Abstract
Cocaine users represent an Emergency Department (ED) population that has been shown to be at increased risk for ACS; however, there is controversy about whether this higher risk is mediated through advanced atherosclerosis. Thus, we aimed to determine whether history of cocaine use is associated with acute coronary syndrome (ACS) and coronary artery disease using coronary computed tomography (CT). In this matched cohort study, we selected patients with a history of cocaine use and age- and gender-matched controls from a large cohort of consecutive patients who presented with acute chest pain to the ED. Coronary atherosclerotic plaque as detected by 64-slice coronary CT was compared between the groups. Among 412 patients, 44 had a history of cocaine use (9%) and were matched to 132 controls (mean age: 46±6 years, 86% male). History of cocaine use was associated with a 6-fold higher risk for ACS (odds ratio: 5.79, 95%-confidence interval: 1.24–27.02, p=0.02), but was not associated with a higher prevalence of any plaque, calcified plaque, or non-calcified plaque (p=1.0, p=1.0; and p=0.58, respectively) or the presence of significant stenosis (p=0.09). History of cocaine use was also not associated with the extent of any, calcified, or non-calcified plaque (p=0.67, p=0.30, and p=0.12, respectively). These associations persisted after adjustment for other cardiovascular risk factors. In conclusion, among ED patients presenting with acute chest pain, history of cocaine use is associated with an increase in risk for ACS; however, this was not attributable to a higher presence or extent of coronary atherosclerotic plaque.
INTRODUCTION
Coronary multidetector computed tomography (MDCT) generates high quality images of the coronary vasculature, enabling the detection of significant coronary artery stenosis with high sensitivity and specificity (>90%) when compared to invasive coronary angiography.1 Additionally, MDCT has good agreement with intravascular ultrasound (IVUS) and can qualitatively assess for the presence and extent coronary atherosclerotic plaque.2,3 The aim of the present study was to determine whether the risk of acute coronary syndrome (ACS) in patients who present to the emergency department (ED) with acute chest pain and a history of cocaine use may be associated with the presence and extent of coronary artery disease (CAD) when compared to age- and gender-matched controls.
METHODS
We performed a nested matched-cohort study within the “Rule Out Myocardial Ischemia using Computed Assisted Tomography” (ROMICAT) study, which was designed to assess the diagnostic utility of coronary MDCT in patients with acute chest pain but inconclusive initial ED evaluation.3,4 In this prospective, double-blinded observational cohort study, we enrolled consecutive adult patients presenting to the ED with acute chest pain but with no ischemic electrocardiographic changes and negative initial serum biomarkers who were awaiting admission to the hospital to rule out myocardial infarction. Exclusion criteria were previously reported and mainly related to contrast administration (i.e. serum creatinine greater than 1.3 mg/dl).4 In this substudy, we also excluded patients with prior history of percutaneous coronary intervention with or without stent implantation and history of coronary artery bypass graft. For this analysis, subjects who reported previous use of cocaine were matched by age and gender at a 1:3 sampling ratio with subjects who did not report previous cocaine use. All subjects successfully underwent coronary MDCT scanning and were followed during index hospitalization for the occurrence of ACS. The study was approved by our Institutional Review Board and all participants provided written informed consent.
Cocaine users were defined as subjects with a self-reported and documented (medical chart review) history of non-occasional (>3 time within 1 year) cocaine use.5–7 ACS was defined by the occurrence of either acute myocardial infarction (ST-Elevation Myocardial Infarction [STEMI] or Non-ST-Elevation Myocardial Infarction [NSTEMI]) or unstable angina pectoris (UAP) according to the AHA/ACC/ESC guidelines.8 An expert panel consisting of one cardiologist and one ED physician reviewed all patient data forms including prospectively collected information on the chest pain history, demographics, cardiovascular risk factors, medical history, and results of coronary biomarkers, electrocardiograms, and other test performed during index hospitalization. The reviewers were blinded to the findings of coronary CT angiography.
