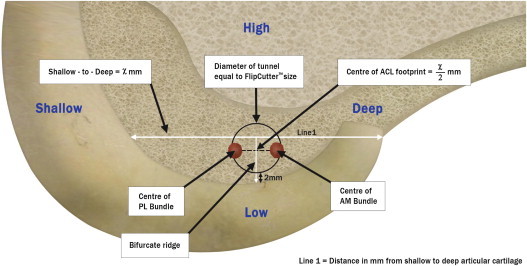
Medial aspect of lateral femoral condyle. The anatomic footprint of the native ACL is shown, as are the graft tunnel and measurements. The position of the femoral tunnel is in the anatomic midbundle position. Reprinted with permission.13 (PL, posterolateral.)
Fig 5.
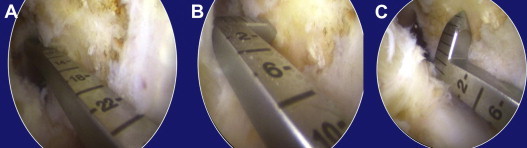
Arthroscopic view of direct measurement of medial aspect of lateral femoral condyle with marking/measuring tool. All the arthroscopic images are of a left knee in 90° of flexion through the AM portal. (A) Measuring deep to shallow. (B) Measuring shallow articular cartilage to center of femoral footprint. This point lies halfway between the deep and shallow articular cartilage. (C) Measuring from low articular cartilage along line of bifurcate ridge. The height of the center of the femoral tunnel is 2 mm plus the radius of the femoral tunnel above the low articular cartilage.
Fig 6.
Caliblator curved RF device. (A) Measuring deep to shallow. (B) Measuring shallow articular cartilage to center of femoral footprint, which lies halfway between deep and shallow articular cartilage. (C) Measuring from low articular cartilage along line of bifurcate ridge. The height of the center of the femoral tunnel is 2 mm plus the radius of the femoral tunnel above the low articular cartilage.
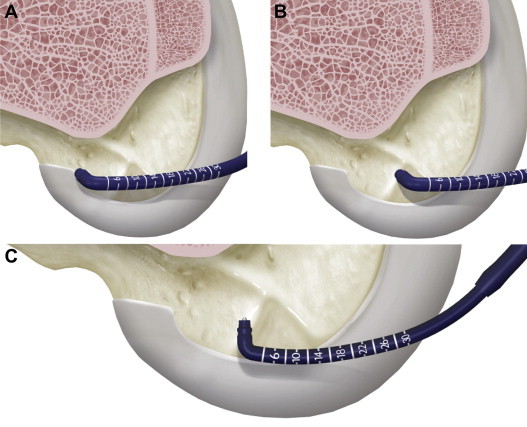
The femoral and tibial tunnels are created by the retrosocket approach: the FlipCutter aiming device is inserted through the modified AL portal and positioned at the premarked anatomic femoral origin (Fig 7). With the knee flexed to 90°, a 3.5-mm femoral pilot hole is then created with the FlipCutter by an outside-in drilling technique. The end of the FlipCutter is deployed and drilled in a retrograde manner to produce a femoral retrosocket. We routinely drill this socket to a depth of 20 mm. A FiberStick (Arthrex), a stiffened plastic tube containing a high–tensile strength loop of suture, is then passed through the femoral tunnel, and the contained FiberWire is retrieved from the knee joint. The tibial retrosocket is created by the same technique, with the tibial aiming jig placed in the midbundle position. We routinely drill this socket to a depth of 35 mm using the FlipCutter. A TigerStick (Arthrex), a stiffened plastic tube containing a looped, striped high–tensile strength suture, is passed through the tibial tunnel, and the contained TigerWire is retrieved with the femoral FiberWire simultaneously through the AM portal to ensure that there is no soft-tissue bridge. As an additional measure to prevent snagging or entwining of the looped sutures, 1 end of each suture is pulled out of the AM portal to create a single strand. Pull-through loops are then fashioned at the end of each suture for the TightRope buttons, which are then pulled into their respective sockets. First, the femoral TightRope RT is pulled through to “bottom out,” or fully seat, the graft within the femoral socket. By doing this we avoid inadvertently pulling too much of the graft link into the femoral socket. We then turn our attention to the tibial socket, and the Tibial TightRope RT is passed through the tibial tunnel. The GraftLink is pulled into the tibial retrosocket, and final tensioning is achieved in full extension by reciprocal toggling of the 2 suture ends to snug the graft home. Cortical suspensory fixation is thus achieved at both ends of the graft. The knee is cycled, and if necessary, the TightRopes can be retensioned before finally removing excess suture (Video 1). This all-inside approach is a modification of our original translateral technique. In the first-generation technique, a traditional tibial tunnel was drilled and tibial fixation was achieved with an interference screw.
