Abstract
This article describes the formation and initial outcomes of a research-community collaborative group that was developed based on community-based participatory research principles. The group includes a transdisciplinary team of practitioners, funding agency representatives, researchers, and families of children with autism spectrum disorders, who partnered to improve community-based care for infants and toddlers at risk for autism through the implementation of evidence-based practices. Data from this group provide support for the feasibility of developing and sustaining a highly synergistic and productive research-community collaborative group who shares common goals to improve community care.
Caring for children with autism spectrum disorders (ASD) represents a significant public health challenge (Landa, Holman, & Garrett-Mayer, 2007). The number of children identified with ASD continues to increase at dramatic rates with recent research estimating a prevalence of 1 in 88 children (Baird et al., 2001; Fombonne, 2003; Centers for Disease Control and Prevention, 2012; Rice et al., 2007). The cost of caring for children with ASD in the United States is estimated at approximately $35–51 billion per year (Ganz, 2006).
Although ASD is not typically diagnosed until after 2 years of age, infants and toddlers with early developmental problems that may be indicative of ASD are being identified much earlier (Landa et al., 2007; Maestro et al., 2005; Zwaigenbaum et al., 2005). Specifically, infants and toddlers who later receive a diagnosis of ASD often exhibit difficulty developing relationships and engaging in reciprocal social interactions necessary for emotional development and learning, verbal and nonverbal communication, sensory regulation, attention, cognition, and affective processes long before a formal diagnosis is made (Landa & Garrett-Mayer, 2006; Zero to Three, 2005; Yirmiya et al., 2006). Early identification provides an opportunity to deliver intervention addressing this symptomatology at its first presentation, which may help ameliorate or reduce later difficulties (Reynolds et al., 2007). Typically, children with social/behavioral concerns receive the majority of early intervention services in community-based systems of care providing early intervention services (e.g., speech/language therapy, occupational therapy, behavioral services, parent training, special educational services; Thomas, Morrissey, & McLaurin, 2007). However, these systems do not have the capacity to effectively intervene with this very young population once ASD-related difficulties have been identified.
Quality early intervention efforts are not misplaced. Cost-benefit analyses of early intervention beginning at 3 years of age for children with ASD indicate that for the 40%–50% of children achieving normal functioning, the savings realized through early intervention is approximately $280,000 by 22 years of age (Ganz, 2007; Jacobson, Mulick, & Green, 1998). Implementation of early interventions with infants and toddlers can potentially decrease the long-term cost of caring for children with ASD and further increase potential savings across the lifespan. On both local and national levels there is a call for capacity building in the area of early childhood mental and developmental health promotion (San Diego County Commission on Children, Youth, and Families, 2003; Zero to Three, 2005; Walsh, 2004).
Researchers posit that intervention across linked areas (behavior, social, communication, regulation) early in development can have a significant positive impact on later intelligence level, grade retention, and use of special education services for children with ASD (Reynolds et al., 2007; Shonkoff & Phillips, 2000). Because social-emotional and communicative competencies expand most rapidly between 9 and 36 months of age, early intervention may affect risk processes in young children by influencing brain circuitry during early periods of plasticity and improve later functioning (Green, Brennan, & Fein, 2002; Kaiser, Hancock, & Nietfeld, 2000; Vismara, Colombi, & Rogers, 2009). Blended interventions based on the principles of behavior analysis combined with developmental teaching have been shown to be effective for very young children (Rogers & Dawson, 2009; Stahmer, Akshoomoff, & Cunningham, 2011) and are now being recommended for children with risk for ASD (Wallace & Rogers, 2010). In addition, parent-implemented interventions are recommended for these very young children due to the importance of the caregiver-child relationship at this early age (National Research Council, 2001; Wallace & Rogers, 2010). These evidence-based interventions, however, have not been translated into community settings where the majority of children can benefit from them (Institute of Medicine, 2001; Stahmer, Collings, & Palinkas, 2005).
The traditional model of translating evidence-based practices (EBPs) into the community is to test an intervention or practice in the community settings only after it has been fully developed and examined in efficacy studies under tightly controlled conditions (Gresham, Beebe-Frankenberger, & MacMillan, 1999). Researchers have called for innovative models of intervention development and implementation that shift from the traditional, unidirectional models of translating research into practice toward a more reciprocal, interactive effort between researchers and practitioners (Bondy & Brownell, 2004; Meline & Paradiso, 2003; Weisz, Chu, & Polo, 2004). Specifically, there have been calls for more bidirectional or multidirectional knowledge exchange involving active collaboration and partnership between researchers and community stakeholders at all stages of the research and the research-practice transfer process (Addis, 2002; Beutler, Williams, Wakefiled, & Entwistle, 1995; Wells & Miranda, 2006).
One promising method of developing community capacity to promote EBPs is through close collaboration with community providers. The use of participatory or collaborative models to develop effective community interventions is congruent with a recent call for a paradigm shift in how intervention research for the ASD population is conducted (Lord et al., 2005). This reframing of the process of intervention research is critical for infants/toddlers with ASD as they may be underserved due to lack of funding and community capacity. Given the status of the evidence and community need for guidelines on how to work with young children with ASD, a collaborative approach among researchers and other ASD stakeholders is a promising method to ensure EBPs are translated in a timely manner for these families. It is hypothesized that, using a collaborative approach, identifying and implementing an EBP for the targeted population/community (Stahmer, Suhrheinrich, Reed, Bolduc, & Schreibman, 2011) will ultimately result in better “fit,” adoption, and sustainability in community settings.
Community-based participatory research (CBPR) is one such collaborative approach often used in the field of public health to reduce inequities in care through active involvement of community members, organizations, and researchers in all aspects of the research process (Israel, Schulz, Parker, & Becker, 1998). It addresses disparities by promoting mutual transfer of expertise and shared decision making between researchers and community members (Israel, Eng, Schulz, & Parker, 2005). Community-partnered participatory research (CPPR) is a form of CBPR that specifically supports efforts to implement EBPs in community-based mental health services (Jones & Wells, 2007). This model was designed to support the use of EBPs in ways consistent with community needs and values (Wells & Miranda, 2004) and has been successfully adapted by mental health researchers to examine the participatory process in collaboratively selecting and testing interventions (Bluthenthal et al., 2006). The model suggests developing clear goals among multiple stakeholders, including education regarding EBPs for community members and on community needs and priorities for researchers, as well as matching community needs with EBP strategies that can then be tailored for community contexts.
The Southern California BRIDGE Collaborative (Stahmer, Brookman-Frazee et al., 2011) is one such research-community partnership developed based on CBPR and CPPR principles that brings together a transdisciplinary team of practitioners, funding agency representatives, researchers, and families of children presenting with ASD to develop a community-wide, sustainable plan for serving infants/toddlers at risk for ASD. The purpose of this article is to (a) describe the formation of the BRIDGE Collaborative, (b) assess proximal outcomes of the research-community partnership, and (c) assess initial sustainability of the group.
