Abstract
Detailed anatomic dissections of the deep medial knee retinaculum have shown a consistent prominent anatomic structure extending from the distal deep quadriceps tendon to the adductor tubercle region, forming a distinct medial quadriceps tendon–femoral ligament (MQTFL). Reconstruction of this anatomic structure has yielded consistent medial stabilization of the patellofemoral joint without drilling into the patella over more than 3 years in patients with recurrent patella instability and dislocation. Results are similar to those of MPFL reconstruction but with reduced risk of patella fracture, a known and serious complication of MPFL reconstruction. The reconstruction graft is secured at the anatomic femoral origin of the MQTFL and brought under the vastus medialis such that it may be woven and attached to the deep distal medial quadriceps tendon to provide a secure, reliable reproduction of the MQTFL and excellent stabilization of the patellofemoral joint without risk of patella fracture.
Currently accepted medial patellofemoral ligament (MPFL) reconstruction techniques require transosseous patella drilling or bone tunnels for suture anchor placement.1,2 These fixation methods can create a stress riser within the patella, leading to reported cases of iatrogenic patella fracture (Fig 1), a devastating postoperative complication.3,4 Parikh and Wall3 recently published a series of 5 patella fractures after MPFL reconstruction using transosseous patella fixation, highlighting this potential catastrophic complication of intrapatellar fixation. Tanaka et al.4 have reviewed the literature on patella fracture after MPFL reconstruction. Bollier et al.5 further noted the unforgiving nature of intraosseous fixation if graft placement is inaccurate. One alternative to intrapatellar fixation is medial retinacular advancement/imbrication,6 but this procedure has limited indications.
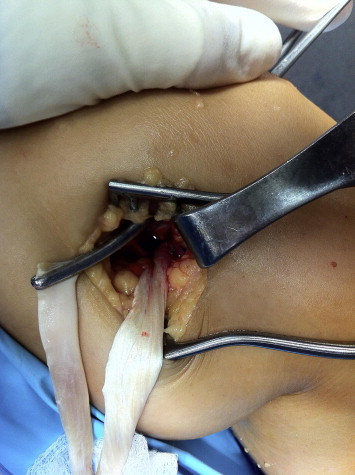
Fig 1.

Patella fracture as a result of MPFL fixation into patella.
We describe an anatomically validated technique for medial patellofemoral stabilization without drilling into the patella. This technique offers an alternative procedure for the surgeon who wishes to avoid patella bone tunnels or intraosseous fixation.
Our dissections of the relevant anatomy in 10 embalmed cadaveric knees in the University of Connecticut Medical School gross anatomy laboratories mirror those previously reported.7-9 During cadaveric dissection, the medial quadriceps mechanism is reflected anteriorly and superiorly to view its posteromedial, undersurface anatomy. Similar to the findings of Mochizuki et al.,7 an anatomically distinct structural component of the medial retinaculum extends from the region just proximal to the MPFL (at the distal anterior extent of the adductor tubercle) and inserts anteriorly into the distal quadriceps tendon (Fig 2). This structure (which we call the medial quadriceps tendon–femoral ligament [MQTFL]) provides a static connection between the medial femur and the extensor mechanism of the anterior knee throughout flexion and extension of the knee (Fig 3).
Fig 2.

MQTFL viewed by reflecting medial retinacular complex anteriorly to see anatomy deep to medialis muscle.
Fig 3.

Anatomically distinct MQTFL in dissected specimen.
Technique for Reconstructing MQTFL
Before an MQTFL reconstruction, patella alignment and patellofemoral dysplasia are evaluated by lateral knee and axial radiography, Q-angle measurement, clinical examination, and selective computed tomography or magnetic resonance imaging. To establish balanced tracking of the patella, a limited lateral release and tibial tubercle medialization or anteromedialization may need to be performed selectively.
We use either semitendinosus autograft or posterior tibial tendon allograft for reconstruction of the MQTFL. The graft is prepared with Ultrabraid (Smith & Nephew, Andover, MA) whipstitches in the end to be used for femoral attachment.
The first skin incision is approximately 2 inches long, extending from the top third of the medial patella border proximally at the level of the distal quadriceps tendon. It is important to make this incision long enough to easily visualize the distal quadriceps and vastus medialis obliquus (VMO) tendons. A 1-cm incision is then placed in the vastus medialis tendon at the level of the proximal patella. Two parallel longitudinal 1.5-cm incisions are then made into the central third of the rectus/intermedius portion of the quadriceps tendon.