Covariates were assessed at the time of subject’s enrollment. Presence of cardiovascular risk factors was established from actual measurements obtained during index hospitalization. Hypertension was defined as systolic blood pressure of at least 140 mm Hg or diastolic blood pressure of at least 90 mm Hg or current antihypertensive treatment. Diabetes mellitus was defined as a fasting plasma glucose ≥126 mg/dL or treatment with a hypoglycemic agent. Hyperlipidemia was defined as total cholesterol of ≥200 mg/dl or treatment with a lipid lowering medication. Subjects were classified as smokers if they had smoked at least one cigarette per day in the year prior to the study. Body mass index (BMI) was defined as weight (kilograms) divided by the height squared (meters). Family history of CAD was defined as having a first-degree relative with a documented history of myocardial infarction (MI) or sudden coronary death (female <65 years or male <55 years).
All MDCT imaging was performed with a 64-slice MDCT scanner (Sensation 64, Siemens Medical Solutions, Forchheim, Germany) as described previously.4 In preparation for the scan, all patients with a heart rate greater than 65 beats per minute received beta-blocker therapy with intravenous metoprolol in 5 mg increments for a maximum of 25 mg, unless contraindications were present. All image acquisitions were performed during a breath hold in inspiration using standard image parameters.4 Contrast injection (Nycomed Amersham GE-Healthcare Vispaque 300 mg I/mL) was administered at an injection rate of 5 mls per second (mean volume 78±11 ml) with a delay calculated during the timing bolus scan. The contrast injection was immediately followed by 40 ml of saline also at a rate of 5 ml per second. Electrocardiogram-correlated tube current modulation was used to minimize radiation exposure (resulting in an estimated effective dose of 6–11 mSv) whenever possible. Overlapping transaxial images were reconstructed using a medium sharp convolution kernel (B25f) with an image matrix of 512×512 pixels, slice thickness of 0.75 mm and increment of 0.4 mm using an ECG-gated half-scan algorithm with a resulting temporal resolution 165 ms in the center of rotation. Image reconstruction was retrospectively gated to the electrocardiogram. The position of the reconstruction window within the coronary cycle was individually optimized to minimize motion artifacts. Reconstructed MDCT data sets of all patients were transferred to an offline workstation (Leonardo; Siemens Medical Solutions, Forchheim, Germany).
For the detection of CAD, the 17-segment model based on the American Heart Association classification with the addition of the posterior left ventricular branch as segment 16 and the ramus intermedius as segment 17 was used.9 Coronary atherosclerotic plaque was visually classified as non-calcified and/or calcified plaque as described previously.3,10 Non-calcified plaque was defined as any discernible structure that could be assigned to the coronary artery wall that had the CT attenuation below the contrast-enhanced coronary lumen but above the surrounding connective tissue/epicardial fat in at least two independent planes. Calcified atherosclerotic plaque was identified as any structure with a CT attenuation of greater than 130 HU that could be visualized separately from the contrast-enhanced coronary lumen (see Figure 1). Atherosclerotic plaque burden as measured by coronary MDCT was evaluated based on: (1) presence of significant coronary stenosis (>50% luminal narrowing), (2) presence of coronary atherosclerotic plaque (any, calcified, non-calcified), (3) extent of coronary atherosclerotic plaque (as categorized by any, calcified, non-calcified) and quantified by presence in each of the 17 segments (grade 0–17), (4) presence of proximal plaque as defined by the presence of any plaque within proximal right coronary artery, left main coronary artery, proximal left anterior descending coronary artery, or proximal circumflex coronary artery, and (5) extent of proximal plaque was defined as the number of proximal segments containing plaque. Two experienced CT readers, blinded to the clinical history, performed the analysis in a joint reading. If a consensus could not be reached, a third expert reader made the final diagnosis. This method has been demonstrated to be highly reproducible (Cohen’s κ= 0.92 and 0.81).4
Figure 1.
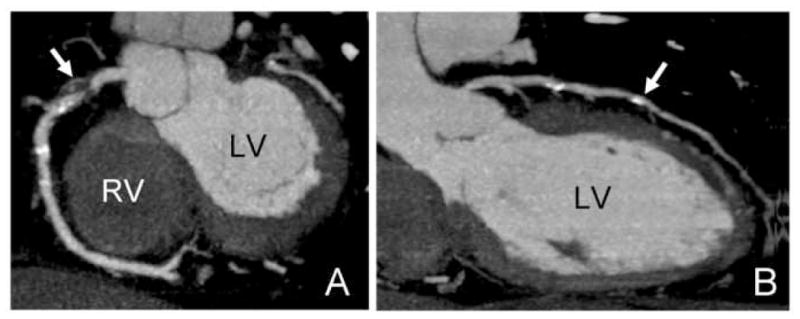
Coronary computed tomography of 56 year-old male with acute coronary syndrome and a history of cocaine use demonstrating non-calcified, calcified plaque, and a significant coronary stenosis. A: Maximum intense projection (MIP) image of the right coronary artery with non-calcified plaque in the proximal portion (arrow) and a significant coronary stenosis (>50% luminal narrowing) in the proximal segment of the vessel. B: Curved multiplanar reformation of the left anterior descending coronary artery with calcified plaque in the mid segment of the vessel. LV: left ventricle; RV: right ventricle.
