Abstract
Objective
The purpose of this study was to determine the impact of different clamping strategies during CABG on the incidence of postoperative stroke.
Methods
In this case-control study, all patients at Emory hospitals from 2002–2009 with postoperative stroke after isolated CABG (N=141) were matched 1:4 to a contemporaneous cohort of patients without postoperative stroke (N=565). Patients were matched according to the Society of Thoracic Surgeons (STS) Predicted Risk of Postoperative Stroke (PROPS), which is based on 26 variables. On- (ONCAB) and off-pump (OPCAB) patients were matched separately. Multiple logistic regression analysis with adjusted odds ratios (OR) was performed to identify operative variables associated with postoperative stroke.
Results
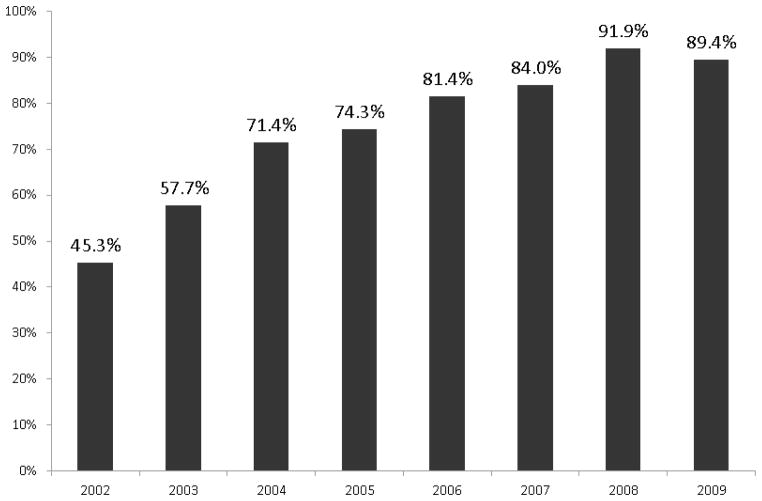
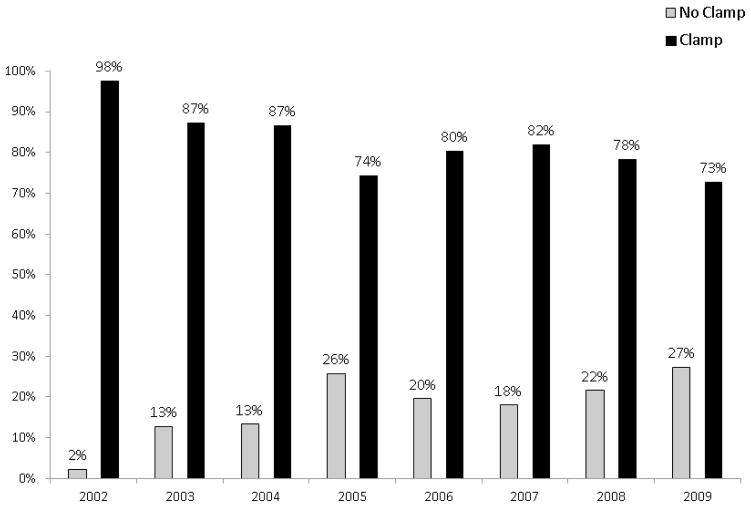
Among the ONCAB cohort, the single cross-clamp technique was associated with a decreased risk of stroke compared to the double clamp (cross clamp + partial clamp) technique (OR=0.385, p=0.044). Within the OPCAB cohort, there was no significant difference in stroke according to clamp use. Epiaortic ultrasound of the ascending aorta increased from 45.3% in 2002 to 89.4% in 2009. From 2002–2009, clamp use decreased from 97.7% of cases to 72.7%.
Conclusions
During ONCAB, the use of a single cross-clamp compared to the double clamp technique decreases the risk of postoperative stroke. The use of any aortic clamp has decreased and epiaortic ultrasound use has increased from 2002–2009, indicating a change in operative technique and surgeon awareness of the potential complications associated with manipulation of the aorta.
INTRODUCTION
Coronary artery bypass surgery (CABG) is the most commonly performed operation by cardiothoracic surgeons. Postoperative stroke is a rare but major cause of morbidity and mortality in patients undergoing CABG. Several operative techniques have been utilized in attempts to minimize the detrimental morbidity and mortality associated with postoperative stroke. Since increased ascending aortic manipulation has been proposed as the primary mechanism for postoperative cerebral atheroembolism, the focus has concentrated on innovative techniques to minimize manipulation of the ascending aorta.
