Abstract
Cocaine is the most commonly abused drug in patients presenting to emergency rooms. Compliance with medical instructions and medications is poor in patients who use cocaine. A case involving a 41-year-old cocaine user who developed subacute stent thrombosis is described. The patient underwent bare metal stent implantation three days before presentation and had confirmed compliance with dual antiplatelet therapy. The stent thrombosis was treated with a manual and mechanical thrombectomy, in addition to percutaneous transluminal coronary angioplasty. Given the issue of compliance and the increased evidence of cocaine-induced thrombosis in native vessels and stents, it is recommended that balloon angioplasty alone should be the treatment of choice when intervention is required.
Keywords: Cocaine, Myocardial infarction, Stent thrombosis
A 41-year-old man without a previous cardiac history presented to the emergency department (ED) with complaints of frequent episodes of chest discomfort. He also reported dyspnea, diaphoresis and left arm numbness in addition to his chest discomfort. His medical history was significant for hypertension, type 2 diabetes mellitus, and tobacco and cocaine use. The physical examination was remarkable for an S4 gallop on cardiac auscultation. The electrocardiogram was significant for T-wave inversion in leads II, III and aVF, as well as V3, V4 and V5 (Figure 1). Serial cardiac enzyme investigations were negative. A urine drug screen was positive for cocaine. A chest x-ray was unremarkable (Figure 2). The patient was diagnosed with unstable angina and was started on dual antiplatelet therapy, an anticoagulant drug and a statin. A beta-blocker medication was not started because of bradycardia. He underwent uneventful left heart catheterization, which revealed a tubular stenosis of 75% to 90% in the mid left anterior descending (LAD) artery (Figure 3), which was stented with two consecutive bare metal stents (BMS) measuring 3.5 mm × 28 mm, and 3.5 mm × 12 mm (Figure 4). Left ventriculography showed an left ventricular (LV) ejection fraction of 60%. Social services were consulted to arrange for clopidogrel therapy as an outpatient. He was discharged home the following day. Inexplicably, he began to use crack cocaine and presented to the ED with an anterolateral ST segment elevation myocardial infarction three days after his initial presentation and a few hours after having smoked crack cocaine (Figure 5). Compliance with dual antiplatelet therapy was verified by checking his home medications. The patient underwent emergent coronary angiography, which revealed thrombus in the mid LAD stents (Figure 6). Left ventriculography was significant for moderate LV systolic dysfunction, anterior and apical akinesis, and an LV ejection fraction of 35%. The patient underwent emergent manual aspiration, as well as AngioJet (MEDRAD Inc, USA) mechanical thrombectomy and balloon angioplasty. Postpercutaneous transluminal coronary angioplasty (PTCA) stent thrombosis was noted to be 80% with restoration of antegrade flow. He was maintained on triple antiplatelet therapy and attended for repeat left heart catheterization three days later with manual thrombectomy and PTCA with minimal residual in-stent thrombosis (Figure 7). The patient was discharged the next day with extensive counselling to discontinue cocaine abuse. A few weeks later, a thalium viability study was performed that revealed a nonviable myocardium in the area supplied by the LAD artery (Figure 8).
Figure 1).
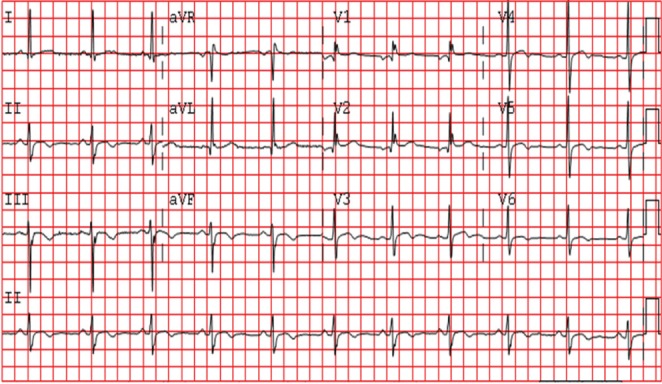
12-lead electrocardiogram at the time of initial presentation
Figure 2).
