Abstract
Introduction
The current salt intake is very high for children as well as adults in China. A reduction in salt intake is one of the most cost-effective measures to curb the rapidly growing disease burden attributed to blood pressure and cardiovascular disease in the Chinese population. A lower salt diet starting from childhood has the potential to prevent the development of such conditions. The School-EduSalt (School-based Education Programme to Reduce Salt) study aims to determine whether an education programme targeted at school children can lower salt intake in children and their families.
Methods and analysis
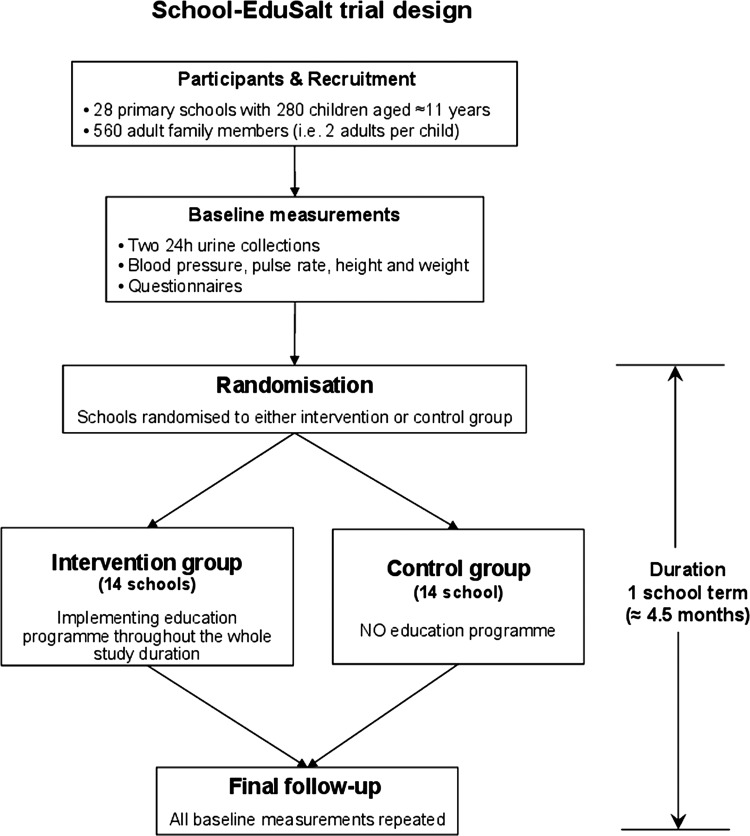
The study is designed as a cluster randomised controlled trial. The location is Changzhi, Shanxi province in northern China. The study population will consist of 28 primary schools with 280 children aged ≈11 years and 560 adult family members. Children in the intervention group will be educated on how to reduce salt intake. They will then be empowered to deliver the salt reduction message home to their families. In particular, children need to persuade the person who does the cooking to reduce the amount of salt used during food preparations. The duration of the intervention is one school term (≈4.5 months). The primary outcome is the difference between the intervention and the control group in the change in 24 h urinary sodium and the secondary outcome is the difference between the intervention and control group in the change of blood pressure. An economic evaluation will be undertaken to assess cost-effectiveness.
Ethics and dissemination
The study has been approved by The Queen Mary Research Ethics Committee (QMREC2012/81) and Peking University Health Science Centre IRB (IRB00001052-12072). Study findings will be disseminated widely through conference presentations and peer-reviewed publications.
Protocol Registration
Protocol Registered on ClinicalTrials.gov NCT01821144.
Keywords: Salt reduction, School-based education programme, Cluster randomised controlled trial
Article summary.
Article focus
This article describes the protocol of a cluster randomised controlled trial to test whether an education programme targeted at school children can lower salt intake in children and their families.
Key messages
Salt reduction is one of the most cost-effective measures to prevent cardiovascular disease (CVD). A lower salt diet starting from childhood has the potential to prevent the development of hypertension and CVD later in life. However, there is no strategy on how to keep children on a lower salt intake.
Our study aims to determine whether the school environment can act as a vehicle to lower the salt intake in children and their families.
The study will be carried out in primary schools in Changzhi, northern China, where salt intake and the prevalence of hypertension and stroke are all very high.
Strengths and limitations of this study
A unique feature of the study is to develop a new approach, that is, to use the primary school education system rather than the healthcare system to prevent hypertension and CVD. This approach reaches a wide range of the population from children to adults and could have a greater impact.
Although the study will be carried out in China, the method could be adapted by many other low-income and middle-income countries where the majority of salt in the diet is added by consumers.