Postoperative stroke occurs in approximately 2% of CABG cases.1,2 Survival among CABG patients at both one and five years is significantly reduced in patients who have had a postoperative stroke compared to those who have not.3 Furthermore, postoperative stroke is also a major source of increased healthcare costs. Compared to those without a postoperative stroke, an additional $19,000 in hospital costs have been attributed to patients with a postoperative stroke.4 Moreover, in patients with a postoperative stroke and two or more complications, greater than $58,000 additional hospital cost has been reported.4
The majority of CABG procedures in the US are performed with cardiopulmonary bypass support. Two different clamping strategies are utilized for the construction of proximal aortocoronary anastomoses: single clamping or double clamping. With off-pump coronary artery bypass (OPCAB), a partial clamp is frequently utilized for construction of proximal anastomoses. However, a clampless approach is possible with facilitating devices (Heartstring™, Maquet Cardiovascular LLC, San Jose, CA) or anastomotic connectors. These devices can be selectively deployed on relatively disease-free portions of the aorta to minimize the risk of atheroembolism. Therefore, the purpose of this study was to test the hypothesis that aortic clamping was associated with an increased risk of stroke. Furthermore, we wanted to determine the impact of different clamping strategies for performing proximal anastomoses on the incidence of postoperative stroke.
METHODS
Patients
Emory University’s Institutional Society of Thoracic Surgeons (STS) Adult Cardiac Database was queried for all patients (cases) with postoperative stroke after isolated, primary CABG. Controls were selected from the entire cohort without postoperative stroke. All consecutive patients from January 1, 2002 to December 31, 2009 were included in the database query.
Design
This study was a retrospective, single center, case-control study. A case-control study design was chosen because operative details about aortic clamping methods are not currently available in the STS database. Operative reports were reviewed and detailed data collected about surgical strategy including on-pump or off-pump approach, details about aortic clamping methods, and the extent of aortic atherosclerosis measured by epiaortic ultrasound. This data was then merged with the STS database to produce the complete dataset. The Institutional Review Board at Emory University in compliance with HIPAA regulations and the Declaration of Helsinki approved the study. The Institutional Review Board waived the need for individual patient consent.
Exclusions
Patients undergoing concomitant cardiac operations, redosternotomy, or emergency CABG were excluded from this study.
Matching algorithm
A predicted risk of postoperative stroke score (PROPS), as part of the STS database, is calculated based on 26 preoperative variables believed to be associated with an increased risk of postoperative stroke. The PROPS score has been identified as a reliable predictor for postoperative stroke by Shroyer et al.5 Controls were matched to the cases in a 1:4 ratio based on PROPS score as well as whether the patient was placed on cardiopulmonary bypass (ONCAB) or not (OPCAB). Since the effect of on- vs. off-pump strategy on postoperative stroke was not the goal of this study, the use of cardiopulmonary bypass was used as part of the matching algorithm. On-pump controls were matched to on-pump cases and off-pump controls to off-pump cases. An optimal matching algorithm was used which is designed to identify the best cutpoint for a continuous variable.6 The optimal matching algorithm is utilized as a SAS macro that defined a distance measure between cases and controls based on PROPS. The control chosen for each case is one that is closest to the case in terms of the distance measure produced by the optimal matching algorithm. This algorithm sequentially matched each stroke patient with potential non-stroke controls by calculating the multivariate distance between the patients based on the 26 variables that comprise the PROPS. The algorithm chooses the set of matches that minimizes the sum of the multivariate distances across all possible sets of matches.
Surgical Technique
For the entire cohort, the overall effect of any aortic clamping was examined for the entire cohort. For ONCAB patients, the two most common clamping strategies were the single cross-clamp and double cross-clamp technique. Other on-pump CABG strategies used by surgeons included on-pump beating heart CABG. In this cohort, 25 patients underwent on-pump beating heart CABG, 15 of these had proximals performed with a partial occluding clamp, and 10 with a Heartstring device. There was only 1 CABG performed under cold fibrillatory arrest. For all other on-pump cases, either a single clamp or double clamp technique was used.
