Abstract
Objectives
To measure the incidence of Bell's palsy and determine the impact of clinical trial findings on Bell's palsy management in the UK.
Design
Interrupted time series regression analysis and incidence measures.
Setting
General practices in the UK contributing to the Clinical Practice Research Datalink (CPRD).
Participants
Patients ≥16 years with a diagnosis of Bell's palsy between 2001 and 2012.
Interventions
(1) Publication of the 2004 Cochrane reviews of clinical trials on corticosteroids and antivirals for Bell's palsy, which made no clear recommendation on their use and (2) publication of the 2007 Scottish Bell's Palsy Study (SBPS), which made a clear recommendation that treatment with prednisolone alone improves chances for complete recovery.
Main outcome measures
Incidence of Bell's palsy per 100 000 person-years. Changes in the management of Bell's palsy with either prednisolone therapy, antiviral therapy, combination therapy (prednisolone with antiviral therapy) or untreated cases.
Results
During the 12-year period, 14 460 cases of Bell's palsy were identified with an overall incidence of 37.7/100 000 person-years. The 2004 Cochrane reviews were associated with immediate falls in prednisolone therapy (−6.3% (−11.0 to −1.6)), rising trends in combination therapy (1.1% per quarter (0.5 to 1.7)) and falling trends for untreated cases (−0.8% per quarter (−1.4 to −0.3)). SBPS was associated with immediate increases in prednisolone therapy (5.1% (0.9 to 9.3)) and rising trends in prednisolone therapy (0.7% per quarter (0.4 to 1.2)); falling trends in combination therapy (−1.7% per quarter (−2.2 to −1.3)); and rising trends for untreated cases (1.2% per quarter (0.8 to 1.6)). Despite improvements, 44% still remain untreated.
Conclusions
SBPS was clearly associated with change in management, but a significant proportion of patients failed to receive effective treatment, which cannot be fully explained. Clarity and uncertainty in clinical trial recommendations may change clinical practice. However, better ways are needed to understand and circumvent barriers in implementing clinical trial findings.
Keywords: Epidemiology, Primary Care, Clinical trials < Therapeutics
Article summary.
Article focus
What is the incidence of Bell's palsy in people aged 16 years onwards in the UK?
What has been the impact of clinical trial findings on the management of Bell's palsy?
Key messages
The incidence of Bell's palsy is 37.7/100 000 person-years, higher than previously thought.
Clinical trial findings were clearly associated with change in management.
A significant proportion of Bell's palsy cases still appear to be untreated.
Strengths and limitations of this study
This is the largest population-based study evaluating Bell's palsy incidence and management.
The dataset used is of high quality and validated for use in research.
Interrupted time series regression assesses association rather than causation.
The reasons for the high proportion of untreated cases remain largely unknown.
Introduction
The foundations of medical evidence are based on findings from clinical trials but their translation into clinical practice is an uncertain process and can be problematic.1–3 The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), which demonstrated an increased risk of cardiovascular events with doxazosin compared to chlorthalidone, was associated with modest but limited reductions in α-blocker prescribing in the USA, but there was no immediate impact in other countries.4 5 Several theoretical and practical barriers to achieve knowledge translation exist in implementation research and it has been suggested that multifaceted approaches tailored to the intervention under review are superior to passive dissemination.6 Two studies assessing the impact of implementing the UK National Institute for Clinical Excellence (NICE) guidelines reported variable results suggesting that factors including professional experience, a stable evidence base and cost implications may all influence the clinician's behaviour.7 8 Similar results from a range of clinical settings have been found in other countries.9–11
Large population-based studies measuring the incidence of Bell's palsy (acute idiopathic facial palsy) are rare. The currently published incidence rates of Bell's palsy are inconsistent, varying from as low as 11/100 000 to 51.9/100 000 person-years.12–18 A part of this variation is related to heterogeneity in the method of case detection and differences in diagnostic criteria used. In addition, not all published studies are large population-based studies and variations in sampling techniques may bias measures of disease occurrence. The incidence of Bell's palsy in the UK has been reported only once at 20.2/100 000 person-years.18 However, this measure was based on electronic health data at a time when electronic medical records (EMRs) were not as widespread or as well integrated into clinical practice as they are now. Currently, 97% of UK family doctors use EMRs.19
In 2007, the results of a large factorial randomised clinical trial examining the effectiveness of corticosteroids alone or in combination with antivirals for Bell's palsy were reported in the New England Journal of Medicine.20 The Scottish Bell's Palsy Study (SBPS) clearly demonstrated that early treatment with prednisolone significantly improved the chance of complete recovery and that treatment with aciclovir conferred no additional benefit. The clinical trial received publicity from other medical journals, evidence-based collections and the general media, raising the profile of the article and helping to disseminate its recommendations.21 22 Prior to SBPS, the recommendations on the effectiveness of corticosteroids and antivirals for Bell's palsy were unclear.23 24 In 2009, a Cochrane review of clinical trials for antivirals in Bell's palsy was published, incorporating both SBPS and data from a large Swedish clinical trial reporting similar findings.25 26 The need for high-quality research in this area was therefore demonstrated; large robust clinical trials were conducted, clear recommendations were made and the results were widely disseminated. In this regard, it would be reasonable to assume changes in clinical practice, would then follow. Use of EMRs provides a valuable opportunity to evaluate the impact of clinical trials at a population level and provide robust measures of occurrence. We decided to evaluate the impact of clinical trial data on Bell's palsy management, which has never been reported, and determine the incidence of Bell's palsy over a 12-year period.
