Abstract
We introduce an anatomic reconstruction technique for the medial patellofemoral ligament using a free hamstring autograft in skeletally immature patients. We dock the 2 ends of the graft in the superior-medial patella using sockets and secure the femoral graft attachment in a socket tunnel distal to the physis. This technique minimizes the risk of injury to the growth plate and still enables accurate and successful anatomic positioning of the hamstring autograft.
Patellar dislocation is commonly diagnosed in children and adolescents and often results in patellofemoral instability. The initial event of dislocation is frequently traumatic in origin, often causing a tear in the medial patellofemoral ligament (MPFL). In a previous study, Kepler et al.1 were able to detect that in 44 children and adolescents with acute primary MPFL disruption, injury occurred at the patellar insertion in 61% of cases, at the femoral insertion in 12%, and at both sites in 12%. Currently, treatment after the first dislocation is a trial of conservative therapy focusing on quadriceps strengthening and improving core stability. If conservative management is ineffective and recurrent episodes of patellar dislocation occur, surgical reconstruction of the MPFL is recommended.
However, surgical treatment in skeletally immature patients is still a subject of discussion, and various techniques have been described.2,3 Although ligamentous reconstruction in adults has proven to be efficient and is well described in the literature, a limited number of reports of MPFL reconstruction in children with open growth plates is available. Special attention should be focused on the anatomic relation of the MPFL insertion around the distal femoral physis, because the distal femoral physis contributes up to 70% of growth of the femur and 37% of overall lower limb growth.4
We report an MPFL reconstruction technique using a free hamstring autograft, docking it distally to the distal femoral epiphysis and by 2 sockets at the patella (Fig 1). This modified technique avoids the distal femoral growth plate, minimizes the risk of injury, and allows a safe, effective, and anatomic treatment option (Tables 1 and 2).
Fig 1.
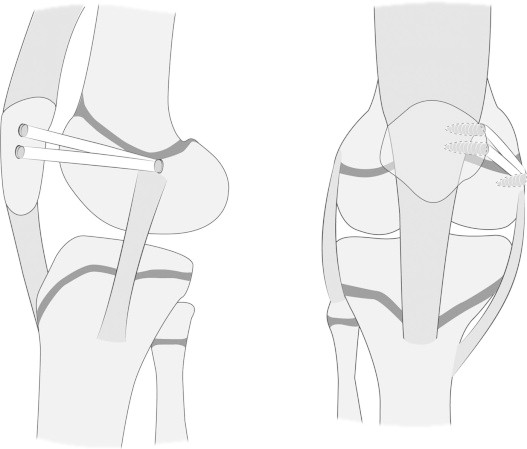
Modified MPFL reconstruction technique. We dock the 2 ends of the graft in the superior-medial patella using partial socket tunnels, resulting in placement of the femoral attachment in a socket tunnel distal to the physis.
Table 1.
Sequence of Steps for MPFL Reconstruction
| 1. Perform diagnostic arthroscopy and treatment of chondral injury. |
| 2. Harvest the ipsilateral hamstring tendon: semitendinosus or gracilis. |
| 3. Expose the area of the medial epicondyle of the distal femur in flexion. |
| 4. Use a guidewire under fluoroscopy to identify the exact position of the femoral socket and create a socket distal to the distal femoral growth plate with a typical diameter of 6 mm and depth of 15 to 20 mm. |
| 5. Expose the superior-medial margin of the patella. |
| 6. Use a guidewire and reamer to create 2 socket tunnels approximately 15 mm long and 4.5 mm diameter; in smaller children, only 1 socket is used. |
| 7. Create a soft-tissue space between the fascia and synovium linking the patella and femoral sockets. |
| 8. Carefully measure the distance between the femoral and patellar sockets; this distance should be measured in 30° of flexion, with patella held in a reduced position on the trochlea. |
| 9. Prepare a double limb graft typically measuring the distance between the femoral and patellar sockets, adding 15 mm for each socket, usually adding up to a final length of 85 to 100 mm. |
| 10. Fix the graft on the femur with a tenodesis screw measuring 6.25 to 7 mm in diameter; secure the free ends with a No. 2-0 suture loop. |
| 11. Using passing sutures, pass the graft through the previously prepared soft-tissue space to the superior half of the patella. |
| 12. Dock the free ends of the graft into the 2 sockets at the patella with two 4.75-mm tenodesis screws while the knee is in 30° of flexion. |
Table 2.