For patients undergoing OPCAB, the strategies examined in this study were the use of a partial-occluding clamp, the use of clampless facilitating devices, and the “no-touch” technique that involves the use of in situ arterial grafts (no aortocoronary proximal anastomoses). A “no-touch” aortic technique was used in 45 OPCAB patients.
Epiaortic Ultrasound
At Emory University, all patients currently undergoing cardiac operations routinely have the aorta evaluated by epiaortic ultrasound. It has become gradually adopted since its implementation in 2002 for patients in whom a clamp is being considered, making it the current standard of care within our institution. It is the test of choice for identifying atherosclerotic lesions within the aorta, and it is superior to transesophageal echocardiography and palpation alone.7–9 Alternative preoperative imaging with computed tomography is another option. Before the aorta is manipulated, patients undergo epiaortic ultrasound examination to grade the amount of atherosclerotic disease within the ascending aorta according to thickness and presence of mobile atheroma. The aorta is graded 1–5: 1-normal (<2 mm thickness); 2-minimal disease (2–3 mm); 3-moderate disease (3–5 mm); 4-severe disease (>5 mm); and 5-indicating the presence of a mobile plaque with any portion of the ascending aorta.
Outcome
Postoperative stroke was the primary outcome of this study. Stroke was defined as a new, focal, permanent neurological deficit on clinical exam diagnosed by an attending neurologist and confirmed with either brain computed tomography or magnetic resonance imaging. Clinical and radiological exam was used to differentiate stroke from transient ischemic attack or postoperative delirium.
Statistical Analysis
A conditional logistic regression analysis was performed to evaluate the effect of clamp versus no-clamp on postoperative stroke controlling for matching factors (PROPS and pump) and epiaortic grade. Epiaortic grade was controlled for as both an ordinal (1,2,3,4,5) and a dichotomous variable (1–2 vs. 3–5) in the regression analysis. The analysis was also performed without controlling for epiaortic grade, as its use was not ubiquitous until recently. In addition, the effect of different clamping or non-clamping strategies within on- and off-pump cases and controls was evaluated using conditional logistic regression. In the original model that looked at the association of any clamping strategy with postoperative stroke incidence, potential preoperative confounding variables were controlled for by the matching algorithm for PROPS (Table 1). The effect of cardiopulmonary bypass, or on-pump, as a potential confounder was also controlled for in the matching strategy, since cases were matched separately to controls based on whether or not an on- or off-pump strategy was utilized. To determine if the year of surgery confounded the analysis, year was also analyzed separately in modifications of the model.
Table 1.
Preoperative Demographic Data
| Variable | Postoperative Stroke (N=141) | No Postoperative Stroke (N=565) | p value |
|---|---|---|---|
| Age (mean ± SD) | 65.7 ± 10.6 | 66.8 ± 10.3 | 0.65 |
| Male (%) | 82 (58.2) | 353 (62.5) | 0.35 |
| Body Mass Index (mean ± SD) | 29.0 ± 6.9 | 28.7 ± 6.5 | 0.62 |
| Preoperative Stroke (%) | 33 (29.7) | 103 (20.6) | 0.04 |
| Cerebrovascular Disease (%) | 44 (31.2) | 161 (28.6) | 0.54 |
| Hypertension(%) | 127 (90.1) | 504 (89.4) | 0.81 |
| Diabetes (%) | 70 (49.7) | 256 (45.4) | 0.36 |
| Renal Insufficiency (%) | 16 (11.4) | 57 (10.1) | 0.67 |
| History of Smoking (%) | 59 (63.4) | 330 (69.8) | 0.23 |
| Left Main disease (%) | 35 (25.0) | 187 (33.3) | 0.06 |
| Prior Myocardial Infarction (%) | 50 (53.8) | 260 (55.0) | 0.83 |
| Peripheral Vascular Disease (%) | 34 (24.1) | 109 (19.4) | 0.21 |
| Arrhythmia (%) | 18 (12.8) | 70 (12.4) | 0.90 |
| PROPS score (mean % ± SD) | 2.6 ± 2.2 | 2.6 ± 2.2 | 0.93 |
Within each subset of operative strategy (on- or off-pump), separate models were developed to determine the association of different clamping strategies on the incidence of postoperative stroke, controlling for PROPS and epiaortic grade. Within the ONCAB group, a double clamping strategy was compared to a single cross-clamp strategy. Within the OPCAB group, a partial-clamping strategy was compared to a Heartstring only strategy and a partial-clamping strategy was compared to a no-clamp strategy (Heartstring or no-touch technique).