METHOD
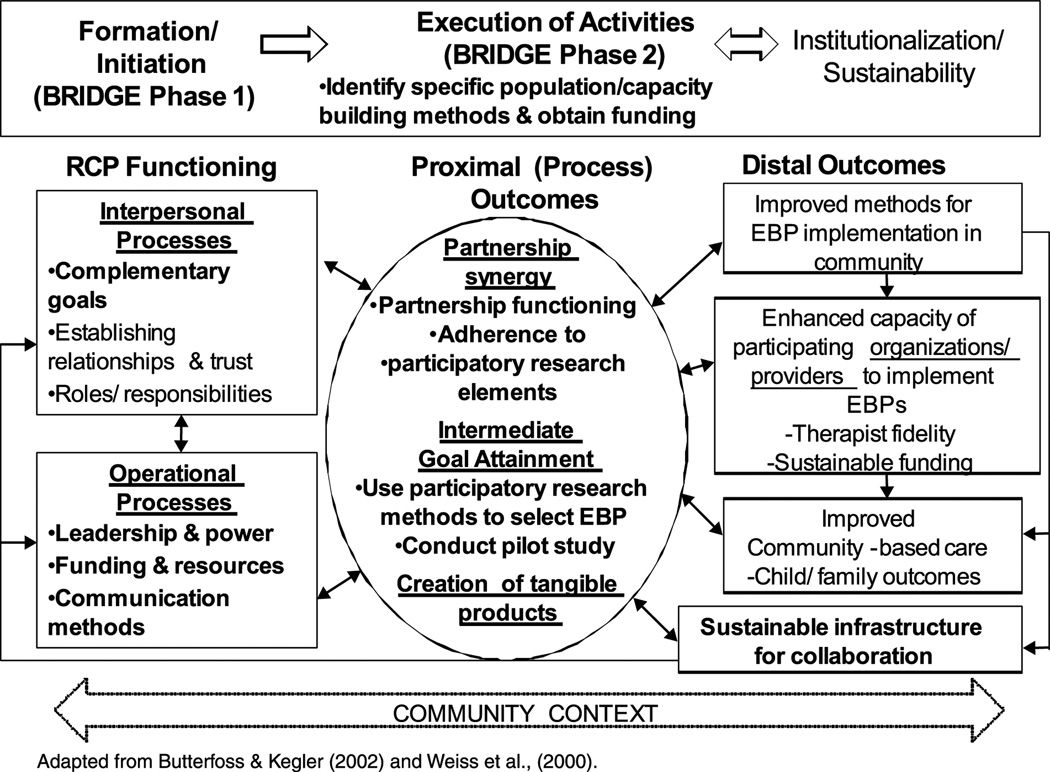
In this section, the development of the BRIDGE Collaborative and procedures for assessing outcomes are described. The description of the BRIDGE Collaborative development and outcomes are framed within a conceptual framework of research-community partnership that draws from the literature from multiple disciplines regarding partnership, collaboration, and knowledge exchange (e.g., Butterfoss & Kegler, 2002; Huxham and Hibbert, 2008; Weiss, Anderson, & Lasker, 2002). Figure 1 illustrates the iterative processes of research-community partnership development and conceptualizes outcome constructs of these efforts. The description of the BRIDGE Collaborative development (Phase 1 and Phase 2), structure of the group (partnership functioning), and outcome measurement (proximal and distal) correspond to elements of this model; elements described or reported in this article are indicated in bold.
Figure 1.
Model of research-community partnership.
Phase 1: Formation (Initiation) of BRIDGE Collaborative
The BRIDGE Collaborative was initiated during 2007 based on conversations between researchers, community providers, and early intervention funding agency representatives all struggling to provide services for children with risk for ASD, who were being identified at increasingly younger ages. Specifically, a local speech-language therapist approached a local researcher to determine methods to examine the effectiveness of intervention provided to very young children in her clinic. At the same time, the local Department of Developmental Services (Regional Center) was attempting to determine appropriate service provision intensity and techniques for this population and a local representative sought advice from researchers. This small group determined that others in the community might have the same interest and began inviting other researchers, clinicians, family members, and funding agency representatives to meet to address these issues. The group began to meet informally (over lunch) on a monthly basis to discuss ideas regarding the population to serve, the type of intervention(s) needed, and the systems on which to focus. Within a few months of the initial meetings, the National Institutes of Health (NIH) issued a call for proposals specifically targeting the development of partnerships through a CBPR mechanism. Therefore, the initial goal of the group was to collaboratively apply for NIH funding as an opportunity to pursue their larger goal to improve early intervention for young children at-risk for ASD.
The eight initial members of the group invited other individuals based on their roles in providing early intervention to this population, in agencies funding services for this population, or as caregivers to a child with ASD, and because they were considered local experts by the community. Initial (and current) participants include 14 individuals (13 female, 1 male), representing 11 agencies, as well as professionals in private practice and individual parents. Characteristics of the participants are listed in Table 1.
Table 1.
Characteristics of BRIDGE Members (n = 14)
| Characteristic | N (%) |
|---|---|
| Gender | |
| Male | 1(7%) |
| Female | 13 (93%) |
| Race/ethnicity | |
| White | 10(71%) |
| Hispanic | 2(14%) |
| African American | 1(7%) |
| Asian | 1(7%) |
| Stakeholder group | |
| Community provider | 6(43%) |
| Funding agency representative | 3(21%) |
| Researcher | 2(14%) |
| Parent | 3(21%) |
| Primary professional discipline | |
| Speech and language pathology | 2(14%) |
| Psychology | 6(43%) |
| Behavior specialist | 1(7%) |
| Occupational therapy | 1(7%) |
| Psychiatry | 1(7%) |
| Parent advocacy/support | 3(21%) |
Note. An additional postdoctoral fellow and a research assistant provide support to the group.
Research Community Partnership (RCP) Functioning: Managing Interpersonal and Operational Processes
Complementary goals
During the first six months of the collaborative the primary target was to identify shared goals and develop a broad mission statement that encompassed the purpose of the group. Initial goals were determined based on the needs that prompted the formation of the group and were revised throughout the first three group meetings, during the process of developing the mission statement. To facilitate this process, the group exchanged specific early intervention ideals with supportive research and a designated recorder wrote them on a white board. Through ongoing discussion, goals not shared by all members of the group were eliminated, with remaining goals matched with level of fundability. The collaborative then modified the language used to more accurately reflect their shared goals and enhance the possibility of funding for the population and intervention. The agreed-upon mission statement was as follows: To build a community dedicated to improving the earliest intervention for children with challenges in relating and communicating.
To enhance visibility and impact in the community, the group jointly named themselves the SoCal BRIDGE Collaborative (to signify the bridge they are building between research and practice, and to stand for their early intervention values: Bond-Regulate-Interact-Develop-Guide-Engage). In addition, the group developed a recognizable logo through one member’s contact with a graphic designer willing to donate time to the project.
Leadership and power
The leadership structure was formalized through consensus among members after the group had been meeting for approximately 6 months. A joint leadership structure, in which a researcher, the community provider that initiated the project and a parent serve as an Operations Group, was developed to ensure that tasks were completed in a clear and timely manner. This subgroup is charged with synthesizing information from the larger group, recommending action steps, and facilitating the completion of actions decided by the larger group. The Operations Group communicates by e-mail or phone approximately semi-monthly and splits tasks based on individual strengths. They also facilitate the monthly full group meetings.
