Abstract
We report the successful arthroscopic treatment of a case of subcalcaneal bursitis with plantar fasciitis. To our knowledge, this is the first report on arthroscopic excision of a subcalcaneal bursa. Right heel pain developed in a 50-year-old woman, without any obvious cause. She reported that the heel pain occurred immediately after waking and that the heel ached when she walked. Magnetic resonance imaging showed an extra-articular, homogeneous, high-intensity lesion in the fat pad adjacent to the calcaneal tubercle on T2-weighted sagittal and coronal images and thickening of the plantar fascia on T2-weighted sagittal images. A diagnosis of a recalcitrant subcalcaneal bursitis with plantar fasciitis was made, and surgery was performed. The arthroscope was placed between the calcaneus and the plantar fascia. With the surgeon viewing from the lateral portal and working from the medial portal, the dorsal surface of the degenerative plantar fascia was debrided and the medial half of the plantar fascia was released, followed by debridement of the subcalcaneal bursal cavity through the incised plantar fascia. Full weight bearing and gait were allowed immediately after the operation. At the latest follow-up, the patient had achieved complete resolution of heel pain without a recurrence of the mass, confirmed by magnetic resonance imaging.
Plantar heel pain is a common symptom in daily clinical podiatric practice, and plantar heel pain may develop in 10% of persons in the general population during their lifetime.1 Conservative therapy for heel pain has been shown to be effective in about 90% of patients.2,3 However, recalcitrant plantar heel pain may require surgical treatment. Plantar fasciitis is the most common cause of plantar heel pain in adults; however, the distinction between plantar fasciitis and other conditions that cause plantar heel pain is sometimes difficult, and multiple lesions may coexist. Recently, the term “heel pain syndrome” has been proposed as an initial diagnosis for patients with symptoms of plantar heel pain.4
Subcalcaneal bursitis is 1 of several differential diagnoses of heel pain syndrome.4 Open excision of the bursa is performed for this condition if conservative treatment fails; however, the morbidity associated with the open excision, such as delayed healing of skin incisions, infection, and prolonged recovery time, is concerning.5,6
We report the successful arthroscopic treatment of a case of subcalcaneal bursitis with plantar fasciitis. Arthroscopic excision of the bursa has been reported in elbow and knee surgery, and compared with open surgery, it is associated with lower morbidity and faster recovery without major complications at both these locations.7,8 To our knowledge, this is the first report on arthroscopic excision of a subcalcaneal bursa.
Case
Right heel pain developed in a 50-year-old woman (height, 153 cm; body weight, 57 kg), without any obvious cause. She was referred to our department for management of the pain after separate attempts by 2 orthopaedic surgeons to treat her with extensive, conservative therapy. She reported that the heel pain occurred immediately after waking and that the heel ached when she walked.
On physical examination, tenderness was found at the plantar medial and central aspect of the heel, but a palpable mass or swelling was not found. The range of ankle motion showed no left-right difference. Dorsiflexion was 10°, and plantar flexion was 45°. The ankle was stable based on the anterior drawer or inversion-eversion stress tests. The patient's neurovascular status was normal. There was no evidence of nerve compression with pain such as the Tinel sign or pain over the nerve to the abductor digiti quinti (Baxter nerve). All laboratory data, including the C-reactive protein level and erythrocyte sedimentation rate, were within normal limits. The patient had not undergone previous foot surgery, and no local steroid injection had been administered. The Japanese Society for Surgery of the Foot ankle/hindfoot scale score was 67 (pain, 20; function, 37; alignment, 10). Plain radiographic findings were interpreted as normal except for a small calcaneal spur, but magnetic resonance imaging (MRI) showed an extra-articular, homogeneous, high-intensity lesion in the fat pad adjacent to the calcaneal tubercle on T2-weighted sagittal and coronal images and thickening of the plantar fascia on T2-weighted sagittal images (Fig 1). These findings were discussed with the patient, and the decision was made to proceed with operative intervention.
Fig 1.

T2-weighted sagittal image of preoperative MRI study shows an extra-articular, homogeneous, high-intensity lesion in the fat pad adjacent to the calcaneal tubercle and thickening of the plantar fascia.