Methods
The study was conducted using data from the Clinical Practice Research Datalink (CPRD) in the UK, formerly known as the General Practice Research Database.27 CPRD is one of the world's largest longitudinal databases containing EMRs from over 640 UK general practices. CPRD contains electronic data about patient demographics, prescriptions, clinical events, medical diagnoses, hospital referrals, admissions and deaths. Medical diagnoses and clinical events are recorded using the Read code system of classification.28 General practices are required to meet defined quality standards in order to contribute data to CPRD, which is of high quality having been validated for use in research.29 30
Study population
The study population consisted of all patients ≥16 years of age with an incident diagnosis of Bell's palsy occurring between 1 January 2001 and 30 September 2012. New Bell's palsy cases were defined by an incident Read code for Bell's palsy in patients with an up-to-standard medical history of at least 1 year before the incident Read code for Bell's palsy (F310). The incidence rates for Bell's palsy were calculated per year and for the overall study period. The numerator was the total number of new Bell's palsy cases recorded by general practitioners and the denominator was the number of person-years of total population from contributing practices. Rates per 100 000 person-years were calculated by gender directly standardised to the European standard population.
Outcome
For each new Bell's palsy case, prescription data were used to define four different treatment categories consisting of oral prednisolone therapy, oral antiviral therapy, oral prednisolone with antiviral (combined) therapy and untreated cases. Treatments were defined by prescriptions occurring within 7 days before and after the date of diagnosis. Antiviral therapy was defined by prescriptions for oral acyclovir, famciclovir or valaciclovir. The proportion of patients treated for Bell's palsy was measured per quarter stratified by treatment category. The denominator used was the total number of new Bell's palsy cases per quarter. Quarters were defined from the beginning of January 2001 (January, February and March) to the end of the third-quarter of 2012. For ease of reference, quarters are labelled 2001q1–2012q3. Referral to secondary care was determined by the presence of a referral code in the primary care records occurring within 14 days of the date of diagnosis for specialties of the ear, nose and throat (ENT), ophthalmology and neurology. Referral codes were based on the National Health Service (NHS) classification. Owing to the limited number of referrals, the proportion of Bell's palsy cases referred to secondary care was measured per year.
Events
Events were prespecified according to the publication of the 2004 Cochrane systematic reviews of clinical trials, which made no clear recommendation on the use of corticosteroids and antivirals for Bell's palsy (2004q2)23 24 and SBPS, which made clear recommendations that treatment with prednisolone alone improved chances of complete recovery (2007q3).20
Statistical analysis
Interrupted time series for the specified outcomes were plotted and the impact was examined in a single-segmented regression analysis model with parameters for the two events.31 Key parameters for each event were estimated: (1) the slope or trend in treatment before the event, (2) the step change in treatment immediately following the event and (3) the change in trend from the pre-event trend. The presence of serial autocorrelation was tested for using the Durbin-Watson statistic with visual inspection of residuals plots. The minimum number of data points between interventions was 13. Associations between untreated cases and the patient characteristics of age and gender were evaluated using multivariate binary logistic regression. Analysis was conducted using PASW Statistics V.18 (IBM Software 2009) and STATA V.11 (StataCorp, 2009).