Descriptive statistics are provided as mean ± standard deviation for continuous and as absolute and relative frequency for categorical variables. Clinical characteristics and CT findings on the presence and extent of plaque and stenosis between the two groups were compared using the Chi-square test for categorical variables and Student’s t-test or Wilcoxon signed rank test for normally and non-normally distributed continuous variables, respectively. To compare the extent of atherosclerotic plaque (all, calcified, and non-calcified) between the two groups, we excluded subjects without any plaque. Multivariable logistic regression analysis was performed to determine the independent association between history of cocaine use and plaque or ACS after adjustment for potential confounders. The models contained the cocaine variable as the dependent variable and the extent or presence of plaque (any, calcified, or non-calcified) as covariates. Similarly, we modeled the association between history of cocaine use and ACS. Each of these models was adjusted for the presence of hyperlipidemia, diabetes, smoking, and hypertension as a predefined set of cardiovascular risk factors and subsequently for the extent of plaque and coronary stenosis. A p-value of <0.05 was considered to be statistically significant. All analyses were performed using SAS Version 9.1 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Among the overall study cohort of 412 patients, 44 patients had a history of cocaine use, who were predominantly younger males. Among them, 16 subjects (36%) reported intravenous use and 8 subjects (18%) reported concomitant abuse of other drugs. These were matched with 132 controls of similar age and gender. Patient demographics were detailed in Table 1. Patients with history of cocaine had a similar prevalence of hypertension, hyperlipidemia, diabetes mellitus, or serum level of low density and high density lipoprotein (all p>0.14) when compared with controls. However, they were more likely to be present or past smokers (p<0.001).
Table 1.
Baseline characteristics of 176 patients with acute chest pain and demographic differences between patient with history of cocaine use and matched controls. Patients with history of cocaine were more likely to be current or past smokers (p<0.001). Hyperlipidemia was defined as total cholesterol of ≥200 mg/dl or treatment with a lipid lowering medication.
| Variable | Total | History of Cocaine | No History of Cocaine | P-Value |
|---|---|---|---|---|
|
| ||||
| (n=176) | (n=44) | (n=132) | ||
| Age (years) | 46.3±7 | 46.3±7 | 46.2±7 | 0.91 |
| Men (%) | 152 (86%) | 38 (86%) | 114 (86%) | 1.0 |
| Hypertension | 56 (32%) | 13 (30%) | 43 (33%) | 0.85 |
| Hyperlipidemia* | 58 (32%) | 16 (36%) | 42 (32%) | 0.58 |
| Diabetes mellitus | 22 (13%) | 8 (18%) | 13 (10%) | 0.19 |
| Smoker | 88 (50%) | 32 (73%) | 56 (42%) | <0.001 |
| Low-density lipoprotein (mg/dl) | 113.1±4 | 106.8±3 | 115.1±3 | 0.21 |
| High-density lipoprotein (mg/dl) | 48.0±2 | 49.6±2 | 47.5±1 | 0.52 |
Patients with history of cocaine use had a significantly higher rate of ACS (14% vs. 2%, p=0.008; Table 2). In contrast, history of cocaine use was not associated with higher prevalence of any, calcified, or non-calcified plaque (p=1.0, p=1.0; and p=0.58, respectively) as illustrated in Figure 2; or the extent of any, calcified or non-calcified plaque (p=0.67, p=0.30, and p=0.12, respectively) as illustrated in Figure 3. In further analyses, there were also no differences in the presence and extent of proximal plaque (p=0.59 and p=0.70, respectively) between patients with a history of cocaine use and controls. Moreover, the prevalence of significant coronary stenosis was not different between the groups (p=0.09).
Table 2.
