Abstract
Background
Medical students are often afforded the privilege of counselling patients. In the past resources were limited to pen and paper or anatomic models. The evolution of mobile applications allows for limitless access to resources that facilitate bedside patient education.
Objectives
To evaluate the utility of six applications in patient education and promote awareness of implementing mobile resources in clinical care.
Methods
Six medical students rotating on various clerkships evaluated a total of six mobile applications. Strengths, limitations, and suggested uses in clinical care were identified. Applications included MeditoonsTM, VisiblePatientTM, DrawMDTM, CardioTeachTM, Visual AnatomyTM, and 360° Patient Education SuiteTM. Data was generated from narrative responses supplied by each student during their evaluation period.
Results
Bedside teaching was enhanced by professional illustrations and animations depicting anatomy and pathophysiology. Impromptu teaching was facilitated, as resources were conveniently available on a student’s smartphone or tablet. The ability to annotate and modify images and subsequently email to patients was an extraordinary improvement in provider-patient communication. Universal limitations included small smartphone screens and the novelty of new technology.
Discussion
Mobile applications have the potential to greatly enhance patient education and simultaneously build rapport. Endless opportunities exist for their integration in clinical practice, particularly for new diagnoses, consent for procedures, and at time of discharge. Providers should be encouraged to try new applications and utilize them with patients.
Keywords: Application, mobile health, electronics, smartphone, patient education
1. Background
Patient counselling is a privilege afforded to medical students as they learn how to address not only the physiologic complications of a disease, but also the chief concerns of their patients. In the past students have used whatever resources they had often limited to pen and paper, their knowledge of anatomy, and artistic skills to help patients understand what brought them into the hospital and what might keep them well in the future.
Tools for patient education and physician-patient communication have been constantly evolving. Since the 1950s, anatomic models have been a cornerstone of patient education [1], offering visual aids to explain disease processes and therapeutic interventions. The first example was Merck, Sharp & Dohme’s Diuril ManTM, a translucent figure demonstrating the interplay of the heart, vasculature, and kidneys in hypertension [1]. The statue could be inverted to drain fluid out of the body and into its hollow base as the patient learned how the kidneys mimicked this task in their own bodies. The Diuril ManTM became the inspiration for countless future anatomic models gifted to physicians by healthcare companies over subsequent 60 years. While greatly facilitating patient education, these models also became marketing tools of complex business interests [1].
Mobile applications (“apps”) allow healthcare providers to access limitless resources to facilitate patient education at the bedside. While there exist a multitude of healthcare applications designed for patients to utilize at home [2, 3], we focus on resources a medical provider can use when educating and counseling patients. We use the terms “patient education” and “bedside teaching” to refer specifically to this process. Additionally, while potentially suitable for any member of the healthcare team, we focus on the perspective of the medical student. Here we review six mobile applications on three devices to explore their utility in facilitating bedside patient education.
2. Methods
The authors of this study formed the evaluation cohort, which consisted of six third-year medical students rotating in various specialties at a large academic medical center. Participants were self-selected for the project via an email to the medical school class, and consisted of five males and one female between the ages of twenty-four and twenty-eight. No computer science or specific “technosaavy” skills were required other than expressing an interest in the topic, and none of the evaluators had any formal training in information technology. Four participants used Apple iOS (two used iPhones and two used iPads) and two used the Android operating system on smartphones. Evaluation consisted of one week of exclusive use of pen and paper to illustrate anatomy, pathophysiology, and planned interventions for patients encountered in a predominately inpatient clinical setting. This was performed to establish a non-technological benchmark and provide context in which to assess the strengths and limitations of the applications. Two weeks were subsequently devoted to each of two applications on an evaluator’s specified device, with each individual using only one specified application at a time. During this period, students used their designated applications in bedside teaching and, if necessary, reverted to pen and paper if the application’s functionality was insufficient to accomplish the task at hand. A summary of the applications evaluated is provided in ► Table 1.
