Abstract
The “Attenuated Psychosis Syndrome” (APS, sometimes referred to as the “schizophrenia prodrome”) is characterized by subthreshold psychotic-like symptoms and functional decline, and is often associated with significant disability. These symptoms may cause impairment and are of further interest due to their predictive relation to schizophrenia and other psychotic disorders. These symptoms currently are not represented in the diagnostic system for mental health, and it is unclear how they are conceptualized by relevant professionals. The current study surveyed a national sample (n=303) of clinical psychologists, psychiatrists, and general practitioners regarding their clinical appraisal of APS. Practitioners were asked to respond to vignettes representing three conditions: psychosis, subthreshold psychosis (indicating ‘attenuated’ psychosis symptoms), and no psychotic symptoms. Practitioners’ responses suggested that APS is viewed consistently with a DSM-IV-TR defined mental disorder and that most clinicians may diagnose this condition as a full threshold psychotic disorder. Findings tentatively suggest that the inclusion of an attenuated psychosis symptoms category in the forthcoming DSM-5 may be helpful in improving diagnostic reliability and facilitating best practice among community practitioners.
Keywords: diagnosis, DSM, prodrome, psychosis, schizophrenia, vignette
1. Introduction
Among those who develop schizophrenia, approximately 70–90% experience attenuated psychotic symptoms prior to meeting diagnostic criteria for the disorder (Compton et al., 2009; Häfner & an der Heiden, 1999; Yung & McGorry, 1996). Recently, the DSM-5 Psychotic Disorders Workgroup coined the term “Attenuated Psychosis Syndrome” (APS) to characterize subthreshold positive symptoms (e.g., unusual thought content, suspiciousness, perceptual disturbances) that co-occur with distress and/or disability (Association). Though APS does not inevitably signal an impending psychotic break, attenuated symptoms may predict psychosis onset and cause functional decline (Yung, Nelson, Thompson, & Wood, 2010).
A growing body of literature documents the disability often associated with attenuated psychotic symptoms. Researchers have reported average Global Assessment of Functioning (GAF) scores of 60.5, 40, and 37 in samples of those with attenuated psychotic symptoms, indicating notable impairment (Miller et al., 2003; Yung et al., 2003). In a study comparing quality of life among individuals with psychosis, attenuated psychosis, and no symptoms, Bechdolf (Bechdolf et al., 2005) found that the attenuated psychosis group reported the poorest quality of life. Preda (Preda et al., 2002) found that 90% of individuals meeting criteria for APS had prior treatment history, suggesting high frequency of help-seeking behavior in this population.
Recent research efforts (Cannon et al., 2008; Klosterkötter, 2008) have focused on conceptualizing the period of attenuated symptoms that often precedes psychosis onset. Researchers have developed reliable instruments to identify those at heightened risk for developing psychotic disorders, with rates of psychosis onset ranging from 14 to 54 percent over a one to two year period among individuals determined to be ‘high risk’ according to various paradigms (Cannon et al., 2008; Klosterkötter, Hellmich, Steinmeyer, & Schultze-Lutter, 2001; Miller et al., 2003; Nelson & Yung, 2010; Ruhrmann et al., 2010; Yung et al., 2005). In addition, researchers tested promising treatments for APS that may reduce associated distress and delay or prevent the onset of psychosis (Amminger et al., 2010; Compton, McGlashan, & McGorry, 2007; McGlashan et al., 2006; McGorry et al., 2009; Morrison et al., 2007). Advances in identification and treatment of APS are also important as shorter duration of untreated psychosis (DUP) has been associated with better long-term prognosis in schizophrenia (Marshall et al., 2005).
Despite this potential for improved treatments and outcomes, advances in research are not yet incorporated into the diagnostic system for mental disorders. The Diagnostic and Statistical Manual of Mental Disorders, fourth edition text revision (DSM-IV-TR) (American Psychiatric Association, 2000) defines the term ‘psychotic’ loosely, referring simply to “the presence of certain symptoms” (i.e., delusions, hallucinations, and disorganization symptoms). The DSM-IV-TR acknowledges the existence of “prodromal” and “residual” periods in which individuals “may express a variety of unusual or odd beliefs; they may have unusual perceptual experiences; their speech may be generally understandable but digressive, vague, or overly abstract or concrete; and their behavior may be peculiar but not grossly disorganized” (2000; p. 302). Though it contains this description of attenuated psychotic symptoms within the section on schizophrenia, the DSM-IV-TR gives clinicians no diagnosis which uniquely captures the construct. Attenuated symptoms are restricted to a subset of personality disorders (e.g., schizotypal personality disorder), which are, by definition, “stable over time.” APS, in contrast, can result in various outcomes, and often precedes further deterioration into psychotic symptoms (Yung et al., 2010).
Despite the evidence that individuals experiencing APS exist and seek treatment in community settings, there is no diagnostic category appropriate for this group. It is unclear how community providers diagnose or conceptualize individuals with APS. Assessment tools for the identification of APS have been employed in tightly controlled research contexts (Miller et al., 2003; Yung et al., 2005), but little is known about providers’ perspectives on such cases in real-world practice.
