Abstract
Study Objectives:
To evaluate whether blue-light-blocking intraocular lens implantation affects the sleep quality of cataract patients.
Design:
Pre-test/post-test experiment.
Setting:
N/A.
Participants:
40 patients having bilateral cataracts with level higher than N3 (LOCS II) nucleus hardness, including 26 females (65%) and 14 males (35%).
Interventions:
Cataract phacoemulsification followed by blue-light-blocking intraocular lens (IOLs, SN60WF, Alcon Laboratories, USA) implantation.
Measurements and Results:
Patients were contacted in site before cataract surgery and followed by telephone at least 2 months later after second-eye surgery. Pittsburgh Sleep Quality Index (PSQI) questionnaires were administered to evaluate sleep quality. Median age of patients was 74 years (IQR 70 to 78). The median PSQI globe scores were 7 before surgery and 4 after surgery (Z = -2.121, p = 0.037). More specifically, there were significant differences on subjective sleep quality (Z = -2.064, p = 0.045), sleep duration (Z = -2.037, p = 0.047) and daytime dysfunction (Z = -2.142, p = 0.034) when compared between before and after surgeries. The ratio of poor sleepers (PSQI > 5) was reduced significantly after surgery (χ2 = 14.532, p < 0.001).
Conclusions:
Blue-light-blocking IOL had a significantly beneficial effect on the sleep quality of cataract patients.
Citation:
Wei X; She C; Chen D; Yan F; Zeng J; Zeng L; Wang L. Blue-light-blocking intraocular lens implantation improves the sleep quality of cataract patients. J Clin Sleep Med 2013;9(8):741-745.
Keywords: Sleep quality, cataract, blue light, IOL, PSQI
With aging, the human lens becomes a strong color filter attenuating light transmission, particularly for the short wavelengths.1 However, light of short wavelength is important in the control of the sleep-wake cycle (circadian rhythm), which is well known as photo entrainment of circadian rhythm. Circadian rhythm is regulated by melatonin produced by the pineal gland. Photo entrainment of circadian rhythm is mainly mediated by intrinsically photosensitive retinal ganglion cells (ipRGC) containing melanopsin that allows melatonin suppression via the retinohypothalamic tract.2 Even though the ipRGCs can function in the absence of rods and cones, their output is normally regulated by input from the rod and cone photoreceptors.3,4
Brainard et al.5 reported the influence of various monochromatic lights on melatonin secretion and found that a peak of the action spectrum at 464 nm. Morita and Tokura6 also indicated that a light with more short wavelengths reduced melatonin secretion and decreased the fall of core temperature in the evening and night, causing an inhibitory effect on nocturnal sleep.
In pathological conditions such as cataract, the reduction in light transmission in the eye can be very dramatic. Short wavelength light plays an important role on the inhibition of melatonin secretion. Therefore cataract patients, whose optical systems transmit light poorly (especially short wavelengths), would be likely to experience sleepiness in the daytime because there is not enough short wavelength light to reduce melatonin secretion. Consequently, they commonly have poor sleep in the night and are susceptible to sleep disturbances. For this reason, cataract surgery may improve not only their sight but also the quality of their sleep. Initially, intraocular lenses (IOLs) implanted during cataract surgery allowed the passage of all the visible light.7 However, it was found erythropsia8 (a temporary distortion of color vision where objects appear with an abnormal reddish hue), photic retinopathy (retinal dysfunction which induced by too much light exposure), and cystoid macular edema9–12 (fluid accumulation in the outer plexiform layer and cyst formation, a common cause of decreased vision following cataract surgery) occurred in patients with these IOLs.
BRIEF SUMMARY
Current knowledge/Study Rationale: For cataract patients, blue-light-blocking intraocular lens (IOLs) have beneficial effect on the retina, it can lower the risk of many retina diseases which are caused by too much light exposure. The ophthalmologist's only concern is whether blue-light-blocking IOLs affect the sleep quality of cataract patients because blue light is important in the control of the sleep-wake cycle.
Study Impact: Based on large sample size in Sichuan, China, our data indicate that blue-light-blocking IOL had a significantly beneficial effect on the sleep quality of cataract patients. Thus blue-blocking intra-ocular implants could be used routinely during cataract phacoemulsification surgery.