Table 1.
Overview of Applications
| Application | Device | Developer | Description |
|---|---|---|---|
| Meditoons™ | iPhone | Pearlswan Communications, LLC | Animations of pathophysiology of commopn GI conditions |
| Visible Patient™ | iPhone | IRCAD | Provides an array of actual radiologic studies from anonymous patients |
| DrawMD™ | iPad | Visible Health | Series of apps by specialty providing professional anatomic illustrations and tools for user modification |
| CardioTeach™ | iPad | Boston Scientific | Short interactive presentations on cardiac pathophysiology |
| Visual Anatomy | Android | Education Mobile | Searchable interactive anatomy modules |
| 360° Patient Education Suite™ | Android | Incendant LLC | Broad scope of modifiable images and educational videos for patients |
Applications were identified by browsing the Medical and Health categories as well as searching for terms such as “patient education” in iTunesTM and Google PlayTM stores. Two applications were selected for each device based on their description, and firsthand impressions of potential value for patient education. Only free applications were evaluated, though some applications also had a paid version available with additional features discussed in below.
Applications evaluated on the iPhone included MeditoonsTM (version 2.0) [4] and Visible PatientTM (version 0.3) [5]. MeditoonsTM is an application developed by Pearlswan Communications that provides animations of normal anatomy and function in addition to common disease processes of the gastrointestinal tract. Visible PatientTM is distributed by Research Institute Against Digestive Cancer (IRCAD) and offers a set of three-dimensional virtual anatomic models reconstructed from medical images of anonymous patients.
Applications utilized on the iPad included DrawMDTM (version 2.6.575) [6] and CardioTeachTM (version 2.0) [7]. DrawMDTM is marketed by Visible Health and is a series of applications by specialty that provides professional illustrations of normal anatomy as templates which can be modified and distributed to patients. CardioTeachTM is developed by Boston Scientific and provides anatomic images, animations, and educational text explaining cardiac physiology and common pathologies.
Android applications included Visual AnatomyTM (version 3.1) [8] and 360° Patient Education SuiteTM (version 1.10) [9]. Visual AnatomyTM is distributed by Education Mobile and provides labeled anatomy images with interactive content. Incendant’s 360° Patient Education SuiteTM is an application that provides modifiable anatomic images, educational videos, and information on procedures and medications.
Data was collected from narrative responses by evaluators on each modality’s overall advantages, limitations, and suggested uses for patient education. At the culmination of each application’s evaluation period, all investigators submitted free text assessments for 4 parameters surrounding the application: strengths, shortcomings, ideas for improvement, and suggested clinical uses. Feedback was aggregated at the culmination of the study, and the sentiments of all responses are appropriately represented.
3. Results
3.1 Pen and Paper: our benchmark modality
Strengths
Paper and writing utensils are easily available in any clinical setting, and in our institution dry-erase boards with markers are mounted in each inpatient hospital room. Access to this simple modality is a clear advantage and disposability allowed students to leave the patient with the diagram they created together. Simplicity is another consideration, as one evaluator noted:
“With any other modality, the patient could easily be overwhelmed by irrelevant aspects of a complex image, but here they only focus on what I am drawing.”
The value of provider-patient communication cannot be overstated. One student’s reflection beautifully illustrated this impact during our study:
“There is no question that patients often have an unquenchable thirst to understand what it is that is going on or going wrong in their bodies. I often saw patients carry around for days or even weeks the drawings that physicians had made for them to explain their anatomy or operation.”
Limitations
Individual variations in artistic talent are an obvious limiting factor, as no student felt they consistently had the ability to draw anatomy with adequate detail and clarity. Additional shortcomings included restriction to two-dimensional space, time required to create a desired image, and variations in ability to recall complex anatomy. These limitations provided an opportunity for mobile applications to improve on current techniques of patient education.