Technically, meeting criteria for APS alone would not warrant a formal diagnosis under the current classification system, yet this syndrome indicates current impairment and implies future risk. As such, in many mental health systems, an individual with APS would not be afforded care or future monitoring. Alternatively, clinicians might lower diagnostic thresholds in order to diagnose someone experiencing APS with a full psychotic disorder. In these cases, treatments would likely be made available, but the recommended treatments might be inappropriate for APS clients. APS creates a predicament for clinicians, who lack a diagnostic label for these clients. Understanding how practitioners approach the current diagnostic dilemma related to APS may contribute to the ongoing debate regarding the potential inclusion of an attenuated psychosis risk category in DSM-5 (Carpenter, 2009; Corcoran, First, & Cornblatt, 2010; Yang, Wonpat-Borja, Opler, & Corcoran, 2010).
The current study examines how providers perceive and diagnose APS. Clinicians were asked to read vignettes depicting individuals with different levels of psychotic-like symptoms and provide diagnostic impressions. Given the impairment associated with APS, it was hypothesized that clinicians would lower the DSM-IV-TR threshold for psychosis to incorporate cases illustrating APS into the schizophrenia spectrum class of disorders.
2. Methods
2.1 Participants
A national sample of clinical psychologists (n=500), psychiatrists (n=500), and general practitioners (n=500) were targeted for participation in this study. The sample of clinical psychologists was drawn from the membership directory of the American Psychological Association (APA) through their Center for Workforce Studies. The samples of psychiatrists and general practitioners were obtained from the physician directory of the American Medical Association (AMA) through one of their database licensees, Direct Medical Data.
This study was reviewed and found to be exempt by the University of Hawaii at Manoa institutional review board, as no significant risk was anticipated from participation in a survey of practitioner behavior. In addition, the study was reviewed by the APA Committee on Workforce Studies to evaluate the study’s appropriateness for its members. It was also reviewed for appropriateness by the AMA’s database licensee, Direct Medical Data.
2.2 Materials
The current study utilized a mail/web mixed mode survey design. Consistent with the recommendation of Dillman (Dillman, 2007), all surveys materials (cover letter, postage paid envelope, survey including three vignettes with an identical set of questions following each vignette, and a set of basic demographic questions) were mailed to potential participants with an option to participate by email via a link printed on the front of the survey booklet. To avoid differences in response patterns as a result of administration mode, efforts were made to keep the presentation of the information in both formats as similar as possible.
Prior to receiving their survey, participants were mailed a pre-notice letter. One week later, they were mailed the first survey along with a cover letter and postage paid return envelope. Approximately two weeks after the first survey was mailed, a reminder postcard was sent to those individuals who had not responded. Two weeks later, a replacement survey was mailed to those who did not respond initially, along with the second version of the cover letter.
2.3 Vignettes
Vignette methodology has numerous strengths when compared to similar methods to assess practitioner performance in clinical settings (e.g., chart review, standardized patients; Fihn, 2000). Strengths include the ability to craft standardized cases, to alter cases systematically, and to present cases to a large sample of practitioners given relative time and cost effectiveness.
Vignettes in this study were developed by the first author of this study (E.J.) using methods similar to those of Epstein et al. (Epstein et al., 2001) and Kirk et al. (Kirk, Wakefield, Hsieh, & Pottick, 1999). The author created four ‘cases’ of fictional individuals (Diego, Paul, Mike, and Claire) and drafted three ‘conditions’ for each case, resulting in twelve individual vignettes. Conditions represented variations in the level of psychotic symptoms. Each vignette described the presenting case with no psychotic symptoms; attenuated psychotic symptoms; and ‘fully’ psychotic symptoms consistent with definitions of psychotic disorder presented in the DSM-IV-TR. Demographic descriptions of each character remained consistent for each symptom condition. ‘Psychosis’-level vignettes all depicted individuals in the first episode of psychotic illness. Four characters were created in order to avoid systematic covariations of symptom level, gender, and ethnicity.
The vignettes were initially rated by five graduate students in a clinical psychology doctorate program trained in the administration of the most widely used diagnostic instrument for APS (SIPS; Miller et al., 2003). Raters were asked to (a) compare the vignettes to a set of criteria used to develop the vignettes, (b) write which level of symptoms were being described, and (c) estimate the GAF score of the individual depicted in each vignette. Graduate student raters were in complete agreement on 12 of 12 vignettes as to which levels of symptoms were being described. Average GAF scores were in the intended range for each vignette with the exception of one attenuated symptoms vignette that was subsequently revised.
Each vignette was then reviewed by five experts in the field of psychotic disorders and was further revised based on expert suggestions. All vignettes were rated by one of the authors J.S.), as well as a Masters level clinical psychology graduate student of the author (five relevant publications) who was otherwise uninvolved with this study. Other experts included six clinical psychologists (average of 31 relevant publications), one Masters level psychology researcher (nine publications), and two psychiatrists (average of 13 relevant publications).
Experts were asked to read vignettes developed by the author and respond to the question “How well do you feel the vignette depicts the construct of someone experiencing [psychotic level, APS level, and no psychotic] symptoms?” At least 80% of the expert raters described each vignette as representing the intended conditions “well” or “very well.” See Table 1 for sample vignettes for each symptom level.
Table 1.
