Abstract
The National Heart, Lung, and Blood Institute developed the Honoring the Gift of Heart Health (HGHH) curriculum to promote cardiovascular knowledge and heart-healthy lifestyles among American Indians and Alaska Natives (AI/ANs). Using data from a small randomized trial designed to reduce diabetes and cardiovascular disease (CVD) risk among overweight/obese AI/ANs, we evaluated the impact of an adapted HGHH curriculum on cardiovascular knowledge. We also assessed whether the curriculum was effective across levels of health literacy (defined as the ‘capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions’). We examined change in knowledge from baseline to 3 months for two groups: HGHH (N = 89) and control (N = 50). Compared with controls, HGHH participants showed significant improvement in heart attack knowledge and marginally significant improvement in stroke and general CVD knowledge. HGHH participants attending ≥1 class showed significantly greater improvement than controls on all three measures. Although HGHH participants with inadequate health literacy had worse heart attack and stroke knowledge at baseline and 3 months than did participants with adequate skills, the degree of improvement in knowledge did not differ by health literacy level. HGHH appears to improve cardiovascular knowledge among AI/ANs across health literacy levels.
Introduction
Although cardiovascular disease (CVD) was once rare among American Indians and Alaska Natives (AI/ANs) [1–6], CVD burden is now greater among Native people than the US all-race population [1, 6–8]. Coronary heart disease and stroke are significantly more prevalent among AI/ANs than the general population [1, 7], with serious cardiovascular problems beginning early in life [9–11].
Risk factors for CVD are common among AI/ANs, who have high rates of hypertension [10, 12, 13], hypercholesterolemia [10, 12, 14] and diabetes [12, 13, 15–17]. Behavioral risk factors also are common, with AI/ANs having a high prevalence of smoking [12, 13, 16–18], overweight/obesity [13, 16, 17] and sedentary lifestyles [13, 16, 17].
Many AI/ANs have restricted cardiovascular knowledge. Compared with the US all-race population, AI/ANs have more limited knowledge of heart attack and stroke symptoms [12, 19]. General knowledge of CVD, however, is relatively strong. For example, most AI/ANs know that being overweight is a risk factor for heart disease and that physical activity can reduce CVD risk [19, 20]. Specific limitations have been noted, however. For example, in a recent study, many AI/AN participants could not correctly identify whether a specific blood pressure value would be considered high [19].
To address CVD burden in Native communities, the National Heart, Lung, and Blood Institute (NHLBI) developed the Honoring the Gift of Heart Health (HGHH) curriculum, which targets cardiovascular health in AI/ANs [21, 22]. Although HGHH is recommended for use in Indian healthcare settings [23], no studies of its effectiveness have been published. This article addresses this gap in the literature.
We examined whether participation in educational sessions adapted from the HGHH curriculum improved cardiovascular knowledge among participants in the Fresh Insights Toward Health (FIT Health) study, a small controlled trial designed to reduce diabetes and CVD risk among overweight/obese AI/ANs. In evaluating knowledge gain, we sought to determine whether participants with lower versus higher health literacy levels benefited equally from HGHH-based education. Health literacy is ‘the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions’ [24]. National data indicate that 36% of US adults and 48% of AI/AN adults have limited health literacy skills [25].
Ample evidence indicates that limited health literacy is associated with poor disease knowledge [26–37]. Most studies examining this relationship have been cross-sectional, however, and thus do not clarify whether limited health literacy serves as a barrier to the acquisition of knowledge. The few studies to examine the relationship of health literacy with knowledge acquisition provide inconsistent results. Although four studies showed that knowledge gain did not depend on health literacy [38–41], two studies indicated that low-literate participants learned less in response to educational intervention than did their higher-literacy counterparts [42, 43]. Given that knowledge mediates the relationship between health literacy and outcomes [44–47], ensuring that interventions are effective across health literacy levels is critical.
Methods
FIT Health study
FIT Health was a pilot project designed to reduce diabetes and CVD risk among overweight/obese AI/ANs. Informed by Social Cognitive Theory [48–50] and Transtheoretical Model [51], the study was designed to enhance self-efficacy and positive outcome expectancies related to heart-healthy behaviors, with the goal of increasing participants’ readiness to change their current lifestyles. Such change was expected to result in improved health behaviors and clinical outcomes.
Participants were assigned to one of three study arms: (i) HGHH-based education, (ii) WiiFit Plus™ and (iii) control. Participants randomized to the second group received WiiFit Plus™ gaming consoles for home use at the time of randomization. Using a wait list control design, participants in the HGHH and control groups received WiiFit consoles following the 3-month visit. This article addresses cardiovascular knowledge among HGHH and control participants.
The study was conducted in 2010–11 at two urban Indian clinics: Denver Indian Health and Family Services (DIHFS) and First Nations Community HealthSource (FNCH) in Albuquerque. Funded by the Indian Health Service (IHS), these clinics provide healthcare services to AI/ANs living in their local areas. The protocol was approved by the Institutional Review Board (IRB) of the University of Colorado Anschutz Medical Campus and the National IHS IRB.
Participants
Recruitment
Participants were recruited through clinic mailings. The clinics limited their mailing lists to AI/ANs within a few years of the eligible age range and who had attended a clinic visit within the past year. Recruitment information also was made available in the clinics and at local powwows.
Study staff conducted telephone screenings to assess eligibility of interested patients. Participants had to be AI/ANs aged 18–64 years, to have a Body Mass Index (BMI) of 25.0–39.9 kg/m2, to be active DIHFS or FNCH clients, and to have a permanent address and phone number, with no plans to move. Exclusion criteria included active cancer, dialysis, uncontrolled hypertension, pregnancy and active alcohol/substance abuse. As the study’s primary aim was to reduce diabetes and CVD risk, patients already diagnosed with these conditions were excluded.
Participants who appeared eligible based on the telephone screening participated in a clinical clearance visit. During the visit, participants provided informed consent and Health Insurance Portability and Accountability Act authorization in addition to undergoing a physical exam and blood draw to confirm eligibility.
Randomization
DIHFS participants were randomly assigned to the HGHH or control group. Allocation sequence was determined by the study statistician and stratified by BMI (25.0–29.9 versus 30.0–39.9) using permuted blocks, with randomly varying block sizes, so each group had an equal number of participants within the blocks. As a result of substantial budget cuts early in the project, FNCH staffing was limited to a single health educator. To make the protocol manageable at that site, all participants were assigned to the HGHH group.
