Abstract
Aims
Catheter-based renal nerve ablation (RNA) using radiofrequency energy is a novel treatment for drug-resistant essential hypertension. However, the local endothelial and vascular injury induced by RNA has not been characterized, although this importantly determines the long-term safety of the procedure. Optical coherence tomography (OCT) enables in vivo visualization of morphologic features with a high resolution of 10–15 µm. The objective of this study was to assess the morphological features of the endothelial and vascular injury induced by RNA using OCT.
Methods and results
In a prospective observational study, 32 renal arteries of patients with treatment-resistant hypertension underwent OCT before and after RNA. All pre- and post-procedural OCT pullbacks were evaluated regarding vascular changes such as vasospasm, oedema (notches), dissection, and thrombus formation. Thirty-two renal arteries were evaluated, in which automatic pullbacks were obtained before and after RNA. Vasospasm was observed more often after RNA then before the procedure (0 vs. 42%, P < 0.001). A significant decrease in mean renal artery diameter after RNA was documented both with the EnligHTN™ (4.69 ± 0.73 vs. 4.21 ± 0.87 mm; P < 0.001) and with the Simplicity® catheter (5.04 ± 0.66 vs. 4.57 ± 0.88 mm; P < 0.001). Endothelial-intimal oedema was noted in 96% of cases after RNA. The presence of thrombus formations was significantly higher after the RNA then before ablation (67 vs. 18%, P < 0.001). There was one evidence of arterial dissection after RNA with the Simplicity® catheter, while endothelial and intimal disruptions were noted in two patients with the EnligHTN™ catheter.
Conclusion
Here we show that diffuse renal artery constriction and local tissue damage at the ablation site with oedema and thrombus formation occur after RNA and that OCT visualizes vascular lesions not apparent on angiography. This suggests that dual antiplatelet therapy may be required during RNA.
Keywords: Optical coherence tomography, Catheter-based renal nerve ablation, Vascular lesions, Simplicity catheter system, EnligHTN multi-electrode renal denervation catheter
Introduction
Today approximately one billion people are affected by arterial hypertension.1–5 Data of the World Health Organization suggest that one in three adults suffer from elevated blood pressure resulting in a worldwide socioeconomic health problem. Indeed, the link between high blood pressure and increased cardiovascular morbidity and mortality is well established.6–8 Despite the availability and use of different classes of antihypertensive drugs, 5–30% of patients still show elevated blood pressure.9–12
Blood pressure is regulated by the sympathetic nervous system, hormonal and endothelial factors as well as renal water and sodium handling. The kidney is innervated by efferent and afferent sympathetic nerves regulating renal vascular resistance and renin release.13 Recently, a novel catheter-based radiofrequency ablation technique has been developed allowing for renal nerve ablation (RNA) with a very low complication rate and without major side effects.14 Registry data and small randomized trials have shown that RNA effectively lowers blood pressure in patients with treatment-resistant hypertension. Currently, two different catheter-based systems are primarily used.15–17 The Simplicity® catheter by Medtronic-Adrian is a sequential denervation system allowing for delivery of low-power radiofrequency energy of 5–8 W at several sites within the renal artery. The EnligHTN™ multi-electrode RNA catheter from St Jude Medical consists of a multi-ablation basket with an integrated four-point contact surface to deliver radiofrequency energy. However, data regarding the local vascular injury induced by the radiofrequency energy are lacking. This is of importance for the long-term safety of the procedure, particularly since the development of a renal artery stenosis after RNA has been reported.18
Optical coherence tomography (OCT) has been established as an intracoronary imaging tool visualizing stent apposition and healing, plaque characterization, thrombus formation, and dissection with a high spatial resolution of 10–15 µm,19 which is ∼10-fold higher than intravascular ultrasound (IVUS).20 Therefore, the aim of the present study was to evaluate the morphological features before and after renal ablation by OCT prospectively.
Methods
Patient population
This is a prospective observational double-centre study conducted at the University Hospital of Zurich and Cantonal Hospital of Lucerne, Switzerland. Individuals were eligible for the study if they were >18 years old and had primary and idiopathic cause of resistant arterial hypertension defined as persistent systolic blood pressure >160 mmHg, with at least established three antihypertensive medication (including diuretics) or patients with allergies to antihypertensive drugs. All patients were on daily aspirin 100 mg or received 250–500 mg aspirin intravenously before starting the RNA procedure. One patient was on single clopidogrel treatment because of in-stent thrombosis in the past after myocardial infarction. No patient was on dual antiplatelet therapy at the time of the procedure.
Patients were excluded from the study, if glomerular filtration rate was <45 mL/min.