Vignette excerpts illustrating symptom levels
| Symptom Level | Excerpt |
|---|---|
| No Psychosis | Mike is an 18-year-old African American male, currently enrolled in his senior year of high school. His parents brought him to see you after noticing “odd” behavior that caused them concern. Mike’s father reported that Mike had gotten into several fights in the last year and this worried them. Mike reported that he understood his parents’ concerns, but that the fights had been in self-defense, which the school and his teachers confirmed. Mike has been, according to all reporters, a consistently good student (A–B range) and is well-liked by his peers. He had recently won a high level chess tournament for which he was given recognition, and his mother said that this caused some of the students at his school to tease him. He reported to you that he was taking the situation “in stride”, knowing that he would soon be graduating, and did not feel he needed any help. He said that, in general, he maintains a positive outlook even when difficult situations arise. Throughout the interview, Mike was cooperative and communicated in a clear, effective manner about his situation. Mike and his mother reported that Mike has no history of alcohol or drug use. Medical tests have also not produced any significant findings. |
| Attenuated Psychosis | Claire is a 17-year-old Caucasian female, currently enrolled in her junior year of high school. Her mother brought Claire to see you after noticing “odd” behavior that caused her concern. Claire has an uncle with schizophrenia. Her mother reported that Claire’s “strange” behavior has been occurring for approximately 5 months. Claire reported that once or twice per week she has heard a whispering voice when she’s in her room alone, but she was not sure where it was coming from or what it was saying. Claire felt it was possible that it might be a problem with her hearing, though it sounded real. During the interview, Claire at times needed to be redirected back to the topic and would bring up unrelated issues. Her mother reported that she was concerned because Claire hardly went out with her friends at all lately, and they were not calling the house anymore. Claire reported that she thinks her friends gossip about her behind her back, but she was not sure what they were saying. Claire’s mother had also been contacted by a school counselor who informed her that Claire’s academic performance was deteriorating dramatically from an A average to a C-D average. Claire and her mother both reported that Claire has no history of alcohol or drug use. Medical tests have also not produced any significant findings. |
| Psychosis | Diego is a 17-year-old Hispanic male, currently attending his junior year of high school. His mother brought him to see you after noticing “odd” behavior that caused her concern. Diego’s mother reported that his father has resided in a psychiatric hospital in Mexico for years for “strange” behavior including hearing voices. Diego’s mother reported that she would have brought him in sooner, but previously he had refused saying he did not want to talk to anyone about his experiences. She said that recently, he has not spoken much to anyone. She reported that approximately a year ago, he started being particularly picky about his food, and more recently blamed the neighbor of trying to poison him to take him “out of the picture”. His mother reported that there was no evidence for this and that the neighbor was a close family friend, but that Diego has become very angry in the past when she has attempted to challenge his beliefs. She also said that Diego is frequently agitated at school because he feels other teenagers are plotting against him. Diego initially refused to talk to you, but later opened up, saying in a slow, flat voice that he felt depressed, that the world was “so cruel”, and that he would “probably die soon” from other people’s actions. However, he could not provide specific details on why he thought this. He said that he found it very difficult to do anything and to express himself to others. Diego’s mother stated that he has been in all special education classes for several years, and that she was considering withdrawing him from classes as he was not progressing in his work. Diego reported that he very occasionally has one or two alcoholic beverages when with friends. Medical tests have not produced any significant findings. |
2.4 Mailing
Participants received stapled surveys containing vignettes depicting three of the four different cases (Claire, Diego, Mike and Paul) and questions following each vignette. Twelve versions of the survey were created. Each survey included one vignette describing psychosis, one vignette describing attenuated symptoms, and one vignette describing no psychosis. The order of the three vignettes in the different versions was counterbalanced by level of psychotic symptoms to control for order effects. Each vignette (case and level) was represented equally across versions.
Instructions were provided for participants to read each vignette and answer questions that followed. Respondents were asked to mark ‘yes’ or ‘no’ in response to the question, “Do you think that the individual described above has a MENTAL DISORDER as described by the DSM-IV-TR?” Respondents were asked to provide diagnostic impressions both by choosing a DSM-IV-TR disorder category (e.g., adjustment disorders, mood disorders, personality disorders) from a provided list as well as by generating the diagnostic code or full disorder name for the diagnosis they felt would be most appropriate.
3. Results
The overall adjusted response rate was 20.8% (n=303) after eliminating those without forwarding addresses (n=27) and those who were retired (n=14). Response rates by practitioner types were 26.3% (n=130) for psychologists, 20.4% (n=98) for psychiatrists, and 14.8% (n=72) for general practitioners. Missing data across variables ranged from 1.0 to 8.3% and were analyzed as a separate category as has been done in other studies using similar analyses (Baldwin et al., 2009; Lindstrom & Mohseni, 2009; Nikula, Gissler, Jormanainen, Sevon, & Hemminki, 2009).
3.1 Practitioner Characteristics
The average age of clinicians who participated was 52.7 years (median = 53.0 years); 52.4% were male; 86.3% were White. All participants reported that they were licensed to practice in their field. They reported an average length of time of 21.2 years as active practitioners. Missing data included 2.4% of participants who did not respond to demographic information.
3.2 Primary Analyses
The primary research aim was to examine the frequency with which vignette cases of attenuated psychosis symptoms were considered by practitioners to have a mental disorder. The first survey item following each vignette queried practitioners with regard to whether they thought the individual described in the vignette had a mental disorder, as defined by the DSM-IV-TR. As no significant differences were found between provider types in their consideration of APS to be a mental disorder (χ2 = 5.0, P = .16), data were collapsed across provider type. Results for all three symptom levels are presented in Table 2.
