Abstract
Introduction
Although simulation-based training is increasingly used for medical education, its benefits in continuing medical education (CME) are less established. This study seeks to evaluate the feasibility of incorporating simulation-based training into a CME conference and compare its effectiveness with the traditional workshop in improving knowledge and self-reported confidence.
Methods
Participants (N=27) were group randomized to either a simulation-based workshop or a traditional case-based workshop.
Results
Post-training, knowledge assessment score neither did increase significantly in the traditional group (d=0.13; p=0.76) nor did significantly decrease in the simulation group (d= − 0.44; p=0.19). Self-reported comfort in patient assessment parameters increased in both groups (p<0.05 in all). However, only the simulation group reported an increase in comfort in patient management (d=1.1, p=0.051 for the traditional group and d=1.3; p= 0.0003 for the simulation group). At 1 month, comfort measures in the traditional group increased consistently over time while these measures in the simulation group increased post-workshop but decreased by 1 month, suggesting that some of the effects of training with simulation may be short lived.
Discussion
The use of simulation-based training was not associated with benefits in knowledge acquisition, knowledge retention, or comfort in patient assessment. It was associated with superior outcomes in comfort in patient management, but this benefit may be short-lived. Further studies are required to better define the conditions under which simulation-based training is beneficial.
Keywords: patient simulation, continuing medical education, pregnancy-induced hypertension
Introduction
In order for professional self-regulation to continue, physicians’ participation in lifelong learning is the foundation that underlies society's trust in the profession (1). Continuing medical education (CME) in the form of participation in certified educational activities is a widely recognized method to ensure that physicians maintain their medical knowledge and skills (2). However, multiple studies have questioned the effectiveness of CME activities in modifying physician behaviors and performance, and those in the format of didactic lectures, in particular, were found to be largely ineffective (3–5). Nonetheless, CME activities are not entirely without merit (6–8). What has consistently emerged in the literature is the notion that interactive or mixed CME activities can be effective in modifying physician practices (9, 10).
Simulation is an interactive educational tool that is increasingly used in medical education (11) and there is mounting evidence to support its role in improving knowledge, behaviors, and product skill outcomes (12–14). Yet despite this evidence, simulation is seldom discussed within the CME setting (15). The adoption of new technology into the CME arena may be limited, in part, by cultural barriers and forces of inertia (15). Given a choice, physicians tend to prefer traditional passive modalities of education, such as the didactic lecture (16–18). In addition, the usual limitations of and barriers to implementation of simulation-based education apply equally to the non-CME setting as to the CME setting, in that this form of learning can be expensive and cumbersome to deliver. In view of the potential reluctance to adopt new technology into CME activities, this pilot study seeks to evaluate the feasibility of incorporating simulation-based training into an existing CME conference and discuss the role of simulation-based CME education with respect to the currently available evidence, feasibility, and future research directions.
Methods
Participants
All consenting attendees of the 2011 Rocky Mountain/American College of Physicians Internal Medicine Meeting enrolled in the ‘Assessment of Shortness of Breath in Pregnancy’ workshop were included in the study. Participants included academic- and community-based general internists. A minority of participants, approximately 30%, were residents.
Participants were group randomized to either a simulation-based workshop or a traditional case-based interactive workshop. Both groups were exposed to the same obstetric-internal medicine case (shortness of breath in pregnancy, secondary to pulmonary edema from severe pre-eclampsia) by the same workshop leaders. The duration of the workshop for both groups was 1 h. This study was approved by the University of Calgary Conjoint Health Research Ethics Board.
Simulation-based workshop
Participants in the simulation group were provided with a 5-min orientation and an introduction to the features of the computer-based pregnant mannequin (Noelle® S575, Gaumard®, Miami, FL, USA). The patient's clinical status was controlled remotely using a wireless tablet, with patient's vital signs displayed on a touchscreen monitor at the bedside. Participants were encouraged to work as a group. One nurse confederate assisted in running the scenario. The duration of the interactive case was 30 min, followed by a 15-min debriefing session and a 10-min didactic session covering the key teaching points of the workshop.