Results
Incidence of Bell's palsy
A total of 14 460 patients with incident Bell's palsy were identified (table 1). The overall incidence of Bell's palsy for the study period was 37.7/100 000 person-years. The incidence of Bell's palsy increased with age and was similar for gender. The annual standardised incidence of Bell's palsy remained fairly constant throughout the period of study (figure 1).
Table 1.
Incidence of Bell's palsy (per 100 000 person-years) by age and gender
| Age (years) | Male |
Female |
Overall incidence | ||
|---|---|---|---|---|---|
| N (%) | Incidence* | N (%) | Incidence | ||
| 16–29 | 949 (46.2) | 24.0 | 1107 (53.8) | 30.3 | 27.0 |
| 30–39 | 1155 (49.2) | 33.6 | 1194 (50.8) | 35.6 | 34.5 |
| 40–49 | 1313 (52.2) | 34.4 | 1202 (47.8) | 32.5 | 33.4 |
| 50–59 | 1341 (52.0) | 40.0 | 1237 (48.0) | 37.6 | 38.8 |
| 60–69 | 1229 (51.0) | 45.9 | 1180 (49.0) | 42.9 | 44.4 |
| ≥70 | 1154 (45.2) | 66.6 | 1399 (54.8) | 68.2 | 67.4 |
Figure 1.
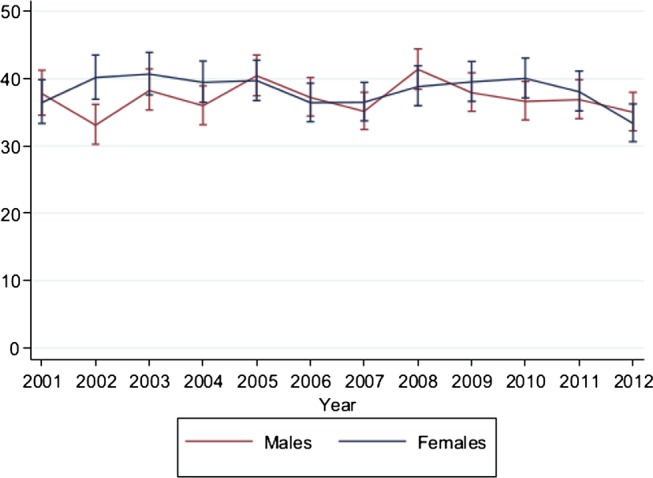
Image showing the incidence of Bell's palsy in the UK (per 100 000 person-years) from 2001 to 2012, standardised to the European standard population. Error bars, 95% CIs.
Effect of clinical trials on management
Time trends for the management of Bell's palsy are shown in figure 2. In 2001q1, Bell's palsy was treated with prednisolone only in 33.4% (95% CI 29.8 to 37.0), combined therapy in 5.1% (95% CI 1.7 to 8.5), antivirals only in 1.1% (95% CI −0.1 to 2.3) and was untreated in 60.4% (95% CI 57.1 to 63.8). The baseline trend was flat for all treatment categories, that is, there were no significant quarter-to-quarter changes in treatment (table 2). The 2004 Cochrane systematic reviews of clinical trials were associated with a significant absolute step fall in treatment with prednisolone −6.3% (95% CI −11.0 to −1.6) during 2004q2 without any significant change in trend, change from a flat to a significantly rising trend in treatment with combined therapy of 1.1% per quarter (95% CI 0.5 to 1.7) and change from a flat to a significantly falling trend in untreated patients (−0.8% per quarter (95% CI −1.4 to −0.3)).
Figure 2.
Image showing the management of Bell's palsy in the UK according to treatment. Reference line 1 shows the 2004 Cochrane systematic reviews for Bell's palsy. Reference line 2 shows the 2007 Scottish Bell's Palsy Study (SBPS).
Table 2.