All collaborative members felt one person leading the meetings led to consistency and strength in the group; therefore, the researcher develops an initial agenda and tasks for the meeting, obtains input from one Operations Group, incorporates feedback, and typically leads meeting discussions. To ensure joint decision making, workgroups based on specific tasks are chaired by collaborative members. These groups are comprised of collaborative members, as well as outside consultants who have expertise needed for the group. Example workgroups include a literature review workgroup, a training workgroup, and an assessment workgroup. Workgroup chairs report back on a monthly basis to the collaborative.
Additionally, the Collaborative Process Committee ensures evaluation of the collaborative, reports findings to the group, and recommends changes if needed. It is led by a researcher with experience in qualitative methods and a community provider with extensive collaboration experience.
Funding and resources
In the first year, partnering organizations provided support for BRIDGE, and a number of individuals volunteered their time during the process of writing the NIH grant proposal and while waiting for funding decisions to be made. During the second through fourth year, BRIDGE was supported through NIH funding (MH083893), which provided financial support in the form of an honorarium for the individual collaborative members and funding for materials and a research staff.
Some members contributed time through their agencies. Members received annual honorariums, which are higher for those leading workgroups. Community and research members of the Operations Group were included as investigators and received salary support. Resources such as travel funds for presentations at conferences, supplies, and research assistant support are transparent and procedures are in place to ensure access by all members. Currently, BRIDGE does not have external funding. It continues to operate through contributed time from organizations and individuals as the groups seeks funding from new sources.
Communication methods
Primary communication among members occurs through monthly meetings. Individual workgroups meet as needed and always report to the full group. We have used web-based audio and video communication (primarily Skype and gotomeeting.com) as a method to include members who are unable to physically attend meetings. Meetings typically occur over the lunch hour to facilitate participation. Lunch is consistently provided, which is reported to be an important aspect of encouraging attendance. Additional communication occurs through e-mail, a Google Group and Google Site, where all documents are shared.
Phase 2: Execution of Activities
Since 2004, the group has held monthly lunch meetings at a central community location. As described above, the initial activities involved establishing the goals of the BRIDGE Collaborative.
Identifying specific target population and methods to build community capacity
After determining the broad mission of the group, the collaborative clearly defined the target population and identified methods to build community capacity to serve this population. The group first discussed which population of children and families to target. Many agencies, clinicians, and families had concerns regarding the rapidly increasing numbers of children diagnosed with ASD and the limited services for very young children with this disorder. The group quickly agreed that intervention should be implemented as soon as developmental anomalies were evident but before a clear diagnosis could be made, although this was inconsistent with a majority of current community practices. Review of the literature and discussion of clinician and family experiences moved the group to focus on 12- to 24-month-old children with risk for ASD, using the symptoms described by First Signs as well as signs defined by Zero to Three (Zero to Three, 2005) as indicative of severe disorders of relating and communicating.
Once the population had been defined, the method of building capacity was discussed. The group determined that an evidence-based intervention that would fit the community, build agency capacity, and fit the current funding structure would provide the most support for this population. Members used the American Psychological Association definition of evidence-based practice: “the integration of the best available research with clinical expertise in the context of patient characteristics, culture, and preferences (American Psychological Association Presidential Task Force on Evidence-Based Practice, 2006).” The group was unanimous in their belief that the parent-child relationship was paramount to development in this population and an EBP had the greatest likelihood of being effective and sustainable.
Obtain funding
Once the population was defined, the group submitted and received funding through NIH for initial activities. The specific aims of the project were to (a) develop a coalition for community and research collaboration, (b) identify and adapt an effective, sustainable intervention model for infants and toddlers at-risk for ASD and their families, and (3) conduct feasibility testing of the adapted intervention (pilot study).
Procedures for Evaluating Partnership Outcomes
All outcome measures were collected as part of the evaluation of the partnership process; collection was conducted by the BRIDGE Collaborative Process Committee, a subgroup of members responsible for assessing the functioning and progress of the larger group. This study was approved by affiliated university and hospital research review committees. At the beginning of the study, all members (n = 14) were recruited to participate in the evaluation process (i.e., complete surveys described below). All 14 members provided informed consent to participate (refer to Table 1 and the description of BRIDGE members above). The survey measures are described below. All surveys were administered through a web-based instrument (Survey Monkey) and analyses conducted in SPSS. Other process measures were extracted through study materials (e.g., NIH progress reports, meeting sign in sheets).
Proximal (Process) Outcome Measures
As indicated in Figure 1, outcomes refer to three constructs: partnership synergy, intermediate goal attainment, and creation of tangible projects. “Partnership synergy” refers to a process whereby the knowledge and skills of diverse partners are combined to (a) foster new and better ways to achieve goals, (b) plan innovative, comprehensive programs, and (c) strengthen the relationship with the broader community (Lasker, Weiss, & Miller, 2001; Weiss et al., 2002).
Partnership synergy: Partnership functioning survey
The BRIDGE Collaborative Process Committee adapted a survey from Schulz, Israel, and Lantz (2003) to measure collaborative development, make recommendations for changing the group dynamic, and ensure the process was inclusive and equitable. The resulting survey included 46 questions in seven domains. The domains included general satisfaction, impact, trust, collaborative decision making, community-based research and the research team, organization/structure of meetings, and communication. Each question was rated on a 1–5 Likert scale ranging from 1 (very dissatisfied or highly disagree) to 5 (very satisfied or highly agree). For questions in which a negative response was favorable (e.g., “I often think of having my organization sever its relationship to BRIDGE”), numerical ratings were reversed for analyses so that a higher number always indicated a positive response. This survey was administered via a web-based instrument after the end of Years 1–3 and the middle of Year 4.
Partnership synergy: Adherence to participatory research elements survey
The Naylor, Wharf-Higgins, Blair, Green, and O’Connor (2002) rating scale of participatory research elements was used to summarize the collaborative process across seven participatory elements on a 4-point scale regarding the role of the community ranging from a consultative role, to cooperation, to collaboration, and finally full control. The participatory research elements measured include: (a) identification of need; (b) definition of research goals and activities; (c) mobilization of resources; (d) methodology of evaluation; (e) indicators used to determine success; and (f) sustainability of programs. Respondents were asked to make comments after each question to clarify and expand upon their responses. One hundred percent of BRIDGE Collaborative members participated in each survey (n = 14). As a group, BRIDGE members reviewed all comments that were collected on the surveys and the group then selected representative comments to illustrate the scores on the individual scales.
Intermediate goal attainment
Intermediate goal attainment refers to achieving the aims of the R21 study as this was the focus of most of the group’s activities. Indicators include the number of agencies who participated in the pilot study, number of providers trained in the intervention, and number of children receiving the selected intervention.
Creation of tangible products
This measure was defined as the number of products (a) created by BRIDGE members and (b) related to the work of the BRIDGE Collaborative. They are divided into eight categories: publications, presentations, community recognition/ awards, advocacy, grants/contracts, conferences/trainings held, supplemental intervention materials, and dissemination/marketing tools. The BRIDGE Collaborative members compiled the list and then indicated the target audience of each product (i.e., parents, providers, researchers, funders, policy makers). Tangible products are listed in Table 2.
Table 2.