Prevalence of acute coronary syndrome and atherosclerotic plaque burden as assessed by coronary computed tomography between subjects with history of cocaine use as compared to controls. Stenosis is defined as >50% luminal narrowing. Any plaque includes the presence of any atherosclerotic plaque per patient. Proximal Plaque includes the presence of any plaque within proximal right coronary artery, left main coronary artery, proximal left anterior descending coronary artery, or proximal circumflex coronary artery.
| Variable | Total | Cocaine History | P-Value | |
|---|---|---|---|---|
| Yes | No | |||
|
| ||||
| (n=176) | (n=44) | (n=132) | ||
| Acute Coronary Syndrome | 9 (5%) | 6 (14%) | 3 (2%) | 0.008 |
| Coronary Stenosis | 19 (11%) | 8 (18%) | 11 (8%) | 0.09 |
|
| ||||
|
Presence of coronary atherosclerotic plaque
| ||||
| Any Plaque | 79 (45%) | 20 (45%) | 59 (45%) | 1.0 |
| Any Calcified Plaque | 67 (38%) | 17 (39%) | 50 (38%) | 1.0 |
| Any Non-calcified Plaque | 61 (35%) | 17 (39%) | 44 (33%) | 0.58 |
| Any Proximal Plaque | 69 (39%) | 19 (43%) | 50 (38%) | 0.59 |
|
| ||||
|
Extent of coronary atherosclerotic plaque
| ||||
| Extent of any plaque | 4.6±3.6 | 5.0±3.9 | 4.5±3.5 | 0.67 |
| Extent of calcified plaque | 4.5±3.5 | 5.2±3.6 | 4.3±3.5 | 0.30 |
| Extent of non-calcified plaque | 2.6±2.0 | 2.1±1.8 | 2.8±2.1 | 0.12 |
| Extent of Proximal Plaque | 1.7±1.2 | 1.9±1.1 | 1.6±1.2 | 0.70 |
Figure 2.
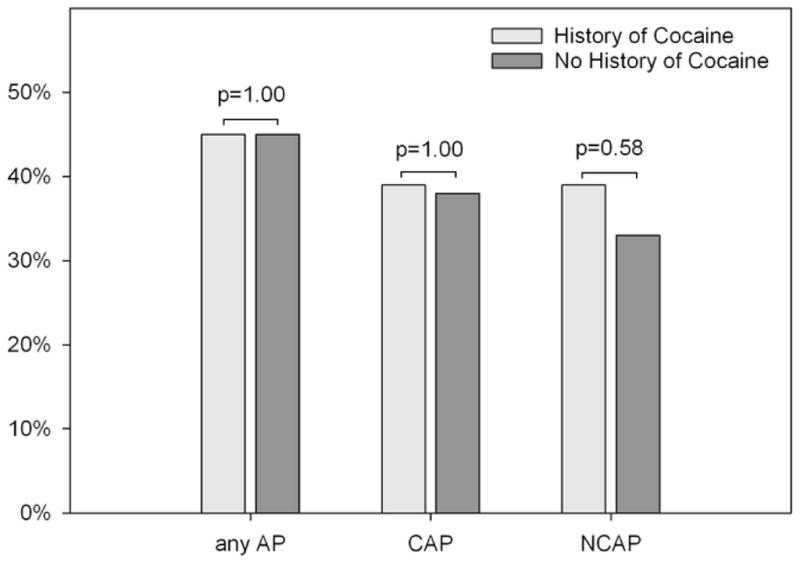
Presence of any atherosclerotic plaque (any AP), calcified atherosclerotic plaque (CAP), and non-calcified atherosclerotic plaque (NCAP) between patients with history of cocaine (white bars) as compared to controls (grey bars).
Figure 3.