Sixteen consecutive patients were included and 32 renal arteries were accurately evaluated. All patients underwent RNA with the Simplicity® catheter by Medtronic-Adrian or the EnligHTN™ multi-electrode by St Jude Medical according to the operator's discretion. All patients provided written informed consent before the procedure.
Catheter-based renal denervation procedure
The RNA procedure with the Simplicity® system (Medtronic, Minneapolis, MN, USA) consists of a catheter-based approach to disrupt renal sympathetic nerves using radiofrequency energy (1 Watt) applied to the renal artery via an electrode at the catheter tip. The catheter was placed in the distal lumen of the main renal artery using a 6F guide via a femoral artery access site. Then the catheter was retracted sequentially by 5 mm each and rotated circumferentially before energy was delivered. A total of six to eight ablations of 2 min duration were applied in each renal artery including the complete circumference of the vessel.
RNA with the EnligHTN™ multi-electrode renal denervation ablation catheter (St Jude Medical Inc., Westford, USA) involves a basket with multiple ablation surface points. The catheter was placed in the distal lumen of the main renal artery using a 6F guide and four ablations were set sequentially in 90-s intervals. Afterwards a minimal catheter repositioning was performed and the procedure was repeated more proximally.
Optical coherence tomography
All patients underwent OCT utilizing the C7-XR imaging system (LightLab Imaging, Inc., Westford, USA) before and after renal denervation. Optical coherence tomography images were performed by using a non-occlusive acquisition technique and a single-mode optical fibre catheter (frequency domain-OCT-catheter, DragonFly™, St Jude Medical). In each renal artery, routinely two pullbacks were obtained pre- and post-RNA. The OCT catheter was advanced over a conventional 0.014′ angioplasty guide wire using a monorail lumen at the tip. Renal arteries were flashed of blood with Ultravist 300 (Bayer House, Berkshire, UK) at a flow rate of 8.0 mL/s. The automated pullback and contrast injection was obtained in all patients to optimize the image quality. The acquisition sequence speed was 20 mm/s.
Optical coherence tomography evaluation
Optical coherence tomography pullbacks were analysed in a teaching core laboratory of the Andreas Gruentzig-Catheterization Laboratory at the University Hospital of Zurich, Switzerland, by two independent investigators blinded to the clinical and procedural characteristics of the patients, using a proprietary software (LightLab Imaging). Image quality was assessed for all OCT images using a four-point scale (excellent, good, moderate, non-diagnostic, and artefact). In the presence of disagreement between the two observers, a consensus agreement was made. All pre- and post-procedural pullbacks were evaluated for local acute morphological vascular changes such as vasospasm, dissections, wall oedemas (vessel notches), and thrombus formations. Lumen and cross-sectional areas were drawn at 3 mm intervals and calculated as appropriate. Automatic detection of mean diameter was manually corrected frame by frame.
Lesion characterization by optical coherence tomography
Oedema was defined as any significant endothelial–intimal notch detected on the luminal wall surface. Vasospasm was defined by immediate loss of lumen area or lumen diameter in any part of renal artery. Endothelial or intimal disruptions of the superficial intimal lining were defined as endothelial detachments or vessel dissections. Intraluminal thrombus was defined as a protruding mass attached to the luminal surface with a diameter of ≥0.5 mm in at least three following cross-sections.
Statistical analysis
Baseline characteristics are summarized using frequency tables with count and proportion for each category, or mean and standard deviation (SD) as appropriate. All data were checked by means of Shapiro–Wilks W test for normal distribution. We then performed paired t-test for the pre- and post-comparisons for continuous variables. McNemars test was used for nominal variables.
SPSS software (Chicago, IL, USA; Version 20.0) was used for all statistical analysis. A two-tailed P-value of ≤0.05 was considered as statistical significant. Data are shown as percentages.
Results
Baseline characteristics
Sixteen patients were included based on the image quality in the final analysis, nine males and seven females. The average age was 58.5 ± 9.9 years. All patients had drug-resistant hypertension (n = 14) or intolerance and/or allergy towards antihypertensive agents (n = 2). Of all patients included into the study, 56% had dyslipidaemia (n = 9), 19% diabetes mellitus (n = 3), 56% obesity (n = 9), 38% were current smoker at the time of inclusion (n = 6), and 25% had known coronary artery disease or a stroke (n = 4). The average number of antihypertensive drugs was 3.8 ± 1.1. Drugs on admission, laboratory values, and baseline characteristics are given in Table 1.
Table 1.