In addition to logistic regression analysis, descriptive analyses were performed to be able to assess trends in clamp use as well as trends in risk profiles and epiaortic use. All analyses were performed using SAS Version 9.2 (Cary, NC). All comparisons were made at the 0.05 alpha level.
RESULTS
Cases and controls were selected from a total cohort of 10,054 consecutive patients undergoing primary isolated CABG at Emory University Hospitals. From this cohort, 141 cases (1.4%) of postoperative stroke were identified (1.4%). From the remaining patients, 565 controls (patients without postoperative stroke) were selected based on the matching algorithm. Epiaortic ultrasound data was not performed in 181 (25.6%) patients in the study.
Multiple logistic regression modeling was performed with the effect of cardiopulmonary bypass (pump), PROPS, and epiaortic grade controlled for in the model for the entire cohort (on- and off-pump patients). When epiaortic grade was controlled for as an ordinal variable (grade 1–5) in the logistic regression analysis, the odds ratio for postoperative stroke was estimated at 1.19 (95% CI 0.53–2.67) for use of any aortic clamp. With epiaortic grade controlled for as a dichotomous variable (low-grade=grade 1–2, high-grade=grade 3–5), the odds ratio was 1.46 (95% CI 0.60–3.56). Because this excluded 181 patients in who epiaortic ultrasound was not performed, the analysis was also performed without controlling for epiaortic grade to include all patients in the study. The estimated odds ratio for this analysis was 1.28 (95% CI 0.76–2.17).
Within the ONCAB cohort, the double-clamp technique was associated with a increased risk of postoperative stroke in comparison to the single cross-clamp technique (OR=2.60, p=0.044) (Table 2). When history of preoperative stroke was included in the regression model, the increased risk of stroke with the double-clamp technique was increased (OR=3.29, p=0.05). Within the OPCAB cohort, no difference was found between partial clamping and no clamping (Table 2).
Table 2.
Comparison According to Pump
| Analysis** | Odds Ratio | 95% CI |
|---|---|---|
| On-pump double clamp (cross-clamp + partial clamp) vs. single clamp | 2.60 | 1.03–6.67 (p=0.044) |
| Off-pump partial clamp vs. off-pump Heartstring | 1.46 | 0.49–4.4 |
| Off-pump partial clamp vs. No clamp (Heartstring + no touch) | 1.21 | 0.48–3.03 |
controlled for epiaortic grade
Epiaortic ultrasound grading was performed in 525 patients (74.4%): 450 (85.7%) had Grade 1–2 aortic disease and 75 (14.3%) had Grade 3–5 disease (Table 3). In patients with epiaortic Grades 3–5, a clampless technique was used in 59.5%, 83.3%, and 93.3% of cases, respectively. In patients with Epiaortic Grades 1–2, clampless techniques were used in only 3.8% and 7.8%, respectively. Epiaortic ultrasound use trended upwards from 45.3% of cases in 2002 to 89.4% in 2009 (Figure 4). Clamp use in general trended downwards from 97.7% of cases in 2002 to 72.7% of cases in 2009 (Figure 5). In the 15 patients with Grade 5 aortic disease, a clampless approach was used in 14 patients and there was no postoperative stroke among any of the Grade 5 patients. Among the postoperative stroke patients that had epiaortic ultrasound exams (n=114), 70 (22.2%) occurred in patients with Grade 1 aortic disease, 27 (21.1%) occurred in patients with Grade 2, 9 (21.4%) occurred in patients with Grade 3, 4 (22.2%) occurred in patients with Grade 4, and none occurred in patients with Grade 5 aortic disease. Year of surgery was evaluated in all analyses and was not found to be significantly associated with the risk of postoperative stroke. Furthermore, surgeon identity was evaluated in the analysis and also found not to be associated with risk of postoperative stroke. The PROPS score ranged from 2.0–3.1 and did not significantly change over the course of the study period.
Table 3.