Quarterly time series regression analysis of Bell's palsy treatment from 2001 to 2012
| Event | Segments* | Percentage of untreated (95% CI) | Percentage of prednisolone (95% CI) | Percentage of combination (95% CI) | Percentage of antiviral (95% CI) |
|---|---|---|---|---|---|
| Baseline | 2001q1 (intercept) | 60.43 (57.10 to 63.78) | 33.39 (29.79 to 36.99) | 5.10 (1.78 to 8.42) | 1.09 (−0.09 to 2.26) |
| 1 | 2001q1–2004q1 | −0.28 (−0.69 to 0.13) | −0.01 (−0.47 to 0.44) | 0.18 (−0.24 to 0.60) | 0.11 (−0.04 to 0.27) |
| 2004q2 step change | 2.15 (−2.15 to 6.44) | −6.32 (−11.03 to −1.60) | 3.61 (−0.74 to 7.96) | 0.57 (−1.05 to 2.18) | |
| 2004q2–2007q3 | −0.81 (−1.36 to −0.25) | −0.27 (−0.88 to 0.34) | 1.09 (0.53 to 1.65) | −0.01 (−0.22 to 0.20) | |
| 2 | 2007q4 step change | −2.13 (−5.96 to 1.70) | 5.10 (0.90 to 9.31) | −2.17 (−6.05 to 1.72) | −0.81 (−2.25 to 0.63) |
| 2007q4–20012q3 | 1.22 (0.79 to 1.64) | 0.71 (0.41 to 1.18) | −1.73 (−2.17 to −1.30) | −0.19 (−0.35 to −0.03) | |
| Final | 2012q3 | 43.98 (38.02 to 49.94) | 33.83 (28.15 to 39.51) | 18.42 (13.76 to 23.08) | 3.76 (1.47 to 6.05) |
*Trends in prescribing before and after the event including step changes. Significantly rising or falling trends underlined.
1=2004 Cochrane systematic reviews of clinical trials on corticosteroids and aciclovir or valaciclovir for Bell's palsy.3 4
2=2007 Scottish Bell's palsy study.5
Final=percentage of patients treated for Bell's palsy at the end of the study period according to the categories of treatment.
SBPS was associated with a significant immediate step rise in treatment with prednisolone only of 5.1% (95% CI 0.9 to 9.3) followed by a rising trend of 0.7% per quarter (95% CI 0.4 to 1.2), change from a rising to a falling trend in treatment with combined therapy of −1.7% per quarter (95% CI −2.2 to −1.3), change from a falling to a rising trend in untreated patients (1.2% per quarter (95% CI 0.8 to 1.6)) and change to a falling trend in treatment with antivirals alone (−0.2% per quarter (95%CI −0.4 to −0.0)).
Untreated cases
The proportion of untreated patients with Bell's palsy fell from a baseline of 60% during the 12-year study period but remained at 44% at 2012q3. The proportion of untreated patients with Bell's palsy was high across all age categories (range 44.4–58%, table 3) but was significantly greater in patients over the age of 60 years. The probability of being untreated was not significantly influenced by gender.
Table 3.
Untreated cases according to age and gender with results from multivariate logistic regression analysis
| Variable | Untreated (%) | OR (95%CI) | p Value |
|---|---|---|---|
| Age groups | |||
| 16–29 | 913 (44.4) | – | |
| 30–39 | 1105 (47.0) | 1.11 (0.99 to 1.25) | 0.077 |
| 40–49 | 1157 (46.0) | 1.07 (0.95 to 1.20) | 0.263 |
| 50–59 | 1225 (47.6) | 1.14 (1.01 to 1.28) | 0.032 |
| 60–69 | 1215 (50.4) | 1.28 (1.13 to 1.44) | <0.001 |
| >70 | 1480 (58.0) | 1.73 (1.54 to 1.94) | <0.001 |
| Gender | |||
| Male | 3459 (48.4) | – | |
| Female | 3636 (49.7) | 1.04 (0.98 to 1.11) | 0.231 |
Referrals to secondary care
Of the 14 460 new Bell's palsy cases identified, a total of 1051 (7.3%, 95% CI 6.9 to 7.7) patients were referred to ENT, ophthalmology or neurology. More treated cases of Bell's palsy were referred to secondary care than untreated cases (9.2% (95% CI 8.5 to 9.9) for treated vs 6.5% (95% CI 5.9 to 7.1) for untreated). The proportion of patients referred to secondary care fell during the study period (figure 3), ranging from 9.2% (95% CI 7.5 to 11.2) in the first quarter of 2001 to 5.9% (95% CI 4.6 to 7.6) in the third quarter of 2012 (difference 3.3%, 95% CI −0.1 to 6.6%).
Figure 3.