Previous works suggest that long time exposure in the blue range (approximately 475 nm) may injure an aging retina and cause photoreceptor damage and possibly lead to the development of other disease processes such as age-related macular degeneration.13–19 Therefore, in recent years, IOLs have been manufactured with a filter that blocks the passage of blue light. Although the filter can protect the posterior segment of the eye in theory, there have been few reports of its advantage, and many researchers still believed that a filter that blocks blue light may have detrimental effects.20–22 Landers and colleagues23 reported that compared to the conventional IOLs, blue-light-blocking IOLs had no detrimental effect on the sleep quality. However, Landers' study lacked assessment of the patient's sleep quality before surgery, and their study was conducted in a geographical region remarkable for its sunny climate. In order to confirm these initial findings in more patients and in a geographical region with less sunshine, we designed a study to evaluate whether cataract phacoemulsification (one kind of cataract extraction surgery, which uses ultrasonic power to emulsify the cataract in to aspirate it from two small incisions) combine blue-light-blocking IOL implantation has an effect on sleep quality based on large sample size in Sichuan, China.
METHODS
Participants
Considering that nucleus hardness is the most important factor for light transmission, 40 bilateral cataract patients with nucleus hardness > level N3 (Lens Opacity Classification System II, LOCS II) were recruited from the outpatient clinic of the Department of Ophthalmology, West China Hospital, Chengdu, China into this study. LOCS II is a grading system for cataract according to the transparency of the lens. Focusing on the nucleus hardness, it can be divided into 4 levels (level N0: transparent nucleus, colorless; N1: soft nucleus, yellow-white color; N2: medium hardness nucleus, yellow color; N3: stiff nucleus, dark brown color). Patients were chosen who required bilateral cataract phacoemulsification followed by blue-light-blocking intraocular lens (SN60WF, Alcon Laboratories, USA) implantation due to visual acuity less than 0.2. To evaluate the nucleus hardness more accurately, 2 doctors provided independent evaluations. If one of these two doctors was not sure the nucleus hardness was > N3, a third doctor provided evaluation. Informed consent was obtained from each patient prior to the beginning of the experiment. Exclusion criteria included: IOL could not implanted during surgery, retinal or optic nerve disorders that might interfere with light perception or color perception (e.g., retinitis pigmentosa, anterior ischemic optic neuropathy, diabetes, glaucoma), color blindness, and inability to complete a questionnaire due to confusion or dementia. Postoperative refractive error and visual acuity were not exclusions.
Study Design
Study design was a pre-test/post-test experiment.
Measurements
Transmission curve measurement