The second skin incision is about 2 inches long and is placed by palpating the adductor magnus tendon posteromedially. The skin incision is just proximal to the adductor tubercle. One may use radiographic criteria to help identify this region if needed,10 although we prefer a careful anatomic delineation of the proper femoral socket location using the adductor magnus tendon as a key landmark for the dissection, leading directly to the anatomically critical adductor tubercle from which the MQTFL emanates. The incision extends distally and slightly anteriorly from above the adductor tendon toward the medial epicondyle.
One then exposes the distal adductor tendon and the proximal medial collateral ligament such that the location is confirmed, taking care to avoid risk of injury to the medial infrapatellar branch of the saphenous nerve and the more posteriorly located saphenous nerve. At this point, it is easy to place a guide pin at the distal aspect of the adductor tubercle such that an 8-mm socket will have its proximal edge just at the distal anterior adductor tubercle, the anatomic origin of the MQTFL, immediately above the MPFL (which originates in the sulcus between the adductor tubercle and the medial epicondyle).
An 8-mm socket is then created over the guide pin, 2.5 cm deep. The whipstitched end of the free tendon reconstruction graft is secured into the socket by use of the desired fixation device (Fig 4). We do not advocate any one particular fixation device because there are several excellent alternatives for socket fixation of the MQTFL reconstruction graft on the femoral side.
Fig 4.

Femoral fixation of MQTFL reconstruction graft at anterior distal adductor tubercle.
The surgeon then places a hemostat into the VMO tendon incision and then under the VMO such that the tip then comes out at the level of the bone socket just created (Fig 5). The hemostat grasps the entire free end of the tendon graft and draws it anteriorly, deep to the medialis tendon and thereby out of the medialis obliquus incision at the proximal medial patella (Video 1).
Fig 5.
Hemostat placed deep to the VMO tendon that will be used to draw reconstruction graft anteriorly for fixation into distal quadriceps tendon just above patella.
After cycling of the knee several times, the graft is further secured by drawing it into the slot created by the 2 parallel incisions in the distal quadriceps tendon (Fig 6). By cycling the knee several more times and using an arthroscope in the joint, one may readily determine the proper location and tension for fixation of the graft. The goal is to tension the graft in a manner that maintains the patella tracking centrally in the trochlea without any hint of medial tracking (medial subluxation). Generally, the patella will be slightly lateral in full extension (as is normal) and be drawn promptly by the graft into the central trochlea upon early flexion of the knee. The knee is kept at 30° of flexion, holding the patella in the central trochlea by tensioning the graft and confirming central patella tracking arthroscopically. The graft is marked with methylene blue at this level of tension, and Ultrabraid sutures are placed to lock the graft into the medialis and intermedius tendons. One must then, again, confirm optimal tracking of the patella without any hint of over-tension, in which case sutures must be released and replaced appropriately. With this technique, re-tensioning is relatively easy.
Fig 6.
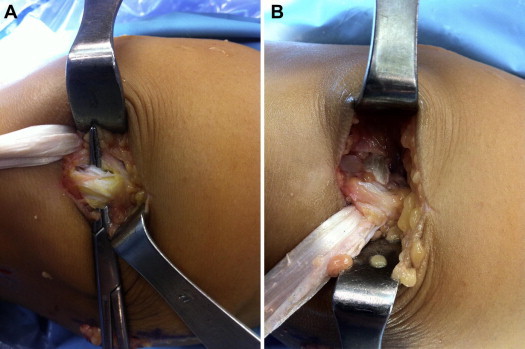
Reconstruction graft is drawn through the VMO tendon and then sutured into a “slot” made by 2 parallel incisions in the distal medial quadriceps tendon. (A) Graft is ready to be pulled into the quadriceps tendon “slot” with a hemostat. (B) Tendon graft has been pulled into the quadriceps tendon slot, reproducing the MQTFL. The graft is then sutured securely in place after tensioning to secure the patella at the precise anatomic center of the trochlea.
The patient is placed in a knee immobilizer after closing and dressing of the wounds. We allow immediate weight bearing with crutches for 6 weeks, at which point the patient starts physical therapy for restoration of function. At the first postoperative visit, the patient is asked to remove the immobilizer and flex the knee to 90° once a day (1 flexion only). Most patients take 1 or 2 weeks to achieve the initial 90° bend. Once physical therapy commences, the patient may begin to resume light daily activity as tolerated but should not return to sports for at least 4 months.