Sample
The sample included 89 HGHH participants (DIHFS = 47; FNCH = 42) and 50 control participants, resulting in an analysis sample of 139 individuals.
Procedures
Once eligibility was established, participants completed the baseline survey—which included items addressing sociodemographics, cardiovascular knowledge and health literacy—and were randomized. HGHH participants were scheduled to attend the next set of HGHH classes and control participants were given written information about heart health (which HGHH participants also received). Three months after randomization, participants completed the survey again.
HGHH curriculum
HGHH is a 10-session curriculum intended to promote heart health among AI/ANs [22]. Sessions cover heart attack symptoms and the importance of 911, risk factors for diabetes and CVD, benefits of and ways to increase physical activity, smoking hazards and cessation, maintaining a healthy weight and controlling blood pressure and cholesterol. To reduce burden and increase participation, we presented the curriculum in five classes covering two sessions each, each class was conducted in the evenings and offered twice, and participants received a $10 gift card to a local vendor (e.g. Walmart) for each class attended. Classes were taught by two Native health educators and a non-Native research assistant; all were well educated in the curriculum.
We adapted the HGHH curriculum, incorporating recent data on CVD in AI/ANs and adding information on diabetes, stroke and the difference between commercial and traditional tobacco (an important topic in Native communities). We also incorporated handouts from the American Heart Association and the American Red Cross as well as excerpts from the documentary videos ‘Unnatural Causes: Is Inequality Making Us Sick?’ and ‘How to Get Fat Without Really Trying’, presented food commercials to initiate discussion of advertising and food choices, and integrated 30 min of physical activity into each class.
Measures
We used survey data from baseline and 3 months to examine the impact of HGHH on cardiovascular knowledge. The following measures were used:
Sociodemographics
Sociodemographic characteristics included age, gender, ethnicity, education, income, employment and marital status. To avoid excluding participants who did not provide income data (5.0%), the income variable included a category representing missing data.
Cardiovascular knowledge
Three types of knowledge were assessed: (i) heart attack symptom knowledge, (ii) stroke symptom knowledge and (iii) general knowledge of CVD and its risk factors. Knowledge of heart attack and stroke symptoms was measured using items from the Behavioral Risk Factor Surveillance System (BRFSS), a state-based, random-digit-dialed telephone survey of US adults [52, 53]. Participants indicated whether six symptoms were warning signs of heart attack and six symptoms were warning signs of stroke (‘Yes,’ ‘No’ or ‘Don’t Know’). In each case, five symptoms were hallmark signs of the condition and one was a decoy (i.e. not a real symptom). Each decoy symptom was, in fact, a hallmark symptom of the alternate condition (e.g. ‘chest pain or discomfort’ was a real symptom for heart attack and a decoy for stroke). One additional BRFSS item asked participants ‘If you thought someone was having a heart attack or stroke, what is the first thing you would do?’ The percentage of participants correctly responding that they would call 911 is reported.
Participants were asked to respond ‘Yes’, ‘No’ or ‘Don’t Know’ to six items assessing general CVD knowledge (e.g. A large waist can increase your risk of heart disease). Items were adapted from measures developed by NHLBI, for which psychometric testing has not been reported [54].
We examined responses to each item and to overall measures of cardiovascular knowledge. For both heart attack and stroke, we computed a continuous measure reflecting the percentage of hallmark symptoms that were correctly recognized. Consistent with prior BRFSS research [12, 19, 55–61], we also computed dichotomous variables identifying (i) whether a participant correctly identified all five hallmark symptoms of heart attack (or stroke) and (ii) whether a participant showed ‘optimal’ heart attack (or stroke) knowledge. Participants had optimal knowledge if they endorsed all five hallmark symptoms, did not endorse the decoy (incorrect) symptom and indicated that they would call 911. To assess general CVD knowledge, we computed a continuous measure reflecting the percentage of items answered correctly.
Health literacy
Health literacy was measured using a single item—‘How confident are you filling out medical forms by yourself?’—which has been shown to provide an accurate indication of health literacy skills [62–67]. As in prior studies [63, 65, 66], we identified participants answering ‘somewhat’, ‘a little bit’ or ‘not at all’ as having inadequate health literacy and participants responding that they were ‘quite a bit’ or ‘extremely’ confident as having adequate health literacy.
Attendance
We report the percentage of HGHH participants who did not attend any educational sessions as well as the average number of sessions attended.
Analysis
Descriptive analyses examined sample characteristics, baseline performance on overall knowledge measures and HGHH attendance. Depending on variable format, we used chi-square or two-sample t-test to determine whether participants differed across groups (i.e. HGHH or control) or data collection sites (i.e. DIHFS or FNCH).
Two sets of analyses were conducted to evaluate the impact of HGHH on cardiovascular knowledge. For the three continuous measures of overall knowledge (i.e. % of heart attack [or stroke] symptoms recognized, % of general CVD knowledge items answered correctly), we tested linear mixed models using all available data to predict knowledge as a function of treatment group, time point (baseline versus 3 month) and the interaction of group by time point. Analyses controlled for age, education, income and site.
McNemar’s chi-square tests examined change over time in performance on individual items and on the four dichotomous measures of overall knowledge (i.e. correctly recognized all real symptoms of heart attack [or stroke], had optimal knowledge of heart attack [or stroke]). Analyses were conducted separately by group and indicated whether a particular group showed significant improvement from baseline to 3 months. Analyses included participants who had survey data at both time points (N = 136).
Finally, we assessed the impact of health literacy on knowledge acquisition. Linear mixed models using all available data were conducted to predict the three continuous measures of overall knowledge as a function of health literacy (controlling for age, education, income and site). Analyses examined whether performance differed across health literacy groups at baseline and 3 months and whether the degree of change over time differed across health literacy groups.
Consistent with the intention-to-treat approach to analysis of randomized controlled trials [68], linear mixed model analyses included all participants (N = 139) and tables present results based on this sample. To account for non-attendance, analyses were repeated including only HGHH participants who attended at least one session (i.e. the As-Treated sample). When results using the As-Treated and full samples differed, we report both sets of findings in the text. Analyses and randomization were conducted using SAS versions 9.2 and 9.3 [69].