Advantages and Disadvantages
| Advantages |
| Anatomic placement is performed below the distal femoral growth plate of the graft. |
| The technique avoids long tunnels. |
| Aperture fixation is used, which may be stronger than fixation with soft tissue alone. |
| The effect of longitudinal growth on the isometrics of the reconstructed graft is minimized. |
| The hamstring tendon allows robust reconstruction of the MPFL, which is stronger than the original MPFL. |
| Small incisions are required. |
| Early range of motion and weight bearing are allowed. |
| Disadvantages |
| Precise positioning and assessment of graft length are required before graft fixation. |
| Intraoperative fluoroscopy is required. |
Surgical Technique
This retrospective review was approved by the Institutional Review Board of the Hospital for Special Surgery.
Harvesting Hamstring Autograft
After completion of diagnostic arthroscopy to rule out intra-articular lesions, the ipsilateral gracilis or semitendinosus tendon is harvested with a hamstring tendon stripper, taking caution to avoid stripping of the periosteum of the proximal tibial tubercle and growth plate. The graft length is estimated by measuring the distance of the medial border of the reduced patella to the femoral insertion site, adding a total of 25 to 30 mm of length to allow the graft to be fixed within the bony sockets at each end. The total length of the tendon should be 170 to 200 mm to allow sufficient length for reconstruction of the MPFL. The tendon is prepared as a double-link graft typically measuring 85 to 100 mm, depending on the size and age of the individual patient (Fig 2).
Fig 2.

Preparation of a double link graft typically measuring 85 to 100 mm.
Fixation of Graft at Femoral Insertion Site
In 30° of flexion, a 1- to 2-cm longitudinal skin incision is made in the area of the medial epicondyle and the adductor tubercle (Video 1). By use of fluoroscopic imaging, a guidewire is placed first on the anteroposterior image 5 to 7 mm distal to the medial femoral growth plate and then on a true lateral view, the starting point for the socket should be placed in line with the posterior cortex of the femur as described by Schottle et al.5 (Fig 3). It should be noted that on the lateral radiograph (Fig 3B), the femoral insertion point may falsely appear to be proximal to the physis because of the nonlinear structure of the distal femoral growth plate. Therefore accurate assessment of the location of the femoral socket is essential.1 The socket is typically created with a diameter of 6.00 mm to a depth of 15 to 20 mm. The direction of the drill hole should angulate slightly away from the femoral physis and towards the articular surface. The previously harvested double-bundled autograft is then secured with a tenodesis screw measuring 6.25 × 20 mm. The 2 free ends are passed subcutaneously beneath the fascia but superficial to the joint capsule.
Fig 3.
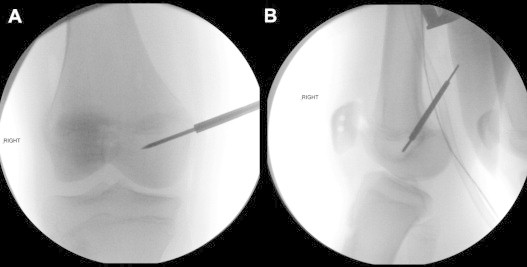
MPFL reconstruction in a skeletally immature patient. Intraoperatively, a guidewire is placed (A) first on the anteroposterior image 5 to 7 mm distal to the medial femoral growth plate and then (B) onto the lateral view in line with the posterior cortex of the diaphysis of the femur.
Fixation of Graft at Patellar Insertion Site
At this point, attention is focused on the patella, and a 2-cm anterior skin incision is made over the superior-medial margin of the patella. A small periosteal flap is cut to expose the medial border of the patella. By use of a guidewire and 4.5-mm reamer, 2 socket tunnels about 15 mm long are drilled in the patella. These sockets do not completely cross the patella. The 2 free ends are passed subcutaneously beneath the fascia to the superior half of the patella. With the patella reduced into the trochlea at 30° of flexion, the appropriate length of the graft is determined. Before screw fixation, the graft length and isometry should be evaluated by assessing patellar tracking and range of motion. With the patella reduced into the trochlea, the 2 ends of the graft are then docked in the bony patellar sockets with two 4.75-mm tenodesis screws (Arthrex, Naples, FL). In younger children, aged younger than 10 years, 1 fixation point and a single-bundle reconstruction at the patella are often used.
Postoperatively, we recommend a knee brace locked in extension and weight bearing as tolerated with crutches until pain and swelling have resolved. Use of the brace is continued until the quadriceps strength returns to grade 4. Early range of motion, by use of physical therapy and continuous passive motion, is prescribed.