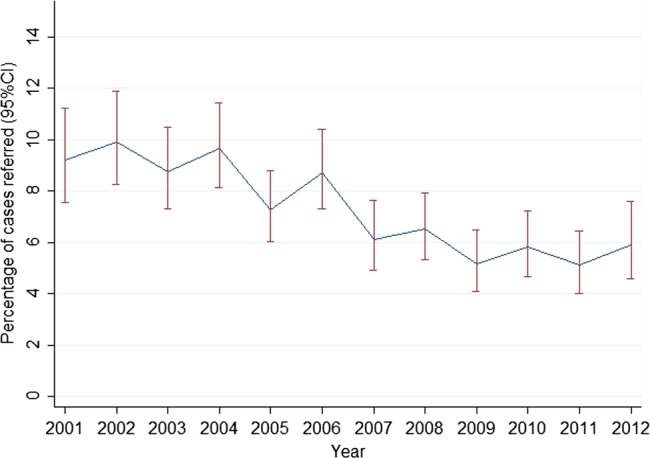
Image showing the trends in referral to secondary care for Bell's palsy in the UK from 2001 to 2012.
Discussion
Clinical trial findings are the cornerstone of medical evidence to judge the effectiveness of interventions, but not all recommendations effectively translate into clinical practice. Evaluating changes in prescribing behaviour at a population level can support clinical trials in measuring their impact.
Impact of clinical trial evidence
SBPS was associated with a significant clinical impact on Bell's palsy management by increasing treatment with corticosteroids and reducing combination therapy with antivirals based on the results of time series regression analysis. Use of prednisolone alone increased by 70% from the point immediately before publication of SBPS to the highest point in 2010. Conversely, combination therapy fell by 41% from the point immediately before publication of SBPS to the lowest point in 2010. Equally important, however, uncertainty in recommendation or lack of evidence from clinical trials also appears to significantly influence clinical practice. This is highlighted by the 2004 reviews, which were associated with an increase in combination therapy by 323% from the lowest point in 2004 to the highest point in 2007. There are several reasons why this may have occurred. Clinical uncertainties regarding effectiveness may have justified the use of antivirals with increasing pharmaceutical promotion. This would also indirectly promote corticosteroid use and help explain the falling trend in untreated patients. When no evidence for antivirals was found, promotion of combination therapy for Bell's palsy may have stopped, thus halting the falling trend in untreated patients. Corticosteroids being off-patent cheap drugs were unlikely to be marketed in the same way. Uncertainty in clinical management partly stems from uncertainty regarding aetiology. If a non-viral aetiology for Bell's palsy was confirmed, the use of antiviral therapy would be biologically implausible. Further work could usefully address the aetiology of Bell's palsy.
Adoption of clinical trial findings from SBPS clearly occurred but was limited despite clear recommendations and subsequent dissemination. In this regard, a significant number of patients are still treated with antivirals and even more appear to receive no effective treatment despite updated recommendations.26 32 In addition, there is a suggestion that the rising trend in prednisolone-only therapy and the falling trend in combination therapy over the past year of observation is plateauing, which may be an effect related to the time since publication. This may be related to the conflicting recommendations for antiviral use appearing in the literature after SBPS, especially in relation to severe cases.33–35 These uncertainties make recommendations less likely to be adopted.10 Relatively few studies have attempted to evaluate the impact of clinical trials on clinical practice. The ALLHAT trial was a large randomised double-blind trial in which the study doxazosin arm was terminated early due to an unfavourable risk of cardiovascular events compared to treatment with chlorthalidone. The ALLHAT trial was associated with a 26% reduction in annual α-blocker prescription orders, a 22% reduction in dispensed α-blocker prescriptions and a 54% reduction in physician-reported α-blocker drug use in the USA.4 Despite the clinically significant reductions, significant numbers of patients with hypertension still received treatment with α-blockade and it was proposed that further strategies are required to increase the impact that clinical trial findings should have. Our study observed similar findings in that, although a clinically significant impact occurred, clinical evidence was not fully adopted.
Untreated cases
Significant numbers of patients failed to receive effective therapy for Bell's palsy. Increasing age is associated with increasing comorbidity, which may lead to relative contraindications to therapy. Although older patients had the greatest probability of being untreated, the proportion of untreated patients was high among all age categories with 44.4% of patients under the age of 30 years appearing to not receive any effective treatment by the end of the study period. It is therefore likely that the relative contraindications to therapy as a result of comorbidities would account for only a minority of untreated cases. In older patients, the main differential diagnosis of Bell's palsy is stroke, which may have resulted in more patients receiving investigation and treatment from secondary care services. In this regard, cases may have presented to accident and emergency rather than primary care as a result of recommendations for rapid urgent assessment of suspected stroke, potentially overestimating the number of untreated patients in this age category. Conversely, concerns regarding a diagnosis of stroke may also lead to delayed diagnosis of Bell's palsy, potentially missing the opportunity for early effective treatment with prednisolone therapy in these patients.