Chest x-ray film at the time of presentation
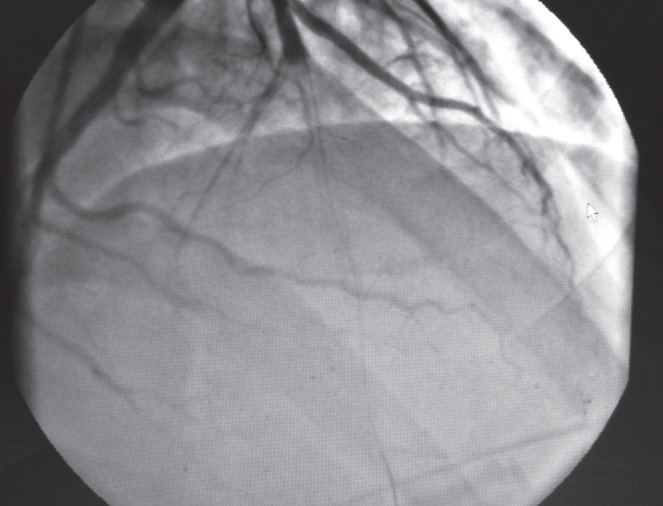
Figure 3).
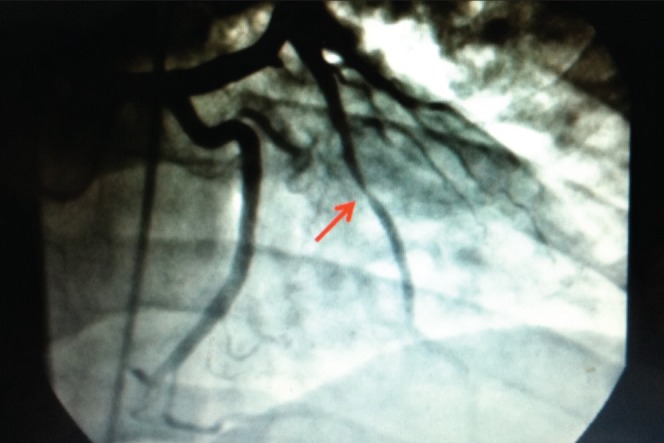
Coronary angiography. The arrow indicates the left anterior descending artery (LAD) stenosis
Figure 4).

Coronary angiography. The arrow indicates the left anterior descending artery after stenting
Figure 5).
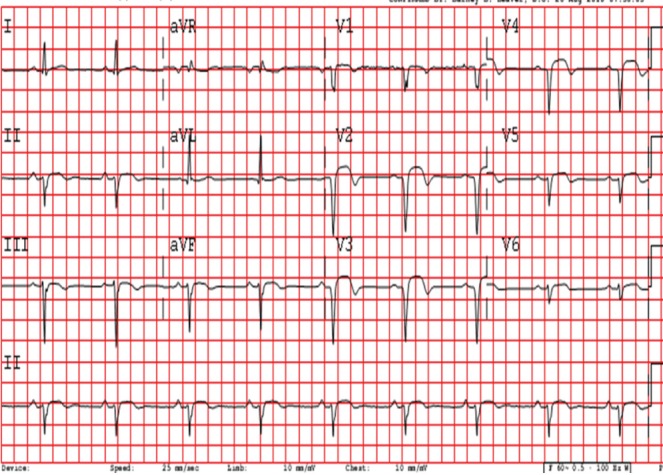
12-lead electrocardiogram at the time of second admission. Sinus bradycardia and acute anterior ST elevation myocardial injury are present
Figure 6).
Coronary angiography. Occlusion of the left anterior descending artery with a wire passing through
Figure 7).