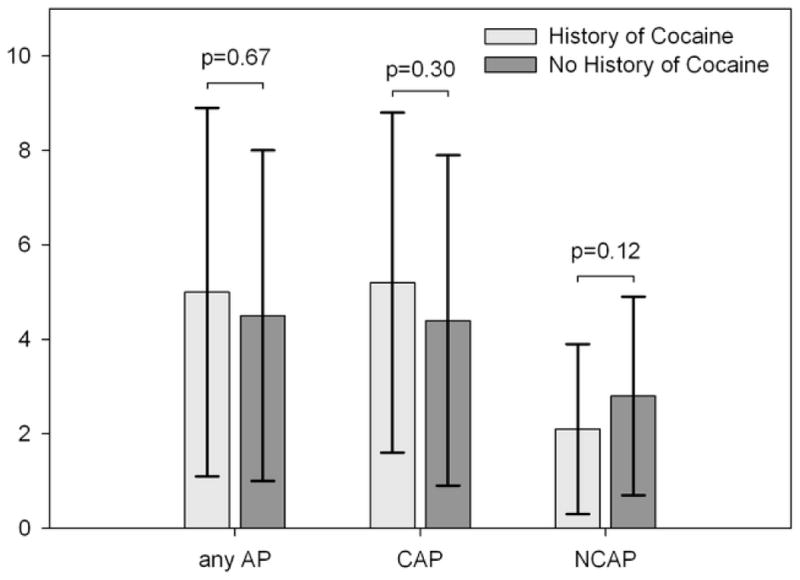
Extent of coronary segments containing any atherosclerotic plaque (any AP), calcified atherosclerotic plaque (CAP), and non-calcified atherosclerotic plaque (NCAP) between patients with history of cocaine (white bars) as compared to controls (grey bars).
History of cocaine use was associated with a six-fold higher risk for ACS (odds ratio [OR] 5.79, 95%-confidence interval [CI]: 1.24–27.02; p=0.02) after adjustment for hyperlipidemia, diabetes, smoking, and hypertension. This strong association persisted after adjustment for the extent of calcified and non-calcified plaque and the presence of significant stenosis (OR: 12.13, 95%-CI: 1.47–100.39; p=0.02; Figure 4).
Figure 4.
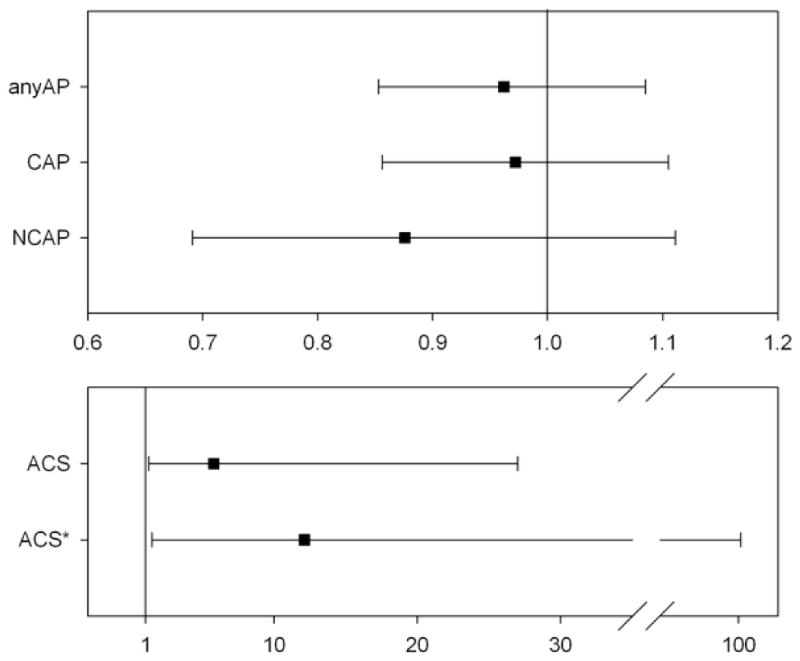
Forrest-plots demonstrating the association between different coronary atherosclerotic plaque findings (extent of any atherosclerotic plaque [anyAP], calcified [CAP], and non-calcified atherosclerotic plaque [NCAP], upper graph) and occurrence of acute coronary syndrome (ACS, lower graph) with history of cocaine use. All associations were adjusted for hypertension, hyperlipidemia, smoking and diabetes mellitus. * Further adjustment for the extent of calcified and non-calcified plaque and presence of coronary stenosis.
Consistent with the univariate comparisons, there was no association between history of cocaine use and the presence and extent of any of the plaque variables after adjustment for hyperlipidemia, diabetes, smoking, and hypertension (all p>0.38).
DISCUSSION
In this study, we determined differences in ACS rate and atherosclerotic plaque burden as detected by coronary CT between patients with a history of cocaine use and age- and gender-matched controls. Our results indicate that among patients presenting with acute chest pain, history of cocaine use is associated with a 6-fold increased in risk for ACS. However, this difference cannot be explained with differences in the presence and extent of coronary atherosclerotic plaque burden as detected by coronary CT.