Clamp use according to epiaortic grade
| Epiaortic Grade | No Clamp (N=79) | Clamp (N=446) | Total |
|---|---|---|---|
| 0 | 3 (42.9%) | 4 (57.1%) | 7 |
| 1 | 12 (3.8%) | 303 (96.2%) | 315 |
| 2 | 10 (7.8%) | 118 (92.2%) | 128 |
| 3 | 25 (59.5%) | 17 (40.5%) | 42 |
| 4 | 15 (83.3%) | 3 (16.7%) | 18 |
| 5 | 14 (93.3%) | 1 (6.7%) | 15 |
DISCUSSION
Postoperative stroke continues to be a major complication after CABG. Although aortic manipulation remains the most important risk factor associated with postoperative stroke other risk factors include: female sex, advanced age, previous stroke, postoperative atrial fibrillation, carotid stenosis, hypertension, and diabetes.1,2,10–14 Studies have shown that 50–75% of all strokes after CABG are embolic2 and are discovered within 24 hours after surgery. Through the use of transcranial Doppler ultrasonography, it has been shown that emboli are produced during aortic cannulation and clamping.15–19 Thus, minimizing aortic manipulation by eliminating cannulation and clamping may decrease the incidence of postoperative stroke by decreasing the production of emboli.
In a study by Hannan et al20, 49,830 patients from the New York state registry underwent risk-adjusted analysis (Cox proportional hazard models and propensity analysis) comparing outcomes after OPCAB vs. ONCAB. In this study, OPCAB patients had significantly lower 30-day mortality, as well as a lower incidence of postoperative stroke. However, the mechanisms responsible for the observed reduction in postoperative stroke were not defined. OPCAB obviates the need for cardiopulmonary bypass; however, two recent meta-analyses did not show a reduction in postoperative stroke in low risk patients.21–22 This may be related to the use of a partial clamp on the ascending aorta during construction of proximal anastomoses. One study did report a lower incidence of postoperative stroke in patients undergoing OPCAB without aortic manipulation in comparison to patients undergoing OPCAB with partial clamping and patients undergoing ONCAB.23 Moreover, Hammon and colleagues reported a reduced incidence of postoperative neuropsychological deficits in patients undergoing single cross-clamp compared to double-clamp ONCAB or OPCAB patients with partial clamping.24
Avoiding partial clamping during construction of proximal anastomoses in OPCAB cases can be achieved by performing proximal anastomoses to in situ arterial grafts or by using proximal anastomotic connectors or facilitating devices such as the Heartstring proximal anastomosis system, both of which can be performed without a partial aortic clamp. In a randomized clinical trial evaluating the PAS-Port proximal anastomotic connector (Cardica, Inc, Redwood City, California) versus construction of hand-sewn proximal anastomoses with partial clamping, all of the reported strokes occurred in patients in which an aortic clamp was used.25 In previous work at our institution, we randomized 57 OPCAB patients with mild ascending aortic disease to receive either partial clamping (n=28) or the Heartstring clampless device (n=29) for proximal graft construction on the ascending aorta. Continuous TCD monitoring was used intraoperatively to monitor embolic signals in the middle cerebral arteries, signifying embolic events. The number of embolic signals was significantly lower in the Heartstring group than in the partial-clamping group (50.8±36.6 vs.90.0±64.0; p=0.007).26 Two delayed clinical strokes were observed in the clamping group and none observed in the Heartstring group, but the study was not powered to detect clinically significant events. These preliminary data suggest add to the growing body of evidence that minimizing aortic manipulation by avoiding an aortic clamp may be a valuable tool to reduce atheroembolic cerebral events.27–29
In this study, the primary goal was to determine the association of clamping strategies with the incidence on postoperative stroke. Although controversial, there is no clear consensus on the association between the use of cardiopulmonary bypass and the incidence of postoperative stroke. Both cardiopulmonary bypass use (pump strategy) and epiaortic grade were controlled for in the analysis since both are believed to play a role in the incidence of postoperative stroke. Because matching was done within treatment type, i.e. OPCAB cases matched to other OPCAB cases, this reduces the potential bias associated with treatment type. The main difference is that an on-pump strategy mandates at least some degree of aortic manipulation whereas a strategy of minimal manipulation is possible with an off-pump approach, either by having no manipulation or by using clampless facilitating devices.