Table 2.
Practitioners’ ratings of whether vignettes depicted a disorder as defined by DSM-IV-TR
| Symptom Level | Mental Disorder? | |
|---|---|---|
| Yes | No | |
| No psychosis (missing = 5) | 40 (13.4%) | 258 (86.6%) |
| Attenuated psychosis (missing = 16) | 265 (92.3%) | 22 (7.7%) |
| Full-threshold psychosis (missing = 8) | 280 (94.9%) | 15 (5.1%) |
APS vignettes vs. no symptoms vignette as representative of a mental disorder (χ2 = 364.80, P < .001)
APS vignettes vs. full-threshold psychosis vignette as representative of a mental disorder (χ2 = 1.62, P = NS)
Chi-square statistics were calculated to evaluate the degree to which practitioners view APS as a mental disorder relative to the other symptom levels. In other words, we were interested in whether practitioners were more likely to conceptualize APS more similarly to no psychosis or more similarly to full psychosis. Practitioners were significantly more likely to consider vignettes depicting APS as representative of a mental disorder compared with vignettes depicting “no symptoms” (χ2 = 364.80, P < .001). No significant differences emerged between the number of practitioners who considered symptoms of full-threshold psychosis to indicate the presence of a mental disorder relative to symptoms of APS (χ2 = 1.62, P = .40).
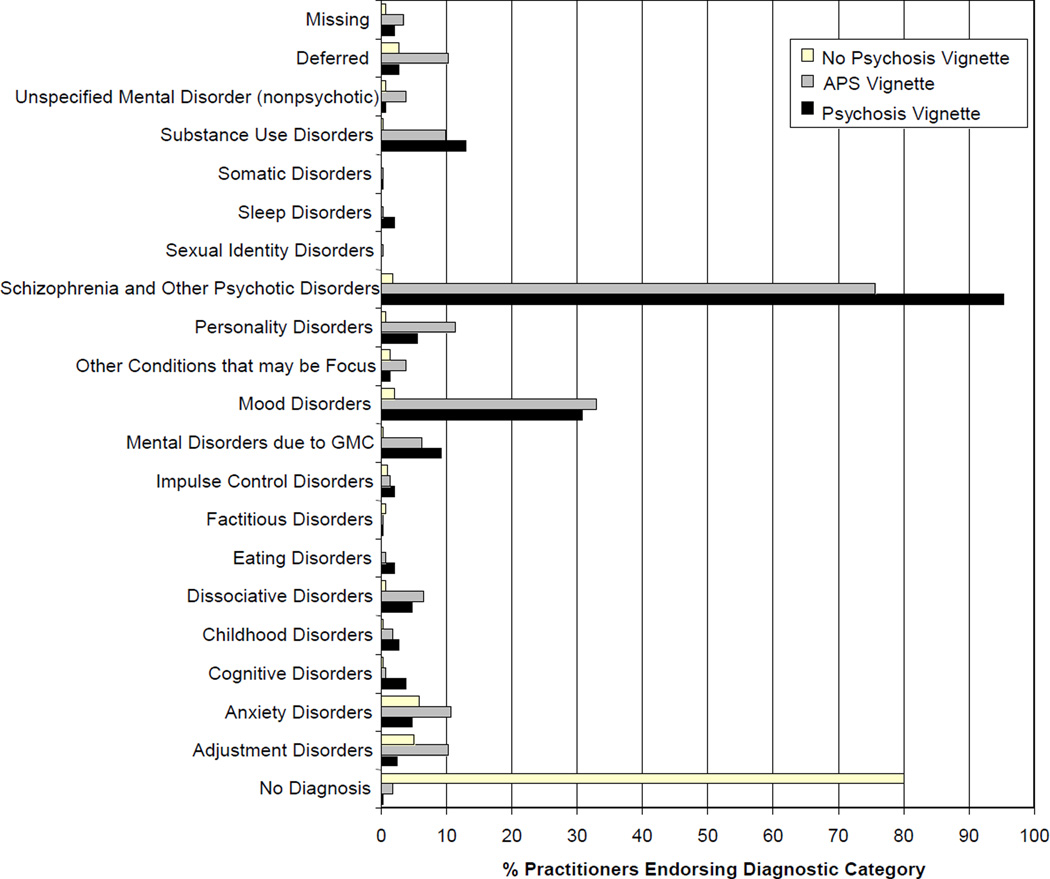
The secondary research aim was to discover the DSM-IV-TR classes of disorders which practitioners utilized to diagnose APS. A graph depicting practitioners’ choices of diagnostic classes for each symptom level appears below [Figure 1]. Schizophrenia and other psychotic disorders was the class most frequently chosen by practitioners responding to both the psychosis vignettes (280 of 295 responders, or 94.9%) and the APS vignettes (228 of 291 responders, or 78.4%). For the ‘no psychosis’ condition, only 5 of 298 responders (1.7%) considered the symptoms in the vignette to represent schizophrenia or other psychotic disorders.
Figure 1.