Baseline characteristics
| All patients (n = 16) | Simplicity® (n = 11) | EnligHTN™ (n = 5) | P value | |
|---|---|---|---|---|
| Age (years), mean (±SD) | 58.5 (±9.9) | 58.3 (±8.7) | 59.0 (±13.7) | 0.90 |
| Male gender, n (%) | 9 (56) | 6 (55) | 3 (60) | 0.84 |
| Cardiovascular risk factors, n (%) | ||||
| Arterial hypertension | 16 (100) | 11 (100) | 5 (100) | 1.00 |
| Dyslipidaemia | 9 (56) | 6 (55) | 3 (60) | 0.84 |
| Current smoker | 6 (38) | 5 (45) | 1 (20) | 0.33 |
| Diabetes mellitus | 3 (19) | 2 (18) | 1 (20) | 0.93 |
| Obesity | 9 (56) | 5 (45) | 4 (80) | 0.20 |
| Cardiovascular history, n (%) | ||||
| Known CAD or stroke | 4 (25) | 4 (36) | 0 | 0.12 |
| Laboratory values, mean (±SD) | ||||
| Creatinine before RNA, (μmol/L) | 78.5 (±16.5) | 77.2 (±20.3) | 81.4 (±5.7) | 0.65 |
| Creatinine after RNA, (μmol/L) | 84.5 (±23.8) | 87.1 (±28.4) | 79.4 (±11.9) | 0.57 |
| Medication, n (%) | ||||
| ACE inhibitor | 5 (31) | 5 (45) | 0 | 0.07 |
| ARB | 12 (75) | 8 (73) | 4 (80) | 0.76 |
| Beta-blocker | 12 (75) | 9 (82) | 3 (60) | 0.35 |
| Calcium-channel blocker | 10 (63) | 6 (55) | 4 (80) | 0.33 |
| Diuretics | 13 (81) | 9 (82) | 4 (80) | 0.93 |
| Statins | 8 (50) | 6 (55) | 2 (40) | 0.59 |
| Sum of medications per patient, mean (±SD) | 3.8 (±1.1) | 3.9 (±0.9) | 3.4 (±1.7) | 0.44 |
| No. of patients with drug intolerance/allergy, n (%) | 2 (13) | 1 (9) | 1 (20) | 0.54 |
ACE, angiotensin-converting enzyme; ARB, angiotensin-receptor blocker; CAD, coronary artery disease; RNA, renal nerve ablation.
Optical coherence tomography evaluation
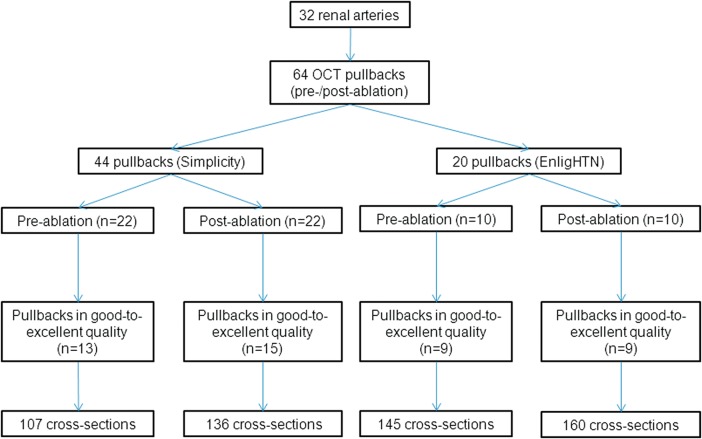
In total, 32 renal arteries were evaluated, in which two automatic pullbacks had been obtained before and after RNA. Forty-four pullbacks were performed before and after RNA with the Simplicity® catheter and 20 with the EnligHTN™ catheter. Only good-to-excellent quality pullbacks were included into the final analysis. The study flow chart is presented in Figure 1. Pullbacks with poor-to-moderate quality (n = 16, with Simplicity® catheter; n = 2, with EnligHTN™ catheter) were excluded from the analysis. Five hundred and forty-eight cross-sections with an excellent quality were drawn to calculate lumen diameters.
Figure 1.
Study flow chart.