Overall, aortic clamping strategy did not have a statistically significant effect on the incidence of postoperative stroke. This did not change when epiaortic grade was controlled for either as an ordinal or dichotomous variable or was omitted altogether from the analysis. However, within the subgroup of ONCAB cases, there was a significant association with postoperative stroke. The double clamp on-pump strategy had a 2.5-fold increase in the risk of postoperative stroke in comparison to the single cross-clamp technique, even after controlling for epiaortic grade. Although not statistically significant, there was a trend toward higher risk of stroke in the patients undergoing OPCAB with the use of partial clamping strategy compared to the no-clamp strategy.
The interpretation of these results can be explained by several limitations. Although the case control design made data collection possible by limiting review of operative notes to 706 patients, the sample size may have been inadequate to detect statistically significant differences between the various clamping strategies. In order to make this a cohort instead of a case-control study design, operative notes of over 10,000 patients (the sample from which this case control study was obtained) would have required review. Because the overall incidence of postoperative stroke in this cohort was relatively low (<2%) detecting differences in clamping strategies is difficult. In addition, because controls were matched to patients with a postoperative stroke based on PROPS score, the stroke risk may be limited to those patients with certain variables that may have put them at higher risk for stroke. Furthermore, controlling for epiaortic grade may have further limited since this variable was incomplete and precluded analysis in patients that did not have epiaortic ultrasound performed. Finally, as the descriptive analyses revealed, surgeon behavior changed over the time course of the study, which may have introduced bias into the study. This likely was influenced by data obtained from epiaortic scans, which undoubtedly influenced surgeon behavior. Despite controlling for stroke risk using PROPS, pump strategy, and epiaortic grade, it is apparent that surgeons used clamping less frequently toward the end of the study period compared to the beginning of the study. Furthermore, surgeons were unlikely to use clamping methods in patients with high-grade aortas, which may have minimized the effect of aortic clamping on the incidence of stroke since these aortas were rarely clamped. This change in approach likely reflects selection bias on the perceived risk of postoperative stroke associated with aortic clamping, especially in patients with advanced aortic disease determined by epiaortic ultrasound. Although the risk profile of patients did not change appreciably over the study period, the use of epiaortic ultrasound and clamping did. This reflects surgeons’ beliefs that clamping high-grade aortas are associated with higher atheroembolic stroke risk. The lack of increase in stroke according to epiaortic grade can be interpreted in two ways: 1) that epiaortic grade does not influence stroke or 2) that stroke incidence did not increase in higher grade aortas because of changes in strategy that occurred because of the epiaortic data available with this modality of testing. An additional limitation of this study is that timing, etiology, or type of postoperative stroke was not defined, because this outcome was attained from the STS database.
Approximately 80% of CABG cases in the US are performed on-pump and this study supports the use of single cross-clamp compared to the double clamp strategy to decrease postoperative stroke in patients undergoing primary, isolated, non-emergent CABG. From this study, it is still unclear as to whether patients undergoing clamping during OPCAB are at an increased risk of postoperative stroke compared to the clampless strategies. Further research investigating the impact of clamping strategies during CABG or other cardiac operations may allow for continued progress to reduce the incidence of postoperative stroke after cardiac surgery.
Figure 1.
Trends in Epiaortic Ultrasound Use At Emory University Hospitals for Isolated Coronary Artery Bypass Surgery
Figure 2.