Disorder classes chosen by practitioners responding to vignettes
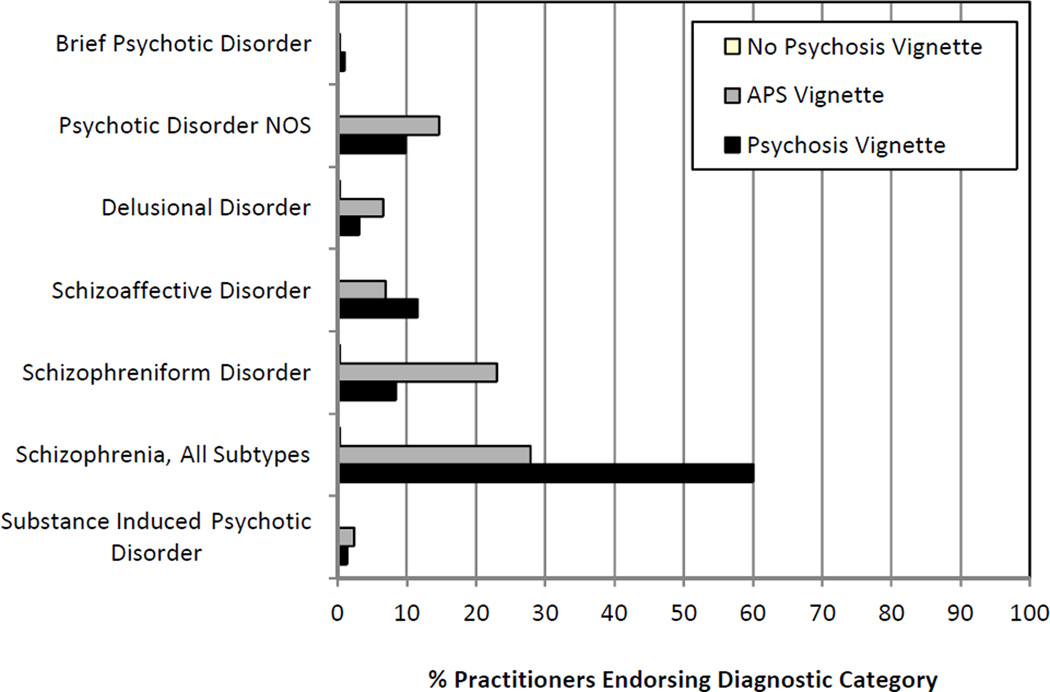
Statistically, the APS vignette was far more likely to be rated within the schizophrenia spectrum relative to the no psychosis vignette (χ2 = 362.00, P < .001, effect size d = 2.53). The APS vignette was significantly less likely to be rated within the schizophrenia spectrum relative to the psychosis vignette (χ2 = 34.84, P < .001, effect size d = 0.50). Although the vast majority of practitioners diagnosed the APS vignettes as in the schizophrenia spectrum, relative to the psychosis vignettes, visual analysis of graphed response frequency shows that the APS vignettes were categorized more often by this sample as personality disorders, anxiety disorders, adjustment disorders, and “deferred” compared with the psychosis vignettes. Within the schizophrenia spectrum, more practitioners assigned a “schizophreniform” or “psychosis NOS” label to APS vignettes relative to full psychosis vignettes [Figure 2].
Figure 2.
Schizophrenia spectrum disorders chosen by practitioners responding to vignettes
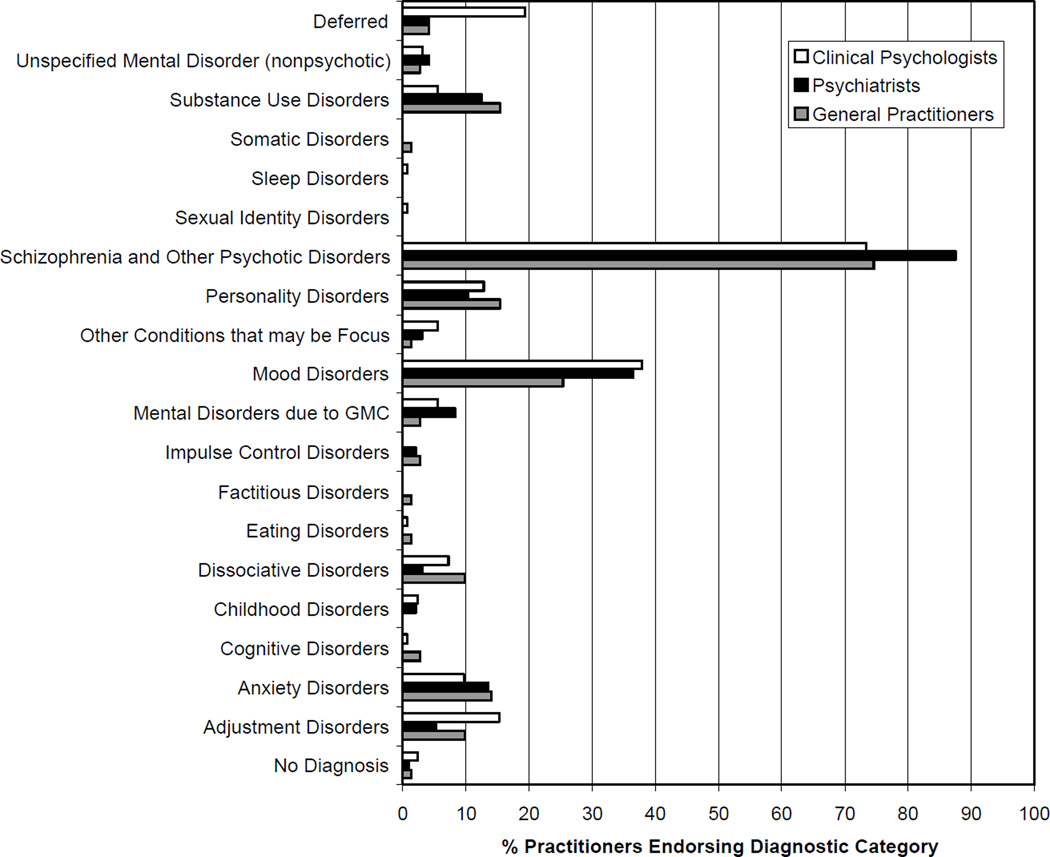
Also of interest are differences with regard to which diagnostic categories were chosen in response to the APS vignette by the three types of practitioners surveyed. Figure 3 illustrates the percentage of each type of practitioner choosing the various diagnostic classes.