Discussion
Anatomic reconstruction of the MPFL is essential to restore biomechanical kinematics of the knee. Several techniques to reconstruct the MPFL have been advocated by various authors.2,3 The MPFL insertion on the medial femur has been described as being distal to the adductor tendon insertion and proximal to the femoral insertion of the medial collateral ligament, which is in very close proximity to the medial aspect of the distal femoral growth plate.1,5-7 Shea et al.,8 in an indirect radiographic study using lateral radiographs, reported that the insertion of the MPFL was 2 to 5 mm proximal to the distal femoral physis. Kepler et al.,1 as well as Balcarek et al.,9 have shown that the zone of insertion is just distal to the distal femoral physis. It is essential to consider the distal femoral anatomy to prevent damage to the physis and subsequent growth disturbance during MPFL reconstruction. Bone fixation proximal to the distal femoral physis may result in proximal migration of the femoral insertion of the MPFL, causing excessive graft tension, loss of graft isometry, and loss of knee motion.10 Therefore our preferred method is to dock the 2 ends of the graft in the superior-medial patella using partial socket tunnels and to place the femoral socket tunnel distal to the physis.
From 2009 to 2012, we performed the described reconstruction in 41 patients, of whom 23 were skeletally immature. No cases of distal femoral growth plate disturbance were observed in this cohort, with an average follow-up of 16 months. Excellent stability was restored as no subsequent dislocation events were reported. At short-term follow-up, all patients had significant improvement in patellar instability, with no subsequent dislocation events.
We believe that our technique has advantages in relation to previously published approaches to reconstruct the MPFL, minimizing the risk of iatrogenic injury to the distal femoral growth plate in skeletally immature patients and resulting in a surgically sound and anatomic reconstruction. Relative contraindications for this procedure are severe osteopenia or inability to participate in postoperative physical therapy. This surgical approach may not be sufficient in cases with severe lower extremity deformity such as genu valgum or severe rotational malalignment.
Anatomic reconstruction of the MPFL is regarded as a safe treatment for patellofemoral instability in children and adolescents. MPFL reconstruction with hamstring autograft may reliably be performed in children and adolescents with patellar instability with open growth plates. However, careful intraoperative fluoroscopic guidance is required to avoid injury to the open distal femoral growth plate in skeletally immature patients. We recommend this surgical technique for symptomatic children and adolescents with recurrent patellar dislocation.
Footnotes
Supported by the Paracelsus Medical University Research Fund (S-12/01/003-LAD). The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
MPFL reconstruction using hamstring autograft in children and adolescents.
References
- 1.Kepler C.K., Bogner E.A., Hammoud S., Malcolmson G., Potter H.G., Green D.W. Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med. 2011;39:1444–1449. doi: 10.1177/0363546510397174. [DOI] [PubMed] [Google Scholar]
- 2.Weeks K.D., Fabricant P.D., Ladenhauf H.N., Green D.W. Surgical options for patellar stabilization in the skeletally immature patient. Sports Med Arthrosc. 2012;20:82–88. [PubMed] [Google Scholar]
- 3.Nelitz M., Dreyhaupt J., Reichel H., Woelfle J., Lippacher S. Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates. Am J Sports Med. 2013;41:58–63. doi: 10.1177/0363546512463683. [DOI] [PubMed] [Google Scholar]
- 4.Dimeglio A. Growth in pediatric orthopaedics. J Pediatr Orthop. 2001;21:549–555. [PubMed] [Google Scholar]
- 5.Schottle P.B., Fucentese S.F., Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13:516–521. doi: 10.1007/s00167-005-0659-0. [DOI] [PubMed] [Google Scholar]
- 6.Baldwin J.L. The anatomy of the medial patellofemoral ligament. Am J Sports Med. 2009;37:2355–2361. doi: 10.1177/0363546509339909. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade R.F., Engebretsen A.H., Ly T.V., Johansen S., Wentorf F.A., Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 8.Shea K.G., Grimm N.L., Belzer J., Burks R.T., Pfeiffer R. The relation of the femoral physis and the medial patellofemoral ligament. Arthroscopy. 2010;26:1083–1087. doi: 10.1016/j.arthro.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 9.Balcarek P., Ammon J., Frosch S. Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy. 2010;26:926–935. doi: 10.1016/j.arthro.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Nelitz M., Dornacher D., Dreyhaupt J., Reichel H., Lippacher S. The relation of the distal femoral physis and the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19:2067–2071. doi: 10.1007/s00167-011-1548-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
MPFL reconstruction using hamstring autograft in children and adolescents.