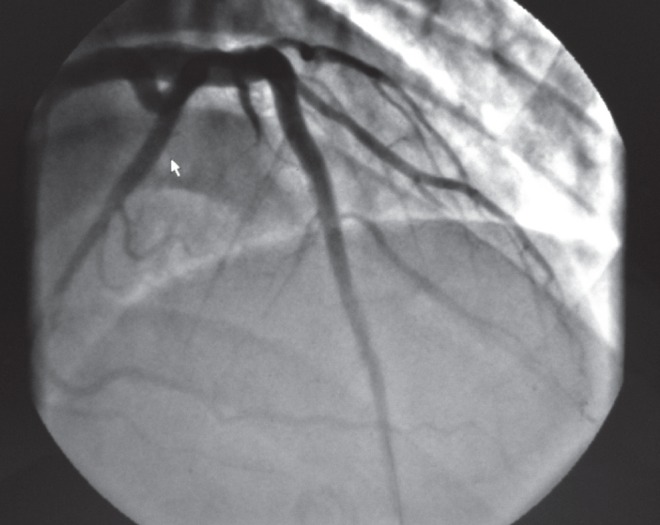
Coronary angiography after percutaneous transluminal coronary angioplasty to the left anterior descending artery
Figure 8).
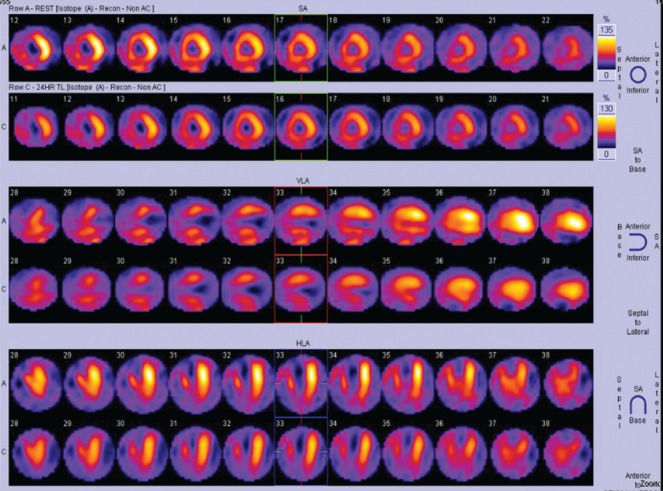
Thallium-201 viability nuclear scan showing decreased uptake in the anteroapical, inferoapical and septal walls
DISCUSSION
It is clear from work performed by Fischman et al (1) and others that restenosis is generally lower in stents than PTCA; however, thrombosis as a complication of coronary intervention is higher in patients with stents compared with PTCA. BMS appear to have a poorer in-stent restenosis rate compared with drug-eluting stents (DES). However, problems with stent thrombosis remain an issue that requires dual antiplatelet drug therapy for at least one month. Thrombosis has been recognized as an important complication since the earliest stent implants (1985 to 1988), with an incidence of up to 16%. Moreover, 15% to 30% of stent thrombosis patients die within 30 days of the event, and virtually all sustain a myocardial infarction (2). Drug regimens have evolved from acetylsalicylic acid, dipyridamole and low-molecular weight dextran to the addition of warfarin, to modern dual-antiplatelet regimens (2–4). The combination of dual-antiplatelet therapy combined with high-pressure stent deployment has reduced the incidence of stent thrombosis with BMS to approximately 0.6% in straightforward lesions (2).
To avoid premature discontinuation of antiplatelet therapy and in-stent thrombosis, a Science Advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians, recommended the following (5):
Health care providers who perform invasive or surgical procedures on patients who have undergone coronary stent placement should contact the patient’s cardiologist to discuss optimal management of the patient’s antiplatelet therapy.
Elective procedures in which discontinuation of dual antiplatelet therapy is believed necessary should be deferred for one month in the case of BMS and 12 months for DES.
Patients treated with DES who undergo procedures that mandate discontinuation of the thienopyridine (clopidogrel or ticlopidine) should remain on acetysalicylic acid if at all possible with the thienopyridine restarted as soon as possible postprocedure.