Traditional case-based workshop
Participants in the traditional group participated in a case-based interactive workshop. The same obstetric-internal medicine case as the simulation-based workshop was discussed in a 55-min session by the same workshop leaders, covering the same key teaching points as the simulation-based workshop.
Outcome assessment
Participants from both groups completed a baseline survey and knowledge assessment pre- and immediately post-workshop. Knowledge retention was assessed at 1-month with an internet-based knowledge assessment tool.
Knowledge assessment pre- and post-workshop was done using two parallel forms, each containing 10 multiple-choice questions (MCQ). Retention knowledge assessment used the same form as the post-workshop MCQs. MCQs were constructed by an expert panel based on a table of specifications, covering items on pathophysiology, epidemiology, diagnosis, and management, and assessed for knowledge comprehension and knowledge application. The expert panel consisted of one specialist in obstetric-internal medicine and two specialists in general internal medicine. The MCQs were piloted on and revised based on input on appropriateness of content, wording clarity, and difficulty level from internal medicine residents (N=3) and faculty with maternal–fetal medicine expertise (N=1).
Statistical analysis
Comparisons between groups were performed using standard parametric and non-parametric tests: Student's t-tests, paired t-tests, Wilcoxon's rank sum tests, Fisher's exact tests, and Chi-square tests. Measures of effect size are reported using Cohen's d (19).
Repeated-measures mixed-factor analyses of variance (ANOVA) were conducted to assess whether there were group and score differences, after examination of normality and sphericity using Mauchly's test of sphericity.
All reported p-values are two-sided. For all post-hoc multiple comparisons between groups, the nominal α level was adjusted by Bonferroni correction. All analyses were performed using SAS version 9.3 (SAS Institute Inc, Cary, NC, USA) and PASW Statistics Software, version 18.0 for Windows (PASW, IBM Corporation, Somers, NY, USA).
Results
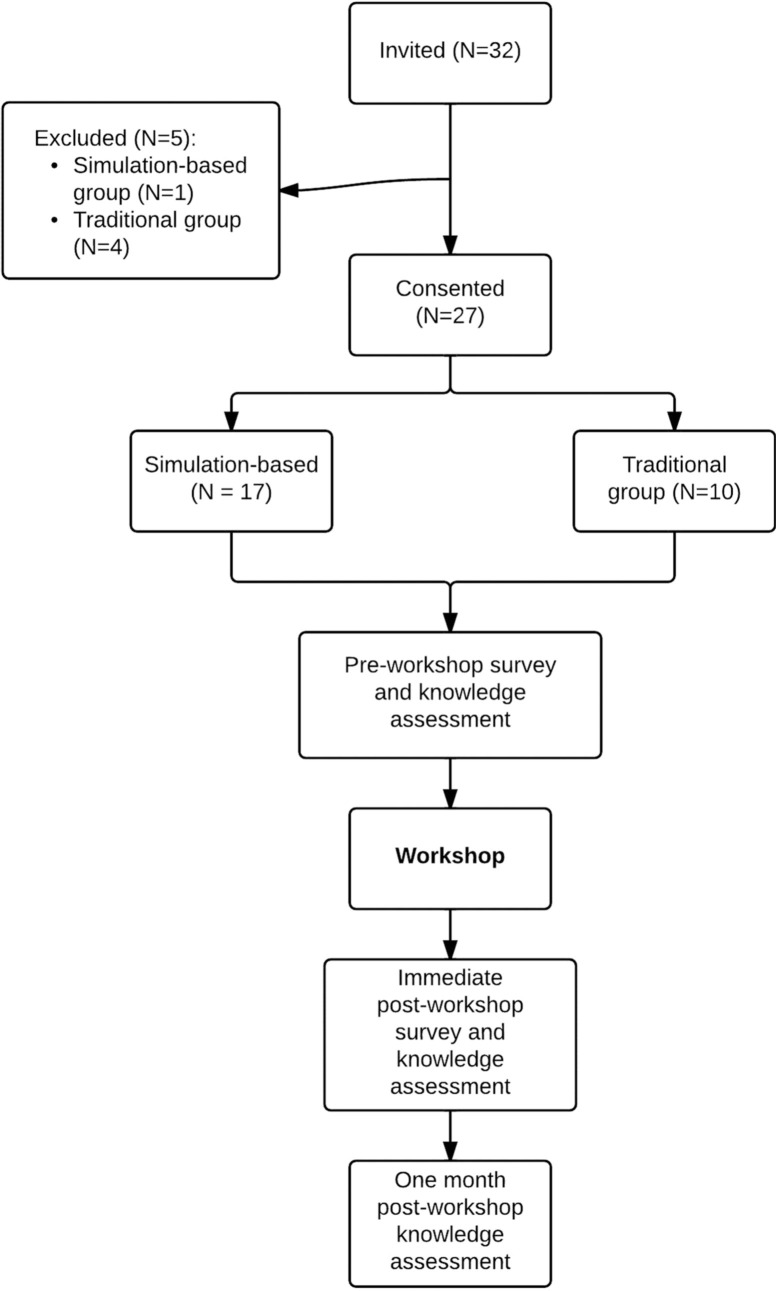
Of the 32 participants invited, 27 consented to the study. In total, three 1-h workshops were conducted. Of the 27 participants, a group of 10 was randomized to the traditional group, while a group of 9 and a group of 8 were randomized to the simulation group (Fig. 1).