Incidence
The incidence of Bell's palsy was similar between genders, increased with age and remained fairly constant throughout the 12-year period. The incidence of Bell's palsy varies markedly throughout the literature with differences partly relating to the method of case detection or diagnostic criteria used. Although the incidence of Bell's palsy in this study was greater than for others,14 15 17 18 a large US study using electronic health surveillance data reported a similar incidence of 42.7/100 000 person-years.16 Our study also reported similar increases in incidence with age found elsewhere.16 18
Given the low rate of referrals to ENT, ophthalmology and neurology specialties (the main specialties patients with Bell's palsy would be referred to in the UK), it suggests that primary care physicians diagnose and treat the great majority of cases. For the UK at least, primary care data are therefore a valuable source for measuring the incidence of Bell's palsy. Only one other study has reported incidence rates from the UK. Rowlands et al18 used EMRs from 1992 to 1996 to estimate an incidence of 20/100 000 person-years, a figure significantly lower than ours. It remains uncertain whether the incidence of Bell's palsy has truly increased or simply been measured more accurately. The previous study used data at a time when EMRs and established coding practices were not as widespread or as well integrated into clinical practice as they are now, which may have led to an under-recording of cases. The fairly stable trend in incidence over a 12-year period from our study also makes it less likely that the incidence of Bell's palsy has increased over time.
Strengths and limitations
This is the largest population-based study evaluating the incidence and management of Bell's palsy in adults. Bell's palsy may occur rarely in children; however, the vast majority of cases will occur in adults and increases substantially with age. Acute idiopathic facial palsy in children is more likely to be managed in secondary care, from which no prescribing data are available. As such, the inclusion of patients assessing the impact of clinical trial data would be to underestimate the impact of clinical trial findings. Perhaps of greater importance lies in demonstrating the impact of clinical trials on Bell's palsy management, which has never been reported potentially having wider implications. Cochrane systematic reviews are considered a gold standard for summaries of evidence-based healthcare in the UK and internationally, because of the rigorous approach in combining high-standard medical research. For this reason, the Cochrane systematic reviews of clinical trials were evaluated, especially as changes in recommendation occurred during the study period. In the UK, patients register with general practices in order to access free healthcare from NHS. Most prescriptions, including those recommended from secondary care, are issued electronically from general practice making UK EMRs a valuable tool for research. Bell's palsy cases were diagnosed by family physicians in real-life settings and no scale was used to quantify the degree of facial nerve dysfunction. We are unable to ascertain whether or not the diagnosis of Bell's palsy was recorded at initial presentation or following complete investigation. For this reason, we included prescriptions issued within a 7-day period before and after the date of Bell's palsy recording. Some patients may have received treatment from other sources (eg, accident and emergency units) with potential overestimation of untreated patients. However, this is likely to be a minority of patients due to the culture of healthcare provision in the UK and the size and quality of the database used. Although it would appear from the low rate of referrals to ophthalmology, ENT and neurology that Bell's palsy is primarily managed in primary care, we cannot exclude the possibility that patients were referred to other disciplines, potentially underestimating the number of referrals. Time series regression assesses association rather than causation, but remains a strong design for estimating the effects of interventions in non-randomised settings.29 Despite this, we cannot exclude the possibility that other events may have occurred which influenced the findings.
Clinical implications
A large proportion of patients do not appear to receive any effective treatment for their condition. Although the majority of Bell's palsy cases will resolve spontaneously, full recovery is more likely and quicker in those treated with prednisolone.20 36 This is important as around 30% of untreated patients will suffer long-term problems, including facial disfigurement potentially complicated by facial contracture, reduced sense of taste, speech problems, eye–mouth synkinesias, corneal ulceration and adverse psychological impact. Clearly, any treatment which reduces the risk of long-term complications and speeds up recovery should be considered. Therefore, more people should be offered early treatment with corticosteroids for Bell's palsy. More broadly, there is a societal need in healthcare research to better evaluate the impact of large clinical trials and not to assume that knowledge translation occurs naturally via passive dissemination. More work is therefore needed to understand and circumvent the barriers to adoption of clinical trial evidence. In conclusion, clinical trial findings had a clear impact on primary care management of Bell's palsy, but a significant proportion of patients failed to receive effective treatment. Clinical trials making clear recommendations could be associated with changes to clinical practice, but their impact may still be limited. Conversely, lack of evidence or uncertain clinical trial recommendations may also be associated with changes in clinical practice. Better ways are needed to circumvent the barriers to implementing clinical trial results.