Although the science advisory recommended discussion with the patient regarding the importance of medication compliance, it did not address prevention of stent thrombosis in patients who use cocaine, although cocaine remains the most commonly abused drug in patients presenting to EDs, accounting for almost 40% of all drug-related visits (6). The National Survey on Drug Use and Health estimated that in 2008, there were 1.9 million current (past month) cocaine users, of which approximately 359,000 were current crack users (7). Recent investigations have shown that cocaine is associated with increased cardiac morbidity and mortality in acute and chronic settings. Acutely, cocaine causes coronary artery vasoconstriction, increases myocardial oxygen demand, and induces platelet aggregation and thrombus formation leading to acute cardiac ischemia regardless of the presence of underlying coronary artery disease (8–10). Rusovici et al (11) reported three cases of severe life-threatening coronary arterial thrombosis manifesting as acute coronary syndromes. The thrombotic occlusions were frequently not superimposed on flow-limiting atherosclerotic lesions. In a similar report, Meltser et al (12) described a case of multi-vessel coronary thrombosis secondary to cocaine use that was successfully treated with multivessel primary angioplasty. In a study investigating cocaine-related sudden death in southwestern Spain, Lucena et al (13) identified coronary thrombosis in 14.3% of patients who died suddenly. However, in patients with acute stent thrombosis in the setting of cocaine abuse, Makaryus et al (14) proposed that a confluence of factors may be responsible, including coronary vessel vasoconstriction, impaired vascular compliance as well as the platelet-activating effect of cocaine. In a study involving 71 cocaine abusers who underwent percutaneous coronary intervention, McKee et al (15) found that stent thrombosis occurred in 7.6% of the stented cocaine abusers during the nine-month follow-up period compared with a stent thrombosis rate of 0.6% rate in the control database. Thus, it was suggested that because of the increased risk of stent thrombosis, consideration should be given to a more conservative approach in cocaine abusers who present with acute coronary syndromes. Similar findings were reported in the same year by Karlsson et al (16), who studied 247 patients who underwent coronary stent placement at an inner-city hospital. It was also identified in this study that patients who actively used cocaine had a markedly higher risk of stent thrombosis compared with patients without a documented history of cocaine use. Although there is a higher chance of stent thrombosis in cocaine users as described previously, early percutaneous coronary intervention is still preferred over fibrinolysis in patients with cocaine-associated myocardial infarction due to the increased risk for intracranial hemorrhage after administration of fibrinolytic agents in cocaine users (17).
Our patient was compliant with his medications for a short period after stent deployment. However, he started smoking crack cocaine and developed a thrombus in a BMS. Cocaine may induce thrombus formation in the coronary arteries or in stents, even in patients who appropriately take dual-antiplatlet therapy, as shown by our patient. Enhanced platelet activation and aggregatability, as well as an increase in the concentration of plasminogen-activator inhibitor, which may promote thrombus formation, have been previously reported. Recently, a report described four patients with BMS and documented cocaine abuse who developed stent thrombosis without restenosis. Noncompliance notwithstanding, it was believed that stent thrombosis could be almost 10 times greater in patients using cocaine (5%) compared with nonusers (0.6%) (2,18). We add to this cohort another patient with documented compliance with acetylsalicylic acid and clopidigrel, according to the current guidelines, in whom stent thrombosis also occurred.
CONCLUSION
In cocaine users who may require a coronary intervention, it appears reasonable to intervene when necessary with balloon angioplasty only, thus obviating the need for long-term dual antiplatelet therapy.