The transmission curves of the blue-light-blocking intraocular lens (+20.0D SN60WF IOL, Alcon Laboratories, USA) and the typical conventional intraocular lens (+20.0D AR40e IOL, Abbott Medical Optics Inc, USA) were obtained by using an UV/Vis Spectrometer Lambda 14 (Perkin-Elmer Lambda; Shelton, CT). The sources are 2 lamps, one halogen and the other deuterium, which can cover both the UV and the visible lights. The apparatus uses 2 monochromators to select the wavelength (λ) accurately. Light passes through the IOLs and is measured before entering the integrating sphere. A suitable cuvette is used to place the IOLs directly in front and covering the complete entrance hole of the integrating sphere. Spectral of the human lenses were adapted from Boettner and Wolter.24
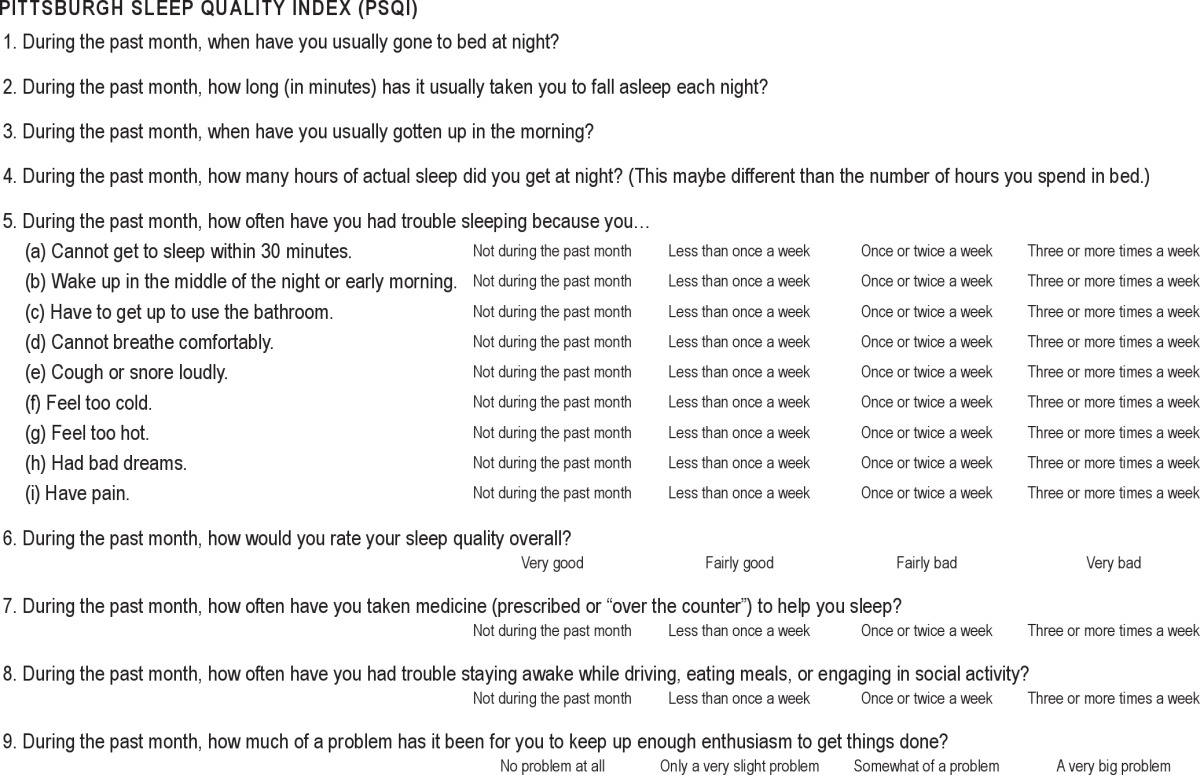
Pittsburgh Sleep Quality Index (PSQI)
The questionnaire administered in this study was the Pittsburgh Sleep Quality Index (PSQI; Table 1). This 17-item questionnaire was designed to assess self-rated sleep quality and disturbances over a 1-month time period and to help investigators distinguish between “good” and “poor” sleepers. The PSQI included 7 component scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, daytime dysfunction, and a total global score. Each component was scored 0 to 3, with 3 indicating the worst score. The highest possible global score is 21; and a score > 5 indicates a poor sleeper. The PSQI has been in clinical use for almost 20 years and over that time has consistently shown robust validity and reliability.25–28 The surgeries of this study were carried out between January 2012 to March 2012. All eligible patients completed the questionnaire within 3 days before their cataract surgery. Investigators did not tell subjects the supposed relationship between IOL and sleep quality. This was followed by a telephone call 2 months later after they completed bilateral surgeries. During the call, the same questionnaire was administered.
Table 1.
The Pittsburgh Sleep Quality Index Questionnaire
Statistical Analyses
Given that the data were not normally distributed, Statistical Analysis System software (SigmaPlot 12.2, SYSTAT) was used for statistical analysis, including Wilcoxon's signed rank test, chi-square test. Medians and interquartile ranges (IQR) were recorded. Odds ratios and 95% confidence intervals were also recorded.
RESULTS
Our study confirmed that in visible light, the shorter wave-length (380-480 nm) light's transmittance of the blue-light-blocking lens (SN60WF) was much lower than that of the conventional intraocular lens (AR40e), but interestingly, it is very close to that of the 53-year-old human's natural crystalline lens at short wavelengths range from 350 nm to 465 nm.
Of 40 patients who were eligible, 26 were women (65%) and 14 were men (35%). The data were not normally distributed, the median age of all patients was 74 years (IQR 70 to 78); of female patients, 73 years (IQR 67 to 79) and of male patients, 75 years (IQR 70 to 80). The median PSQI component score before surgery of all patients was 2 (IQR 0 to 3) for subjective sleep quality, 0 (IQR 0 to 1) for sleep latency, 2 (IQR 0 to 3) for sleep duration, 1 (IQR 0 to 1) for habitual sleep efficiency, 1 (IQR 0 to 2) for sleep disturbances, 0 (IQR 0 to 1) for use of sleeping medication, and 1 (IQR 0 to 1) for daytime dysfunction. The median global score of all patients was 7 (IQR 3 to 13); 30 patients (75%) had a global score > 5 and were considered to be poor sleepers (Table 2).