Fig. 1.
Overview of study design.
As demonstrated in Table 1, there were no significant baseline differences between the two groups with the exception of one variable. Participants in the simulation group at baseline felt that simulation was more valuable for medical teaching (mean 4.7±0.5) compared to the traditional group (mean 4.2±0.4; p<0.01).
Table 1.
Baseline characteristics of workshop participants
| Traditional (N=10) | Simulation (N=17) | p | |
|---|---|---|---|
| Males – number (%) | 3 (30) | 7 (41) | 0.69 |
| Duration of practice | |||
| 1–5 years – number (%) | 2 (20) | 0 | 0.33 |
| 6–10 years – number (%) | 0 | 0 | |
| 11–15 years – number (%) | 1 (10) | 1 (6) | |
| 16–20 years – number (%) | 0 | 0 | |
| 21 years or more – number (%) | 1 (10) | 2 (12) | |
| Not yet in practice – number (%) | 6 (60) | 14 (82) | 0.36 |
| University-based – number (%) | 5 (50) | 15 (75) | 0.14 |
| Received additional training in Obstetric Internal Medicine – number (%) | 1 (10) | 4 (24) | 0.62 |
| Previously learned skills using high-fidelity simulation – number (%) | 6 (60) | 11 (65) | 1.00 |
| I am comfortable participating in the care of medically complicated pregnant patients* | 2.2±0.8 | 2.5±0.9 | 0.45 |
| I am comfortable evaluating a pregnant patient with shortness of breath* | 2.9±1.0 | 2.8±0.8 | 0.71 |
| I am comfortable managing shortness of breath in the pregnant patient* | 2.7±0.9 | 2.8±0.8 | 0.85 |
| I am comfortable being taught with high-fidelity simulation* | 4.2±0.4 | 3.9±0.7 | 0.28 |
| I think simulation in general is valuable for the purposes of medical teaching* | 4.2±0.4 | 4.7±0.5 | 0.01 |
1 = strongly disagree; 5 = strongly agree.
Knowledge assessment scores
Baseline MCQ scores were not different between the two groups (p=0.22; Table 2). Post-workshop MCQ scores were also not significantly different between the two groups (p=0.90; Table 2). The change in scores pre-and post-workshop was not significant for either group (p>0.05).
Table 2.