REFERENCES
- 1.Fischman DL, Leon MB, Baim DS, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. N Engl J Med. 1994;331:496–501. doi: 10.1056/NEJM199408253310802. [DOI] [PubMed] [Google Scholar]
- 2.Leon MB, Baim DS, Popma JJ, et al. A clinical trial comparing three antithrombotic-drug regimens after coronary-artery stenting. N Engl J Med. 1998;339:1665–71. doi: 10.1056/NEJM199812033392303. [DOI] [PubMed] [Google Scholar]
- 3.Schomig A, Neumann FJ, Kastrati A, et al. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N Engl J Med. 1996;334:1084–9. doi: 10.1056/NEJM199604253341702. [DOI] [PubMed] [Google Scholar]
- 4.Colombo A, Hall P, Nakamura S, et al. Intracoronary stenting without anticoagulation accomplished with intravascular ultrasound guidance. Circulation. 1995;91:1676. doi: 10.1161/01.cir.91.6.1676. [DOI] [PubMed] [Google Scholar]
- 5.Grines CL, Bonow RO, Casey DE, Jr, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents. A Science Advisory From the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, With Representation From the American College of Physicians. Circulation. 2007;115:813–8. doi: 10.1161/CIRCULATIONAHA.106.180944. [DOI] [PubMed] [Google Scholar]
- 6.Macdonald DI. Cocaine heads ED drug visits. JAMA. 1998;258:2029. [Google Scholar]
- 7.Volkow ND, National Institute on Drug Abuse . Cocaine: Abuse and Addiction. Washington, DC: US Department of Health and Human Services; 2009. [Google Scholar]
- 8.Hollander JE, Hoffman RS. Cocaine induced myocardial infarction: An analysis and review of the literature. J Emerg Med. 1992;10:169–177. doi: 10.1016/0736-4679(92)90212-c. [DOI] [PubMed] [Google Scholar]
- 9.Isner JM, Chckshi SK. Cocaine and vasospasm. N Engl J Med. 1989;321:1604–6. doi: 10.1056/NEJM198912073212309. [DOI] [PubMed] [Google Scholar]
- 10.Minor RL, Scott BD, Brown DD, Winniford MD. Cocaine induced myocardial infarction in patients with normal coronary arteries. Ann Inter Med. 1991;125:1441–3. doi: 10.7326/0003-4819-115-10-797. [DOI] [PubMed] [Google Scholar]
- 11.Rusovici A, Varkey S, Saeed Q, Klapholz M, Haider B, Kaluski E. Cocaine-induced coronary thrombosis: What is the optimal treatment strategy. Cardiovasc Revasc Med. 2011;12:133.e1–6. doi: 10.1016/j.carrev.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Meltser H, Bhakta D, Kalaria V. Multivessel coronary thrombosis secondary to cocaine use successfully treated with multivessel primary angioplasty. Int J Cardiovasc Intervent. 2004;6:39–42. doi: 10.1080/14628840310016871. [DOI] [PubMed] [Google Scholar]
- 13.Lucena J, Blanco M, Jurado C, et al. Cocaine-related sudden death: A prospective investigation in south-west Spain. Eur Heart J. 2010;31:318–29. doi: 10.1093/eurheartj/ehp557. [DOI] [PubMed] [Google Scholar]
- 14.Makaryus JN, Volfson A, Azer V, Bogachuk E, Lee A. Acute stent thrombosis in the setting of cocaine abuse following percutaneous coronary intervention. J Interv Cardiol. 2009;22:77–82. doi: 10.1111/j.1540-8183.2008.00386.x. [DOI] [PubMed] [Google Scholar]
- 15.McKee SA, Applegate RJ, Hoyle JR, Sacrinty MT, Kutcher MA, Sane DC. Cocaine use is associated with an increased risk of stent thrombosis after percutaneous coronary intervention. Am Heart J. 2007;154:159–64. doi: 10.1016/j.ahj.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Karlsson G, Rehman J, Kalaria V, Breall JA. Increased incidence of stent thrombosis in patients with cocaine use. Catheter Cardiovasc Interv. 2007;69:955–8. doi: 10.1002/ccd.21151. [DOI] [PubMed] [Google Scholar]
- 17.McCord J, Jneid H, Hollander JE, et al. Management of cocaine-associated chest pain and myocardial infarction: A scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Circulation. 2008;117:1897. doi: 10.1161/CIRCULATIONAHA.107.188950. [DOI] [PubMed] [Google Scholar]
- 18.Singh S, Rohit A, Ahmad K, et al. Increased incidence of in-stent thrombosis related to cocaine use: Case series and review of literature. J Card Pharm Thera. 2007;12:298–303. doi: 10.1177/1074248407306671. [DOI] [PubMed] [Google Scholar]