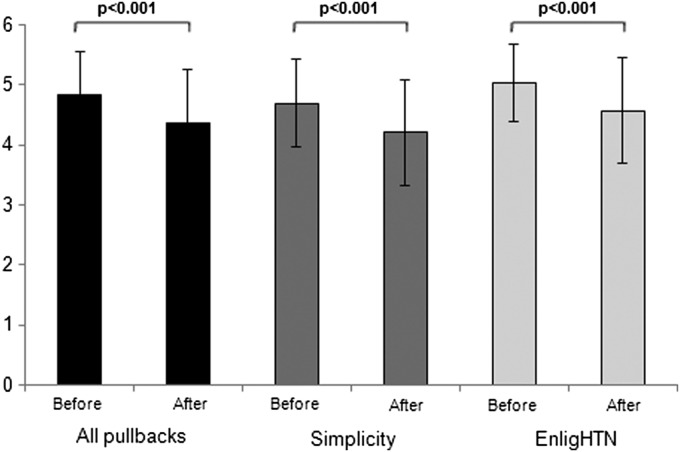
Vascular spasm
We observed vasospasm in 10 renal arteries (42%) after RNA and no vasospasm before the procedure (P < 0.001) (Table 2). Vessel spasm was encountered along the entire length of the treated artery resulting in a significant reduction of the mean renal artery diameter after the procedure. The mean renal artery diameter before and after the procedure was 4.84 ± 0.72 vs. 4.37 ± 0.89 mm (P < 0.001). The difference between the mean diameter before and after RNA was significant in both groups with the EnligHTN™ catheter (4.69 ± 0.73 vs. 4.21 ± 0.87 mm, P < 0.001) and the Simplicity® catheter (5.04 ± 0.66 vs. 4.57 ± 0.88 mm, P < 0.001) (Figures 2 and 3).
Table 2.
OCT findings before and after RNA
| Before RNA, pullbacks (n = 22) | After RNA, pullbacks (n = 24) | P value | |
|---|---|---|---|
| Oedema, n pullbacks (%) | 10 (45) | 23 (96) | <0.001 |
| Oedema in total | 14 | 72 | |
| Oedema per RA | 0.58 ± 0.83 | 3.0 ± 2.0 | <0.001 |
| Thrombus, n pullbacks (%) | 4 (18) | 16 (67) | <0.001 |
| Thrombi in total | 8 | 64 | |
| Thrombi per RA | 0.33 ± 0.87 | 2.67 ± 2.76 | <0.001 |
| Vasospasm, n pullbacks (%) | 0 | 10 (42) | <0.001 |
| Vasospasm in total | 0 | 18 | |
| Vasospasm per RA | 0 | 0.75 ± 1.07 | 0.0013 |
| Dissection/tissue disruption, n pullbacks (%) | 0 | 3 (13) | 0.086 |
| Dissection/tissue disruption in total | 0 | 5 | |
| Dissection per RA | 0 | 0.21 ± 0.59 | 0.09 |
RA, renal artery; RNA, renal nerve ablation.
Figure 2.
Changes of vessel diameter after renal nerve ablation. Significant differences of vessel diameters before and after renal nerve ablation were observed with both the EnligHTN™ (St. Jude Medical) and the Simplicity® (Medtronic) catheters. Vessel spasm was documented along the whole length of the treated artery.
Figure 3.
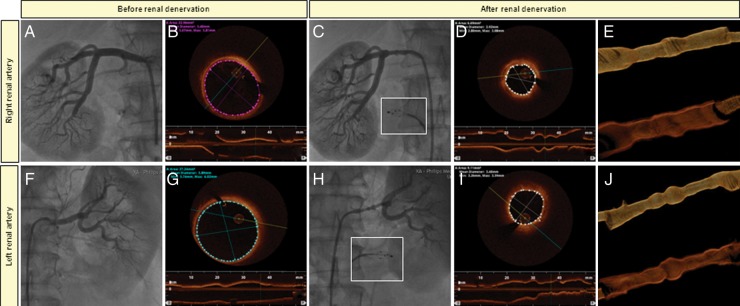
Vasospasm of renal arteries after renal nerve ablation. Right renal artery (A–E) and left renal artery (F–J). Baseline angiography (A and F) and OCT imaging (B and G) before renal artery ablation with the EnligHTN™ catheter. Vasospasm observed after radiofrequency therapy with both angiography (C and H) and OCT (D and I). Three-dimensional OCT reconstruction of right and left renal artery after renal denervation (E and J).