3.2 MeditoonsTM (iPhone)
Strengths
MeditoonsTM contains high quality images and animations organized by regions of the digestive system. The format is convenient for explaining related conditions with appropriate differential diagnoses. For example, someone with right upper quadrant pain could view animations within the “Biliary Tree” section including Acute Cholecystitis, Common Duct Stone, or Pancreatic Lesion. Dynamic animations have a clear advantage to static images, demonstrating the progression of pathology from inciting events to development of symptoms or potential complications. One evaluator commented:
“One of my patients was having difficulty understanding how she had been told she had gallstones years ago but they were not causing her any problems until very recently. The animation, which showed gallstones in the gallbladder without any initial obstruction, helped to clarify the sequence of events.”
This application achieved an appropriate balance of detail and simplicity. The clarity and color of the images guided the users to view important structures and processes without becoming distracted by unnecessary detail.
Limitations
This application currently covers only gastrointestinal conditions, specifically diseases of the upper gastrointestinal tract, biliary tree, colon, and anorectum. While it succeeds at describing the few diseases it addresses, this greatly hindered the ability of our evaluators to use it widely during the evaluation period.
None of the animations currently contain narration. This limits their utility for independent patient use, but allows for the provider to explain the pathophysiology, pausing or rewinding to address a patient’s specific concerns. While limited text on the screen does allow patients to follow along to a degree, we experienced confusion on patient’s part due to variable levels of literacy. Ideally a narration would be included that could be muted, promoting physician-patient interaction, but simultaneously allowing the patient to return to the video independently at a later time.
3.3 Visible PatientTM (iPhone)
Strengths
This application creates three-dimensional models of different organ systems based on CT and MRI scans of real anonymous patients. Use of actual radiology scans was considered a strength to the degree that it represented true anatomy, though it was associated with a limitation of quality. Different portions of anatomy could be removed to enhance the focus on a desired region or organ of interest and the ability to rotate and zoom on these models impressively allowed anatomy to be viewed at any angle. This feature was notably missing from many of the applications we used and it enabled our evaluators to better convey three-dimensional anatomic relationships to patients. Additional cases were available for download to provide examples over a wide range of topics.
Limitations
The user interface of this application was the most significant limitation. The organization was less intuitive and the format less aesthetically pleasing than what we observed in other applications. While praised for representing real patient anatomy images were of substantially lower visual quality. One user described:
”The resolution of the different images is very poor. I have trouble interpreting what all of the structures are in each of the images even though I know what they should be, so I can imagine how hard it would be to understand as a layperson to see what is going on in the image.”
We felt that in its current form, the application had limited utility for patient education. Additionally, each image must be downloaded separately, making the process substantially more time consuming and less convenient for impromptu bedside teaching on a topic that may not have yet been downloaded. Though the images are locally stored once downloaded, it would more convenient to have all the data downloaded initially with the application rather than needing to do so in segments.
3.4 DrawMDTM (iPad)
Strengths
DrawMDTM has an impressive series of applications in fields including General Surgery, Cardiology, Urology, Pediatrics, Orthopedics, ENT, Thoracic Surgery, OB/GYN, and Vascular [6]. Each application contains a range of anatomic templates. Alternatively, students could use a blank template or import images from their camera. Images can be modified with “stamps” to reflect pathology, variations in anatomy, or surgical change. One creative student used the camera feature to take a picture of a patient’s coronal CT scan and subsequently added stamps to better demonstrate pathology. While the provider can also draw on the image, these stamps allowed pathology and treatment to be explained with increased clarity, rather than relying on the provider’s ability to illustrate these processes. The provider or patient can insert notes, and even share annotated images via email. One author recalls:
”In a pre-op area, after a patient had been consented for a thyroidectomy, they wanted to know how exactly the complications of hoarseness or hypocalcaemia could occur. To the patient’s satisfaction, the application allowed us to demonstrate the location of the parathyroids and recurrent laryngeal nerve intimate to the thyroid.”