BRIDGE Collaborative Products (April, 2007–July, 2011)
| Target audience |
|||||
|---|---|---|---|---|---|
| Products | Parents | Providers | Researchers | Funders | Policy makers |
| Publications | |||||
| Stahmer, A.C., Brookman-Frazee, L., Lee, E., Searcy, K., & Reed, S. (2011). Parent and Multi-Disciplinary Provider Perspectives on Earliest Intervention for Children at-risk for Autism Spectrum Disorders. Infants and Young Children, 24, 344–363. |
X | ||||
| Stahmer, A.C., Schreibman, L., & Cunningham, A.B., (2011). Towards a technology of treatment individualization for young children with autism spectrum disorders. Brain Research, 1380, 229–239. (invited) |
X | ||||
| Searcy, K. (2011). Early Intervention for Speech and Language: Empowering Parents. San Diego, CA: Plural Publishing, Inc. |
X | ||||
| Presentations | |||||
| Stahmer, A. “Services research in autism: Translating research into community practice” UCSD Psychology Department Colloquium Series, La Jolla, CA, October 2009. |
X | ||||
| Feder, J. BRIDGE Summary. ICDL Southern California DIR/Floortime Regional Institute, Pasadena, CA, February 13, 2010. |
X | X | |||
| Feder, J. Research Panel, ICDL DIR/Floortime Institute, Washington, DC July 9, 2010 |
X | X | |||
| Feder, J. Getting to Engagement. ICDL Southern California DIR/Floortime Regional Institute, Pasadena, CA, October 9, 2010. |
X | X | |||
| Stahmer, A., & Reed, S. “Bridging the gap between research and community practice” Rady Children’s Autism Workgroup, San Diego, CA, March, 2010. |
X | X | |||
| Stahmer, A. “Effective community-based early intervention for young children with autism” Keynote Address, Autism Society of North Carolina Annual Conference, Chapel Hill, NC, April, 2010. |
X | X | X | ||
| Lee, E., Stahmer, A., Searcy, K., Brookman-Frazee, L., & Reed, S. Earliest Intervention for Young Children with Risk for Autism: What Community Providers and Families Value. Paper presented at the 9th Annual International Meeting for Autism Research, Philadelphia, PA, May, 2010. |
X | ||||
| Stahmer, A. Towards a technology of treatment individualization for young children with Autism. In S. Rogers (Chair) Cutting edge research in behavioral interventions for ASD. Symposium conducted at the Annual Brain Research Meeting: The Emerging Neuroscience of Autism Spectrum Disorders, San Diego, CA, November 2010. |
X | ||||
| Lee, E., & Searcy, K. Early intervention for children at risk for autism: What community providers and families value. Paper presented at Project ABC National Conference, Los Angeles, CA. February, 2011. |
X | X | |||
| Searcy, K., & Stahmer, A. Evidence-based early interventions for infants and toddlers with autism and their caregivers. Paper presented at the California Speech and Hearing Association Annual Meeting, Los Angeles, CA, March 2011. |
X | ||||
| Stahmer, A. “Diffusion of Evidence Based Practice to the Community: Example of Early Intervention” Autism Intervention Research Network for Behavioral Health (AIR-B), Meeting on Evidence Based Practices for Community Based Outreach, Los Angeles, CA May 2011. |
X | ||||
| Lee, E. Earliest intervention for young children with risk for autism: Community feedback. Poster presented at the 118th Annual American Psychological Association Convention, San Diego, CA, August 2010. |
X | ||||
| Searcy, K., Cervantes, L., & Stahmer, A. The BRIDGE Collaborative Project. Presentation to the Chula Vista Community Collaborative. June 2011. |
X | X | |||
| Searcy, K. Earliest intervention for young children with risk for autism: Community feedback. Poster presented at the Infant Development Association Annual Conference; Early Intervention: Practices that Make a Difference. Riverside, CA. April 2010. |
X | ||||
| Searcy, K., & Casper, S. The collaborative process and early intervention: Autism and related disorders. American Speech Language Hearing Association Annual Convention. San Diego, CA. November, 2011. |
X | ||||
| Searcy, K., & Burgeson, M. Communication & behavioral intervention for young children: integrating therapies. American Speech Language Hearing Association Annual Convention. San Diego, CA. November 2011. |
X | ||||
| Community recognition/awards | |||||
| San Diego Community and Youth Roundtable 2011 Knight Award recognizing Dr. Stahmer for her BRIDGE collaborative research with a goal of improving community services |
X | X | |||
| BRIDGE Members (Cook-Clark; Feder; Stahmer) invited to join the San Diego community’s Early Childhood Mental Health Super Leaders group to advance infant and early childhood mental health services in San Diego Community (2011) |
X | X | |||
| Advocacy | |||||
| Feder, J. July 13, 2011, Sacramento, CA California State Senate Select Committee on Autism and Related Disorders Hearing on Autism and Insurance Reform. |
X | ||||
| Grants/contracts— | |||||
| U.S.P.H.S. Research Grant 1R21MH083893–01A1 “Research on Infant/Toddler Mental Health: Building a Community Partnership.” |
X | ||||
| Community Programs Vendored through San Diego Regional Center to provide TSC /BRIDGE intervention: |
|||||
|
|||||
| Kaiser Permanente provides TSC/BRIDGE to their patients in San Diego |
|||||
| Conferences/trainings hosted | |||||
| Ingersoll, B. Teaching Social Communication (TSC) November, 2009 |
X | X | X | ||
| Solomon, R. P.L.A.Y. Project November, 2009 | X | X | X | ||
| Kaiser, A. Enhanced Milieu Teaching (EMT) December, 2009 |
X | X | X | ||
| BRIDGE TSC Training, May 26–27, 2010 | X | ||||
| Intervention materials | |||||
| Supplemental Parent Handouts to Enhance TSC Curriculum |
X | X | |||
| Supplemental Therapist Training Materials to Enhance TSC Curriculum |
X | ||||
| Dissemination/marketing tools | |||||
| BRIDGE Therapist Newsletters (Quarterly since September, 2010) |
X | X | |||
| BRIDGE Website/Fliers www.bridgecollaborative.com |
X | X | X | X | X |
Distal Outcome Measures
Sustainability of partnership infrastructure: Rates of participation in monthly meetings
BRIDGE participation was measured through sign-in sheets completed at each monthly meeting. The participation rate was calculated by dividing the number of people in attendance by the total number of members.
Sustainability of partnership infrastructure: Retention of BRIDGE members
The Principal Investigators of the R21 (second and third authors) maintain a list of all actively participating members that is updated semi-annually. Retention was defined as the percentage of original BRIDGE members who remained members at the time this manuscript was prepared.