Table 2.
Pittsburgh Sleep Quality Index scores before and after surgery
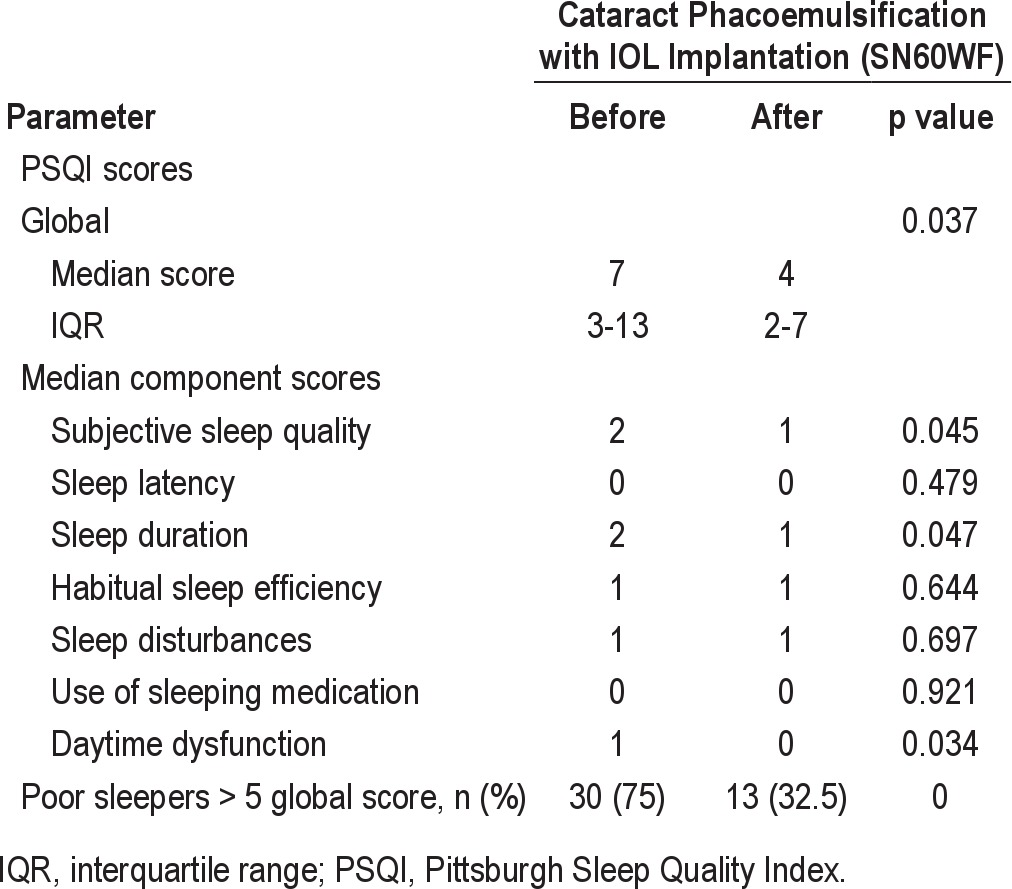
Two months after patients received bilateral cataract phacoemulsification and blue-light-blocking lens implantation, the median PSQI component score of all patients was 1 (IQR 0 to 2) for subjective sleep quality, 0 (IQR 0 to 1) for sleep latency, 1 (IQR 0 to 3) for sleep duration, 1 (IQR 0 to 1) for habitual sleep efficiency, 1 (IQR 0 to 2) for sleep disturbances, 0 (IQR 0 to 1) for use of sleeping medication, and 0 (IQR 0 to 1) for day-time dysfunction. The median global score of all patients was 4 (IQR 2 to 7); only 13 patients (32.5%) had a global scores > 5 and were considered poor sleepers (Table 1).
Between the two timepoints, there was a significant difference in global score (Z = -2.121, p = 0.037). More specifically, there were significant differences in subjective sleep quality (Z = -2.064, p = 0.045), sleep duration (Z = -2.037, p = 0.047), and daytime dysfunction (Z = -2.142, p = 0.034) before and after surgeries (Table 2). As a result of cataract phacoemulsification with blue-light-blocking intraocular lens implantation, 56.67% of subjects went from having an abnormal PSQI (> 5) to normal < 5 PSQI. The ratio of poor sleepers (PSQI > 5) reduced significantly after surgery (χ2 = 14.532, p = 0.000); the odds ratios were 6.231 and 95% confidence intervals were (2.351, 12.513).