Results
Sample description
Participants were AI/ANs age 20–64 years, with an average age of 36.8 years (Table I). Three-quarters of the sample was female, with 10.9% self-identifying as Hispanic/Latino (as well as AI/AN), and nearly half reporting being married/cohabiting. The sample was well educated, with three-quarters having at least some college or vocational training. Participants faced significant challenges, however, with 45.3% having a household income of <$20 000 for the prior year, more than half being unemployed, and nearly one-quarter having inadequate health literacy. Participant characteristics did not differ across treatment groups or sites (Ps > 0.10).
Table I.
Baseline characteristics by groupa
| Raw mean (SD) or frequency (%)b |
|||
|---|---|---|---|
| Participant characteristics | Total sample (N = 139) | HGHH group (N = 89) | Control groupc (N = 50) |
| Age, mean (SD) | 36.8 (10.5) | 35.7 (10.1) | 38.9 (11.0) |
| Gender: female (%) | 75.5 | 75.3 | 76.0 |
| Ethnicity: Hispanic/Latino (%) | 10.9 | 9.1 | 14.0 |
| Education: highest grade completed | |||
| <High school graduate (%) | 5.8 | 6.7 | 4.0 |
| High school grad/GED (%) | 20.1 | 20.2 | 20.0 |
| Some college/vocational (%) | 45.3 | 47.2 | 42.0 |
| College degree or more (%) | 28.8 | 25.8 | 34.0 |
| Income: pre-tax household income for prior year | |||
| <$10K (%) | 27.3 | 27.0 | 28.0 |
| $10K to <$20K (%) | 18.0 | 21.4 | 12.0 |
| $20K to <$30K (%) | 16.6 | 16.8 | 16.0 |
| $30K to <$40K (%) | 16.6 | 15.7 | 18.0 |
| ≥$40K (%) | 16.6 | 16.8 | 16.0 |
| Income missing (%) | 5.0 | 2.2 | 10.0 |
| Currently employed (%) | 46.3 | 45.4 | 47.9 |
| Married/cohabiting (%) | 47.8 | 51.1 | 42.0 |
| Inadequate health literacy (%) | 22.3 | 19.1 | 28.0 |
| Overall knowledge variables: baseline values | |||
| Knowledge of heart attack symptoms | |||
| % Real symptoms correctly identified, mean (SD) | 61.5 (28.0) | 61.7 (28.2) | 61.2 (27.8) |
| Correctly identified all real symptoms (%) | 15.9 | 13.6 | 20.0 |
| Correctly identified all real symptoms, did not endorse decoy symptom and knew to call 911 (%) | 4.4 | 2.3 | 8.0 |
| Knowledge of stroke symptoms | |||
| % Real symptoms correctly identified, mean (SD) | 71.7 (27.9) | 71.2 (26.3) | 72.4 (30.7) |
| Correctly identified all real symptoms (%) | 32.4 | 29.2 | 38.0 |
| Correctly identified all real symptoms, did not endorse decoy symptom and knew to call 911 (%) | 10.1 | 7.9 | 14.0 |
| General cardiovascular knowledge | |||
| % Items answered correctly, mean (SD) | 87.2 (14.7) | 87.5 (14.3) | 86.7 (15.4) |
| Intervention attendance by HGHH participants | Total HGHH (N = 89) | Denver (N = 47) | Albuquerque (N = 42) |
| Number of sessions attended, mean (SD) | 5.3 (3.8) | 4.5 (3.8) | 6.3 (3.7) |
| Attended ≥1 session (%) | 78.6 | 72.3 | 85.7 |
aChi-square and two-sample t-test analyses indicated that HGHH participants did not differ across sites (i.e. Denver and Albuquerque) on baseline participant characteristics or knowledge scores (Ps > 0.10). However, HGHH participants in Albuquerque did attend significantly more HGHH sessions on average than did their counterparts in Denver (P < 0.05).
bRaw means (SDs) and frequencies are reported.
cChi-square and two-sample t-test analyses indicated that the HGHH and control groups did not differ on baseline participant characteristics or baseline performance on the overall knowledge measures (Ps > 0.10).
At baseline, participants recognized 61.5% of heart attack symptoms, with 15.9% recognizing all five symptoms and 4.4% having optimal knowledge (Table I). Participants recognized 71.7% of stroke symptoms, with nearly one-third identifying all real symptoms and 10.1% having optimal knowledge. On average, participants answered 87.2% of the general CVD knowledge questions correctly. Baseline knowledge did not differ by treatment group or site (Ps > 0.10).
Participants in the HGHH group attended an average of 5.3 out of 10 sessions, although 21.4% of participants failed to attend any sessions (Table I). A two-sample t-test indicated that HGHH participants from FNCH attended significantly more sessions than did HGHH participants from DIHFS (P ≤ 0.05).
Overall knowledge
Table II presents performance on the overall knowledge measures at baseline and 3 months. Linear mixed models showed that the percentage of heart attack symptoms correctly recognized improved significantly more over time for HGHH than control participants (P ≤ 0.01) and that stroke and general CVD knowledge scores improved marginally more in the HGHH than the control group (P ≤ 0.10). When analyses were restricted to the As-Treated sample, the HGHH group showed significantly greater improvement than the control group on all three measures (P ≤ 0.05).
Table II.
Change over time in overall outcome measuresa
| HGHH group |
Control group |
|||
|---|---|---|---|---|
| Baseline | 3 months | Baseline | 3 months | |
| Continuous measuresa | (N = 89) | (N = 50) | ||
| % Real heart attack symptoms correctly identified** | 60.7 | 81.7 | 60.7 | 63.5 |
| % Real stroke symptoms correctly identified^ | 70.6 | 81.5 | 75.1 | 78.2 |
| % General CVD knowledge items answered correctly^ | 86.4 | 92.0 | 86.3 | 87.3 |
| Dichotomous measuresb | (N = 86) | (N = 50) | ||
| Heart attack | ||||
| Correctly identified all real heart attack symptoms | 13.6 | 52.3** | 20.0 | 20.0 |
| Showed ‘optimal’ knowledge of heart attackc | 2.3 | 5.8 | 8.0 | 10.0 |
| Stroke | ||||
| Correctly identified all real stroke symptoms | 29.2 | 46.5** | 38.0 | 40.0 |
| Showed ‘optimal’ knowledge of strokec | 7.9 | 12.8 | 14.0 | 14.0 |
aFor continuous outcome measures, the table presents least-squared means (predicted values) by group and time point. Linear mixed models assessed whether change in performance over time was significantly different in the HGHH and control groups: ^P ≤ 0.10, **P ≤ 0.001.
bFor dichotomous measures, raw frequencies are presented. McNemar’s chi-square analyses assessed whether performance within a group (HGHH or control) improved significantly over time: ^P ≤ 0.10, **P ≤ 0.01.
cParticipants were identified as having ‘optimal’ knowledge if they correctly recognized all real symptoms of heart attack (or stroke), knew that the decoy symptom was not a real symptom of heart attack (or stroke) and knew to call 911 in the event of a heart attack or stroke.