Limitations
The greatest shortcoming to the DrawMDTM series was inability to rotate images, which occasionally impeded users’ ability to fully demonstrate three-dimensional relationships of structures. Lack of animation was also noted specifically in the cardiology application as multiple patients noted a desire to see the heart beating to help them understand their disease. The applications do cover an impressive range of topics, though each individual application has a very narrow scope, making it necessary for a general practitioner or a medical student to use multiple applications.
3.5 CardioTeachTM (iPad)
Strengths
The user interface of this application is excellently tailored for patient education with a logical sequence of information, numerous tabs to quickly navigate topics, and large font that displays beautifully on a tablet-sized screen. In addition to simple anatomic figures, the application contains basic text written at the level of a layperson that explains normal heart function, common arrhythmias, coronary artery disease, and heart failure. The user is able to draw on the page, insert notes, and email the page to a patient for future reference. One evaluator reflected on his experience after using CardioTeachTM:
”One patient who had been transferred to an intensive care unit multiple times for atrial fibrillation commented to me that she ‘had never understood what was going on before’.”
Perhaps the greatest strength of CardioTeachTM is that each presentation on pathophysiology includes a final tab entitled “Living With (Disease).” We found that this section contained extremely important lifestyle considerations and suggestions that unaffected individuals would not be able to anticipate. Even if he was not specifically planning to use this application with a patient, one evaluator claimed that he strongly recommended reviewing these lists with patients at discharge to address any barriers to long-term quality of life.
Limitations
The application was developed by Boston Scientific, and each page contains their company logo and several pages contain links to their website. This could be construed as a potential conflict of interest analogous to drug company gifts, and may not be permissible for use at all institutions. Additionally, there is no ability to zoom or rotate images, which our evaluators noted was especially limiting when describing structural defects or posterior-wall myocardial infarctions due to difficulty demonstrating anatomic relationships. The interactive content present in the application was one of the most valuable features, though it was only available in a few select areas and could be more widely implemented.
3.6 Visual Anatomy-FreeTM (Android)
Strengths
This application includes a multitude of high quality images of gross anatomy. Zooming, panning, and rotating are smoothly incorporated in the application. These are features that were absent in several of the applications we reviewed and function well here to ensure patients can visualize relevant anatomic details even on a small phone screen. The images were also aesthetically pleasing and our evaluators noted that even when zooming in, details were clear to patients. The application also contains interactive features known as “feature points” which provide interesting information about certain structures and physiology in addition to quizzes. In our experience, the greatest value for patient education was as the application’s simple anatomic images.
Limitations
The application ultimately appears to be more valuable for student education with the interactive features describing information highly useful in an anatomy class. The images were high quality at a level of detail beyond what would be appropriate for patient education, ultimately creating overly cluttered images on the Android phone’s small screen. One student recounted:
”It's hard to see the connections of various organs, which is really why I would pull out such an app in the first place (e.g. ‘Your biliary tree normally drains the liver into your intestines, so if we remove part of it, we need another way of connecting your liver to the intestine so that bile can still drain out’). That explanation is impossible to illustrate with this app.”
The added interactive content did not provide additional value for patient education. The application also occasionally froze, interrupting the provider-patient interaction. We used the free version of the application, though an enhanced version, which contains more images, feature points, and covers more content areas, could be purchased for $2.49 [8].
3.7 360° Patient Education SuiteTM (Android)
Strengths
This application has an attractive user interface with a variety of features specifically designed for patient education. The content consists of both anatomic images and videos explaining common conditions, medications, and medical procedures. Students especially valued the ability to modify images and save them for later reference of common conditions to multiple patients. Stepwise processes, for instance the pathogenesis of gallstones causing biliary colic, were clearly delineated and facilitated patient understanding. The application can also send an email with a link to the content, such as videos, covered in the educational session.