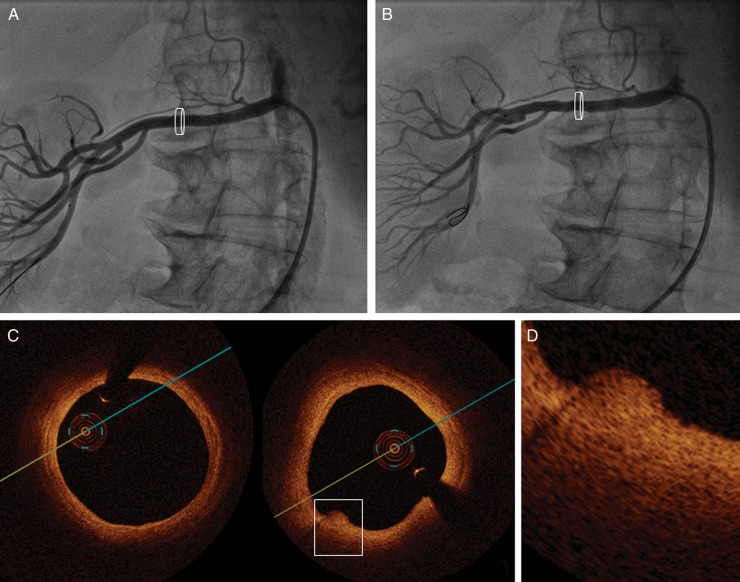
Oedema
The OCT cross-sections showed angiographically inapparent prominent vessel notches at the sites where radiofrequency-derived energy had been delivered (Figure 4). We documented the presence of endothelial–intimal oedema in all patients after renal denervation with the Simplicity® catheter (n = 15) and in 89% after using the EnligHTN™ catheter (n = 8). However, not all ablations points (4–11 per renal artery) resulted in a similar degree of notch formation as documented by OCT. We notified 72 notches in all 24 pullbacks performed after the RNA procedure. The mean amount of vessel notches before and after RNA was 0.58 ± 0.83 and 3.0 ± 2.0, respectively (P < 0.001).
Figure 4.
Vessel wall oedemas after renal nerve ablation. Renal artery before (A) and after (B) Simplicity® catheter-based renal denervation. Direct after ablation vessel notches are inapparent in angiography (B) and discernible at the lesion site by OCT imaging (C, frame and D).
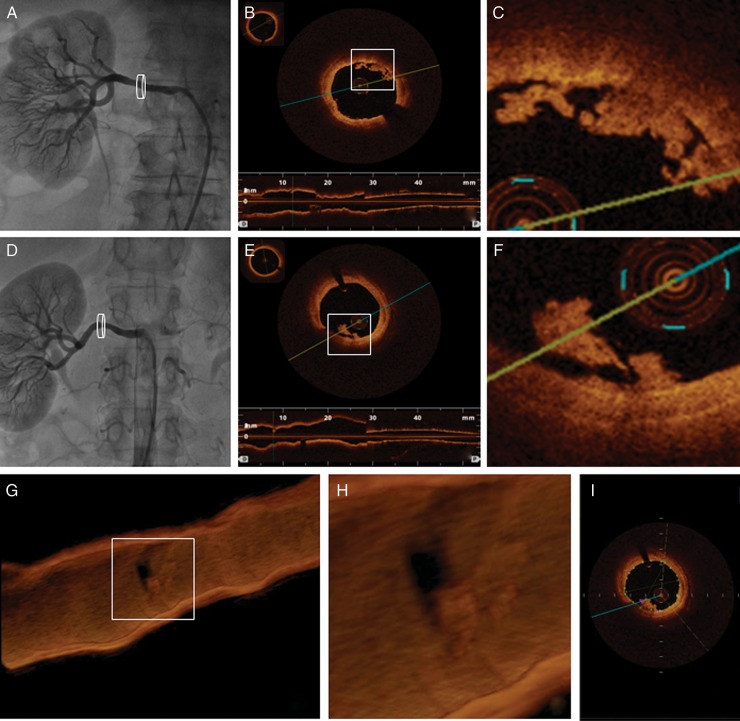
Thrombus formation
We found evidence for intraluminal thrombus formation more often after RNA than before the procedure (67 vs. 18%, P < 0.001) (Table 2, Figure 5), 64 thrombi were documented during all pullbacks after RNA and only 8 before the procedure. Also the mean amount of thrombus formations measured per renal artery was significantly higher after the procedure (2.67 ± 2.76 vs. 0.33 ± 0.87, P < 0.001).
Figure 5.
Thrombus formation after renal nerve ablation. Significant intraluminal thrombus formation after renal nerve denervation are inapparent in angiography (A and D), however displayed in different OCT cross-sections (B, C, E, F and I) and in three-dimensional reconstructed renal artery (G and H).
Dissection
We have documented five arterial dissections/disruptions after RNA in three renal arteries (Table 2, Figure 6).
Figure 6.
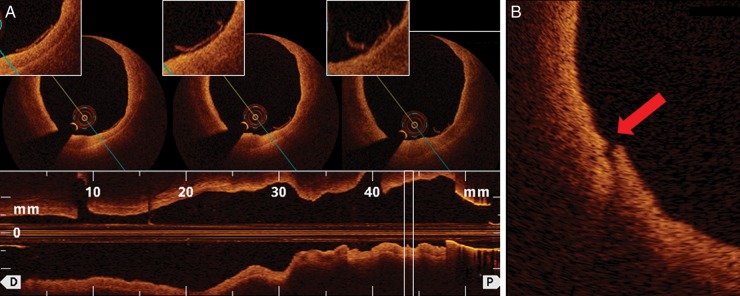
Dissections after renal nerve ablation. Endothelial detachments (A, white box) and vessel wall dissections (B, red arrow) detected in treated renal arteries with the EnligHTN™ catheter.