Differences in measures for traditional group pre- and post-workshop and simulation group pre- and post-workshop
| Traditional Group Pre-Workshop (N=10) (mean±SD) | Traditional Group Post-Workshop (N = 10) (mean±SD) | Cohen's d; p-value | Simulation-based Pre-Workshop (N=17) | Simulation-based Post-Workshop (N=17) (mean±SD) | Cohen's d; p-value | |
|---|---|---|---|---|---|---|
| Baseline knowledge assessment scores | 50.0%±16.3% | 52.0%±15.5% | d=0.13; p=0.76 | 58.8%±18.3% | 51.2%±16.2% | d= −0.44; p=0.19 |
| Self-reported comfort in participating in the care of medically complicated pregnant patients | 2.2±0.8 | 3.3±0.95 | d=1.26; p=0.003 | 2.5±0.9 | 3.3±0.85 | d=0.91; p=0.004 |
| Self-reported comfort in evaluating a pregnant patient with shortness of breath | 2.9±1.0 | 3.8±0.63 | d=1.1; p=0.02 | 2.8±0.8 | 3.9±0.33 | d=1.8; p<0.001 |
| Self-reported comfort in managing shortness of breath in a pregnant patient | 2.7±0.9 | 3.3±0.95 | d=0.63; p=0.051 | 2.8±0.8 | 3.6±0.61 | d=1.3; p<0.001 |
Self-reported comfort
Self-reported comfort in participating in the care of medically complicated pregnant patients increased for both groups (d=1.26; p=0.003 for the traditional group and d=0.91; p=0.004 for the simulation group; Table 2). Self-reported comfort in evaluating a pregnant patient with shortness of breath also significantly increased in both groups (d=1.1; p= 0.02 for the traditional group and d=1.8; p<0.001 for the simulation group; Table 2). However, only the simulation group reported a significant increase in self-reported comfort in managing shortness of breath in a pregnant patient (d=0.63; p=0.051 for the traditional group and d=1.3; p=0.0003 for the simulation group, Table 2).
Retention knowledge assessment scores and self-reported comfort
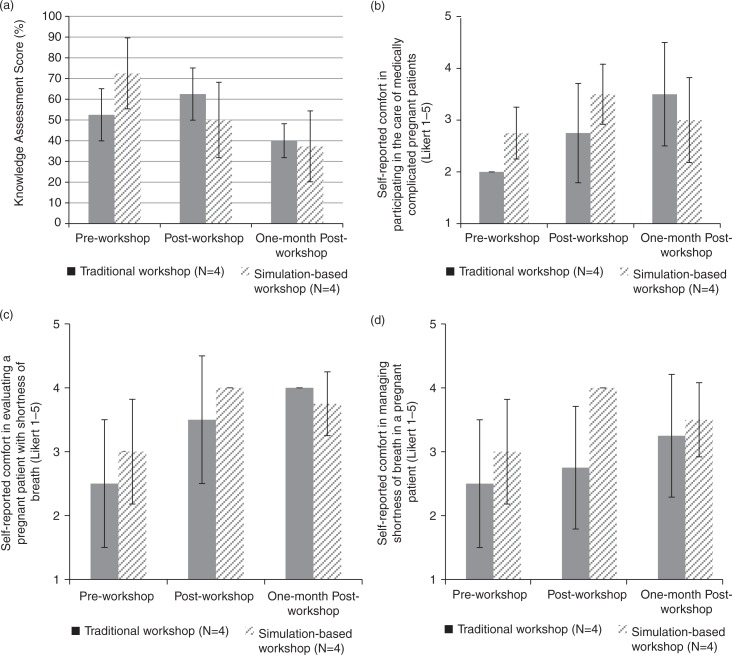
Data were only available for eight participants (29.6%): four participants from the traditional group and four from the simulation group.
MCQ scores increased post-workshop for the traditional group but declined at 1-month (52.5±12.6%, 62.5±12.6%, and 40.0±8.2%, respectively, Fig. 2a). MCQ score pre-workshop, post-workshop, and at 1-month decreased steadily for the simulation group (72.5±17.1%, 50.0±18.2, and 37.5±17.1%, respectively).
Fig. 2.
One-month retention scores of participants (N=8) in the traditional case-based interactive workshop and simulation-based workshop. (a) Knowledge assessment scores; (b) self-reported comfort in participating in the care of the medically complicated pregnant patient; (c) self-reported comfort in evaluating a pregnant patient with shortness of breath; and (d) self-reported comfort in managing shortness of breath in a pregnant patient.
Self-reported comfort measures in participating in the care of medically complicated pregnant patients, evaluating a pregnant patient with shortness of breath, and managing shortness of breath in a pregnant patient all rose steadily between pre-workshop, post-workshop, and at 1-month for the traditional group (Fig. 2b–d, respectively). While these measures increased post-workshop, they decreased at 1-month for the simulation group (Fig. 2b–d, respectively).