Surgical Technique
Under general anesthesia, the patient was placed in the supine position without traction. The right lower extremity was prepared and draped in the usual sterile fashion. Preoperative antibiotics were administered. A pneumatic tourniquet was inflated to 280 mm Hg at the thigh. Two short arthroscopes (2.7-mm-diameter 30° and 70° arthroscopes) were used. First, a medial portal was made 10 mm anterior and 5 mm proximal to the medial calcaneal tubercle under fluoroscopy. A 5-mm vertical incision was made only in the skin to avoid nerve injuries. The incision was deepened with a blunt mosquito clamp. Then, a blunt obturator was inserted perpendicular to the skin. The obturator was passed through and advanced to tent up the lateral skin, by gliding on the plantar fascia with the tip of the trocar. By palpation, care was taken to ensure that the obturator was dorsal to the fascia. A 5-mm vertical skin incision was made over the tip of the obturator, which was brought out through the skin on the lateral aspect of the heel. The arthroscope cannula was then inserted over the trocar tip and was advanced to the midcalcaneal point. The obturator was removed, and the 2.7-mm, 30° arthroscope was introduced from the lateral portal and the inflow line was connected to the cannula.
We used an infusion pump with the pump pressure set at 50 mm Hg to maintain optimal visualization. A small amount of the flexor digitorum brevis muscle was excised with the 2.9-mm full-radius shaver introduced from the medial portal to clear the working space (Video 1). Once the plantar fascia was visible, we observed a partial tear on its dorsal surface (i.e., frayed or fragmented fiber), which was debrided with the shaver and VAPR device (DePuy Mitek, Westwood, MA) to create healthy tissue margins. The medial half of the planter fascia was incised with the VAPR device and a small basket punch (Fig 2). When the plantar fascia was released, a yellow fluid flowed out and the cyst cavity was shown through the incised plantar fascia. At this time, the 30° arthroscope was switched for a 70° arthroscope. The cyst wall was sampled for histopathologic analysis and was debrided until surrounding fat tissue could be seen (Fig 3). All portals were sutured with No. 5-0 nylon, the pneumatic tourniquet was released, and a compressive dressing was placed on the foot.
Fig 2.

With the surgeon viewing from the lateral portal with the 2.7-mm, 30° arthroscope, the medial half of the plantar fascia is released.
Fig 3.

The bursal cavity is shown through the incised plantar fascia, with the surgeon viewing from the lateral portal with the 70° arthroscope. The cyst is debrided until surrounding fat tissue can be seen.
Full weight bearing and gait were allowed 3 hours after the surgery. Histologic examination showed the cystic lesion to be composed of hyalinized connective tissue (Fig 4), which appeared to be part of the subcalcaneal bursa. A diagnosis of a subcalcaneal bursitis with plantar fasciitis was made based on both the operative and histologic findings.
Fig 4.
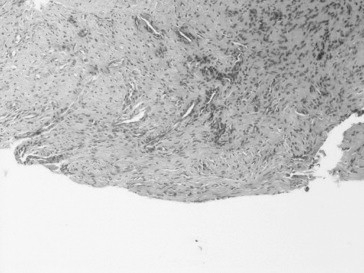
Histologic section shows the cystic lesion to be composed of hyalinized connective tissue, which appeared to be part of the subcalcaneal bursa (H&E stain, original magnification ×200.)
Preoperative pain was relieved shortly after surgery, and range of motion of the foot was maintained. Five months later, an MRI evaluation confirmed that the subcalcaneal mass had disappeared (Fig 5). At the 13-month follow-up examination, the patient had achieved complete resolution of heel pain without a recurrence of the mass (confirmed by MRI) and continued to maintain full range of motion (dorsiflexion, 10°; plantar flexion, 60°). The Japanese Society for Surgery of the Foot ankle/hindfoot scale improved to 100 (the highest possible score).
Fig 5.

T2-weighted, sagittal image of the MRI study at latest follow-up (13 months after surgery) shows the complete resolution of the heel mass.
Discussion
The plantar fascia is a dense band of fibrous tissue that originates from the medial calcaneal tuberosity, fans out, and inserts into the connective tissue at the base of the proximal phalanges of the 5 digits. The plantar fat pad is a multilobular fatty mass, which is thought to be an important supportive structure of the hindfoot. The subcalcaneal bursa lies between the plantar fascia and the plantar fat pad. Plantar fasciitis is 1 of the most common causes of heel pain in adults; however, several other conditions (such as peripheral nerve entrapment, fat pad degeneration, rheumatoid nodule beneath the calcaneus, calcaneal stress fracture, or subcalcaneal bursitis) may cause plantar heel pain or coexist.4
This case suggests that a subcalcaneal bursitis may occur in conjunction with plantar fasciitis and vice versa. Degeneration of the plantar fascia may be related to the development of subcalcaneal bursitis. Plantar fasciitis has been shown to be related to the degeneration of the plantar fascia. Mechanical overload and excessive strain are thought to produce microtears of the plantar fascia, resulting in an inflammatory response and eventual degeneration.9 Histologic analysis of the resected specimen from a patient with plantar fasciitis has shown that there are chronic degenerative changes, such as myxoid degeneration, necrosis of fibroblasts, chondroid metaplasia, angiofibroblastic proliferation, and collagen degeneration.10
In this case we identified degenerative changes of the plantar fascia, which may also be related to the pathogenesis of subcalcaneal bursitis. On the other hand, subcalcaneal bursitis is associated with fat pad atrophy in many cases, inducing loss of the cushioning effect, which is thought to be responsible for the development of plantar fasciitis.4 Open excision of the bursa may increase the risk of fibrosis of the fat pad, leading to further loss of the cushioning effect. The arthroscopic resection appeared to minimize these complications.