Comparison of two catheter-based systems used in our study: EnligHTN™ vs. Simplicity®
There was no significant difference in the amount of oedema between the Simplicity® and the EnligHTN™ catheters measured per renal artery (3.1 ± 1.9 vs. 2.3 ± 2.0, P = 0.35). We did not notified also any differences after the Simplicity® and the EnligHTN™ catheters regarding the vessel spasm (40 vs. 44%, P = 0.83). We have documented one evidence of arterial dissection after renal ablation with the Simplicity® catheter, while endothelial and intimal disruptions were observed in two patients after the EnligHTN™ catheter use (P = 0.26; Figure 6).
However, we observed a trend towards the intraluminal thrombus formation, i.e. in 89% of the cases using the EnligHTN™ catheter and in 53% with the Simplicity® catheter-based basket ablation system (P = 0.07). Moreover, a significantly greater thrombus load per renal artery was observed after RNA with the EnligHTN™ system compared with the Simplicity® system (4.6 ± 3.1 vs. 1.5 ± 1.8, P = 0.006).
Discussion
This is the first study to evaluate prospectively the morphologic features of RNA-induced renal vascular injury by OCT in patients before and after renal denervation using two different catheter systems, i.e. the Simplicity® catheter and the EnligHTN™ multi-electrode basket. While the feasibility and effectiveness in reducing blood pressure have been documented in registries and randomized trials using the Simplicity® catheter16,17 and to a lesser degree with the EnligHTN™ multi-electrode basket, little is known about the vascular injury induced by the RNA procedure at the site of ablation. We here, for the first time, demonstrate with OCT that local tissue damage not apparent with angiography occurs, i.e. local and diffuse vasospasm, oedema formation, and endothelial injury with thrombus generation.
An initial observation revealed that catheter-based RNA could be complicated by vascular lesions, i.e. vessel notches, post-procedural vasospasm, dissections, and thrombus formations. Moreover, with the EnligHTN™ multi-electrode system, more thrombus formation per renal artery occurred than with the Simplicity® catheter.
In this regard, recent animal studies are of interest demonstrating local loss of the endothelial monolayer resulting in thrombus formation even at 6 month follow-up.21,22 These observations in patients and animal models suggest that an antithrombotic therapy should be used before and after RNA, possibly for prolonged periods of time. This notion is further supported by the fact that renal artery stenosis may indeed occur after RNA, possibly evolving from such injuries.18
In contrast to Steigerwald, we have observed one dissection after RNA in our series with the Simplicity® catheter.22 In this regard, one patient of the Simplicity® HTN-1 study developed also renal artery dissection.23 Of note, the true incidence of renal artery dissection could be markedly underestimated in the Simplicity® HTN-1 study, since no intravascular imaging was performed in these patients.
Local notches, which are signs of vessel wall oedema, occurred after RNA with both catheter systems without statistically significant difference between the two. Based on histological analyses of a preclinical study, notches correspond to cellular swelling and connective tissue coagulation within the medial and adventitial layer.22 This formation of local oedema with water retention within the ablated tissue and an inflammatory response is also known from electrophysiological studies in which radiofrequency ablation is used. It is assumed that such oedemas are only present in the acute phase immediately after RNA and therefore a transient phenomenon of inflammation.21 Possibly, local oedema may reflect effective renal denervation. Obviously, whether the larger tissue damage really leads to a more effective decrease in blood pressure needs to be elucidated. Furthermore, it is unclear whether the presence of a concomitant atherosclerotic disease in renal arteries has an impact on the success of RNA on arterial blood pressure.