DISCUSSION
Any medical device must be evaluated to ensure that it has no adverse effects. Our study found there is beneficial effect to cataract patients on sleep quality after cataract surgery and blue-light-blocking IOL implantation. Patients in our study who with the nucleus hardness over than level N3 (LOCS II) typically slept for a median of 5.5 hours per day, and they slept for 6.5 hours per day after cataract surgery combined blue-light-blocking IOL implantation. Very high ratio (75%) patients before surgery were considered to be poor sleepers as their PSQI scores were greater than 5 and their median PSQI scores were similar with those in a previous population-based assessment of patients of the same age.29
The circadian rhythm is controlled by suprachiasmatic nucleus inhypothalamus30,31 whose activity increases and decreases over a period of nearly 24.5 hours.32 One of its target organs is the pineal gland which secretes melatonin in a cyclical fashion. The secretion of melatonin could induce sleep.32 As mentioned above, the lighttriggered melatonin suppression is most sensitive to blue light, and it has also been proved theoretically that short-wavelength light is important in maintaining a balanced circadian rhythm and a regular sleep-wake cycle.33–36 This suggests that the patients with blue-light-blocking IOLs may be susceptible to sleep disturbances, daytime sleepiness, and insomnia or depression because of the blue light-blocking effect.37 However in stark contrast, our results clearly indicate this is not the case, blue-light-blocking IOLs actually improve the sleep quality of cataract patients. One reason for this phenomenon is that blue-light-blocking IOLs block blue lights only partially. Indeed, based on the spectral transmittance spectral curve as shown in Figure 1, though the blue light transmittance of the blue light-blocking IOL is much lower than that of conventional IOL, but it is very close to that of a 53-year-old human natural lens, which still allows 10% to 70% of 400-500 nm light go through. It seems that this amount of blue lights is sufficient to suppress the melatonin production, and thus keep the circadian rhythm. Another possibility is that patients with blue light-blocking IOL may have more rods, cones, and ipRGCs (as this type of IOL can protect retina from light damages), thus are more sensitive to blue light. This will compensate for the lost blue lights by this type of IOL. This conclusion is consistent with Landers' finding that the sleep quality is the same in cataract patients with conventional IOLs and blue-light blocking IOLs.23
Figure 1. Spectral transmittance curves of the human natural lens at age 53 years, a +20.0D blue-light-blocking IOL(SN60WF) and a +20.0D conventional IOL(AR40e).
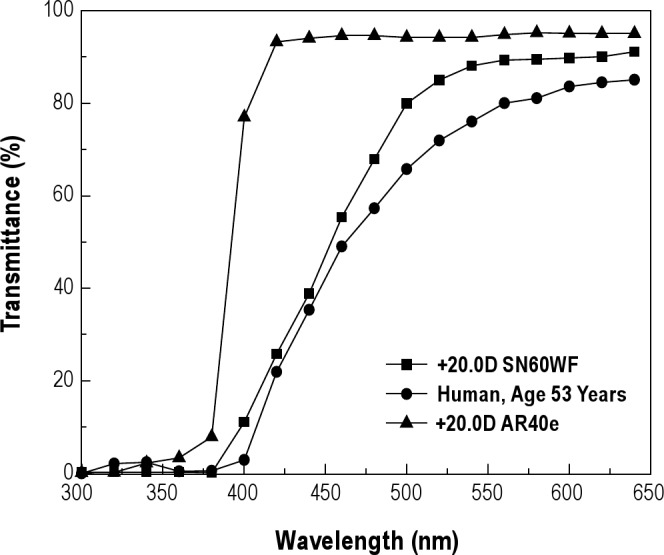
Spectral of the human lenses were adapted from Boettner and Wolter.25
Blue-light-blocking IOLs have beneficial effect on the retina of cataract patients. They could lower the risk of erythropsia,8 photic retinopathy, and cystoid macular edema.9–12 Blue light-blocking IOLs do not reduce visual acuity, contrast sensitivity, color vision,38–41 or scotopic sensitivity42–44 of cataract patients. The ophthalmologist's only concern is whether blue-light-blocking IOLs affect the sleep quality of cataract patients. Based on our data and Landers' results, blue-light-blocking IOL is a good choice for cataract patients because thy have beneficial effects not only on retina, but also on sleep quality.