Fig 7.

Arthroscopic images of femoral tunnel preparation. Images show a left knee at 90° of flexion through the AM portal. (A) Aiming jig in position at anatomic midbundle point. This can be confirmed by the calibrations on the jig arm. (B) View of femoral tunnel. (C) Confirming tunnel position with measuring tool.
Discussion
There are many advantages to the translateral all-inside technique. The instruments allow all femoral preparation to be carried out through a single modified AL portal with the knee at 90° of flexion. This includes soft-tissue debridement and identification and marking of the center of the ACL footprint, together with creation of the femoral retrosocket.
Bird et al.17 previously described the ruler technique with the midbundle position being located halfway along a line measured on the lateral intercondylar wall from the deep articular cartilage margin to the most shallow position. Anatomic placement of the femoral tunnel is achieved while avoiding the pitfalls of the AM portal technique identified by Lubowitz.12 The most notable of these is the need for hyperflexion, which can lead to disorientation, a short femoral tunnel, malpositioning of the femoral aiming jig, “portal tightening,” iatrogenic damage to the articular cartilage of the medial femoral condyle, and increased fat pad ingression.12 In our practice, anatomic femoral socket placement using the accessory medial portal has been complicated by instrument crowding. We have shown that, with the use of specifically designed instrumentation, the translateral technique provides a facile approach to anatomic ACL reconstruction, dispensing with the requirement for an accessory medial portal or hyperflexion of the knee during femoral socket preparation.
The all-inside modification of the translateral technique requires only isolated harvesting of the semitendinosus tendon, which has previously been shown to preserve postoperative hamstring strength,16 and allows the remaining hamstring to function as a secondary stabilizer or to be used as a graft for further ligament reconstructions. The use of bicortical suspensory fixation of the graft has also been shown to withstand higher force to failure over conventional interference fixation devices (data on file at Arthrex).
The quadrupled semitendinosus graft has consistently provided a good graft diameter in our series, 8.6 mm mean. However, inadvertent harvesting of the gracilis can occur. In this event, a quadrupled gracilis can be used if this graft is of a suitable diameter. In cases in which the graft is of insufficient girth, a quadrupled semitendinosus and gracilis composite graft can be used to form a “mega-GraftLink.” GraftLink preparation can be more time-consuming and technically challenging than traditional whipstitching. A competent assistant is required. Despite these caveats, this new technique has significant advantages with specifically designed instrumentation that permits a facile approach, namely, all work is carried out through the lateral portal with all viewing through the medial portal and a single quadrupled hamstring graft can be readily used with cortical fixation at both the femoral and tibial tunnels.
Footnotes
The authors report the following potential conflict of interest or source of funding in relation to this article: Arthrex, Naples, FL.
Supplementary Data
Step-by-step demonstration of anatomic all-inside ACL reconstruction using translateral technique.