For all retention scores, results from mixed ANOVA indicated a significant main effect of scores but no effect of group. No significant interaction between scores and group was found. Post-hoc analyses indicated that there were no differences in the scores between or within group (p>0.05 in all instances).
Satisfaction
Although satisfaction with the workshop was higher for all items for the simulation group (Table 3), none of these differences were significant.
Table 3.
Workshop satisfaction for both traditional and simulation groups
| Traditional (N=10) | Simulation (N=17) | p | |
|---|---|---|---|
| Met stated objectives* | 4.0±1.2 | 4.2±0.8 | 0.54 |
| Enhanced my knowledge* | 4.0±1.2 | 4.4±0.9 | 0.37 |
| Satisfied my expectations* | 4.0±1.2 | 4.4±0.9 | 0.39 |
| Conveyed information that applied to my practice* | 4.0±1.2 | 4.1±0.8 | 0.88 |
| Allocated at least 25% of the time for interaction* | 3.5±1.6 | 4.2±0.7 | 0.19 |
| Was free from commercial bias* | 4.0±1.2 | 4.6±0.5 | 0.12 |
| Will help me practice more safely* | 4.0±1.2 | 4.2±0.9 | 0.56 |
| Will change my clinical practice* | 3.8±1.1 | 3.9±1.0 | 0.73 |
| Exposed me to new clinical situations* | 3.7±1.3 | 4.2±1.0 | 0.27 |
1 = strongly disagree; 5 = strongly agree.
Discussion
In this pilot randomized controlled study comparing the use of a traditional case-based workshop with a simulation-based workshop in a CME setting, our results suggest that although implementing a simulation-based workshop was feasible and well-received, we did not identify significant differences in knowledge acquisition, retention, self-reported comfort in medical care assessment parameters or satisfaction. The benefits of this simulation-based workshop appeared restricted only to improving comfort in management only, demonstrating a large effect size pre-and post-training (d =1.1). However, even this benefit of our simulation-based workshop appeared short-lived.
Our study is limited by a small sample size and it involved only one CME conference. These issues preclude definitive conclusions and generalizability about the effects of simulation-based workshops on learning outcomes in the CME setting. The pattern of results that emerged from our study should therefore only be considered as hypothesis generating. Nonetheless, these patterns of results deserve some discussion. In particular, three points regarding the use of simulation-based training in CME merit further discussion. First, what is the currently available evidence supporting the use of simulation-based CME training and how do these results fit in within the context of available evidence? Second, what is the feasibility of using simulation in a CME setting? Third, what future studies are needed to enable educators to optimally implement simulation training in the CME setting?
Evidence
Simulation-based health education strategies range from part-task trainers and virtual reality systems to integrated scenarios with high-fidelity manikins (20). In a recent systematic review, compared to other instructional methods, simulation-based education was found to be effective (21). However, only 6% of the studies found in the review involved physicians in practice. The majority of the studies were conducted in a non-CME setting.
Because instructional strategies that are beneficial for novice learners may not always be beneficial for expert learners (expertise reversal effect) (22–24), it is important that the effectiveness for the use of simulation in the CME setting be established empirically rather than inferred from non-CME studies.
Theoretically, simulation-based education should be well suited for CME training. Experiential learning techniques, after all, are recommended based on the adult learning theory (25). Furthermore, interactivity has consistently been shown to be effective for learning in CME (26), while passive learning approaches are generally shown to be ineffective in changing behaviors (27). As simulation-based teaching techniques are generally interactive in nature, superior learning outcomes should be expected. However, emotions and cognitive load associated from participation in novel simulation-based exercises may negatively impact on learning outcomes (28).
Despite the theoretical advantages of the use of simulation, few studies have directly evaluated the use of simulation in CME (15, 29, 30), outside technical skill training (31–35). Our study indicates that simulation-based education can be feasible, and may result in similar learning outcomes. However, of particular concern is our study's finding that simulation-based training may be potentially associated with a decrement in knowledge. Although this decrement is not significant, our study sample size is small. Therefore, larger studies are needed to preclude a detrimental effect of simulation-based training on knowledge outcomes. Despite the notion that knowledge is considered the lowest level of competence in Miller's model of clinical competence (36), it is also noteworthy that knowledge is the basic foundation of competence and expertise (37). Therefore, any significant decrement in knowledge should merit concern. Additional evidence is needed to clarify the effect of simulation-based education on knowledge acquisition and knowledge application.