There are still several limitations of this observation. First, there is no control group, so we cannot compare the sleep quality between conventional IOL and blue-light-blocking IOL implantation. Second, we did not measure other circadian rhythm indicators such as the Horne Ostberg morningness-eveningness questionnaire or core temperatures. While our patients have improved sleep quality, we have no idea if they have a normal circadian rhythm. Third, it is difficult for us to be double-blinded to the treatment, so there might be bias. Nevertheless, our data indicate that blue-light-blocking IOL had a significantly beneficial effect on the sleep quality of cataract patients. Thus blue-blocking intraocular implants could be used routinely during cataract phacoemulsification surgery.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Author contributions: Xin Wei and Lin Wang were responsible for drafting the manuscript, study concept, data acquisition and manuscript revision; Chunyan She, Fangbing Yan, Jihong Zeng, and Liping Zeng were responsible for data acquisition, analysis, and interpretation; Danian Chen provided comments on the manuscript. This work was supported by grants from Natural Science Foundation of China #81200687, Research Fund of Young Scholars For The Doctoral Program of Higher Education of China #20120181120014, and Science and Technology Support Program of Chengdu #12DXYB058JH-002 to Dr. Wei.
REFERENCES
- 1.Brainard GC, Rollag MD, Hanifin JP. Photic regulation of melatonin in humans: ocular and neural signal transduction. J Biol Rhythms. 1997;2:537–46. doi: 10.1177/074873049701200608. [DOI] [PubMed] [Google Scholar]
- 2.Hankins MW, Peirson SN, Foster RG. Melanopsin: an exciting photopigment. Trends Neurosci. 2008;31:27–36. doi: 10.1016/j.tins.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Altimus CM, Guler AD, Alam NM. Rod photoreceptors drive circadian photoen-trainment across a wide range of light intensities. Nat Neurosci. 2010;13:1107–12. doi: 10.1038/nn.2617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dollet A, Albrecht U, Cooper HM, Dkhissi-Benyahya O. Cones are required for normal temporal responses to light of phase shifts and clock gene expression. Chronobiol Int. 2010;27:768–81. doi: 10.3109/07420521003695704. [DOI] [PubMed] [Google Scholar]
- 5.Brainard GC, Hanifin JP, Greeson JM, et al. Action spectrum for melatonin regulation in humans: Evidence for a novel circadian photoreceptor. J Neurosci. 2001;21:6405–12. doi: 10.1523/JNEUROSCI.21-16-06405.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morita T, Tokura H. The influence of different wavelengths of light on human biological rhythms. Appl Hum Sci. 1998;17:91–6. doi: 10.2114/jpa.17.91. [DOI] [PubMed] [Google Scholar]
- 7.Mainster MA. The spectra, classification and rationale of ultraviolet-protective intraocular lenses. Am J Ophthalmol. 1986;102:727–32. doi: 10.1016/0002-9394(86)90400-9. [DOI] [PubMed] [Google Scholar]
- 8.Mainster MA. Solar retinitis, photic maculopathy and the pseudophakic eye. Am Intraoc Implant Soc J. 1978;4:84–6. doi: 10.1016/s0146-2776(78)80112-8. [DOI] [PubMed] [Google Scholar]
- 9.Noell WK, Walker VS, Kang BS, Berman S. Retinal damage by light in rats. Invest Ophthalmol. 1966;5:450–73. [PubMed] [Google Scholar]
- 10.Ham WT, Jr, Mueller HA, Sliney DH. Retinal sensitivity to damage from short wavelength light. Nature. 1976;260:153–5. doi: 10.1038/260153a0. [DOI] [PubMed] [Google Scholar]
- 11.Lawwill T. Three major pathologic processes caused by light in the primate retina: a search for mechanisms. Trans Am Ophthalmol Soc. 1982;80:517–79. [PMC free article] [PubMed] [Google Scholar]