Recently, an arthroscopic technique for plantar fascia release has gained popularity and has been shown to be effective in cases in which there is no need for Baxter nerve decompression.11-15 The arthroscopic approach for the plantar fascia includes either a superficial fascial dry technique (without arthroscopic fluid lavage), by use of a slotted or transparent cannula similar to the arthroscopic carpal tunnel release (the arthroscope is located between the skin and the fascia),11-13 or a deep fascial technique with arthroscopic fluid lavage (the arthroscope is located deep in the fascia).14,15 Komatsu et al.15 reported that the deep fascial approach for plantar fasciitis allows a wide visual field and working space. In our case we used the deep fascial approach, which showed a degenerative tear of the plantar fascia, after dissection of the subcalcaneal bursa simultaneously. We believe that the superficial fascial approach is not suitable (or may be impossible) for access to the subcalcaneal bursa because of the limited visual field and the working space.
The optimal amount of plantar fascia to be released is still under debate.4 Recent clinical and biological studies suggest that plantar fasciotomy, particularly complete fasciotomy, may lead to loss of stability of the medial longitudinal arch, resulting in an excessively pronated foot and abnormal gait.16-18 Although the appropriate amount remains controversial and controlling and ensuring the exact amount of partial fasciotomy is difficult,19 complete release of the plantar fascia is not recommended.4,13,17
The advantages of the described arthroscopic approach over traditional open surgery include precise detection of the lesion, less scarring of the skin over the weight-bearing area and the fat pad, immediate full weight bearing, rapid recovery, minimal dissection of soft tissue, and prevention of potential wound complications. However, there are several potential complications associated with the arthroscopic approach, such as fluid extravasation, incomplete fascial release, cutaneous nerve injury, and persistent portal drainage. Continuous accumulation of fluid may lead to compartment syndrome. Another concern is the proximity of the cutaneous nerves to the portals; the first branch of the lateral plantar nerve (Baxter nerve),15 which passes directly over the medial process of the calcaneal tuberosity, is at the greatest risk. Therefore the skin incision should not extend into the subcutaneous fat (“nick-and-spread” technique). Furthermore, it is difficult to observe the Baxter nerve by arthroscopy.20,21 If entrapment of the first branch of the lateral plantar nerve is suspected (e.g., signs of tenderness and/or Tinel-like sign at the proximal level of the abductor hallucis muscle, nocturnal burning pain, and numbness), the arthroscopic approach should not be used.4,9
Footnotes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
Supplementary Data
The arthroscope is placed between the calcaneus and the plantar fascia. With the surgeon viewing from the lateral portal and working from the medial portal, a small amount of the flexor digitorum brevis muscle is excised with the 2.9-mm full-radius shaver. The dorsal surface of the degenerative plantar fascia is debrided, and the medial half of the plantar fascia is released, followed by debridement of the subcalcaneal bursal cavity through the incised plantar fascia.