Figure 3.
Disorder classes chosen in response to APS vignette, by practitioner type
4. Discussion
4.1 Implications of current findings
Real-world practitioner participants in this study were asked to apply DSM-IV-TR criteria for a mental disorder to symptoms of APS, a category not formally recognized by the manual. They were asked to consider whether individuals exhibiting APS have a mental disorder, and if so, which class of disorder best captures these symptoms. The DSM-IV-TR defines a ‘mental disorder’ somewhat loosely as:
A clinically significant behavioral or psychological syndrome or pattern that occurs in an individual and that is associated with present distress (e.g., a painful symptom) or disability (i.e., impairment in one or more important areas of functioning) or with a significantly increased risk of suffering death, pain, disability, or an important loss of freedom. (American Psychiatric Association, 2000)
The results presented above indicate that the vast majority (92.3%) of practitioners sampled considered APS to constitute a mental disorder. These clinicians categorized APS as a mental disorder about as often as they did psychosis itself. Research suggesting that attenuated psychotic symptoms are often associated with distress and impairment (Bechdolf et al., 2005; Rosen, Woods, Miller, & McGlashan, 2002; Yung et al., 2010) supports the appropriateness of this conceptualization of APS as a mental disorder.
The great majority of clinicians judged APS to be within the schizophrenia spectrum of disorders. Thus, clinicians in our sample recognized APS as being more related to psychosis than to other classes of disorders. Clinically this may be problematic, as these symptoms do not reflect ‘true’ psychosis. Practitioners who diagnose clients with APS as having a schizophrenia spectrum disorder may, for instance, implement the American Psychiatric Association (APA) recommendation of antipsychotic medication as a first-line treatment for schizophrenia (Lehman et al., 2004), despite the lack of evidence supporting pharmacotherapy’s effectiveness for treating APS ("International clinical practice guidelines for early psychosis", 2005). Nelson and Yung (2010) found that many community practitioners appear to over-prescribe antipsychotic medications to individuals with APS symptoms.
Within the schizophrenia spectrum, APS vignettes were more likely to elicit diagnoses of schizophreniform disorder or psychosis NOS than were full psychosis vignettes, which were more frequently categorized as schizophrenia. This divergence may indicate that respondents were mindful of the emerging or subthreshold nature of symptoms in the APS vignettes, and sought out a diagnostic category to reflect this difference.
Not all clinicians, however, categorized the APS group within the schizophrenia spectrum. As such, clinicians in our sample exhibited greater divergence with regard to which diagnostic class best captured the symptoms of APS compared to the symptoms of full psychosis. This result suggests that clinicians were not as reliable in selecting an existing category for APS. The absence of a diagnostic category which specifically captures subthreshold psychosis symptoms in DSM-IV-TR may undermine diagnostic reliability for clients who present with APS.
Clinical guidance for the treatment of APS has been issued by both the APA (Lehman et al., 2004) and the International Early Psychosis Writing Group (2005). In the most recent Practice Guideline, the APA recommends that persons who are “prodromally symptomatic and at risk for psychosis” receive assessment and monitoring until symptoms remit or evolve into “schizophrenia or another diagnosable and treatable mental disorder” (Lehman et al., 2004). Similarly, the International group advises regular monitoring of symptoms, treatment for any comorbid syndromes such as depression or substance abuse, and psychoeducation for individuals with APS ("International clinical practice guidelines for early psychosis", 2005). This group states that due to high rates of adverse effects and limited evidence supporting the usefulness of pharmacotherapy for attenuated psychosis, antipsychotic medications are not recommended for APS except in the case of rapid deterioration or severe suicidal risk ("International clinical practice guidelines for early psychosis", 2005).
These treatment guidelines place clinicians who encounter individuals with APS in a bind. Providers have practice guidelines for a disorder that cannot be diagnosed using the current manual. Thus the practice guidelines of the APA and Early Psychosis Writing Group apply, at least theoretically, to a clinical population that does not exist. Clients who meet criteria for APS are in a position of being either over- or under-treated. This confusion is relevant to current discussions regarding the inclusion of APS in DSM-5, as it highlights the primacy problem at the core of the debate. Which comes first, the diagnostic category or the treatment guidelines?