The percentage of HGHH participants who recognized all real symptoms of heart attack or stroke significantly increased over time (Ps ≤ 0.01) (Table II). HGHH participants did not show significant improvement on the measures of optimal knowledge, however (Ps > 0.10). For control participants, performance on these measures did not change over time (P > 0.10).
Item-level analyses
Table III presents performance on each knowledge item over time. The HGHH group showed significant improvement over time in recognition of four hallmark symptoms of heart attack (Ps ≤ 0.01). Participants in the control group showed significant improvement in recognition of one symptom (P ≤ 0.05) and a significant decline in recognition of another symptom (P ≤ 0.05). Unlike control participants (P > 0.10), HGHH participants showed a significant increase in incorrect endorsement of the decoy symptom (P ≤ 0.01).
Table III.
Performance on each heart attack/stroke or general CVD knowledge item over timea
| HGHH group (N = 86) |
Control group (N = 50) |
|||
|---|---|---|---|---|
| Baseline | 3 months | Baseline | 3 months | |
| Symptoms of heart attack | % Endorsing each symptom | |||
| Pain or discomfort in the jaw, neck or back | 30.7 | 72.1** | 28.0 | 30.0 |
| Feeling weak, lightheaded or faint | 47.2 | 77.9** | 48.0 | 64.0* |
| Chest pain or discomfort | 85.4 | 97.7** | 98.0 | 86.0* |
| Pain or discomfort in the arms or shoulder | 73.0 | 89.5** | 68.0 | 70.0 |
| Shortness of breath | 71.9 | 79.1 | 64.0 | 70.0 |
| Incorrect symptom | ||||
| Sudden trouble seeing in one or both eyes | 42.7 | 65.1** | 42.0 | 44.0 |
| Symptoms of stroke | % Endorsing each symptom | |||
| Sudden confusion or trouble speaking | 80.9 | 93.0** | 88.0 | 90.0 |
| Sudden numbness/weakness of face, arm or leg | 94.4 | 95.4 | 90.0 | 96.0 |
| Sudden trouble seeing in one or both eyes | 57.3 | 77.9** | 62.0 | 66.0 |
| Sudden trouble walking, dizziness or loss of balance | 82.0 | 90.7^ | 78.0 | 80.0 |
| Severe headache with no known cause | 41.6 | 52.3^ | 44.0 | 46.0 |
| Incorrect symptom | ||||
| Chest pain or discomfort | 55.1 | 65.1 | 48.0 | 50.0 |
| What do if someone has a heart attack/stroke | % Answering correctly | |||
| Call 911 | 92.1 | 96.5 | 96.0 | 98.0 |
| General cardiovascular knowledge items | % Answering correctly | |||
| A large waist can increase your risk of heart disease | 82.6 | 93.0* | 82.0 | 86.0 |
| Foods high in sodium can increase your risk of high blood pressure | 96.5 | 96.5 | 92.0 | 96.0 |
| Eating too much saturated and trans fat can raise your bad cholesterol level | 91.9 | 95.4 | 96.0 | 98.0 |
| Blood pressure of 140/90 mm Hg is considered high | 57.0 | 73.3** | 54.0 | 54.0 |
| Overweight/obesity can increase your risk of high cholesterol | 97.7 | 100.0b | 98.0 | 96.0 |
| Physical activity can reduce your risk for heart disease | 98.8 | 100.0b | 98.0 | 96.0 |
aRaw frequencies of participants endorsing each symptom or answering each item correctly are presented. McNemar’s chi-square analyses assessed whether performance within a group (HGHH or control) improved significantly over time: ^P ≤ 0.10,*P ≤ 0.05,**P ≤ 0.01.
bTest statistic could not be calculated because there was no variability at the 3-month time point.
HGHH participants improved significantly in their recognition of two hallmark symptoms of stroke (Ps ≤ 0.01) and marginally in their recognition of two others (P < 0.10) (Table III). When analyses were restricted to the As-Treated sample, these two marginal findings became non-significant (P > 0.10). Although HGHH participants showed an increase in incorrect endorsement of the decoy symptom, this change was non-significant (P > 0.10). Control participants showed no significant changes in stroke knowledge over time (P > 0.10).
At baseline and 3 months, the majority of participants in both groups understood that one should call 911 in the event of a heart attack or stroke (Table III). Neither group showed significant improvement over time on this measure.
General CVD knowledge was strong at baseline, with 82.0–98.8% of participants answering each item correctly (Table III). One item that proved particularly challenging asked respondents whether a blood pressure value of 140/90 mm Hg is considered high. Approximately half of participants answered this question correctly at baseline.
HGHH participants showed significant improvement over time on two general CVD knowledge items (Ps ≤ 0.05), including the blood pressure item that proved challenging at baseline. For two additional items, chi-square statistics could not be computed because 100% of HGHH participants answered the items correctly at 3 months. When analyses were restricted to the As-Treated sample, the HGHH group showed significant improvement on one additional item (i.e. saturated and trans fat; P ≤ 0.01) and a significance value could not be computed for the challenging blood pressure item because 100% of HGHH participants answered the item correctly at 3 months. The control group did not experience change on any general CVD knowledge items (Ps > 0.10).