A three-dimensional OCT image reconstruction documented a circumscribed vascular spasm for both catheter systems leading to a ‘pearl-of-string’ feature with a significant reduction in the mean renal artery diameter as well after RNA. Obviously renal vasospasm can also result from catheter manipulation by the operator; however, the ‘pearl-of-string’ pattern (encountered along the entire length of the treated renal artery) strongly suggests that such a generalized vasospasm of treated renal arteries most likely results from the mechanical stress induced by the ablation catheter tip or basket, respectively, and/or the applied radiofrequency energy itself rather than from catheter manipulation. The mechanism of such a diffuse vasoconstriction not only at the site of ablation remains unknown, but may involve a reduced nitric oxide release after endothelial damage. However, in the experience of most operators, nitrates and calcium antagonists are not very effective in this context. Possibly, endothelin release, which leads to prolonged vasospasm, may be involved.24
Limitations
It is a limitation of this study that a rather small number of patients has yet been studied and thus these results have to be confirmed in a larger patient population. The comparison of both catheter-based systems is observational and selection bias could have occurred. However, the selection of the system was done by an independent study coordinator who was not involved in the RNA procedure, which would help to alleviate concerns of obvious selection bias. Furthermore, the maximal field of view in OCT is limited to 11 mm; therefore, patients with a large renal artery diameter are difficult to study. Moreover, imaging depth is limited to 0.5–2.0 mm with OCT. Therefore, renal arteries with thick walls cannot be properly evaluated in their entirety. The number of pullbacks excluded due to poor quality is much higher with the Simplicity system when compared with the EnligHTN system. This reflects the real-world practice for which reason we have not excluded the failed cases from our enrolment. However, the imbalance in excluded data could impair the validity of the analysis. Furthermore, no renal artery flow measurements with renal duplex-sonography before and after RNA was performed.
Conclusions
This study, for the first time, demonstrates that renal artery OCT is feasible in most patients before and after RNA and useful to depict acute vascular injury after the procedure. OCT after RNA allows for a better understanding of the local vascular injury induced by different ablation systems. Indeed, this first experience suggests that the EnligHTN™ multi-electrode basket induces a different tissue response with a higher amount of thrombus formation measured per renal artery than the Simplicity® catheter. Larger studies with short- and long-term follow-up by OCT now need to further document the type and extent of the healing response after RNA and the relation between local injury and the blood pressure response after the procedure. Based on our findings, we recommend to perform OCT routinely in patients after RNA and to effectively inhibit platelet activation with either acetylsalicylic acid or an ADP-receptor antagonist.
Funding
The institution of the authors has received educational and research grants from Medtronic, Tollachenaz, Switzerland and St. Jude Medical, Brussels, Europe.
Conflict of interest: T.F.L. has received consultant honoraria from Medtronic and St Jude Medical.
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Turnbull F, Neal B, Ninomiya T, Algert C, Arima H, Barzi F, Bulpitt C, Chalmers J, Fagard R, Gleason A, Heritier S, Li N, Perkovic V, Woodward M, MacMahon S. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 2008;336:1121–1123. doi: 10.1136/bmj.39548.738368.BE. doi:10.1136/bmj.39548.738368.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. doi:10.1016/S0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 4.Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518. doi: 10.1016/S0140-6736(08)60655-8. doi:10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 5.Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, Cifkova R, Clement D, Coca A, Dominiczak A, Erdine S, Fagard R, Farsang C, Grassi G, Haller H, Heagerty A, Kjeldsen SE, Kiowski W, Mallion JM, Manolis A, Narkiewicz K, Nilsson P, Olsen MH, Rahn KH, Redon J, Rodicio J, Ruilope L, Schmieder RE, Struijker-Boudier HA, van Zwieten PA, Viigimaa M, Zanchetti A. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens. 2009;27:2121–2158. doi: 10.1097/HJH.0b013e328333146d. doi:10.1097/HJH.0b013e328333146d. [DOI] [PubMed] [Google Scholar]
- 6.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Intern Med. 1993;153:598–615. doi: 10.1001/archinte.153.5.598. doi:10.1001/archinte.1993.00410050036006. [DOI] [PubMed] [Google Scholar]
- 7.Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. J Am Med Assoc. 1996;275:1571–1576. doi:10.1001/jama.1996.03530440051036. [PubMed] [Google Scholar]