RESULTS
Proximal (Process) Outcomes
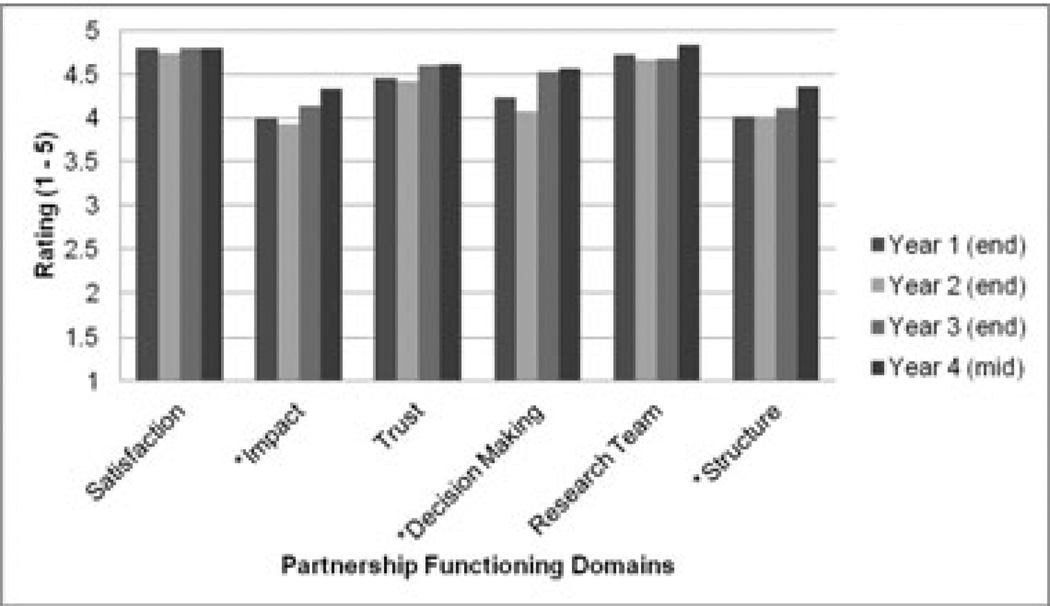
Partnership synergy: Partnership functioning survey
Descriptive statistics were used to evaluate partnership functioning in the six domains. Refer to Figure 2 for mean ratings across the first three and a half years of BRIDGE. Overall, BRIDGE members rated each area positively across all time periods and increases in positive responses are observed to occur over time. Overall satisfaction, trust and perceptions of the research team were initially rated high and remained high during Year 4. Impact ratings increased significantly from Year 1 (mean [M] = 4.01, standard deviation [SD] = 0.32) to Year 4 (M= 4.33, SD = 0.34), t(13) = −2.71, p = .02. It is important to note that the proportion of members reporting that BRIDGE had a positive high impact in the community increased from 64% (Year 1) to 87% (Year 4). Decision-making ratings also increased significantly from Year 1 (M = 4.23, SD = 0.55) to Year 4 (M = 4.56, SD = 0.45); t(13) = −3.37, p = .01. Last, positive ratings of the structure/organization of the group increased significantly from Year 1 (M = 4.02, SD = 0.44) to Year 4 (M = 4.36, SD = 0.48); t(13) = −4.28, p = .001.
Figure 2.
Partnership functioning ratings Year 1–4 (n = 14).
Note. * = Statistically significant increases from Year 1 to Year 4.
Partnership synergy: Adherence to participatory research elements
Refer to Table 3 for the proportion of participants endorsing each of the participatory research elements in the evaluation conducted in Year 4. Results indicate that, overall, participants felt that the researchers had equal decision making power (participation/collaboration), with a small group (22%) reporting that the community controlled that decision making with advice from researchers (full control). The same results were reported for identification of research goals and activities. Representative comments collected from the online survey illustrate the sense of collaboration: “Participation in all aspects of BRIDGE has been the most collaborative to the truest sense of my career. Decisions never felt imposed. My views were frequently sought and valued”; and “This collaborative represents a model for a reflective process in which the leaders create a setting for the participants to problem solve and move forward.”
Table 3.
Participatory Research Elements Evaluation (Year 4; n = 14)
| Role of community |
||||
|---|---|---|---|---|
| Participatory research element |
Consultative (%) |
Cooperation (%) |
Collaboration/ participation (%) |
Full control (%) |
| Identification of need/initial goals for the group |
0 | 0 | 77 | 22 |
| Definition of research goals and activities |
0 | 0 | 77 | 22 |
| Mobilization of resources | 0 | 43 | 57 | 0 |
| Methodology of evaluation | 0 | 25 | 75 | 0 |
| Indicators used to determine success |
0 | 50 | 25 | 25 |
| Sustainability of programs | 0 | 0 | 50 | 50 |
When asked to consider mobilization of resources in terms of who contributed resources, what resources were contributed, how they were mobilized, who benefited from this process, and who decided on the allocation of resources, 57% reported a balance of funding and in-kind services (participation/collaboration), and the rest (43%) felt that the group currently relied on outside funding with advice from experts (cooperation). A member stated, “Although we currently have federal funding, BRIDGE has sustained itself with in-kind contributions from all members/participating organizations. This contributes to the sustainability of the collaborative.”
Members rated the methodology of the evaluation while considering the community’s role in the evaluation process, with whom lay the responsibility for the evaluation, and how evaluation findings were utilized for group process and the research goals. Seventy-five percent reported that they felt they were partners in the design and conduct of evaluation methods that used multiple methods of data collection in natural context (collaboration). The rest (25%) reported they felt evaluation methods were designed by researchers, and conducted by community members, with the significance of results statistically determined (cooperation). One member reported, “The existing survey was adapted by the group to evaluate our process. Qualitative interview questions for intervention evaluation were developed in collaboration, and the group jointly interprets data.”
In terms of the indicators of success used by the group, 50% reported feeling that measures primarily looked at research outcomes but included skill development in planning for evaluation (cooperation). The rest endorsed that findings were used in ongoing planning, that they had increased their knowledge of research, and had high participation in evaluation (collaborative; 25%), or that the results enhanced capabilities for evaluation such that other issues could be examined with a participatory research design (full control; 25%).One person commented, “The enhanced capacities and skills occur at all levels: organization, participant, provider, parents, children. BRIDGE is a generalizable model to address multiple problem types.”
Finally, the group was asked about sustainability of the program in terms of ongoing intervention use, processes, networks, and partnerships. Half of the group members were confident the programs would continue when research funding ended (collaborative) and the other half felt there would also be ongoing initiation of new programs with citizens applying for research funds (full control). One member commented, “Although further research will provide greater implementation and distribution of techniques throughout the community, the program can continue as currently designed.” Another stated, “We are building, have built, a committed community, that is actively seeding other communities and providing enrichment to the revision and improvement of an intervention. It is bigger than most of us, and the loss of one person would not stop its growth.” Overall, this evaluation indicates a general use of collaborative methods and a balance of power in the group.
Intermediate Goal Attainment
Use participatory research methods to select an appropriate EBP for community implementation
This process involved a number of steps (see full description in Stahmer, Brookman-Frazee et al., 2011):
BRIDGE members identified four key components necessary for an intervention to be considered for community presentation: (a) parent-implemented, (b) evidence of efficacy in children with ASD, (c) comprehensive focus across developmental areas, and (d) broad applicability for community providers and parents (across disciplines, theoretical orientation and settings).
BRIDGE members systematically reviewed parent-implemented interventions for very young children with ASD and other difficulties with relating and communicating (e.g., attachment, trauma, language delay), based on established best practices guidelines and published reviews of intervention efficacy.
Interventions were further examined for community fit by the collaborative through review of (a) published peer-reviewed research, (b) intervention materials including treatment manuals, training videos, and (c) discussions with program developers. Based on these factors, the BRIDGE Collaborative members chose three interventions to be reviewed by the community.