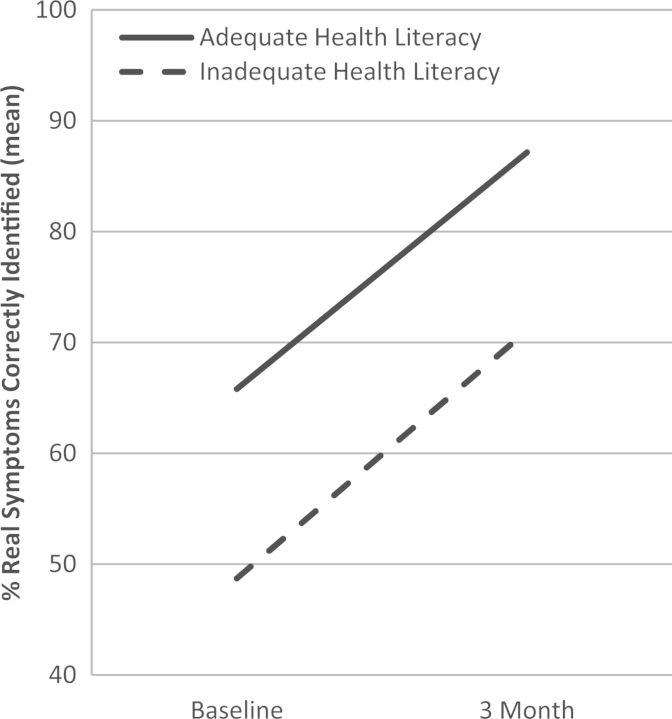
Health literacy and knowledge acquisition
Participants with inadequate health literacy had more limited knowledge of heart attack symptoms than did those with adequate health literacy at both the baseline and 3-month visits (Ps ≤ 0.05; Fig. 1). However, there was no difference in the amount of knowledge gained over time (i.e. 21.4 points for participants with adequate health literacy and 22.4 points for participants with inadequate health literacy). Using the As-Treated sample, the difference between health literacy groups in baseline knowledge scores remained (P ≤ 0.05), but the group difference at 3 months failed to reach significance (P ≤ 0.06). Again, there was no difference in the amount of knowledge gained over time between groups (P > 0.10).
Fig. 1.
Change over time in heart attack knowledge (% real symptoms correctly identified) by health literacy level. Linear mixed models indicated that participants with adequate health literacy had significantly better heart attack knowledge at baseline (P < 0.05) and 3 months (P < 0.05) than did participants with inadequate health literacy. Participants did not differ by literacy group in the amount of knowledge gained between the baseline and 3-month visits (P > 0.10).
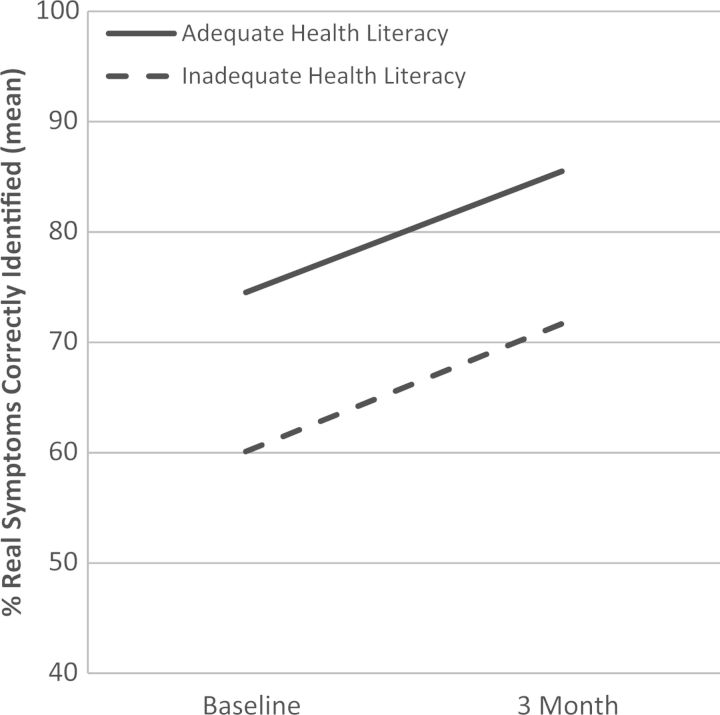
Participants with inadequate health literacy had significantly lower stroke knowledge at baseline and 3 months than did participants with adequate health literacy (Ps ≤ 0.05; Fig. 2). Improvement over time, however, did not differ by group (P > 0.10). Participants with adequate health literacy gained 10.8 points, while those with inadequate health literacy gained 10.6 points. Using the As-Treated sample, group differences at baseline and 3 months were not significant (P > 0.10).
Fig. 2.
Change over time in stroke knowledge (% real symptoms correctly identified) by health literacy level. Linear mixed models indicated that participants with adequate health literacy had significantly better stroke knowledge at baseline (P < 0.05) and 3 months (P < 0.05) than did participants with inadequate health literacy. Participants did not differ by literacy group in the amount of knowledge gained between the baseline and 3-month visits (P > 0.10).
The overall measure of general CVD knowledge showed a different pattern of results. Participants in the two health literacy groups did not differ at baseline or 3 months on general CVD knowledge (Ps > 0.10), nor did the two groups experience different degrees of improvement over time (P > 0.10).
Discussion
Results corroborate prior work suggesting limitations in cardiovascular knowledge among AI/ANs [12, 19, 20]. Participants recognized 62% of heart attack symptoms and 72% of stroke symptoms. Although most knew to call 911 in the event of a heart attack or stroke, limited symptom recognition could hinder their ability to respond appropriately in an emergency.
Heart attack and stroke knowledge appeared more limited in this sample than national samples. This study and earlier work [19] indicated that 13–20% of AI/ANs recognized all hallmark symptoms of heart attack, compared with 31% nationally [58]. Studies using national data showed that 10–16% of participants had optimal heart attack knowledge [12, 56, 58], compared with 2% of HGHH participants and 8% of controls in this study. Likewise, 20–38% of AI/ANs in this and an earlier study [19] correctly recognized all symptoms of stroke, compared with 44% nationally [59]. Further, this study and earlier work indicated that 8–15% of AI/ANs have optimal stroke knowledge [12], compared with 16–21% of participants nationally [12, 55, 57, 59].
Consistent with earlier work [19], general CVD knowledge was strong at baseline. It is possible that urban AI/ANs are exposed to general information about CVD risk (e.g. risks of eating too much salt, being overweight) from multiple sources, including care providers, media and public health campaigns. The specific symptoms of heart attack and stroke may receive less public attention and thus be less well recognized.