Trends in Clamp Use by Year at Emory University Hospitals for Isolated Coronary Artery Bypass
Acknowledgments
Supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR000454. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Puskas JD, Winston AD, Wright CE, Gott JP, Brown WM, Craver JM, et al. Stroke after coronary artery operation: incidence, correlates, outcome, and cost. Ann Thorac Surg. 2000;69:1053–6. doi: 10.1016/s0003-4975(99)01569-6. [DOI] [PubMed] [Google Scholar]
- 2.Filsoufi F, Rahmanian PB, Castillo JG, Bronster D, Adams DH. Incidence, topography, predictors and long-term survival after stroke in patients undergoing coronary artery bypass grafting. Ann Thorac Surg. 2008;85:862–70. doi: 10.1016/j.athoracsur.2007.10.060. [DOI] [PubMed] [Google Scholar]
- 3.Schachner T, Zimmer A, Nagele G, Hangler H, Laufer G, Bonatti J. The influence of ascending aortic atherosclerosis on the long-term survival after CABG. Eur J Cardiothorac Surg. 2005;28:558–62. doi: 10.1016/j.ejcts.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Brown PP, Kugelmass AD, Cohen DJ, Reynolds MR, Culler SD, Dee AD, et al. The frequency and cost of complications associated with coronary artery bypass grafting surgery: results from the United States Medicare program. Ann Thorac Surg. 2008;85:1980–6. doi: 10.1016/j.athoracsur.2008.01.053. [DOI] [PubMed] [Google Scholar]
- 5.Shroyer AL, Coombs LP, Petersen ED. The Society of Thoracic Surgeons: 30-Day Operative Mortality and Morbidity Risk Models. Ann Thorac Surg. 2003;75:1856–6. doi: 10.1016/s0003-4975(03)00179-6. [DOI] [PubMed] [Google Scholar]
- 6.Rosenbaum PR. Optimal Matching for Observational Studies. JASA. 1989;84:1024–32. [Google Scholar]
- 7.Bolotin G, Domany Y, de Perini L, Frolkis I, Lev-Ran O, Nesher N, et al. Use of intraoperative epiaortic ultrasonography to delineate aortic atheroma. Chest. 2005;127:60–5. doi: 10.1378/chest.127.1.60. [DOI] [PubMed] [Google Scholar]
- 8.Sylivris S, Calafiore P, Matalanis G, Rosalion A, Yuen HP, Buxton BF, et al. The intraoperative assessment of ascending aortic atheroma: epiaortic imaging is superior to both transesophageal echocardiography and direct palpation. J Cardiothorac Vasc Anesth. 1997;11:704–7. doi: 10.1016/s1053-0770(97)90161-0. [DOI] [PubMed] [Google Scholar]
- 9.Suvarna S, Smith A, Stygall J, Kolvecar S, Walesby R, Harrison M, et al. An intraoperative assessment of the ascending aorta: a comparison of digital palpation, transesophageal echocardiography, and epiaortic ultrasonography. J Cardiothorac Vasc Anesth. 2007;21:805–9. doi: 10.1053/j.jvca.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Halkos ME, Puskas JD, Lattouf OM, Kilgo P, Guyton RA, Thourani VH. Impact of preoperative neurologic events on outcomes after coronary artery bypass grafting. Ann Thorac Surg. 2008;86:504–10. doi: 10.1016/j.athoracsur.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med. 1996;335:1857–63. doi: 10.1056/NEJM199612193352501. [DOI] [PubMed] [Google Scholar]
- 12.McKhann GM, Goldsborough MA, Borowicz LM, Jr, Mellits ED, Brookmeyer R, Quaskey SA, et al. Predictors of stroke risk in coronary artery bypass patients. Ann Thorac Surg. 1997;63:516–21. doi: 10.1016/s0003-4975(97)83384-x. [DOI] [PubMed] [Google Scholar]
- 13.Redmond JM, Greene PS, Goldsborough MA, Cameron DE, Stuart RS, Sussman MS, et al. Neurologic injury in cardiac surgical patients with a history of stroke. Ann Thorac Surg. 1996;61:42–7. doi: 10.1016/0003-4975(95)00903-5. [DOI] [PubMed] [Google Scholar]
- 14.Anyanwu AC, Filsoufi F, Salzberg SP, Bronster DJ, Adams DH. Epidemiology of stroke after cardiac surgery in the current era. J Thorac Cardiovasc Surg. 2007;134:1121–27. doi: 10.1016/j.jtcvs.2007.06.031. [DOI] [PubMed] [Google Scholar]
- 15.van der Linden J, Casimir-Ahn H. When do cerebral emboli appear during open heart operations? A transcranial doppler study. Ann Thorac Surg. 1991;51:237–41. doi: 10.1016/0003-4975(91)90793-p. [DOI] [PubMed] [Google Scholar]
- 16.Blauth CI. Macroemboli and microemboli during cardiopulmonary bypass. Ann Thorac Surg. 1995;59:1300–3. doi: 10.1016/0003-4975(95)00105-t. [DOI] [PubMed] [Google Scholar]