Limitations
We used the demo version of this application, though with the purchase of a license, more videos that cover an increased number of conditions can be accessed. Multiple features, including the ability to create and distribute discharge summaries, were potentially of use but were not directly applicable to our evaluators or to their activities educating patients. Certain topics, such as smoking cessation, did not seem well addressed in such a generic format. One evaluator explained:
”I'm not sure a video on smoking cessation is the best approach to patient care as we know, what patients need is motivational counselling that is individualized, not a lecture on the dangers of smoking/benefits of quitting.”
We felt that such a personalized matter was better addressed between a provider and patient in a manner that emphasized the provider’s understanding of the patient’s unique circumstances.
► Table 2 provides an overview of the strengths and limitations of each application.
Table 2.
Strengths and Limitations
| Application | Strengths | Limitations |
|---|---|---|
| Meditoons™ |
|
|
| Visible Patient™ |
|
|
| DrawMD™ |
|
|
| CardioTeach™ |
|
|
| Visual Anatomy™ |
|
|
| 360° Patient Education Suite™ |
|
|
4. Discussion
Medical students are in a unique position to engage in patient education because we are often able to spend more time with our patients than more senior team members. Throughout our evaluation students repeatedly acknowledged the importance of visualization in healing. For many patients this involved putting a face on their disease, and one patient even requested his drawing so he could refer Education to it “when things got tough.” Mobile applications offer the provider an arsenal of valuable tools to utilize at their discretion.
The narrative comments of the evaluators generally focused on ease of use, targeted audience, available and innovative features, overall quality, and limitations. The comments where categorized by their relevance to the above themes and analyzed accordingly. These themes were each tied into the ultimate benefit to patients and led to suggested uses and potential future directions. Consequently, here we focus on considerations regarding mobile application use, our experiences with their effects on patient rapport, and suggested circumstances for routine integration of applications in clinical practice.
The user interface, referring both to a visually appealing layout and logical organization, is often the most striking feature of any application. It is particularly important when considering that these applications are effectively presentation aids for the bedside. Simplicity, accuracy, and quality of anatomic images were universally considered the most important features of these applications. To this effect it is important to acknowledge that these apps are not currently subject to peer review [10, 11]. While we encourage exploration for application potential, it is also important to maintain awareness of potential inaccuracy.
Several applications also had the ability to email the image that was produced, which patients greatly appreciated. This allowed the digital illustrations to achieve a similar lasting effect as noted with pen and paper illustrations that patients often carried and referred to throughout their time in the hospital.
Screen size is also an important consideration in the utility of any application. We found the smaller screens of smartphones were a significant strain for many of our patients who already have limited vision, despite high quality of images or user interface. Though phones are certainly more compact and convenient, we fully endorse the value provided by a tablet’s additional screen size. For applications confined to small screens, the ability to zoom and rotate images was especially appreciated, allowing users to hone in on the salient content and maximize resolution despite limited screen size.
Several limitations were present in this study. First, the small sample size of evaluators was not amenable to an objective comparison of experiences. Consequently, we focused on the narrative experiences of the students as they systematically evaluated the applications and informatively conveyed their experiences. Additionally, while variation in the operating systems and devices was a valuable consideration for discussion, a more objective approach would either involve rotating devices in the same order through all evaluators, or simply a utilizing larger cohort of users for each device and operating system. Finally, we did not collect data on the demographics of patients with whom evaluators interacted during the trial periods, nor did we survey patients regarding their opinions. It is conceivable that these factors may have influenced the evaluators’ perceptions, and indeed may represent an interesting subject for further study.
Any educational time spent one-on-one with a patient has the potential to build rapport as patients become more confident in their own understanding as well as their provider’s expertise. It was our experience that patients gained more respect for a trainee who specifically devoted time to bedside teaching and was able to nurture the patients’ desires to comprehend and take ownership of their own health. While we felt applications improved our ability to effectively teach due to high quality images, animations, and information, the use of technology was occasionally noted as a distracter. For patients who were less familiar with smartphones or tablets, the novelty of the device was a source of fascination or at times even overwhelming. We caution that it is important to be aware of patient comfort with technology and advise a low threshold to return to baseline modalities of education such as pen and paper illustrations.