Although general CVD knowledge was strong, identifying whether a specific blood pressure value is high was challenging for participants in this and an earlier study [19]. Across the two samples, approximately half of participants correctly identified a blood pressure value of 140/90 mm Hg as high. Given that accurate knowledge of normal blood pressure values is associated with better blood pressure control [70, 71], these findings highlight the need for improved hypertension awareness among AI/ANs.
The adapted HGHH curriculum improved cardiovascular knowledge. HGHH participants showed significantly greater improvement over time in heart attack knowledge than did control participants and marginally greater improvement in stroke and general CVD knowledge. When analyses were restricted to participants who attended at least one class, HGHH participants showed significantly greater improvement on all three continuous measures.
There are two main reasons participants may have shown more substantial improvement in heart attack than stroke or general CVD knowledge. First, because participants had a lower level of heart attack than stroke or general CVD knowledge at baseline, there was more opportunity for improvement in their knowledge of heart attack symptoms. Second, even with our adaptation of the curriculum, stroke was not addressed as fully as was heart attack. The adapted curriculum covered heart attack extensively, addressing why heart attack happens, presenting symptoms and highlighting the need for immediate treatment. Participants received handouts related to symptoms and the importance of rapid treatment, engaged in role-plays, completed a heart attack survival plan and made a pledge to prepare themselves in case of heart attack. Although we added content addressing the symptoms and causes of stroke, facts about stroke in AI/ANs and the importance of calling 911, less class time and fewer interactive activities were focused on stroke than heart attack.
Although HGHH participants improved in recognition of heart attack and stroke symptoms, the percentage of respondents with optimal knowledge remained low. In part, this pattern occurred because HGHH participants showed an increase in incorrect endorsement of decoy symptoms. Although this may suggest that participants developed a tendency to endorse any symptom—a possibility to which future intervention researchers using BRFSS items should be alert—it also may indicate that participants recognized all symptoms but were unable to identify with which condition each symptom was associated. Because confusion of symptoms may result in less effective identification of heart attack or stroke, it may be valuable for health promotion curricula to more clearly distinguish between the two conditions.
As few studies have examined the relationship of health literacy with change in knowledge over time, this work provides important insight. In this study, participants with inadequate health literacy experienced the same degree of improvement in heart attack and stroke knowledge as did participants with adequate skills. Corroborating some earlier work [38–41], these results suggest that low- and high-literate individuals are equally capable of acquiring knowledge in response to appropriate intervention. Like some other studies have shown, however [41], knowledge among low-literate participants continued to lag behind that of participants with higher health literacy skills. Although those with limited skills made significant gains, their lower baseline knowledge was difficult to overcome. It may be that low-literate individuals would benefit from additional class sessions or supplemental interventions to enhance knowledge gain.
As with all studies, the project had limitations. The moderate sample size and lack of a control group at FNCH—both necessitated by substantial budget cuts—may have influenced results. Further, because the study was conducted in two urban Indian clinics, results might not generalize to other AI/AN populations, including reservation communities or tribal groups unlikely to be represented in these western samples. Also, because we adapted the HGHH curriculum, this work does not provide a pure test of HGHH effectiveness.
The high rate of non-attendance by HGHH participants was an important limitation and may have resulted in underestimation of intervention effects. A multitude of factors may have influenced participation, including individual-level factors (e.g. geographic distance from the classroom), site-level factors (e.g. having a single project staff member in Albuquerque versus a multi-person project team in Denver), and HGHH instructor-level factors (e.g. Native versus non-Native). The authors are planning analyses of participant evaluation feedback and site-level data to identify factors influencing participation.
In conclusion, this work suggests that many AI/ANs have strong knowledge of general CVD risk but limited awareness of heart attack and stroke symptoms. These results are concerning given the high prevalence of CVD in AI/ANs and support the importance of educational interventions to improve cardiovascular knowledge. Findings suggest that the adapted HGHH curriculum improved knowledge and that participants with limited health literacy skills benefitted to the same degree as more literate participants. As the first reported evaluation of HGHH, this work provides important insight and suggests that HGHH-based education can support development of cardiovascular knowledge among AI/ANs across a range of health literacy levels.
Funding
National Institute on Minority Health and Health Disparities (RC2 MD004749 to J.B. and K.M.); Centers for Disease Control and Prevention (U58 DP00120 to Spero Manson).
Conflict of interest statement
None declared.
Acknowledgements
We would like to thank Denver Indian Health and Family Services, First Nations Community HealthSource, and the participants who gave so graciously of their time and effort. We are also grateful to Dakotah Jim and Rhonda Dick for their excellent work on this project.
References
- 1.Howard BV, Lee ET, Cowan LD, et al. Rising tide of cardiovascular disease in American Indians. The Strong Heart Study. Circulation. 1999;99:2389–95. doi: 10.1161/01.cir.99.18.2389. [DOI] [PubMed] [Google Scholar]
- 2.Howard BV, Lee ET, Cowan LD, et al. Coronary heart disease prevalence and its relation to risk factors in American Indians. The Strong Heart Study. Am J Epidemiol. 1995;142:254–68. doi: 10.1093/oxfordjournals.aje.a117632. [DOI] [PubMed] [Google Scholar]
- 3.Rhoades DA, Rhoades ER, Welty TK. The rise of cardiovascular diseases. In: Rhoades ER, editor. American Indian Health: Innovations in Health Care, Promotion, and Policy. Baltimore: Johns Hopkins University Press; 2000. pp. 151–78. [Google Scholar]
- 4.Sievers ML, Fisher JR. Diseases of North American Indians. In: Rothschild HR, editor. Biocultural Aspects of Disease. New York, NY: Academic Press; 1981. pp. 191–252. [Google Scholar]
- 5.Nelson RG, Sievers ML, Knowler WC, et al. Low incidence of fatal coronary heart disease in Pima Indians despite high prevalence of non-insulin-dependent diabetes. Circulation. 1990;81:987–95. doi: 10.1161/01.cir.81.3.987. [DOI] [PubMed] [Google Scholar]
- 6.Rhoades DA. Racial misclassification and disparities in cardiovascular disease among American Indians and Alaska Natives. Circulation. 2005;111:1250–6. doi: 10.1161/01.CIR.0000157735.25005.3F. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y, Galloway JM, Welty TK, et al. Incidence and risk factors for stroke in American Indians: The Strong Heart Study. Circulation. 2008;118:1577–84. doi: 10.1161/CIRCULATIONAHA.108.772285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Prevalence of heart disease—United States, 2005. Morb Mortal Wkly Rep. 2007;56:113–8. [PubMed] [Google Scholar]
- 9.Indian Health Service. Trends in Indian Health. Rockville, MD: United States Department of Health and Human Services; 1997. [Google Scholar]
- 10.Rhoades DA, Welty TK, Wang W, et al. Aging and the prevalence of cardiovascular disease risk factors in older American Indians: The Strong Heart Study. J Am Geriatr Soc. 2007;55:87–94. doi: 10.1111/j.1532-5415.2006.01018.x. [DOI] [PubMed] [Google Scholar]
- 11. Indian Health Service. Trends in Indian Health. 2000–2001. Washington DC: United States Department of Health and Human Services, 40–163.