Program developers of the final three selected interventions were invited to provide a half-day conference to the community (the order of conferences was based on presenter availability). These interventions included (in alphabetical order) Enhanced Milieu Teaching (EMT; Hancock & Kaiser, 2006), the P.L.A.Y. Project (Play and Language for Autistic Youngsters; Solomon, Necheles, Ferch, & Bruckman, 2007), and Teaching Social Communication (Ingersoll & Dvortcsak, 2010). The community audience completed surveys regarding intervention fit. Ten community providers (representing a variety of agencies and disciplines) and 10 parents of children with ASD provided feedback about early intervention in general and each of the interventions in separate focus groups following conference presentations. BRIDGE members facilitated focus group discussions using a guided interview. The transcripts were independently coded by research, parent, and provider members and reviewed by qualitative experts. The results of mixed qualitative and quantitative analyses indicated that providers and parents had similar views of early intervention needs for the community (Please refer to Stahmer, Brookman-Frazee et al., 2011 for a full description of analytic methods and results regarding a full description of the intervention selection process and discussion of provider and parent intervention values).
BRIDGE members then reviewed the evaluation data from conferences and themes from the focus groups and rated the interventions based on the level of research evidence with the population, quality, availability and usability of the training materials, and fit of the methodology with current community practice. Final intervention selection took place through a collaborative decision-making process of all group members using an outside facilitator. Based on this systematic process, the group chose to adopt the Ingersoll and Dvortcsak (2010) Teaching Social Communication (TSC) curriculum.
Conduct a pilot study to assess EBP feasibility and preliminary outcomes
Through the ongoing pilot study of the TSC intervention selected through the systematic process described above, the BRIDGE Collaborative has trained five community agency supervisors, 10 agency providers, and are providing intervention to 21 infants/toddlers and their families. Preliminary analyses indicate that it is feasible to implement TSC in one community: Treatment was funded through San Diego Regional Center and private insurance; agency supervisors reached fidelity and trained participating therapists from their agency; therapists used the intervention with fidelity; therapists and families are satisfied with the intervention; and all agencies have agreed to ongoing participation in the intervention. Preliminary analyses of child outcomes indicate improvement in child communication and engagement and parent skills to facilitate child social communication skills.
Creation of tangible products
As indicated in Table 2, tangible products to date include three publications; 16 presentations, two community recognition/awards, one advocacy presentation, five grants/contracts, four conferences/trainings, two sets of supplemental intervention materials, and two dissemination/marketing tools. As illustrated in Table 2, products were “led” by multiple BRIDGE members and targeted a range of audiences.
Distal Outcomes
Sustainability of partnership infrastructure: Rates of participation in monthly BRIDGE meetings
Participation at monthly BRIDGE meetings has increased from 70% in Years 1 and 2 to over 85% in Years 3 and 4.
Sustainability of partnership infrastructure: Retention of BRIDGE members
One hundred percent of members who began with the group have remained active participants and 100% of agencies have committed to ongoing participation, indicating good sustainability of the BRIDGE Collaborative.
DISCUSSION
In this study, we examine multiple outcomes of a research-community partnership for early intervention that was developed based on CBPR (Israel et al., 1998) and CPPR (Wells, Miranda et al., 2004) models. Results support initial proximal and initial distal outcomes of the BRIDGE Collaborative. Specifically, data indicate that the group exhibited a high level of partnership synergy (i.e., adhered to the participatory research elements outlined by Naylor et al. (2002) and had strong collaborative functioning). The BRIDGE Collaborative was highly productive as indicated by attainment of all initial goals and the large number of tangible products targeting multiple audiences. Although demonstrating positive impacts of partnerships can be challenging (Butterfoss & Francisco, 2004) and there are no established methods to empirically examine research-community partnership outcomes, this study provides initial empirical support for a research-community partnership approach and some support for measuring process outcomes. Proximal outcomes and initial sustainability data support the potential for future positive distal outcomes.
This study adds to the growing number of examples of research-community partnerships in the field of mental health. To date, partnerships have been employed to conduct practice-based research to characterize community-based mental health care (Garland, 2006), promote knowledge exchange between researchers, practitioners, and service organizations (Sullivan et al., 2005), conduct research that is relevant to practice (McMillen, Lenze, Hawley, & Osborne, 2009), and improve the quality of community-based mental health care overall (Lindamer, Lebowitz, & Hough, 2008; Lindamer, Lebowitz, & Hough, 2009; Wells, Miranda et al., 2004). Although there are examples of research-community partnerships to implement EBPs in community-based mental health services, (Chorpita & Mueller, 2008; Chorpita et al., 2002; Southam-Gerow, Hourigan, & Allin, 2009; Wells, Miranda et al., 2004), this is the first effort to use a partnership model in the field of early intervention for ASD.
A few limitations of this study should be noted. First, the purpose of this study was to report initial outcome data for the formation and processes of the BRIDGE Collaborative. Although the results are promising, it is not known if this model is feasible in other geographic locations that have different structures for community early intervention programs and may not have local services researchers with whom to partner. Additionally, we cannot conclude from our data whether the CBPR model used in this study is more effective at implementing EBPs than other implementation approaches. Last, this study included limited data on distal outcomes.
Despite these limitations, this study also has a number of strengths and implications. First, multiple measures of proximal outcomes were included. Taken together, these data suggest that the BRIDGE Collaborative achieved partnership synergy, met initial goals, and was highly productive. Next steps in this research are to examine the replicability and longer term sustainability of the BRIDGE Collaborative model to implement the selected EBP (TSC) for infants and toddlers at-risk for ASD. It is hypothesized that the BRIDGE model can be successfully adopted and replicated in a new community with high acceptability, penetration of collaboration, shared leadership, and shared decision making. Based on the strong commitment of individual group members and agencies, strong collaborative process, and strong relationships, it is also hypothesized that the BRIDGE Collaborative will continue to demonstrate sustainability.
The potential for sustainability is also supported by the BRIDGE Collaborative’s ongoing process of sustainability planning. At this point, all partners have committed to contributing their time to the group in the absence of grant funding to complete ongoing activities (e.g., revising the TSC treatment manual and training materials in collaboration with the intervention developer). Given the current funding environment, the group is also exploring and pursuing multiple sources of funding outside of federal research grants (multiple, smaller foundation grants, charging agencies small fees to cover training expenses, continued involvement in community boards that fund training that BRIDGE could provide).
Future research also includes examining the large-scale implementation of an EBP for infant mental health intervention in multiple communities. It is hypothesized that the intervention model will be successfully adopted and implemented as evidenced by high therapist fidelity, satisfaction, acceptability, and cost effectiveness ratings. It is also expected that adaptations made to the intervention by the community will actually improve treatment integrity and consistent use of the intervention model. If successful, the project has the potential to demonstrate the usefulness of CBPR approaches in moving evidence-based interventions into the community quickly and with high acceptability. The initial data (see Table 2), which indicated that community agencies have already received contracts to provide the TSC intervention, provide support for the potential large-scale impact of BRIDGE.
Last, further research will examine child-related and family-related outcomes of the intervention to determine public health impact. Based on preliminary data from the pilot study, it is hypothesized that children participating in the intervention will demonstrate improvements in communication, social engagement, and diagnostic outcomes. Further, parents participating in the intervention will report reduced stress, increased feelings of competence and support, and an improved parent-child relationship.
In sum, the BRIDGE collaborative was developed based on participatory research models to improve access to and quality of early intervention for infants and toddlers who are increasingly being identified at risk for ASD. Data from this group provide support for the feasibility of developing and sustaining a highly synergistic and productive group who share common goals to improve community care through the implementation of EBPs.