4.2 Limitations
Limitations of the current study include the low response rate and limitations inherent to vignette methodology. The overall crude response rate for practitioners targeted in our sample was 20.2%. Responding was likely non-random and may have been related to variables such as practitioner experience, type, and setting. Non-responding clinicians may also represent those who did not participate due to lack of familiarity and confidence with APS symptoms. Nonetheless, efforts to capture a wide sample of practitioners yielded a fairly large N, providing confidence in the pattern of findings.
Vignettes also convey limitations relative to real-world practice data. Although vignettes provide a time- and cost-efficient standardized assessment of clinician practices, vignettes lack the complexity and ambiguity of real-life practice situations (Fihn, 2000). Vignettes may elicit optimized responses from practitioners that do not accurately reflect everyday practice (Leonard & Masatu, 2005).
4.3 DSM-5 discussion
The findings presented above may be useful in the current debate over the possible inclusion of an attenuated symptoms category in the forthcoming DSM-5. Data from the current study indicate that the vast majority of clinicians surveyed perceive APS to constitute a mental disorder, and that the lack of an appropriate diagnostic category in DSM-IV-TR may undermine diagnostic reliability. Taken together with the existence of reliable instruments to identify APS (e.g., the SIPS), these findings tentatively suggest that the inclusion of an APS category may help to improve diagnostic reliability and facilitate evidence-based practice.
Contributor Information
Elizabeth Jacobs, University Of Hawaii, Manoa.
Emily Kline, University Of Maryland, Baltimore County.
Jason Schiffman, University Of Maryland, Baltimore County.
References
- Amminger GP, Schäfer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, et al. Long-chain ω-3 fatty acids for indicated prevention of psychotic disorders: A randomized, placebo-controlled trial. Arch. Gen. Psychiatry. 2010;67(2):146–154. doi: 10.1001/archgenpsychiatry.2009.192. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. DSM-5 Development: Attenuated Psychosis Syndrome. Retrieved January 25, 2011, from http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=412.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th, Text-Revised ed. Washington, DC: Author; 2000. [Google Scholar]
- Baldwin L-M, Grossman DC, Murowchick E, Larson EH, Hollow WB, Sugarman JR, et al. Trends in perinatal and infant health disparities between rural American Indians and Alaska Natives and rural Whites. Am. J. Public Health. 2009;99(4):638–646. doi: 10.2105/AJPH.2007.119735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechdolf A, Pukrop R, Köhn D, Tschinkel S, Veith V, Schultze-Lutter F, et al. Subjective quality of life in subjects at risk for a first episode of psychosis: A comparison with first episode schizophrenia patients and healthy controls. Schizophr. Res. 2005;79(1):137–143. doi: 10.1016/j.schres.2005.06.008. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, et al. Prediction of psychosis in youth at high clinical risk: A multisite longitudinal study in North America. Arch. Gen. Psychiatry. 2008;65(1):28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter WT. Anticipating DSM-V: Should psychosis risk become a diagnostic class? Schizophr. Bull. 2009;35(5):841–843. doi: 10.1093/schbul/sbp071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Kelley ME, Ramsay CE, Pringle M, Goulding SM, Esterberg ML, et al. Association of pre-onset cannabis, alcohol, and tobacco use with age at onset of prodome and age at onset of psychosis in first-episode patients. Am. J. Pyschiatry. 2009;166(11):1251–1257. doi: 10.1176/appi.ajp.2009.09030311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, McGlashan TH, McGorry PD. An overview of prodromal states, the duration of untreated psychosis, and early intervention paradigms. Psychiatric Annals. 2007;37(5):340–348. [Google Scholar]
- Corcoran CM, First MB, Cornblatt B. The psychosis risk syndrome and its proposed inclusion in the DSM-V: A risk–benefit analysis. Schizophr. Res. 2010;120(1–3):16–22. doi: 10.1016/j.schres.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd ed. Hoboken: John Wiley and Sons, Inc; 2007. [Google Scholar]
- Epstein SA, Gonzales JJ, Weinfurt K, Boekeloo B, Yuan N, Chase G. Are psychiatrists' characteristics related to how they care for depression in the medically ill? Results from a national case-vignette survey. Psychosomatics. 2001;42(6):482–489. doi: 10.1176/appi.psy.42.6.482. [DOI] [PubMed] [Google Scholar]
- Fihn SD. The quest to quantify quality. JAMA, J. Am. Med. Assoc. 2000;283(13):1740–1742. doi: 10.1001/jama.283.13.1740. [DOI] [PubMed] [Google Scholar]
- Häfner H, an der Heiden W. The course of schizophrenia in the light of modern follow-up studies: The ABC and WHO studies. Eur. Arch. Psychiatry and Clin. Neurosci. 1999;249(Suppl 4):IV/14-IV/26. doi: 10.1007/pl00014180. [DOI] [PubMed] [Google Scholar]