- 17.Barbut D, Yao FS, Lo YW, Silverman R, Hager DN, Trifiletti RR, et al. Determination of size of aortic emboli and embolic load during coronary artery bypass grafting. Ann Thorac Surg. 1997;63:1262–7. [PubMed] [Google Scholar]
- 18.Liu YH, Wang DX, Li LH, Wu XM, Shan GJ, Su Y, et al. The effects of cardiopulmonary bypass on the number of cerebral microemboli and the incidence of cognitive dysfunction after coronary artery bypass graft surgery. Anesth Analg. 2009;109:1013–22. doi: 10.1213/ane.0b013e3181aed2bb. [DOI] [PubMed] [Google Scholar]
- 19.Motallebzadeh R, Bland JM, Markus HS, Kaski JC, Jahangiri M. Neurocognitive function and cerebral emboli: randomized study of on-pump versus off-pump coronary artery bypass surgery. Ann Thorac Surg. 2007;83:475–82. doi: 10.1016/j.athoracsur.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 20.Hannan EL, Wu C, Smith CR, Higgins RS, Carlson RE, Culliford AT, et al. Off-pump versus on-pump coronary artery bypass graft surgery: differences in short-term outcomes and in long-term mortality and need for subsequent revascularization. Circulation. 2007;116:1145–52. doi: 10.1161/CIRCULATIONAHA.106.675595. [DOI] [PubMed] [Google Scholar]
- 21.Cheng DC, Bainbridge D, Martin JE, Novick RJ Evidence-Based Perioperative Clinical Outcomes Research Group. Does off-pump coronary artery bypass reduce mortality, morbidity, and resource utilization when compared with conventional coronary artery bypass? A meta-analysis of randomized trials. Anesthesiology. 2005;102:188–203. doi: 10.1097/00000542-200501000-00028. [DOI] [PubMed] [Google Scholar]
- 22.Wijeysundera DN, Beattie WS, Djaiani G, Rao V, Borger MA, Karkouti K, et al. Off-pump coronary artery surgery for reducing mortality and morbidity: meta-analysis of randomized and observational studies. J Am Coll Cardiol. 2005;46:872–82. doi: 10.1016/j.jacc.2005.05.064. [DOI] [PubMed] [Google Scholar]
- 23.Kim KB, Kang CH, Chang WI, Lim C, Kim JH, Ham BM, et al. Off-pump coronary artery bypass with complete avoidance of aortic manipulation. Ann Thorac Surg. 2002;74:S1377–82. doi: 10.1016/s0003-4975(02)04060-2. [DOI] [PubMed] [Google Scholar]
- 24.Hammon JW, Stump DA, Butterworth JF, Moody DM, Rorie K, Deal DD, et al. Coronary artery bypass grafting with single cross-clamp results in fewer persistent neuropsychological deficits than multiple clamp or off-pump coronary artery bypass grafting. Ann Thorac Surg. 2007;84:1174–8. doi: 10.1016/j.athoracsur.2007.04.100. [DOI] [PubMed] [Google Scholar]
- 25.Puskas JD, Halkos ME, Balkhy H, Caskey M, Connolly M, Crouch J, et al. Evaluation of the PAS-Port Proximal Anastomosis System in coronary artery bypass surgery (the EPIC trial) J Thorac Cardiovasc Surg. 2009;138:125–32. doi: 10.1016/j.jtcvs.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 26.El Zayat H, Puskas J, Hwang S, Thourani VH, Lattouf OM, Kilgo P, et al. Avoiding the Clamp for Aortocoronary Proximal Anastomoses is Associated with Fewer Intraoperative Cerebral Embolic Events: Results of a Prospective Randomized Trial. Interact Cardiovasc Thorac Surg. 2012;14:12–6. doi: 10.1093/icvts/ivr004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolf LG, Abu-Omar Y, Choudhary BP, Pigott D, Taggart DP. Gaseous and solid cerebral microembolization during proximal aortic anastomoses in off-pump coronary surgery: The effect of an aortic side-biting clamp and two clampless devices. J Thorac Cardiovasc Surg. 2007;133:485–93. doi: 10.1016/j.jtcvs.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 28.Misfeld M, Brereton RJL, Sweetman EA, Doig GS. Neurologic complications after off-pump coronary artery bypass grafting with and without aortic manipulation: Meta-analysis of 11,398 cases from 8 studies. J Thorac Cardiovasc Surg. 2011;142:e11–17. doi: 10.1016/j.jtcvs.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 29.Emmert MY, Seifert B, Wilhelm M, Grünenfelder J, Falk V, Salzberg SP. Aortic no-touch technique makes the difference in off-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2011;142:1499–1506. doi: 10.1016/j.jtcvs.2011.04.031. [DOI] [PubMed] [Google Scholar]