- 12.Liao Y, Bang D, Cosgrove S, et al. Surveillance of health status in minority communities—Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. Morb Mortal Wkly Rep Surveill Summ. 2011;60:1–44. [PubMed] [Google Scholar]
- 13.Barnes PM, Adams PF, Powell-Griner E. Health Characteristics of the American Indian or Alaska Native Adult Population: United States, 2004-2008 National health statistics reports; No 20. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC) Trends in cholesterol screening and awareness of high blood cholesterol—United States, 1991-2003. Morb Mortal Wkly Rep. 2005;54:865–70. [PubMed] [Google Scholar]
- 15.National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics, 2007 Fact Sheet. Bethesda, MD: United States Department of Health and Human Services, National Institutes of Health; 2008. [Google Scholar]
- 16.Pleis JR, Lethbridge-Çejku M. Vital Health Stat. Summary health statistics for U.S. adults: National Health Interview Survey, 2006. National Center for Health Statistics. 10(235), 2007. [PubMed] [Google Scholar]
- 17.Steele CB, Cardinez CJ, Richardson LC, et al. Surveillance for health behaviors of American Indians and Alaska Natives—findings from the behavioral risk factor surveillance system, 2000-2006. Cancer. 2008;113:1131–41. doi: 10.1002/cncr.23727. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC) Prevalence of cigarette use among 14 racial/ethnic populations: United States, 1999-2001. Morb Mortal Wkly Rep. 2004;53:49–52. [PubMed] [Google Scholar]
- 19.Brega AG, Noe T, Loudhawk-Hedgepeth C, et al. Cardiovascular knowledge among Urban American Indians and Alaska Natives: first steps in addressing community needs. Prog Community Health Partnersh. 2011;5:273–9. doi: 10.1353/cpr.2011.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schweigman K, Eichner J, Welty TK, et al. Cardiovascular disease risk factor awareness in American Indian communities: the strong heart study. Ethn Dis. 2006;16:647–52. [PubMed] [Google Scholar]
- 21.Wallace MF, Fulwood R, Alvarado M. NHLBI step-by-step approach to adapting cardiovascular training and education curricula for diverse audiences. Prev Chronic Dis. 2008;5:A61. [PMC free article] [PubMed] [Google Scholar]
- 22.National Heart, Lung, and Blood Institute, Indian Health Service. Honoring the Gift of Heart Health: A Heart Health Educator's Manual. Bethesda, MD: United States Department of Health and Human Services; 2006. [Google Scholar]
- 23.Indian Health Service. Indian Health Diabetes Best Practices: Cardiovascular Health and Diabetes. Albuquerque, NM: United States Department of Health and Human Services, Division of Diabetes Treatment and Prevention; 2011. [Google Scholar]
- 24.Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan SC, et al., editors. National Library of Medicine Current Bibliographies in Medicine: Health Literacy NLM Pub No CBM 2000-1. Bethesda, MD: National Institutes of Health, United States Department of Health and Human Services; 2000. [Google Scholar]
- 25.Kutner M, Greenberg E, Jin Y, et al. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006–483) U.S. Department of Education. Washington, DC: National Center for Education Statistics; 2006. [Google Scholar]
- 26.Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007;33:144–51. doi: 10.1177/0145721706297452. [DOI] [PubMed] [Google Scholar]
- 27.Ussher M, Ibrahim S, Reid F, et al. Psychosocial correlates of health literacy among older patients with coronary heart disease. J Health Commun. 2010;15:788–804. doi: 10.1080/10810730.2010.514030. [DOI] [PubMed] [Google Scholar]
- 28.Schillinger D, Machtinger EL, Wang F, et al. Language, literacy, and communication regarding medication in an anticoagulation clinic: a comparison of verbal vs. visual assessment. J Health Commun. 2006;11:651–64. doi: 10.1080/10810730600934500. [DOI] [PubMed] [Google Scholar]
- 29.Persell SD, Osborn CY, Richard R, et al. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med. 2007;22:1523–6. doi: 10.1007/s11606-007-0334-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mancuso JM. Impact of health literacy and patient trust on glycemic control in an urban USA population. Nurs Health Sci. 2010;12:94–104. doi: 10.1111/j.1442-2018.2009.00506.x. [DOI] [PubMed] [Google Scholar]
- 31.Ishikawa H, Takeuchi T, Yano E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care. 2008;31:874–9. doi: 10.2337/dc07-1932. [DOI] [PubMed] [Google Scholar]
- 32.Gerber BS, Pagcatipunan M, Smith EV, Jr, et al. The assessment of diabetes knowledge and self-efficacy in a diverse population using Rasch measurement. J ApplMeas. 2006;7:55–73. [PubMed] [Google Scholar]
- 33.Gazmararian JA, Williams MV, Peel J, et al. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–75. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 34.DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. Am J Health Behav. 2007;31(Suppl. 1):S27–35. doi: 10.5555/ajhb.2007.31.supp.S27. [DOI] [PubMed] [Google Scholar]
- 35.Arnold CL, Davis TC, Berkel HJ, et al. Smoking status, reading level, and knowledge of tobacco effects among low-income pregnant women. Prev Med. 2001;32:313–20. doi: 10.1006/pmed.2000.0815. [DOI] [PubMed] [Google Scholar]
- 36.Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. 2011;13:335–41. doi: 10.1089/dia.2010.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dennison CR, McEntee ML, Samuel L, et al. Adequate health literacy is associated with higher heart failure knowledge and self-care confidence in hospitalized patients. J Cardiovasc Nurs. 2011;26:359–67. doi: 10.1097/JCN.0b013e3181f16f88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eckman MH, Wise R, Leonard AC, et al. Impact of health literacy on outcomes and effectiveness of an educational intervention in patients with chronic diseases. Patient Educ Couns. 2012;87:143–51. doi: 10.1016/j.pec.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 39.Gerber BS, Brodsky IG, Lawless KA, et al. Implementation and evaluation of a low-literacy diabetes education computer multimedia application. Diabetes Care. 2005;28:1574–80. doi: 10.2337/diacare.28.7.1574. [DOI] [PubMed] [Google Scholar]