- International clinical practice guidelines for early psychosis. Br. J. Psychiatry. 2005;187(Suppl48):s120–s124. doi: 10.1192/bjp.187.48.s120. [DOI] [PubMed] [Google Scholar]
- Kirk SA, Wakefield JC, Hsieh DK, Pottick KJ. Social context and social workers' judgment of mental disorder. Soc. Serv. Review. 1999;73(1):82–104. [Google Scholar]
- Klosterkötter J. Indicated prevention of schizophrenia. Dtsch. Arztebl. Int. 2008;105(30):532–539. doi: 10.3238/arztebl.2008.0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klosterkötter J, Hellmich M, Steinmeyer EM, Schultze-Lutter F. Diagnosing schizophrenia in the initial prodromal phase. Arch. Gen. Psychiatry. 2001;58(2):158–164. doi: 10.1001/archpsyc.58.2.158. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. Practice guideline for the treatment of patients with schizophrenia. 2004 [PubMed] [Google Scholar]
- Leonard KL, Masatu MC. The use of direct clinician observation and vignettes for health services quality evaluation in developing countries. Soc. Sci. Med. 2005;61(9):1944–1951. doi: 10.1016/j.socscimed.2005.03.043. [DOI] [PubMed] [Google Scholar]
- Lindstrom M, Mohseni M. Social capital, political trust and self-reported psychological health: A population-based study. Soc. Sci. Med. 2009;68(3):436–443. doi: 10.1016/j.socscimed.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association Between Duration of Untreated Psychosis and Outcome in Cohorts of First-Episode Patients. Arch. Gen. Psychiatry. 2005;62(9):975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller T, Woods SW, et al. Randomized, Double-Blind Trial of Olanzapine Versus Placebo in Patients Prodromally Symptomatic for Psychosis. Am. J. Pyschiatry. 2006;163(5):790–799. doi: 10.1176/ajp.2006.163.5.790. [DOI] [PubMed] [Google Scholar]
- McGorry PD, Nelson B, Amminger GP, Bechdolf A, Francey SM, Berger G, et al. Intervention in individuals at ultra-high risk for psychosis: a review and future directions. J. Clin. Psychiatry. 2009;70(9):1206–1212. doi: 10.4088/JCP.08r04472. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, et al. Prodromal Assessment With the Structured Interview for Prodromal Syndromes and the Scale of Prodromal Symptoms: Predictive Validity, Interrater Reliability, and Training to Reliability. Schizophr. Bull. 2003;29(4):703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- Morrison AP, French P, Parker S, Roberts M, Stevens H, Bentall RP, et al. Three-year follow-up of a randomized controlled trial of cognitive therapy for the prevention of psychosis in people at ultrahigh risk. Schizophr. Bull. 2007;33(3):682–687. doi: 10.1093/schbul/sbl042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson B, Yung AR. Can clinicians predict psychosis in an ultra high risk group? Aust. N. Z. J. Psychiatry. 2010;44(7):625–630. doi: 10.3109/00048671003620210. [DOI] [PubMed] [Google Scholar]
- Nikula M, Gissler M, Jormanainen V, Sevon T, Hemminki E. Sexual behaviour and lifestyles of young men in Finland, 1998–2005. Cross-sectional survey of military conscripts. Eur. J. Contracept. Reprod. Health Care. 2009;14(1):17–26. doi: 10.1080/13625180802635654. [DOI] [PubMed] [Google Scholar]
- Preda A, Miller TJ, Rosen JL, Somjee L, McGlashan TH, Woods SW. Treatment histories of patients with a syndrome putatively prodromal to schizophrenia. Psych. Serv. 2002;53(3):342–344. doi: 10.1176/appi.ps.53.3.342. [DOI] [PubMed] [Google Scholar]
- Rosen JL, Woods SW, Miller TJ, McGlashan TH. Prospective observations of emerging psychosis. J. Nerv. Ment. Dis. 2002;190(3):133–141. doi: 10.1097/00005053-200203000-00001. [DOI] [PubMed] [Google Scholar]
- Ruhrmann S, Schultze-Lutter F, Salokangas RKR, Heinimaa M, Linszen D, Dingemans P, et al. Prediction of psychosis in adolescents and young adults at high risk: Results from the prospective european prediction of psychosis study. Arch. Gen. Psychiatry. 2010;67(3):241–251. doi: 10.1001/archgenpsychiatry.2009.206. [DOI] [PubMed] [Google Scholar]
- Yang LH, Wonpat-Borja AJ, Opler MG, Corcoran CM. Potential stigma associated with inclusion of the psychosis risk syndrome in the DSM-V: An empirical question. Schizophr. Res. 2010;120(1–3):42–48. doi: 10.1016/j.schres.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung AR, McGorry PD. The initial prodrome in psychosis: Descriptive and qualitative aspects. Aust. N. Z. J. Psychiatry. 1996;30(5):587–599. doi: 10.3109/00048679609062654. [DOI] [PubMed] [Google Scholar]
- Yung AR, Nelson B, Thompson A, Wood SJ. The psychosis threshold in ultra high risk (prodromal) research: Is it valid? Schizophr. Res. 2010;120(1–3):1–6. doi: 10.1016/j.schres.2010.03.014. [DOI] [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, et al. Psychosis prediction: 12-month follow up of a high-risk ('prodromal') group. Schizophr. Res. 2003;60(1):21–32. doi: 10.1016/s0920-9964(02)00167-6. [DOI] [PubMed] [Google Scholar]
- Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, et al. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust. N. Z. J. Psychiatry. 2005;39(11–12):964–971. doi: 10.1080/j.1440-1614.2005.01714.x. [DOI] [PubMed] [Google Scholar]