Acknowledgments
This work was supported by the National Institutes of Health grants K23MH077584 and R21MH083893. Additionally, Dr. Brookman-Frazee is an investigator with the Implementation Research Institute (IRI), at the George Warren Brown School of Social Work, Washington University in St. Louis; through an award from the National Institute of Mental Health (R25 MH080916). The authors thank Ember Lee and Tiffany Wang for their assistance preparing this manuscript; Drs. Ann Garland, Shelia Broyles and Sandra Daley for their input on the original development of the framework used in this study; and all of the BRIDGE Collaborative members for their years of commitment to this group.
Contributor Information
Lauren Brookman-Frazee, Child & Adolescent Services Research Center-San Diego, and University of California, San Diego.
Aubyn C. Stahmer, Child & Adolescent Services Research Center-San Diego
Karyn Lewis, Crimson Center for Speech & Language.
Joshua D. Feder, Interdisciplinary Council on Developmental and Learning Disorders
Sarah Reed, Child & Adolescent Services Research Center at Rady Children’s Hospital-San Diego.
REFERENCES
- Addis ME. Methods for disseminating research products and increasing evidence-based practice: Promises, obstacles, and future directions. Clinical Psychology: Science and Practice. 2002;9(4):367–378. [Google Scholar]
- American Psychological Association. Presidential Task Force on Evidence-Based Practice. Evidence-based practice in psychology. American Psychologist. 2006;61(4):185–271. doi: 10.1037/0003-066X.61.4.271. [DOI] [PubMed] [Google Scholar]
- Baird G, Charman T, Cox A, Baron-Cohen S, Swettenham J, Wheelwright S, Drew A. Current topic: Screening and surveillance for autism and pervasive developmental disorders. Archives of Disease in Childhood. 2001;84(6):468–475. doi: 10.1136/adc.84.6.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beutler L, Williams R, Wakefiled P, Entwistle S. Bridging scientist and practitioner perspectives in clinical psychology. American Psychologist. 1995;50(12):984–994. doi: 10.1037//0003-066x.50.12.984. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Jones L, Fackler-Lowrie N, Ellison M, Booker T, Jones F, Wells KB. Witness for Wellness: Preliminary findings from a community-academic participatory research mental health initiative. Ethnicity Disease. 2006;16(1 suppl 1):S18–S34. [PubMed] [Google Scholar]
- Bondy E, Brownell MT. Getting beyond the research to practice gap: Researching against the grain. Teacher Education and Special Education. 2004;27:47–56. [Google Scholar]
- Butterfoss F, Francisco V. Evaluating community partnerships and coalitions with practitioners in mind. Health Promotion Practice. 2004;5(2):108–114. doi: 10.1177/1524839903260844. [DOI] [PubMed] [Google Scholar]
- Butterfoss F, Kegler MC. Toward a comprehensive understanding of community coalitions: Moving from practice to theory. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research. San Francisco, CA: Jossey-Bass; 2002. pp. 157–193. [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders - Autism and Developmental Disabilities Monitoring Network, United States, 2008. Morbidity and Mortality Weekly Report (MMWR) Surveillance Summaries. 2012;61(3):1–24. [PubMed] [Google Scholar]
- Chorpita B, Mueller C. Toward new models for research, community, an consumer partnerships: Some guiding principles and an illustration. Clinical Psychology: Science and Practice. 2008;15(2):144–148. [Google Scholar]
- Chorpita B, Yim LM, Donkervoet JC, Arensdorf A, Amundsen MJ, McGee C, et al. Toward large-scale implementation of empirically supported treatments for children: A review and observations by the Hawaii Empirical Basis to Services Task Force. Clinical Psychology: Science and Practice. 2002;9(2):165–190. [Google Scholar]
- Fombonne E. The prevalence of autism. Journal of the American Medical Association. 2003;289(1):87–89. doi: 10.1001/jama.289.1.87. [DOI] [PubMed] [Google Scholar]
- Ganz ML. The costs of Autism. In: Moldin SO, Rubenstein JL, Ganz ML, editors. Understanding autism: From basic neuroscience to treatment. 1st ed. Boca Raton, FL: CRC Press; 2006. pp. 475–502. [Google Scholar]
- Ganz ML. The lifetime distribution of the incremental societal costs of autism. Archives of Pediatrics Adolescent Medicine. 2007;161(4):343–349. doi: 10.1001/archpedi.161.4.343. [DOI] [PubMed] [Google Scholar]
- Garland AF, Plemmons D, Koontz L. Research-practice partnership in mental health: Lessons from participants. Administration and Policy in Mental Health. 2006;33:517–528. doi: 10.1007/s10488-006-0062-2. [DOI] [PubMed] [Google Scholar]
- Green G, Brennan LC, Fein D. Intensive behavioral treatment for a toddler at high risk for autism. Behavior Modification. 2002;26(1):69–102. doi: 10.1177/0145445502026001005. [DOI] [PubMed] [Google Scholar]
- Gresham FM, Beebe-Frankenberger ME, MacMillan DL. A selective review of treatments for children with autism: Description and methodological considerations. School Psychology Review. 1999;28(4):559–575. [Google Scholar]
- Hancock TB, Kaiser AP. Enhanced milieu teaching. In: McCauley R, Fey M, editors. Treatment of language disorders in children. Baltimore, MD: Paul Brookes; 2006. pp. 203–233. [Google Scholar]
- Ingersoll B, Dvortcsak A. Teaching social communication to children with autism: A practitioner’s guide to parent training. New York, NY: The Guilford Press; 2010. [Google Scholar]
- Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: Institute of Medicine; 2001. [PubMed] [Google Scholar]
- Israel BA, Eng E, Schulz AJ, Parker EA, editors. Methods in community-based participatory research for health. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- Israel BA, Schulz A, Parker E, Becker A. Review of community-based research: Assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Jacobson JW, Mulick JA, Green G. Cost-benefit estimates for early intensive behavioral intervention for young children with autism - General model and single state case. Behavioral Interventions. 1998;13(4):201–226. [Google Scholar]
- Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. The Journal of the American Medical Association. 2007;197(4):407–410. doi: 10.1001/jama.297.4.407. [DOI] [PubMed] [Google Scholar]
- Kaiser AP, Hancock TB, Nietfeld JP. The effects of parent-implemented enhanced milieu teaching on the social communication of children who have autism. Early Education and Development. 2000;11(4):423–442. [Google Scholar]
- Landa R, Garrett-Mayer E. Development in infants with autism spectrum disorders: A prospective study. Journal of Child Psychology and Psychiatry. 2006;47(6):629–638. doi: 10.1111/j.1469-7610.2006.01531.x. [DOI] [PubMed] [Google Scholar]
- Landa RJ, Holman KC, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry. 2007;64(7):853–864. doi: 10.1001/archpsyc.64.7.853. [DOI] [PubMed] [Google Scholar]
- Lasker RD, Weiss ES, Miller R. Partnership Synergy:A practical framework for studying and strengthening the collaborative advantage. Milbank Quarterly. 2001;79(2):179. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindamer L, Lebowitz B, Hough R. Improving care for older persons with schizophrenia through an academic-community partnership. Psychiatric Services. 2008;59(3):236–239. doi: 10.1176/appi.ps.59.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindamer L, Lebowitz B, Hough R. Establishing an implementation network: lessons learned from community-based participatory research. Implementation Science. 2009;4:1. doi: 10.1186/1748-5908-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Wagner A, Rogers S, Szatmari P, Aman M, Charman T, Yoder P. Challenges in evaluating psychosocial interventions for Autistic Spectrum Disorders. Journal of Autism and Developmental Disorders. 2005;35(6):695–708. doi: 10.1007/s10803-005-0017-6. [DOI] [PubMed] [Google Scholar]