- 12.Mainster MA, Ham WT, Jr, Delori FC. Potential retinal hazards; instrument and environmental light sources. Ophthalmology. 1983;90:927–31. doi: 10.1016/s0161-6420(83)80019-0. [DOI] [PubMed] [Google Scholar]
- 13.Seiler MJ, Liu OL, Cooper NGF, Callahan TL, Petry HM, Aramant RB. Selective photoreceptor damage in albino rats using continuous blue light; a protocol useful for retinal degeneration and transplantation research. Graefes Arch Clin Exp Ophthalmol. 2000;238:599–607. doi: 10.1007/s004170000143. [DOI] [PubMed] [Google Scholar]
- 14.Gorgels TG, van Norren D. Ultraviolet and green light cause different types of damage in rat retina. Invest Ophthalmol Vis Sci. 1995;36:851–63. [PubMed] [Google Scholar]
- 15.vanNorren D, Schellekens P. Blue light hazard in rat. Vision Res. 1990;30:1517–20. doi: 10.1016/0042-6989(90)90032-g. [DOI] [PubMed] [Google Scholar]
- 16.Nilsson SEG, Textorius O, Andersson BE, Swenson B. Does a blue light absorbing IOL material protect the neuroretina and pigment epithelium better than currently used materials? Lasers Light Ophthalmol. 1990;3:1–10. [Google Scholar]
- 17.Young RW. Solar radiation and age-related macular degeneration. Surv Ophthalmol. 1988;32:252–69. doi: 10.1016/0039-6257(88)90174-9. [DOI] [PubMed] [Google Scholar]
- 18.Osborne NN, Lascaratos G, Bron AJ, Chidlow G, Wood JPM. A hypothesis to suggest that light is a risk factor in glaucoma and the mitochondrial optic neuropathies [perspective] Br J Ophthalmol. 2006;90:237–41. doi: 10.1136/bjo.2005.082230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwartz L, Boëlle PY, D'hermies F, Ledanois G, Virmont J. Blue light dose distribution and retinitis pigmentosa visual field defects: a hypothesis. Med Hypotheses. 2003;60:644–9. doi: 10.1016/s0306-9877(02)00391-2. [DOI] [PubMed] [Google Scholar]
- 20.Mainster MA. Intraocular lenses should block UV radiation and violet but not blue light. Arch Ophthalmol. 2005;123:550–5. doi: 10.1001/archopht.123.4.550. [DOI] [PubMed] [Google Scholar]
- 21.Werner JS. Night vision in the elderly: consequences for seeing through a “blue filtering” intraocular lens. Br J Ophthalmol. 2005;89:1518–21. doi: 10.1136/bjo.2005.073734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mainster MA. Violet and blue light blocking intraocular lenses: photoprotection versus photoreception [perspective] Br J Ophthalmol. 2006;90:784–92. doi: 10.1136/bjo.2005.086553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Landers JA, Tamblyn D, Perriam D. Effect of a blue-light-blocking intraocular lens on the quality of sleep. J Cataract Refract Surg. 2009;35:83–8. doi: 10.1016/j.jcrs.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 24.Boettner EA, Wolter JR. Transmission of the ocular media. Invest Ophthalmol. 1962;1:776–83. [Google Scholar]
- 25.Doi Y, Minowa M, Uchiyama M. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000;97:165–72. doi: 10.1016/s0165-1781(00)00232-8. [DOI] [PubMed] [Google Scholar]
- 26.Jankelowitz L, Reid KJ, Wolfe L, Cullina J, Zee PC, Jain M. Cystic fibrosis patients have poor sleep quality despite normal sleep latency and efficiency. Chest. 2005;127:1593–9. doi: 10.1378/chest.127.5.1593. [DOI] [PubMed] [Google Scholar]
- 27.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–40. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 28.Cole JC, Motivala SJ, Buysse DJ, Oxman MN, Levin MJ, Irwin MR. Validation of a 3-factor scoring model for the Pittsburgh Sleep Quality Index in older adults. Sleep. 2006;29:112–6. doi: 10.1093/sleep/29.1.112. [DOI] [PubMed] [Google Scholar]