References
- 1.Crawford F., Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. 2003:CD000416. doi: 10.1002/14651858.CD000416. [DOI] [PubMed] [Google Scholar]
- 2.Gill L.H., Kiebzak G.M. Outcome of nonsurgical treatment for plantar fasciitis. Foot Ankle Int. 1996;17:527–532. doi: 10.1177/107110079601700903. (published erratum appears in Foot Ankle Int 1996;17:722) [DOI] [PubMed] [Google Scholar]
- 3.Wolgin M., Cook C., Graham C., Mauldin D. Conservative treatment of plantar heel pain: Long-term follow-up. Foot Ankle Int. 1994;15:97–102. doi: 10.1177/107110079401500303. [DOI] [PubMed] [Google Scholar]
- 4.Hossain M., Makwana N. “Not plantar fasciitis”: The differential diagnosis and management of heel pain syndrome. Orthop Trauma. 2011;25:198–206. [Google Scholar]
- 5.Kinley S., Frascone S., Calderone D., Wertheimer S.J., Squire M.A., Wiseman F.A. Arthroscopic plantar fasciotomy versus traditional heel spur surgery: A prospective study. J Foot Ankle Surg. 1993;32:595–603. [PubMed] [Google Scholar]
- 6.Tomczak R.L., Haverstock B.D. A retrospective comparison of arthroscopic plantar fasciotomy to open plantar fasciotomy with heel spur resection for chronic plantar fasciitis/heel spur syndrome. J Foot Ankle Surg. 1995;34:305–311. doi: 10.1016/S1067-2516(09)80065-3. [DOI] [PubMed] [Google Scholar]
- 7.Ogilvie-Harris D.J., Gilbart M. Arthroscopic bursal resection: The olecranon bursa and prepatellar bursa. Arthroscopy. 2000;16:249–253. doi: 10.1016/s0749-8063(00)90048-3. [DOI] [PubMed] [Google Scholar]
- 8.Yamakado K. Dissecting a popliteal cyst after failed unicompartmental knee arthroplasty. Arthroscopy. 2002;18:1024–1028. doi: 10.1053/jars.2002.36485. [DOI] [PubMed] [Google Scholar]
- 9.League A.C. Current concepts review: Plantar fasciitis. Foot Ankle Int. 2008;29:358–366. doi: 10.3113/FAI.2008.0358. [DOI] [PubMed] [Google Scholar]
- 10.Lemont H., Ammirati K.M., Usen N. Plantar fasciitis: A degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93:234–237. doi: 10.7547/87507315-93-3-234. [DOI] [PubMed] [Google Scholar]
- 11.Ogilvie-Harris D.J., Lobo J. Arthroscopic plantar fascia release. Arthroscopy. 2000;16:290–298. doi: 10.1016/s0749-8063(00)90053-7. [DOI] [PubMed] [Google Scholar]
- 12.O'Malley M.J., Page A., Cook R. Arthroscopic plantar fasciotomy for chronic heel pain. Foot Ankle Int. 2000;21:505–510. doi: 10.1177/107110070002100610. [DOI] [PubMed] [Google Scholar]
- 13.Bazaz R., Ferkel R.D. Results of arthroscopic plantar fascia release. Foot Ankle Int. 2007;28:549–556. doi: 10.3113/FAI.2007.0549. [DOI] [PubMed] [Google Scholar]
- 14.Blanco C.E., Leon H.O., Guthrie T.B. Arthroscopic treatment of calcaneal spur syndrome: A comprehensive technique. Arthroscopy. 2001;17:517–522. doi: 10.1053/jars.2001.24065. [DOI] [PubMed] [Google Scholar]
- 15.Komatsu F., Takao M., Innami K., Miyamoto W., Matsushita T. Arthroscopic surgery for plantar fasciitis: Application of a deep-fascial approach. Arthroscopy. 2011;27:1105–1109. doi: 10.1016/j.arthro.2011.02.037. [DOI] [PubMed] [Google Scholar]
- 16.Tweed J.L., Barnes M.R., Allen M.J., Campbell J.A. Biomechanical consequences of total plantar fasciotomy: A review of the literature. J Am Podiatr Med Assoc. 2009;99:422–430. doi: 10.7547/0990422. [DOI] [PubMed] [Google Scholar]
- 17.Cheung J.T., An K.N., Zhang M. Consequences of partial and total plantar fascia release: A finite element study. Foot Ankle Int. 2006;27:125–132. doi: 10.1177/107110070602700210. [DOI] [PubMed] [Google Scholar]
- 18.Ward E.D., Smith K.M., Cocheba J.R., Patterson P.E., Phillips R.D. In vivo forces in the plantar fascia during the stance phase of gait: Sequential release of the plantar fascia. J Am Podiatr Med Assoc. 2003;93:429–442. doi: 10.7547/87507315-93-6-429. [DOI] [PubMed] [Google Scholar]
- 19.Hawkins B.J., Langermen R.J., Jr., Gibbons T., Calhoun J.H. An anatomic analysis of endoscopic plantar fascia release. Foot Ankle Int. 1995;16:552–558. doi: 10.1177/107110079501600907. [DOI] [PubMed] [Google Scholar]
- 20.Lui T.H. Arthroscopic decompression of the first branch of the lateral plantar nerve. Arch Orthop Trauma Surg. 2007;127:859–861. doi: 10.1007/s00402-007-0380-1. [DOI] [PubMed] [Google Scholar]
- 21.Chan L.K., Lui T.H., Chan K.B. Anatomy of the portal tract for arthroscopic decompression of the first branch of the lateral plantar nerve. Arthroscopy. 2008;24:1284–1288. doi: 10.1016/j.arthro.2008.06.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The arthroscope is placed between the calcaneus and the plantar fascia. With the surgeon viewing from the lateral portal and working from the medial portal, a small amount of the flexor digitorum brevis muscle is excised with the 2.9-mm full-radius shaver. The dorsal surface of the degenerative plantar fascia is debrided, and the medial half of the plantar fascia is released, followed by debridement of the subcalcaneal bursal cavity through the incised plantar fascia.