Discussion
Seventeen patients who had MQTFL reconstruction alone (no tibial tubercle transfer) for recurrent patella instability were contacted 1 year or more after surgery. All were stable without recurrence of patella instability. Nine of these patients had undergone MQTFL reconstruction more than 2 years earlier. One patient complained of clicking related to an articular lesion, and 2 patients had ongoing mild discomfort related to patella chondral damage. One patient had been ranked number 2 in the United States in vaulting subsequent to MQTFL reconstruction.
In patients with lateral patella tracking, we correct alignment/tracking of the patella before or at the time of MQTFL reconstruction (usually with medial or anteromedial tibial tubercle transfer).
Patella fracture is a serious complication of MPFL reconstruction. Therefore reconstruction of the MQTFL is a prudent alternative to MPFL reconstruction in patients with recurrent patella instability needing restoration of medial retinacular support.
This anatomic approach has the distinct advantage of ensuring precise location of the femoral fixation site, whereas radiographic localization carries the risk of inadvertent malpositioning of the graft depending on minor shifts of the imaging device or anatomic variations (Table 1). Our anatomic approach also reduces the risk of patella fracture essentially to nil—a major advantage in view of the recent reports of patella fracture from several centers. We are seeing comparable stability results to MPFL reconstruction and therefore no longer attach grafts to the patella itself. MQTFL reconstruction is anatomically correct and effective.
Table 1.
Tips, Pearls, Contraindications, and Pitfalls
| • Tips and pearls |
|
|
|
|
|
| • Contraindications |
|
|
| • Pitfalls |
|
|
|
|
Footnotes
The authors report the following potential conflict of interest or source of funding in relation to this article: J.P.F. is the President of the Patellofemoral Foundation, which receives undirected funding from Smith and Nephew Endoscopy.
Supplementary Data
Method for placing and securing a tendon graft properly for reconstruction of MQTFL.
References
- 1.Christiansen S.E., Jacobsen B.W., Lund B., Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24:82–87. doi: 10.1016/j.arthro.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Ellera Gomes J.L., Stigler Marczyk L.R., César de César P., Jungblut C.F. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: A follow-up study. Arthroscopy. 2004;20:147–151. doi: 10.1016/j.arthro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 3.Parikh S.N., Wall E.J. Patellar fracture after medial patellofemoral ligament surgery: A report of five cases. J Bone Joint Surg Am. 2011;93 doi: 10.2106/JBJS.J.01558. e97(1-8) [DOI] [PubMed] [Google Scholar]
- 4.Tanaka M.J., Bollier M.J., Andrish J.T., Fulkerson J.P., Cosgarea A.J. Complications of medial patellofemoral ligament reconstruction: Common technical errors and factors for success: AAOS Exhibit Selection. J Bone Joint Surg Am. 2012;94:e871–e878. doi: 10.2106/JBJS.K.01449. [DOI] [PubMed] [Google Scholar]
- 5.Bollier M., Fulkerson J., Cosgarea A., Tanaka M. Technical failure of MPFL reconstruction. Arthroscopy. 2011;27:1153–1159. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 6.Bicos J., Fulkerson J., Amis A. Current concepts review: The medial patellofemoral ligament. Am J Sports Med. 2007;35:484–492. doi: 10.1177/0363546507299237. [DOI] [PubMed] [Google Scholar]
- 7.Mochizuki T., Nimura A., Tateishi T., Yamaguchi K., Muneta T., Akita K. A, Tateishi T, Yamaguchi K, Muneta T, Akita K. Anatomic study of the attachment of the medial patellofemoral ligament and its characteristic relationships to the vastus intermedius. Knee Surg Sports Traumatol Arthrosc. 2013;21:305–310. doi: 10.1007/s00167-012-1993-7. [DOI] [PubMed] [Google Scholar]
- 8.Kang H.J., Wang F., Chen B.C., Su Y.L., Zhang Z.C., Yan C.B. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18:1511–1516. doi: 10.1007/s00167-010-1090-8. [DOI] [PubMed] [Google Scholar]
- 9.Waligora A.C., Johanson N.A., Hirsch B.E. Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clin Orthop Relat Res. 2009;467:297–306. doi: 10.1007/s11999-009-1052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Method for placing and securing a tendon graft properly for reconstruction of MQTFL.