Cocaine use is highly prevalent in patients who present with acute chest pain to the ED.11 Various effects of acute cardiovascular of cocaine are known.12 Cocaine has been associated with an increase in heart rate and blood pressure in a dose-dependent fashion 13 and has a vasoconstrictive effect, leading to endothelial dysfunction. 14,15 Further, cocaine has been shown to enhance platelet aggregation 16 and thrombosis 17,18, and to promote transient erythrocytosis.19 Cocaine therefore causes myocardial ischemia in a multifactorial fashion that includes increased oxygen demand, decreased oxygen supply, and the induction of a prothrombotic state.11
While these pathophysiologic effects of cocaine have been well documented, the effect of cocaine on the formation of atherosclerosis is more controversial. Experimental animal studies suggest a potential relationship between cocaine effect and atherosclerosis due to endothelial damage 20 and increased vascular permeability.21 Further, small autopsy studies suggest that atherosclerotic plaque burden is high among cocaine users.22–24 Kolodgie et al. found that 30 year old cocaine users already had significant coronary atherosclerosis. However, due to lack of a control group, these studies limit causal interference.
Using coronary calcification as a marker of atherosclerosis in living patients, Lai et al. reported a borderline significant association between cocaine use and extent of coronary calcification among 197 intravenous drug users after adjustment for age and gender.25 In contrast, Pletcher et al. did not detect and association between cocaine exposure and the extent of coronary calcification among 3038 participants in the Coronary Artery Risk Development in Young Adults (CARDIA) study.26 Our findings confirm these observations and demonstrate no association between history of cocaine use and coronary calcification (p=1.0 and p=0.30, for the presence and extent of CAP; respectively). However, our study extends those observations to the presence and extent of non-calcified plaque. Non-calcified plaque but not calcified is present in culprit lesions in patients with acute coronary syndrome.27 We found that patients with a history of cocaine use had a similar presence and extent of overall non-calcified plaque as compared to age and sex matched controls (39% vs. 33%; p=0.58 and 2.1±2 vs. 2.8±2; p=0.12; respectively).
Our study improves the understanding of the role of a history of cocaine use in ACS. First, it is likely that cocaine may trigger ACS through other mechanisms than atherosclerosis.14 Although cocaine induces vasoconstriction in both normal and diseased segments of coronary arteries, its effects are more pronounced in the diseased segments.14 As such, previous observed associations between cocaine use and CAD are explained primarily by the well-documented acute effect of cocaine.5,17 Second, coronary CT may not be helpful to assess the incremental risk for ACS of patients with a history of cocaine use.
The results of our study are limited to patients with a history of cocaine use but cannot be extended to subjects with acute cocaine consumption. Although validated as a method for estimating plaque burden, our per-segment approach for overall plaque burden assessment provides only a crude estimate of overall plaque burden and we did not study distinct plaque characteristics by CT. However, quantitative CT assessment of coronary plaque has been reported to have high inter-observer variability.28 Our study is limited by the sample size, especially few ACS events and self-reported cocaine use. Thus, our findings need to be replicated and extended in a larger study sample.