Supplementary Material
Footnotes
Contributors: FMS and FD had the original idea for this study. DRM and PTD contributed to the development of the idea and the study design, and undertook the primary analysis. TVS obtained the data and contributed to the design and interpretation. DRM and FMS wrote the first draft of the manuscript. FD, PTD and TVS critically reviewed the manuscript. DRM is the guarantor. All authors approved the submitted version of the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: The role of DRM was funded by a Scottish Government sponsored Chief Scientist Office Clinical Academic Fellowship. TVS is the head of research at Clinical Practice Research Datalink (CPRD). CPRD is owned by the UK Department of Health and operates within the Medicines and Healthcare products Regulatory Agency (MHRA). CPRD has received funding from the MHRA, Wellcome Trust, Medical Research Council, National Institute for Health Research (NIHR) Health Technology Assessment programme, Innovative Medicine Initiative, UK Department of Health, Technology Strategy Board, Seventh Framework Programme European Union (EU), various universities, contract research organisations and pharmaceutical companies. The department of Pharmacoepidemiology & Pharmacotherapy, Utrecht Institute for Pharmaceutical Sciences has received unrestricted funding for pharmacoepidemiological research from GlaxoSmithKline, Novo Nordisk, the private-public funded Top Institute Pharma (http://www.tipharma.nl, includes co-funding from universities, government and industry), the Dutch Medicines Evaluation Board and the Dutch Ministry of Health.
Ethics approval: The study was approved by the Independent Scientific Advisory Committee (ISAC) for MHRA database research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Descriptive statistics for Bell's palsy cases are available from the corresponding author.
References
- 1.Shekelle PG, Kahan JP, Bernstein SJ, et al. The reproducibility of a method to identify the overuse and underuse of procedures. N Engl J Med 1998;338:1888–95 [DOI] [PubMed] [Google Scholar]
- 2.Grimshaw JM, Eccles MP, Lavis JN, et al. Knowledge translation of research findings. Implement Sci 2012;7:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003;362:1225–30 [DOI] [PubMed] [Google Scholar]
- 4.Stafford RS, Furberg CD, Finkelstein SN, et al. Impact of clinical trial results on national trends in alpha-blocker prescribing, 1996–2002. JAMA 2004;291:54–62 [DOI] [PubMed] [Google Scholar]
- 5.Maio V, Gagne JJ. Impact of ALLHAT publication on antihypertensive prescribing patterns in Regione Emilia-Romagna, Italy. J Clin Pharm Ther 2010;35:55–61 [DOI] [PubMed] [Google Scholar]
- 6.Shaw B, Cheater F, Baker R, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2005;(2003):CD005470. [DOI] [PubMed] [Google Scholar]
- 7.Wathen B, Dean T. An evaluation of the impact of NICE guidance on GP prescribing. Br J Gen Pract 2004;54:103–7 [PMC free article] [PubMed] [Google Scholar]
- 8.Sheldon TA, Cullum N, Dawson D, et al. What's the evidence that NICE guidance has been implemented? Results from a national evaluation using time series analysis, audit of patients’ notes, and interviews. BMJ 2004;329:999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Islam R, Tinmouth AT, Francis JJ, et al. A cross-country comparison of intensive care physicians’ beliefs about their transfusion behaviour: a qualitative study using the theoretical domains framework. Implement Sci 2012;7:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patey AM, Islam R, Francis JJ, et al. Anesthesiologists’ and surgeons’ perceptions about routine pre-operative testing in low-risk patients: application of the theoretical domains framework (TDF) to identify factors that influence physicians’ decisions to order pre-operative tests. Implement Sci 2012;7:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenbaum SE, Glenton C, Wiysonge CS, et al. Evidence summaries tailored to health policy-makers in low- and middle-income countries. Bull World Health Organ 2011;89:54–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Diego JI, Prim MP, Madero R, et al. Seasonal patterns of idiopathic facial paralysis: a 16-year study. Otolaryngol Head Neck Surg 1999;120:269–71 [DOI] [PubMed] [Google Scholar]