References
- 1.Kaseta M.K., DeFrate L.E., Charnock B.L., Sullivan R.T., Garrett W.E., Jr. Reconstruction technique affects femoral tunnel placement in ACL reconstruction. Clin Orthop Relat Res. 2008;466:1467–1474. doi: 10.1007/s11999-008-0238-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steiner M.E., Battaglia T.C., Heming J.F., Rand J.D., Festa A., Baria M. Independent drilling outperforms conventional trans-tibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:1912–1919. doi: 10.1177/0363546509340407. [DOI] [PubMed] [Google Scholar]
- 3.Kondo E., Merican A.M., Yasuda K., Amis A.A. Biomechanical comparison of anatomic double bundle, anatomic single bundle and nonanatomic single bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2011;39:279–288. doi: 10.1177/0363546510392350. [DOI] [PubMed] [Google Scholar]
- 4.Nicholson J.A., Sutherland A.G., Smith F.W. Single-bundle anterior cruciate reconstruction does not restore normal knee kinematics at six months: An upright MRI study. J Bone Joint Surg Br. 2011;93:1334–1340. doi: 10.1302/0301-620X.93B10.26481. [DOI] [PubMed] [Google Scholar]
- 5.Maffulli N., Longo U.G., Gougoulias N., Loppini M., Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. 2010;44:21–25. doi: 10.1136/bjsm.2009.069526. [DOI] [PubMed] [Google Scholar]
- 6.Tudisco C., Bisicchia S. Drilling the femoral tunnel during ACL reconstruction: Transtibial versus anteromedial portal techniques. Orthopedics. 2012;35:e1166–e1172. doi: 10.3928/01477447-20120725-14. [DOI] [PubMed] [Google Scholar]
- 7.Fu F.H. The clock face reference: Simple but nonanatomic. Arthroscopy. 2008;24:1433. doi: 10.1016/j.arthro.2008.09.003. (letter) [DOI] [PubMed] [Google Scholar]
- 8.Bedi A., Altchek D.W. The “footprint” anterior cruciate ligament technique: An anatomic approach to anterior cruciate ligament reconstruction. Arthroscopy. 2009;25:1128–1138. doi: 10.1016/j.arthro.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Cohen S.B., Fu F.H. Three-portal technique for anterior cruciate ligament reconstruction: Use of a central medial portal. Arthroscopy. 2007;23:325.e1–325.e5. doi: 10.1016/j.arthro.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 10.Espejo-Baena A., Serrano-Fernandez J.M., de la Torre-Solis F., Irizar-Jiminez S. Anatomic double-bundle ACL reconstruction with femoral cortical bone bridge support using hamstrings. Knee Surg Sports Traumatol Arthrosc. 2009;17:157–161. doi: 10.1007/s00167-008-0642-7. [DOI] [PubMed] [Google Scholar]
- 11.Colvin A.C., Shen W., Musahi V., Fu F.H. Avoiding pitfalls in anatomical ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:1414–1421. doi: 10.1007/s00167-009-0804-2. [DOI] [PubMed] [Google Scholar]
- 12.Lubowitz J.H. Anteromedial portal technique for the anterior cruciate ligament femoral socket: Pitfalls and solutions. Arthroscopy. 2009;25:95–101. doi: 10.1016/j.arthro.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 13.Logan J.S., Elliot R.R., Wilson A.J. TransLateral ACL reconstruction: a technique for anatomic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:1289–1292. doi: 10.1007/s00167-011-1745-0. [DOI] [PubMed] [Google Scholar]
- 14.Lubowitz J.H., Konicek J. Anterior cruciate ligament femoral tunnel length: Cadaveric analysis comparing anteromedial portal versus outside-in technique. Arthroscopy. 2010;26:1357–1362. doi: 10.1016/j.arthro.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 15.Lubowitz J.H., Ahmad C.S., Anderson K. All-inside anterior cruciate ligament graft-link technique: Second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Yosmaoglu H.B., Baltaci G., Ozer H., Atay A. Effects of additional gracilis tendon harvest on muscle torque, motor coordination, and knee laxity in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1287–1292. doi: 10.1007/s00167-011-1412-5. [DOI] [PubMed] [Google Scholar]
- 17.Bird J.H., Carmont M.R., Dhillon M. Validation of a new technique to determine midbundle femoral tunnel position in anterior cruciate ligament reconstruction using 3-dimensional computed tomography analysis. Arthroscopy. 2012;27:1259–1267. doi: 10.1016/j.arthro.2011.03.077. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Step-by-step demonstration of anatomic all-inside ACL reconstruction using translateral technique.