Feasibility
Multiple studies have identified that practicing physicians tend to prefer passive modalities of education (16–18, 38). Amongst interactive modalities of education, simulation in particular poses additional barriers for implementation in the CME setting, such as the concern that participants may feel intimated and embarrassed (39, 40), issues regarding simulator fidelity (29, 39), and costs (37).
In a survey of physicians, only 23% felt that simulation or virtual patients as being helpful for CME (16). Anesthesiologists, however, are more receptive to the use of simulation, with up to 82% expressing an interest in simulation-based CME (40), and simulation courses in crisis resource management for anesthesia faculty have been well-received (41). Feasibility in one medical specialty, however, may not translate into feasibility in another, since medical and surgical specialists may prefer to learn in very different ways (26, 42, 43). Each specialty may have unique barriers to implementing simulation-based CME. Therefore, additional studies on feasibility in other disciplines are needed.
Future research
Our study has identified several areas for future investigations. First, the effect of simulation-based CME activities on knowledge acquisition and application needs to be clarified. Simulation may not be the most efficient or effective modality for knowledge acquisition, since multiple non-simulation-based CME activities have been shown to effect knowledge gain (44). Second, future research should focus on the effect of simulation-based CME activities on clinically important outcomes. For example, research will benefit from the use of Moore's Outcome-based CME valuation Model, which proposes measuring outcomes on six levels: participation, satisfaction, learning, performance, patient health, and population health (45). While effects on patient health and population are the ultimate purposes of CME, research efforts should at a minimum target learning and performance outcomes (37). Third, feasibility of implementation of simulation-based CME education should be further evaluated across different disciplines.
Conclusion
Our study demonstrated that the use of simulation-based CME education was feasible and well-received, but it failed to identify a benefit in knowledge acquisition and retention. Future studies should clarify the effect of simulation on knowledge acquisition and application as well as feasibility across different disciplines.
Acknowledgements
There are no financial disclosures related to the design and conduct of the data, or preparation, review or approval of this article. This study was presented in an abstract form at the 2013 Canadian Conference on Medical Education, Quebec City, QC, Canada.
Conflict of interest and funding
The authors do not have any conflicts of interest to declare. This study was unfunded.
References
- 1.Irvine D. The performance of doctors. I: professionalism and self regulation in a changing world. BMJ. 1997;314:1540. doi: 10.1136/bmj.314.7093.1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis NL, Willis CE. A new metric for continuing medical education credit. J Contin Educ Health Prof. 2004;24:139–44. doi: 10.1002/chp.1340240304. [DOI] [PubMed] [Google Scholar]
- 3.Cantillon P, Jones R. Does continuing medical education in general practice make a difference? BMJ. 1999;318:1276–9. doi: 10.1136/bmj.318.7193.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis DA, Thomson MA, Oxman AD, Haynes R. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 5.Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. Can Med Assoc J. 1995;153:1423–31. [PMC free article] [PubMed] [Google Scholar]
- 6.Marinopoulos SS, Dorman T, Ratanawongsa N, Wilson LM, Ashar BH, Magaziner JL, et al. Effectiveness of continuing medical education. Evid Rep Technol Assess. 2007;149:1–69. [PMC free article] [PubMed] [Google Scholar]
- 7.Haynes R, Davis DA, McKibbon A, Tugwell P. A critical appraisal of the efficacy of continuing medical education. JAMA. 1984;251:61–4. [PubMed] [Google Scholar]