- 13.El Tallawy HN, Farghaly WM, Rageh TA, et al. Epidemiology of major neurological disorders project in Al Kharga district, New Valley, Egypt. Neuroepidemiology 2010;35:291–7 [DOI] [PubMed] [Google Scholar]
- 14.Monini S, Lazzarino AI, Iacolucci C, et al. Epidemiology of Bell's palsy in an Italian health district: incidence and case-control study. Acta Otorhinolaryngol Ital 2010;30:198. [PMC free article] [PubMed] [Google Scholar]
- 15.Morris AM, Deeks SL, Hill MD, et al. Annualized incidence and spectrum of illness from an outbreak investigation of Bell's palsy. Neuroepidemiology 2002;21:255–61 [DOI] [PubMed] [Google Scholar]
- 16.Campbell KE, Brundage JF. Effects of climate, latitude, and season on the incidence of Bell's palsy in the US armed forces, October 1997 to September 1999. Am J Epidemiol 2002;156:32–9 [DOI] [PubMed] [Google Scholar]
- 17.Bleicher JN, Hamiel S, Gengler JS, et al. A survey of facial paralysis: etiology and incidence. Ear Nose Throat J 1996;75:355–8 [PubMed] [Google Scholar]
- 18.Rowlands S, Hooper R, Hughes R, et al. The epidemiology and treatment of Bell's palsy in the UK. Eur J Neurol 2002;9:63–7 [DOI] [PubMed] [Google Scholar]
- 19.Schoen C, Osborn R, Squires D, et al. A survey of primary care doctors in ten countries shows progress in use of health information technology, less in other areas. Health Aff (Millwood) 2012;31:2805–16 [DOI] [PubMed] [Google Scholar]
- 20.Sullivan FM, Swan RC, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell's palsy. N Engl J Med 2007;357:1598–607 [DOI] [PubMed] [Google Scholar]
- 21.Madhok V, Falk G, Fahey T, et al. Prescribe prednisolone alone for Bell's palsy diagnosed within 72 hours of onset. BMJ 2009;338:b255. [DOI] [PubMed] [Google Scholar]
- 22.Haynes RB, Haynes GA. What does it take to put an ugly fact through the heart of a beautiful hypothesis? Evid Based Med 2009;14:68–9 [DOI] [PubMed] [Google Scholar]
- 23.Salinas RA, Alvarez G, Ferreira J. Corticosteroids for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2004;(2):CD001942. [DOI] [PubMed] [Google Scholar]
- 24.Allen D, Dunn L. Aciclovir or valaciclovir for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2004;(1):CD001869. [DOI] [PubMed] [Google Scholar]
- 25.Engström M, Berg T, Stjernquist-Desatnik A, et al. Prednisolone and valaciclovir in Bell's palsy: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet Neurol 2008;7:993–1000 [DOI] [PubMed] [Google Scholar]
- 26.Lockhart P, Daly F, Pitkethly M, et al. Antiviral treatment for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2009(4):CD001869. [DOI] [PubMed] [Google Scholar]
- 27.UK Department of Health Clinical Practice Research Datalink. http://www.cprd.com/home/ (accessed 22 Mar 2013).
- 28.De Lusignan S, Van Weel C. The use of routinely collected computer data for research in primary care: opportunities and challenges. Fam Pract 2006;23:253–63 [DOI] [PubMed] [Google Scholar]
- 29.Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract 2010;60:e128–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Herrett E, Thomas SL, Schoonen WM, et al. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol 2010;69:4–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299–309 [DOI] [PubMed] [Google Scholar]
- 32.Quant EC, Jeste SS, Muni RH, et al. The benefits of steroids versus steroids plus antivirals for treatment of Bell's palsy: a meta-analysis. BMJ 2009;339:b3354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salinas RA, Alvarez G, Ferreira J. WITHDRAWN: corticosteroids for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2009;(2):CD001942. [DOI] [PubMed] [Google Scholar]
- 34.Allen D, Dunn L. WITHDRAWN: aciclovir or valaciclovir for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2009;(2):CD001869. [DOI] [PubMed] [Google Scholar]
- 35.Lee HY, Byun JY, Park MS, et al. Steroid-antiviral treatment improves the recovery rate in patients with severe Bell's palsy. Am J Med 2013;126:336–41 [DOI] [PubMed] [Google Scholar]
- 36.Volk GF, Klingner C, Finkensieper M, et al. Prognostication of recovery time after acute peripheral facial palsy: a prospective cohort study. BMJ Open 2013;3:e003007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