- 29.Zeitlhofer J, Schmeiser-Rieder A, Tribl G, Rosenberger A, Bolitschek J. Sleep and quality of life in the Austrian population. Acta Neurol Scand. 2000;102:249–57. doi: 10.1034/j.1600-0404.2000.102004249.x. [DOI] [PubMed] [Google Scholar]
- 30.Moore RY. Neural control of the pineal gland. Behav Brain Res. 1995;73:125–30. doi: 10.1016/0166-4328(96)00083-6. [DOI] [PubMed] [Google Scholar]
- 31.Teclemariam-Mesbah R, Ter Horst GJ, Postema F, Wortel J, Buijs RM. Anatomical demonstration of the suprachiasmatic nucleus-pineal pathway. J Comp Neurol. 1999;406:171–82. [PubMed] [Google Scholar]
- 32.Sack RL, Brandes RW, Kendall AR, Lewy AJ. Entrainment of free-running circadian rhythms by melatonin in blind people. N Engl J Med. 2000;343:1070–7. doi: 10.1056/NEJM200010123431503. [DOI] [PubMed] [Google Scholar]
- 33.Sasseville A, Paquet N, Sévigny J, Hébert M. Blue blocker glasses impede the capacity of bright light to suppress melatonin production. J Pineal Res. 2006;41:73–8. doi: 10.1111/j.1600-079X.2006.00332.x. [DOI] [PubMed] [Google Scholar]
- 34.Munch M, Kobialka S, Steiner R, Oelhafen P, Wirz-Justice A, Cajochen C. Wavelength-dependent effects of evening light exposure on sleep architecture and sleep EEG power density in men. Am J Physiol Reg Integ Comp Physiol. 2006;290:R1421–8. doi: 10.1152/ajpregu.00478.2005. [DOI] [PubMed] [Google Scholar]
- 35.Cajochen C, Jud C, Munch M, Kobialka S, Wirz-Justice A, Albrecht U. Evening exposure to blue light stimulates the expression of the clock gene PER2 in humans. Eur J Neurosci. 2006;23:1082–6. doi: 10.1111/j.1460-9568.2006.04613.x. [DOI] [PubMed] [Google Scholar]
- 36.Glickman G, Byrne B, Pineda C, Hauck WW, Brainard GC. Light therapy for seasonal affective disorder with blue narrow-band light-emitting diodes (LEDs) Biol Psychiatry. 2006;59:502–7. doi: 10.1016/j.biopsych.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 37.Patel JI. Is cataract surgery a risk factor for progression of macular degeneration? Curr Opin Ophthalmol. 2007;18:9–12. doi: 10.1097/ICU.0b013e3280112a0f. [DOI] [PubMed] [Google Scholar]
- 38.Cionni RJ, Tsai JH. Color perception with AcrySof Natural and AcrySof single-piece intraocular lenses under photopic and mesopic conditions. J Cataract Refract Surg. 2006;32:236–42. doi: 10.1016/j.jcrs.2005.12.129. [DOI] [PubMed] [Google Scholar]
- 39.Leibovitch I, Lai T, Porter N, Pietris G, Newland H, Selva D. Visual outcomes with the yellow intraocular lens. Acta Ophthalmol Scand. 2006;84:95–9. doi: 10.1111/j.1600-0420.2005.00607.x. [DOI] [PubMed] [Google Scholar]
- 40.Hayashi K, Hayashi H. Visual function in patients with yellow tinted intraocular lenses compared with vision in patients with non-tinted intraocular lenses. Br J Ophthalmol. 2006;90:1019–23. doi: 10.1136/bjo.2006.090712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Landers J, Tan T-H, Yuen J, Liu H. A comparison of visual function following implantation of Acrysof Natural intraocular lenses with conventional intraocular lenses. Clin Exp Ophthalmol. 2007;35:152–9. doi: 10.1111/j.1442-9071.2006.01434.x. [DOI] [PubMed] [Google Scholar]
- 42.Schwiegerling J. Blue-light-absorbing lenses and their effect on scotopic vision. J Cataract Refract Surg. 2006;32:141–4. doi: 10.1016/j.jcrs.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 43.Greenstein VC, Chiosi F, Baker P, et al. Scotopic sensitivity and color vision with a blue-light-absorbing intraocular lens. J Cataract Refract Surg. 2007;33:667–72. doi: 10.1016/j.jcrs.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Muftuoglu O, Karel F, Duman R. Effect of a yellow intraocular lens on scotopic vision, glare disability, and blue color perception. J Cataract Refract Surg. 2007;33:658–66. doi: 10.1016/j.jcrs.2006.12.018. [DOI] [PubMed] [Google Scholar]