- 8.Davis DA, Thomson M, Oxman AD, Haynes R. Evidence for the effectiveness of cme: a review of 50 randomized controlled trials. JAMA. 1992;268:1111–7. [PubMed] [Google Scholar]
- 9.Davis D, O'Brien MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282:867–74. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]
- 10.Forsetlund L, Bjørndal A, Rashidian A, Jamtvedt G, O'Brien MA, Wolf F, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009:CD003030. doi: 10.1002/14651858.CD003030.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiniara G, Cole G, Brisbin K, Huffman D, Cragg B, Lamacchia M, et al. Simulation in healthcare: a taxonomy and a conceptual framework for instructional design and media selection. Med Teach. 2012:e1–e16. doi: 10.3109/0142159X.2012.733451. [DOI] [PubMed] [Google Scholar]
- 12.Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306:978–88. doi: 10.1001/jama.2011.1234. [DOI] [PubMed] [Google Scholar]
- 13.Ma IW, Brindle M, Ronksley P, Lorenzetti D, Sauve R, Ghali W. Use of simulation-based education to improve outcomes of central venous catheterization: a systematic review and meta-analysis. Acad Med. 2011;86:1137–47. doi: 10.1097/ACM.0b013e318226a204. [DOI] [PubMed] [Google Scholar]
- 14.McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86:706–11. doi: 10.1097/ACM.0b013e318217e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGaghie WC, Siddall VJ, Mazmanian PE, Myers J. Lessons for continuing medical education from simulation research in undergraduate and graduate medical education. Effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest. 2009;135:62S–68S. doi: 10.1378/chest.08-2521. [DOI] [PubMed] [Google Scholar]
- 16.Bower EA, Girard DE, Wessel K, Becker TM, Choi D. Barriers to innovation in continuing medical education. J Contin Educ Health Prof. 2008;28:148–56. doi: 10.1002/chp.176. [DOI] [PubMed] [Google Scholar]
- 17.Reddy H, Harris I, Galle B, Seaquist ER. Continuing medical education. What do Minnesota physicians want? Minn Med. 2001;84:58–61. [PubMed] [Google Scholar]
- 18.Stancic N, Mullen PD, Prokhorov AV, Frankowski RF, McAlister AL. Continuing medical education: what delivery format do physicians prefer? J Contin Educ Health Prof. 2003;23:162–7. doi: 10.1002/chp.1340230307. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Academic Press; 1988. [Google Scholar]
- 20.Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40:254–62. doi: 10.1111/j.1365-2929.2006.02394.x. [DOI] [PubMed] [Google Scholar]
- 21.Cook DA, Brydges R, Hamstra SJ, Zendejas B, Szostek JH, Wang AT, et al. Comparative effectiveness of technology-enhanced simulation versus other instructional methods: a systematic review and meta-analysis. Simul Healthcare. 2012;7:308–20. doi: 10.1097/SIH.0b013e3182614f95. [DOI] [PubMed] [Google Scholar]
- 22.Kalyuga S, Ayres P, Chandler P, Sweller J. The expertise reversal effect. Educ Psychol. 2003;38:23–31. [Google Scholar]
- 23.Van Merriënboer JJG, Sweller J. Cognitive load theory in health professional education: design principles and strategies. Med Educ. 2010;44:85–93. doi: 10.1111/j.1365-2923.2009.03498.x. [DOI] [PubMed] [Google Scholar]
- 24.Kalyuga S, Renkl A. Expertise reversal effect and its instructional implications: introduction to the special issue. Instr Sci. 2010;38:209–15. [Google Scholar]
- 25.Knowles MS, Swanson RA, Holton EF. 7th ed. Oxford: Butterworth-Heinemann; 2011. The adult learner. The definitive classic in adult education and human resource development. [Google Scholar]
- 26.Abrahamson S, Baron J, Elstein AS, Hammond WP, Holzman GB, Marlow B, et al. Continuing medical education for life: eight principles. Acad Med. 1999;74:1288–94. doi: 10.1097/00001888-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Grimshaw JM, Shirran L, Thomas R, Mowatt G, Fraser C, Bero L, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39:II2–45. [PubMed] [Google Scholar]