- Maestro S, Muratori F, Cesari A, Cavallaro MC, Paziente A, Pecini C, Sommario C. Course of Autism Signs in the First Year of Life. Psychopathology. 2005;38(1):26–31. doi: 10.1159/000083967. [DOI] [PubMed] [Google Scholar]
- McMillen C, Lenze S, Hawley K, Osborne V. Revisiting practice-based research networks as a platform for mental health services research. Administration and Policy in Mental Health and Mental Health Services Research. 2009;36(5):308–321. doi: 10.1007/s10488-009-0222-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meline T, Paradiso T. Evidence-based practice in schools: Evaluating research and reducing barriers. Language, Speech, Hearing Services in Schools. 2003;34(4):273–283. doi: 10.1044/0161-1461(2003/023). [DOI] [PubMed] [Google Scholar]
- National Research Council. Educating children with autism. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Naylor PJ, Wharf-Higgins J, Blair L, Green L, O’Connor B. Evaluating the participatory process in a community-based heart health project. Social Science and Medicine. 2002;55(7):1173–1187. doi: 10.1016/s0277-9536(01)00247-7. [DOI] [PubMed] [Google Scholar]
- Reynolds AJ, Temple JA, Ou S-R, Robertson DL, Mersky JP, Topitzes JW, Niles MD. Effects of a school-based, early childhood intervention on adult health and well-being: A 19 year follow-up of low-income families. Archives of Pediatrics and Adolescent Medicine. 2007;161(8):730–739. doi: 10.1001/archpedi.161.8.730. [DOI] [PubMed] [Google Scholar]
- Rice CE, Baio J, Van Naarden Braun K, Doernberg N, Meaney FJ, Kirby RS. A public health collaboration for the surveillance of autism spectrum disorders. Paediatric and Perinatal Epidemiology. 2007;21(2):179–190. doi: 10.1111/j.1365-3016.2007.00801.x. [DOI] [PubMed] [Google Scholar]
- Rogers SJ, Dawson G. Early start Denver model for young children with autism: Promoting language, learning, and engagement. Baltimore, MD: The Guildford Press; 2009. [Google Scholar]
- San Diego Commission on Children, Youth, and Families. San Diego County commission on children, youth, and families: Annual report. San Diego, CA: Commission on Children, Youth, and Families; 2003. [Google Scholar]
- Schulz AJ, Israel BA, Lantz P. Instrument for evaluating dimensions of group dynamics within community-based participatory research partnerships. Evaluation and Program Planning. 2003;26(3):249–262. [Google Scholar]
- Shonkoff JP, Phillips PA, editors. From neurons to neighborhoods: The science of early childhood development. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Solomon R, Necheles J, Ferch C, Bruckman D. Pilot study of a parent training program for young children with autism. The PLAY Project Home Consultation program Autism. 2007;11(3):205–224. doi: 10.1177/1362361307076842. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow M, Hourigan S, Allin R. Adapting evidence-based mental health treatments in community settings: Preliminary results from a partnership approach. Behavior Modification. 2009;33(1):82–103. doi: 10.1177/0145445508322624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer A, Akshoomoff NA, Cunningham AB. Inclusion for toddlers with autism spectrum disorders: the first ten years of a community program. Autism. 2011:1–17. doi: 10.1177/1362361310392253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer A, Brookman-Frazee L, Searcy K, Lee E, Reed S, Cervantes L. Parent and multi-disciplinary provider perspectives on earliest intervention for children at-risk for autism spectrum disorders. Infants and Young Children. 2011;24:344–363. doi: 10.1097/iyc.0b013e31822cf700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer A, Collings NM, Palinkas LA. Early intervention practices for children with autism: Descriptions from community providers. Focus on Autism Other Developmental Disabilities. 2005;20(2):66–79. doi: 10.1177/10883576050200020301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer A, Suhrheinrich J, Reed S, Bolduc C, Schreibman L. Classroom Pivotal Response Teaching: A Guide to Effective Implementation. Guilford Press; 2011. [Google Scholar]
- Sullivan G, Duan N, Mukherjee S, Kirchner J, Petty D, Henderson K. The Role of Services Researchers in Facilitating Intervention Research. Psychiatric Services. 2005;56(5):537–542. doi: 10.1176/appi.ps.56.5.537. [DOI] [PubMed] [Google Scholar]
- Thomas KC, Morrissey JP, McLaurin C. Use of autism related services by families and children. Journal of Autism and Developmental Disorders. 2007;37:818–829. doi: 10.1007/s10803-006-0208-9. [DOI] [PubMed] [Google Scholar]
- Vismara LA, Colombi C, Rogers SJ. Can one hour per week of therapy lead to lasting changes in young children with autism? Autism. 2009;13:93–115. doi: 10.1177/1362361307098516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace KS, Rogers SJ. Intervening in infancy: Implications for Autism Spectrum Disorders. Journal of Child Psychology and Psychiatry. 2010;51(12):1300–1320. doi: 10.1111/j.1469-7610.2010.02308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh C. Behavioral health planning and coordination study. San Diego: First 5; 2004. [Google Scholar]
- Weiss ES, Anderson RM, Lasker RD .Making the most of collaboration: Exploring the relationship between partnership synergy and partnership functioning. Health Educ Behav. 2002;29(6):683–698. doi: 10.1177/109019802237938. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Chu BC, Polo AJ. Treatment dissemination and evidence-based practice: Strengthening intervention through clinician-researcher collaboration. Clinical Psychology: Science and Practice. 2004;11(3):300–307. [Google Scholar]
- Wells KB, Miranda J, Bruce ML, Alegria M, Wallerstein N. Bridging community intervention and mental health services research. American Journal of Psychiatry. 2004;161:955–963. doi: 10.1176/appi.ajp.161.6.955. [DOI] [PubMed] [Google Scholar]
- Wells K, Miranda J. Promise of interventions and services research: Can it transform practice? Clinical Psychology: Science and Practice. 2006;13(1):99–104. [Google Scholar]
- Yirmiya N, Gamliel I, Pilowsky T, Feldman R, Baron-Cohen S, Sigman M. The development of siblings of children with autism at 4 and 14 months: Social engagement, communication, and cognition. Journal of Child Psychology and Psychiatry. 2006;47(5):511–523. doi: 10.1111/j.1469-7610.2005.01528.x. [DOI] [PubMed] [Google Scholar]
- Zero to Three. Diagnostic classification of mental health and developmental disorders on infancy and early childhood: Revised edition. Washington DC: Zero to Three; 2005. [Google Scholar]
- Zwaigenbaum L, Bryson S, Rogers T, Roberts W, Brian J, Szatmari P. Behavioral manifestations of autism in the first year of life. International Journal of Developmental Neuroscience. Special Issue: Autism: Modeling Human Brain Abnormalities in Developing Animal Systems. 2005;23(2–3):143–152. doi: 10.1016/j.ijdevneu.2004.05.001. [DOI] [PubMed] [Google Scholar]