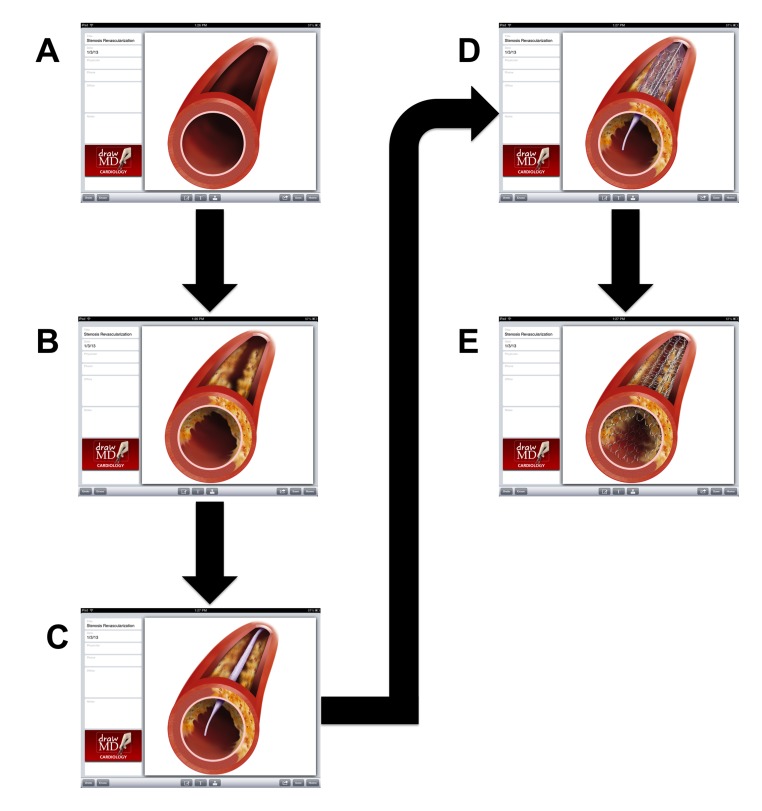
There exist several opportunities to integrate mobile applications as a part of routine clinical practice. First, anatomy-based applications lend themselves nicely to procedures of any form. In fact, we suggest that the preoperative discussion and consent process incorporate these applications to more fully ensure that the patient understands the procedure and has ample opportunity to ask questions. Additionally, we also noted that patients appreciated a post-procedure encounter focused on a recap of what was performed. A prime example involved cardiac catheterization. One evaluator reported using the DrawMDTM program to demonstrate a normal coronary vessel and added an atherosclerotic plaque, explaining that based on the amount of occlusion the patient required a stent to be placed. He was then able to add in an image of an undeployed balloon catheter and stent followed by the deployed versions, and finally a concluding image showing only the remaining stent maintaining artery patency (► Figure 1). In this way the patient understood both the rationale and process of his catheterization.
Fig. 1.
Screenshots Taken From iPad of Angioplasty and Stenting Demonstration with DrawMD. A) Normal coronary vessel. B) Atherosclerotic vessel. C) Undeployed balloon and stent. D) Deployed balloon and stent. E) Remaining stent after removal of catheter.
While these applications are certainly relevant to procedures, there are additionally non-procedural encounters in which this technology can be extremely useful. In fact, we would argue that any time a new diagnosis is made the opportunity exists to use one of these applications. In our medical school we are consistently offered strategies to communicate disease processes to the patient and assess their level of understanding, and these applications offer an additional tool to that armamentarium. The ideal dissemination of these applications across all providers would be incorporation into or communication with existing electronic health record systems, though this process is limited by a number of technical challenges beyond the scope of this article.