Acknowledgments
Funding Source: This work was supported by the NIH (R01 HL080053), and in part supported by Siemens Medical Solutions and General Electrics Healthcare.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 2.Achenbach S, Moselewski F, Ropers D, Ferencik M, Hoffmann U, MacNeill B, Pohle K, Baum U, Anders K, Jang IK, Daniel WG, Brady TJ. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation. 2004;109:14–17. doi: 10.1161/01.CIR.0000111517.69230.0F. [DOI] [PubMed] [Google Scholar]
- 3.Leber AW, Knez A, von Ziegler F, Becker A, Nikolaou K, Paul S, Wintersperger B, Reiser M, Becker CR, Steinbeck G, Boekstegers P. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005;46:147–154. doi: 10.1016/j.jacc.2005.03.071. [DOI] [PubMed] [Google Scholar]
- 4.Hoffmann U, Nagurney JT, Moselewski F, Pena A, Ferencik M, Chae CU, Cury RC, Butler J, Abbara S, Brown DF, Manini A, Nichols JH, Achenbach S, Brady TJ. Coronary multidetector computed tomography in the assessment of patients with acute chest pain. Circulation. 2006;114:2251–2260. doi: 10.1161/CIRCULATIONAHA.106.634808. [DOI] [PubMed] [Google Scholar]
- 5.Qureshi AI, Suri MF, Guterman LR, Hopkins LN. Cocaine use and the likelihood of nonfatal myocardial infarction and stroke: data from the Third National Health and Nutrition Examination Survey. Circulation. 2001;103:502–506. doi: 10.1161/01.cir.103.4.502. [DOI] [PubMed] [Google Scholar]
- 6.Patrizi R, Pasceri V, Sciahbasi A, Summaria F, Rosano GM, Lioy E. Evidence of cocaine-related coronary atherosclerosis in young patients with myocardial infarction. J Am Coll Cardiol. 2006;47:2120–2122. doi: 10.1016/j.jacc.2005.12.060. [DOI] [PubMed] [Google Scholar]
- 7.Satran A, Bart BA, Henry CR, Murad MB, Talukdar S, Satran D, Henry TD. Increased prevalence of coronary artery aneurysms among cocaine users. Circulation. 2005;111:2424–2429. doi: 10.1161/01.CIR.0000165121.50527.DE. [DOI] [PubMed] [Google Scholar]
- 8.Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, Jones RH, Kereiakes D, Kupersmith J, Levin TN, Pepine CJ, Schaeffer JW, Smith EE, 3rd, Steward DE, Theroux P, Gibbons RJ, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Hiratzka LF, Jacobs AK, Smith SC., Jr ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction--2002: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina) Circulation. 2002;106:1893–1900. doi: 10.1161/01.cir.0000037106.76139.53. [DOI] [PubMed] [Google Scholar]
- 9.Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51:5–40. doi: 10.1161/01.cir.51.4.5. [DOI] [PubMed] [Google Scholar]
- 10.Bamberg F, Dannemann N, Shapiro MD, Seneviratne SK, Ferencik M, Butler J, Koenig W, Nasir K, Cury RC, Tawakol A, Achenbach S, Brady TJ, Hoffmann U. Association between cardiovascular risk profiles and the presence and extent of different types of coronary atherosclerotic plaque as detected by multidetector computed tomography. Arterioscler Thromb Vasc Biol. 2008;28:568–574. doi: 10.1161/ATVBAHA.107.155010. [DOI] [PubMed] [Google Scholar]
- 11.Lange RA, Hillis LD. Cardiovascular complications of cocaine use. N Engl J Med. 2001;345:351–358. doi: 10.1056/NEJM200108023450507. [DOI] [PubMed] [Google Scholar]
- 12.Foltin RW, Ward AS, Haney M, Hart CL, Collins ED. The effects of escalating doses of smoked cocaine in humans. Drug Alcohol Depend. 2003;70:149–157. doi: 10.1016/s0376-8716(02)00343-5. [DOI] [PubMed] [Google Scholar]
- 13.Flores ED, Lange RA, Cigarroa RG, Hillis LD. Effect of cocaine on coronary artery dimensions in atherosclerotic coronary artery disease: enhanced vasoconstriction at sites of significant stenoses. J Am Coll Cardiol. 1990;16:74–79. doi: 10.1016/0735-1097(90)90459-3. [DOI] [PubMed] [Google Scholar]
- 14.Kuhn FE, Gillis RA, Virmani R, Visner MS, Schaer GL. Cocaine produces coronary artery vasoconstriction independent of an intact endothelium. Chest. 1992;102:581–585. doi: 10.1378/chest.102.2.581. [DOI] [PubMed] [Google Scholar]