- 8.Sytkowski PA, Kannel WB, D'Agostino RB. Changes in risk factors and the decline in mortality from cardiovascular disease. The Framingham Heart Study. N Engl J Med. 1990;322:1635–1641. doi: 10.1056/NEJM199006073222304. doi:10.1056/NEJM199006073222304. [DOI] [PubMed] [Google Scholar]
- 9.de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, Oliveras A, Ruilope LM. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57:898–902. doi: 10.1161/HYPERTENSIONAHA.110.168948. doi:10.1161/HYPERTENSIONAHA.110.168948. [DOI] [PubMed] [Google Scholar]
- 10.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–1419. doi: 10.1161/HYPERTENSIONAHA.108.189141. doi:10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 11.Prugger C, Keil U, Wellmann J, de Bacquer D, de Backer G, Ambrosio GB, Reiner Z, Gaita D, Wood D, Kotseva K, Heidrich J. Blood pressure control and knowledge of target blood pressure in coronary patients across Europe: results from the EUROASPIRE III survey. J Hypertens. 2011;29:1641–1648. doi: 10.1097/HJH.0b013e328348efa7. doi:10.1097/HJH.0b013e328348efa7. [DOI] [PubMed] [Google Scholar]
- 12.Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124:1046–1058. doi: 10.1161/CIRCULATIONAHA.111.030189. doi:10.1161/CIRCULATIONAHA.111.030189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DiBona GF, Kopp UC. Neural control of renal function. Physiol Rev. 1997;77:75–197. doi: 10.1152/physrev.1997.77.1.75. [DOI] [PubMed] [Google Scholar]
- 14.Schmieder RE, Redon J, Grassi G, Kjeldsen SE, Mancia G, Narkiewicz K, Parati G, Ruilope L, van de Borne P, Tsioufis C. ESH position paper: renal denervation—an interventional therapy of resistant hypertension. J Hypertens. 2012;30:837–841. doi: 10.1097/HJH.0b013e328352ce78. doi:10.1097/HJH.0b013e328352ce78. [DOI] [PubMed] [Google Scholar]
- 15.Schlaich MP, Sobotka PA, Krum H, Whitbourn R, Walton A, Esler MD. Renal denervation as a therapeutic approach for hypertension: novel implications for an old concept. Hypertension. 2009;54:1195–1201. doi: 10.1161/HYPERTENSIONAHA.109.138610. doi:10.1161/HYPERTENSIONAHA.109.138610. [DOI] [PubMed] [Google Scholar]
- 16.Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, Kapelak B, Walton A, Sievert H, Thambar S, Abraham WT, Esler M. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009;373:1275–1281. doi: 10.1016/S0140-6736(09)60566-3. doi:10.1016/S0140-6736(09)60566-3. [DOI] [PubMed] [Google Scholar]
- 17.Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Bohm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (the Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010;376:1903–1909. doi: 10.1016/S0140-6736(10)62039-9. doi:10.1016/S0140-6736(10)62039-9. [DOI] [PubMed] [Google Scholar]
- 18.Kaltenbach B, Id D, Franke JC, Sievert H, Hennersdorf M, Maier J, Bertog SC. Renal artery stenosis after renal sympathetic denervation. J Am Coll Cardiol. 2012;60:2694–2695. doi: 10.1016/j.jacc.2012.09.027. doi:10.1016/j.jacc.2012.09.027. [DOI] [PubMed] [Google Scholar]
- 19.Templin C, Meyer M, Muller MF, Djonov V, Hlushchuk R, Dimova I, Flueckiger S, Kronen P, Sidler M, Klein K, Nicholls F, Ghadri JR, Weber K, Paunovic D, Corti R, Hoerstrup SP, Luscher TF, Landmesser U. Coronary optical frequency domain imaging (OFDI) for in vivo evaluation of stent healing: Comparison with light and electron microscopy. Eur Heart J. 2010;31:1792–1801. doi: 10.1093/eurheartj/ehq168. doi:10.1093/eurheartj/ehq168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, Hee MR, Flotte T, Gregory K, Puliafito CA. Optical coherence tomography. Science. 1991;254:1178–1181. doi: 10.1126/science.1957169. doi:10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rippy MK, Zarins D, Barman NC, Wu A, Duncan KL, Zarins CK. Catheter-based renal sympathetic denervation: chronic preclinical evidence for renal artery safety. Clin Res Cardiol. 2011;100:1095–1101. doi: 10.1007/s00392-011-0346-8. doi:10.1007/s00392-011-0346-8. [DOI] [PubMed] [Google Scholar]
- 22.Steigerwald K, Titova A, Malle C, Kennerknecht E, Jilek C, Hausleiter J, Nahrig JM, Laugwitz KL, Joner M. Morphological assessment of renal arteries after radiofrequency catheter-based sympathetic denervation in a porcine model. J Hypertens. 2012;30:2230–2239. doi: 10.1097/HJH.0b013e32835821e5. doi:10.1097/HJH.0b013e32835821e5. [DOI] [PubMed] [Google Scholar]
- 23.Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension. 2011;57:911–917. doi: 10.1161/HYPERTENSIONAHA.110.163014. doi:10.1161/HYPERTENSIONAHA.110.163014. [DOI] [PubMed] [Google Scholar]
- 24.Yang ZH, Richard V, von Segesser L, Bauer E, Stulz P, Turina M, Luscher TF. Threshold concentrations of endothelin-1 potentiate contractions to norepinephrine and serotonin in human arteries. A new mechanism of vasospasm? Circulation. 1990;82:188–195. doi: 10.1161/01.cir.82.1.188. doi:10.1161/01.CIR.82.1.188. [DOI] [PubMed] [Google Scholar]