Finally, discharge from the hospital also offers ample opportunity to utilize these applications. The provider can walk the patient through their hospital course either by organ system or medical diagnosis, utilizing these resources as needed to clarify a disease process or answer a patient’s questions. Any annotated images produced during this recap can and should be emailed to patients so they can bring them to their follow up appointments or simply retain for their own understanding. After all, sometimes a picture really is worth a thousand words.
5. Conclusion
As mobile applications continue to evolve and the prevalence of mobile devices in the healthcare setting increases, there is limitless potential for their use in patient education. We are enthusiastic about the new and exciting ways software developers are offering physicians to connect with patients, and hope that any feedback we provided will be useful in this creative process. Moving forward it is important that we continue to explore potential value of these applications, both in facilitating bedside teaching as well as patient-provider rapport, while recognizing any limitations. It is our hope that our article facilitates awareness of resources currently available to healthcare professionals and simultaneously promotes a sense of intrigue for the evolution of this new technology.
Cliniclal Relevance Statement
Patient counseling is one of the fundamental privileges of healthcare professionals, and medical students are in a fortunate position to take part in this process. As the availability and quality of mobile applications for healthcare rapidly increases, it is essential that we examine their utility in facilitating understanding and visualization of disease processes for interested patients.
Conflicts Of Interest
The authors declare that they have no conflicts of interest in this research.
Protection Of Human And Animal Subjects
This project was reviewed and approved by the Johns Hopkins Institutional Review Board.
Acknowledgments
The authors would like to thank Mitchell Goldstein, MD who is Assistant Professor of Pediatric Emergency Medicine at the Johns Hopkins Hospital in Baltimore, MD for his assistance in obtaining IRB approval for this research endeavor.
References
- 1.Greene JA. Releasing the Flood Waters: Diuril and the Reshaping of Hypertension. Bull Hist Med 2005; 79: 749-794 DOI: dx.doi.org/10.1353/bhm.2005.0153 [DOI] [PubMed] [Google Scholar]
- 2.Miller KH, Ziegler C, Greenberg R, Patel PD, Carter MB. Why physicians should share PDA/smartphone findings with their patients: A brief report. J Health Commun 2012; 17: 54-61 DOI: dx.doi.org/10.1080/10810730.2011.649102 [DOI] [PubMed] [Google Scholar]
- 3.Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: A review of current and potential use among physicians and students. J Med Internet Res 2012; 14 DOI: dx.doi.org/10.2196/jmir.1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pearlswan Communications LLC. Meditoons, version 2.0. 2012. AccessedJanuary 3, 2013. Available at: http://www.meditoons.com
- 5.Research Institute against Digestive Cancer (IRCAD). The Visible Patient, version 0.3. 2010. AccessedJanuary 3, 2013. Available at:http://visiblepatient.eu
- 6.Visible Health. DrawMD, version 2.6.575. 2013. AccessedJanuary 3, 2013. Available at:http://www. drawmd.com
- 7.Boston Scientific Corporation. CardioTeach for iPad, version 2.0. 2013. AccessedJanuary 3, 2013. Available at:http://www.bostonscientific.com/cardiac-rhythm-resources/campaign/CardioTeach.html
- 8.Education Mobile. Visual Anatomy-Free, version 3.1. 2012. AccessedJanuary 3, 2013. Available at:https://sites.google.com/site/imagemagicstudio
- 9.Indendant LLC. 360 Patient Education Suite, version 1.10. 2012. AccessedJanuary 3, 2013. Available at:http://incendant.com
- 10.Hogan NM, Kerin MJ. Smart phone apps: Smart patients, steer clear. Patient Educ Couns 2012; 89: 360-361 DOI: dx.doi.org/10.1016/j.pec.2012.07.016 [DOI] [PubMed] [Google Scholar]
- 11.Visser BJ, Buijink AWH. Need to peer-review medical applications for smart phones. J Telemed Telecare 2012; 18 DOI: dx.doi.org/10.1258/jtt.2011.110205 [DOI] [PubMed] [Google Scholar]