- 15.Kugelmass AD, Shannon RP, Yeo EL, Ware JA. Intravenous cocaine induces platelet activation in the conscious dog. Circulation. 1995;91:1336–1340. doi: 10.1161/01.cir.91.5.1336. [DOI] [PubMed] [Google Scholar]
- 16.Mittleman MA, Mintzer D, Maclure M, Tofler GH, Sherwood JB, Muller JE. Triggering of myocardial infarction by cocaine. Circulation. 1999;99:2737–2741. doi: 10.1161/01.cir.99.21.2737. [DOI] [PubMed] [Google Scholar]
- 17.Lee HO, Eisenberg MJ, Drew D, Schiller NB. Intraventricular thrombus after cocaine-induced myocardial infarction. Am Heart J. 1995;129:403–405. doi: 10.1016/0002-8703(95)90025-x. [DOI] [PubMed] [Google Scholar]
- 18.Siegel AJ, Sholar MB, Mendelson JH, Lukas SE, Kaufman MJ, Renshaw PF, McDonald JC, Lewandrowski KB, Apple FS, Stec JJ, Lipinska I, Tofler GH, Ridker PM. Cocaine-induced erythrocytosis and increase in von Willebrand factor: evidence for drug-related blood doping and prothrombotic effects. Arch Intern Med. 1999;159:1925–1929. doi: 10.1001/archinte.159.16.1925. [DOI] [PubMed] [Google Scholar]
- 19.McCord J, Jneid H, Hollander JE, de Lemos JA, Cercek B, Hsue P, Gibler WB, Ohman EM, Drew B, Philippides G, Newby LK. Management of Cocaine-Associated Chest Pain and Myocardial Infarction. A Scientific Statement From the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Circulation. 2008;117:1897–1907. doi: 10.1161/CIRCULATIONAHA.107.188950. [DOI] [PubMed] [Google Scholar]
- 20.Langner RO, Bement CL, Perry LE. Arteriosclerotic toxicity of cocaine. NIDA Res Monogr. 1988;88:325–336. [PubMed] [Google Scholar]
- 21.Kolodgie FD, Wilson PS, Cornhill JF, Herderick EE, Mergner WJ, Virmani R. Increased prevalence of aortic fatty streaks in cholesterol-fed rabbits administered intravenous cocaine: the role of vascular endothelium. Toxicol Pathol. 1993;21:425–435. doi: 10.1177/019262339302100501. [DOI] [PubMed] [Google Scholar]
- 22.Kolodgie FD, Virmani R, Cornhill JF, Herderick EE, Smialek J. Increase in atherosclerosis and adventitial mast cells in cocaine abusers: an alternative mechanism of cocaine-associated coronary vasospasm and thrombosis. J Am Coll Cardiol. 1991;17:1553–1560. doi: 10.1016/0735-1097(91)90646-q. [DOI] [PubMed] [Google Scholar]
- 23.Tardiff K, Gross E, Wu J, Stajic M, Millman R. Analysis of cocaine-positive fatalities. J Forensic Sci. 1989;34:53–63. [PubMed] [Google Scholar]
- 24.Dressler FA, Malekzadeh S, Roberts WC. Quantitative analysis of amounts of coronary arterial narrowing in cocaine addicts. Am J Cardiol. 1990;65:303–308. doi: 10.1016/0002-9149(90)90292-9. [DOI] [PubMed] [Google Scholar]
- 25.Lai S, Lai H, Meng Q, Tong W, Vlahov D, Celentano D, Strathdee S, Nelson K, Fishman EK, Lima JA. Effect of cocaine use on coronary calcium among black adults in Baltimore, Maryland. Am J Cardiol. 2002;90:326–328. doi: 10.1016/s0002-9149(02)02475-x. [DOI] [PubMed] [Google Scholar]
- 26.Pletcher MJ, Kiefe CI, Sidney S, Carr JJ, Lewis CE, Hulley SB. Cocaine and coronary calcification in young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am Heart J. 2005;150:921–926. doi: 10.1016/j.ahj.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 27.Hoffmann U, Moselewski F, Nieman K, Jang IK, Ferencik M, Rahman AM, Cury RC, Abbara S, Joneidi-Jafari H, Achenbach S, Brady TJ. Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multidetector computed tomography. J Am Coll Cardiol. 2006;47:1655–1662. doi: 10.1016/j.jacc.2006.01.041. [DOI] [PubMed] [Google Scholar]
- 28.Leber AW, Becker A, Knez A, von Ziegler F, Sirol M, Nikolaou K, Ohnesorge B, Fayad ZA, Becker CR, Reiser M, Steinbeck G, Boekstegers P. Accuracy of 64-slice computed tomography to classify and quantify plaque volumes in the proximal coronary system: a comparative study using intravascular ultrasound. J Am Coll Cardiol. 2006;47:672–677. doi: 10.1016/j.jacc.2005.10.058. [DOI] [PubMed] [Google Scholar]