- 40.Meade CD, McKinney WP, Barnas GP. Educating patients with limited literacy skills: the effectiveness of printed and videotaped materials about colon cancer. Am J Public Health. 1994;84:119–21. doi: 10.2105/ajph.84.1.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wallace AS, Seligman HK, Davis TC, et al. Literacy-appropriate educational materials and brief counseling improve diabetes self-management. Patient Educ Couns. 2009;75:328–33. doi: 10.1016/j.pec.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kandula NR, Nsiah-Kumi PA, Makoul G, et al. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Educ Couns. 2009;75:321–7. doi: 10.1016/j.pec.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 43.Sobel RM, Paasche-Orlow MK, Waite KR, et al. Asthma 1-2-3: a low literacy multimedia tool to educate African American adults about asthma. J Commun Health. 2009;34:321–7. doi: 10.1007/s10900-009-9153-9. [DOI] [PubMed] [Google Scholar]
- 44.Brega AG, Ang A, Vega W, et al. Mechanisms underlying the relationship between health literacy and glycemic control in American Indians and Alaska Natives. Patient Educ Couns. 2012;88:61–8. doi: 10.1016/j.pec.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 45.Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. J Gen Intern Med. 2006;21:813–7. doi: 10.1111/j.1525-1497.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Osborn CY, Paasche-Orlow MK, Bailey SC, et al. The mechanisms linking health literacy to behavior and health status. Am J Health Behav. 2011;35:118–28. doi: 10.5993/ajhb.35.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980–6. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 49.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall, Inc.; 1986. [Google Scholar]
- 50.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 51.Prochaska JO, Johnson S, Lee P. The transtheoretical model of behavior change. In: Shumaker SA, Schron EB, Ockene JK, et al., editors. The Handbook of Health Behavior Change. 2nd edn. New York: Springer Publishing Company; 1998. pp. 59–84. [Google Scholar]
- 52.Centers for Disease Control and Prevention (CDC) The Behavioral Risk Factor Surveillance System User's Guide. Atlanta, GA: U.S. Department of Health and Human Services; 2003. [Google Scholar]
- 53.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA: U.S. Department of Health and Human Services, CDC; 2007. [Google Scholar]
- 54.National Heart, Lung, and Blood Institute. Evaluation Package for “Honoring the Gift of Heart Health” Manual. Bethesda, MD: United States Department of Health and Human Services; 2008. [Google Scholar]
- 55.Croft JB, Greenlund KJ, Ayala C, et al. Awareness of stroke warning signs—17 states and the U.S. Virgin Islands, 2001. Morb Mortal Wkly Rep. 2004;53:359–62. [PubMed] [Google Scholar]
- 56.Greenlund KJ, Keenan NL, Giles WH, et al. Public recognition of major signs and symptoms of heart attack: seventeen states and the US Virgin Islands, 2001. Am Heart J. 2004;147:1010–6. doi: 10.1016/j.ahj.2003.12.036. [DOI] [PubMed] [Google Scholar]
- 57.Greenlund KJ, Neff LJ, Zheng ZJ, et al. Low public recognition of major stroke symptoms. Am J Prev Med. 2003;25:315–9. doi: 10.1016/s0749-3797(03)00206-x. [DOI] [PubMed] [Google Scholar]
- 58.Fang J, Keenan N, Dai S, et al. Disparities in adult awareness of heart attack warning signs and symptoms—14 states, 2005. Morb Mortal Wkly Rep. 2008;57:175–9. [PubMed] [Google Scholar]
- 59.Fang J, Keenan NL, Ayala C, et al. Awareness of stroke warning symptoms—13 States and the District of Columbia, 2005. Morb Mortal Wkly Rep. 2008;57:481–5. [PubMed] [Google Scholar]
- 60.Ellis C, Egede LE. Stroke recognition among individuals with stroke risk factors. Am J Med Sci. 2009;337:5–10. doi: 10.1097/MAJ.0b013e318176abd1. [DOI] [PubMed] [Google Scholar]
- 61.Ellis C, Egede LE. Racial/ethnic differences in stroke awareness among veterans. Ethn Dis. 2008;18:198–203. [PubMed] [Google Scholar]
- 62.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–94. [PubMed] [Google Scholar]
- 63.Wallace LS, Rogers ES, Roskos SE, et al. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21:874–7. doi: 10.1111/j.1525-1497.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23:561–6. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sarkar U, Schillinger D, Lopez A, et al. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2010;26:265–71. doi: 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wallace LS, Cassada DC, Rogers ES, et al. Can screening items identify surgery patients at risk of limited health literacy? J Surg Res. 2007;140:208–13. doi: 10.1016/j.jss.2007.01.029. [DOI] [PubMed] [Google Scholar]
- 67.Powers BJ, Trinh JV, Bosworth HB. Can this patient read and understand written health information? JAMA. 2010;304:76–84. doi: 10.1001/jama.2010.896. [DOI] [PubMed] [Google Scholar]
- 68.Peduzzi P, Henderson W, Hartigan P, et al. Analysis of randomized controlled trials. Epidemiol Rev. 2002;24:26–38. doi: 10.1093/epirev/24.1.26. [DOI] [PubMed] [Google Scholar]
- 69. SAS Institute, Inc. Cary, NC: SAS Institute, Inc.
- 70.Wizner B, Gryglewska B, Gasowski J, et al. Normal blood pressure values as perceived by normotensive and hypertensive subjects. J Hum Hypertens. 2003;17:87–91. doi: 10.1038/sj.jhh.1001516. [DOI] [PubMed] [Google Scholar]
- 71.Naik AD, Kallen MA, Walder A, et al. Improving hypertension control in diabetes mellitus: the effects of collaborative and proactive health communication. Circulation. 2008;117:1361–8. doi: 10.1161/CIRCULATIONAHA.107.724005. [DOI] [PMC free article] [PubMed] [Google Scholar]