- 28.Fraser K, Ma I, Teteris E, Baxter H, Wright B, McLaughlin K. Emotion, cognitive load and learning outcomes during simulation training. Med Educ. 2012;46:1055–62. doi: 10.1111/j.1365-2923.2012.04355.x. [DOI] [PubMed] [Google Scholar]
- 29.Rogers DA. The role of simulation in surgical continuing medical education. Semin Colon Rectal Surg. 2008;19:108–14. [Google Scholar]
- 30.Weller J, Wilson L, Robinson B. Survey of change in practice following simulation-based training in crisis management. Anaesthesia. 2003;58:471–3. doi: 10.1046/j.1365-2044.2003.03078_1.x. [DOI] [PubMed] [Google Scholar]
- 31.Rosser JCJ, Rosser LE, Savalgi RS. Objective evaluation of a laparoscopic surgical skill program for residents and senior surgeons. Arch Surg. 1998;133:657–61. doi: 10.1001/archsurg.133.6.657. [DOI] [PubMed] [Google Scholar]
- 32.Stefanidis D, Sierra R, Korndorffer JR, Jr, Dunne JB, Markley S, Touchard CL, et al. Intensive continuing medical education course training on simulators results in proficiency for laparoscopic suturing. Am J Surg. 2006;191:23–7. doi: 10.1016/j.amjsurg.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 33.Dayal R, Faries PL, Lin SC, Bernheim J, Hollenbeck S, DeRubertis B, et al. Computer simulation as a component of catheter-based training. J Vasc Surg. 2004;40:1112–7. doi: 10.1016/j.jvs.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 34.Patel AD, Gallagher AG, Nicholson WJ, Cates CU. Learning curves and reliability measures for virtual reality simulation in the performance assessment of carotid angiography. J Am Coll Cardiol. 2006;47:1796–802. doi: 10.1016/j.jacc.2005.12.053. [DOI] [PubMed] [Google Scholar]
- 35.Macnab AJ, Macnab M. Teaching pediatric procedures: the Vancouver model for instructing Seldinger's technique of central venous access via the femoral vein. Pediatrics. 1999;103:E8. doi: 10.1542/peds.103.1.e8. [DOI] [PubMed] [Google Scholar]
- 36.Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65:S63–7. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 37.Norman G. The American College of Chest Physicians evidence-based educational guidelines for continuing medical education interventions: a critical review of evidence-based educational guidelines. Chest. 2009;135:834–7. doi: 10.1378/chest.09-0036. [DOI] [PubMed] [Google Scholar]
- 38.Young JM, Hollands MJ, Solomon MJ. Surgeons’ participation in continuing medical education: is it evidence-based? Med Educ. 2006;40:423–9. doi: 10.1111/j.1365-2929.2006.02443.x. [DOI] [PubMed] [Google Scholar]
- 39.Sinz EH. Anesthesiology national CME program and ASA activities in simulation. Anesthesiol Clin. 2007;25:209–23. doi: 10.1016/j.anclin.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 40.ASA Workgroup on Simulation Education White Paper. ASA Approval of Anesthesiology Simulation Programs. 2006. Available from: http://www.asahq.org/For-Members/Education-and-Events/Simulation-Education/White-Paper-on-ASA-Approval-of-Anesthesiology-Simulation-Programs.aspx [cited 3 May 2013]
- 41.Blum RH, Raemer DB, Carroll JS, Sunder N, Felstein DM, Cooper JB. Crisis resource management training for an anaesthesia faculty: a new approach to continuing education. Med Educ. 2004;38:45–55. doi: 10.1046/j.1365-2923.2004.01696.x. [DOI] [PubMed] [Google Scholar]
- 42.Curry L, Adams C. Patterns of learning style across selected medical specialties. Educ Psychol. 1991;11:247–77. [Google Scholar]
- 43.Airey N, Marriott J, Rodd J. Learning styles of psychiatrists and other specialists. Psychiatr Bull. 2001;25:306–9. [Google Scholar]
- 44.Bordage G, Carlin B, Mazmanian PE. Continuing medical education effect on physician knowledge effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest. 2009;135:29S–36S. doi: 10.1378/chest.08-2515. [DOI] [PubMed] [Google Scholar]
- 45.Moore D. A framework for outcomes evaluation in the continuing professional development of physicians. In: Davis D, Barnes B, Fox R, editors. The continuing professional development of physicians; Chicago, IL: American Medical Association Press; 2007. pp. 249–74. [Google Scholar]