Introduction
Cardiovascular disease (CVD; ie, strokes, heart attacks and heart failure) is the leading cause of death and disability worldwide. Approximately 80% of CVD deaths occur in low-income and middle-income countries (LMICs).1 Raised blood pressure (BP) is a major cause of CVD, accounting for 62% of strokes and 49% of coronary heart disease.2 Dietary salt intake is the major factor that increases BP and is largely responsible for the rise in BP with age.3 4 There is compelling evidence in adults that a modest reduction in salt intake lowers BP and reduces cardiovascular risk.4–7 Indeed, salt reduction is one of the most cost-effective measures to prevent CVD in high-income as well as LMICs.8–10
Although CVD events occur most frequently in middle- and older-age adults and the prevalence of overt hypertension is very low in children, the origins of hypertension and CVD occur in childhood.11 Accordingly, the greatest long-term potential to reduce these conditions is to initiate prevention activities in youth. Such a public health strategy aimed at preventing or slowing the progression of rising BP altogether would have enormous benefits.
Several lines of evidence from animal experiments, epidemiological studies and controlled trials demonstrate that salt intake plays an important role in regulating BP in children.12 A meta-analysis of 10 trials in individuals aged 8–16 years showed that a modest reduction in salt intake for an average duration of 4 weeks reduced BP by 1.2/1.3 mm Hg (p<0.001).12 A lower salt diet, if continued, may lessen the subsequent rise in BP with age, which would have major public health implications in terms of preventing the development of hypertension and CVD later in life. Additionally, recent studies have shown that, in children and adolescents, salt intake is a major determinant of sugar-sweetened soft drink consumption which in turn increases childhood obesity—an independent risk factor for raised BP as well as CVD.13
The current salt intake in children in most countries around the world is very high as it is in adults.14 15 However, there is no strategy on how to keep children on a lower salt intake and there is little data available to formulate the policy and engage key stakeholders. The School-EduSalt (School-based Education Programme to Reduce Salt) study aims to determine whether the school environment can act as a vehicle to lower the salt intake in children and their families. The study will be carried out in Changzhi, Shanxi province in northern China.
Why is this research needed in China?
China presents a huge opportunity to achieve major health gains from salt reduction because (1) salt intake is very high with an average intake of 14 g/day in men and 12 g/day in women as measured by 24 h urinary sodium excretion16; (2) the prevalence of hypertension and stroke, both of which are directly related to salt intake, are among the highest in the world. Approximately 177 million people had hypertension in 2002 and raised BP attributed to 2.33 million CVD deaths in 2005.17 These figures are projected to increase rapidly due to the fast economic and epidemiological transition occurring in China; (3) healthcare resources are limited. A reduction in salt intake is highly cost-effective8 18; (4) the major sources of salt in the Chinese diet are salt added by individuals during cooking and in sauces. Therefore, an important strategy to reduce population salt intake is to encourage individuals to reduce the amount of salt used during their own food preparations; (5) salt intake in children is also high. A study in 1986 indicated that salt intake in teenagers was around 10 g/day in rural China19; (6) China has a one-child policy and the ‘little emperors’, as they are often called, have a special power in the family. This provides an excellent opportunity for children to deliver the salt awareness education to and also make a significant impact on their families and (7) school children in China are in a unique position for the proposed research to be carried out because they are more disciplined, cooperative and most likely to comply with the study protocol. Research undertaken in such an environment could provide definitive evidence which would drive the widespread uptake of the intervention strategy nationally as well as internationally.
Addressing system barriers
In China and many other LMICs, health services are less developed. The healthcare system is very much oriented towards hospital-based care and treatment for individuals who already have medical conditions. Such a system has little capacity for hypertension prevention and control because (1) hypertension is a ‘silent killer’ and 75% of the Chinese hypertensive individuals are not aware that they have raised BP20 and (2) the majority of the population in China and other LMICs cannot afford life-long BP treatments. While it is important to make health services more affordable and accessible, a strategy targeted at the whole population will have a greater potential. In the School-EduSalt study, we will develop a new approach, that is, through the primary school education system rather than the healthcare system to prevent hypertension. This approach has the following advantages:
Because universal primary education is a common goal in most national education policies, the School-EduSalt approach is likely to have a greater impact compared with the ‘usual’ healthcare system, which in many LMICs focuses on treatment only.
The School-EduSalt method prevents hypertension from its root, that is, childhood. Therefore, the long-term benefits will be greater than targeting adults alone.
The School-EduSalt approach reaches a wide range of the population from children to adults. Such an approach will have an impact on hypertension prevention and control in the short as well as long term.
Salt substitution versus salt reduction
In China and many other LMICs, where the majority of dietary salt comes from salt added by consumers themselves, an important public health approach is to replace the usual salt (ie, sodium chloride) with a salt substitute (ie, low in sodium and high in potassium). Previous studies have shown that such an approach lowers BP and reduces CVD mortality.21 22 However, it has been realised that salt substitution alone is unlikely to bring the population salt intake down to the recommended level of 6 g/day. This is because only ≈30% of the sodium chloride can be replaced with potassium chloride due to the metallic and bitter taste of potassium chloride. In the China Salt Substitute Study21 which is the largest study using a salt substitute, only 25% of sodium chloride was replaced with potassium chloride. In China, salt intake is very high with an average of 12–14 g/day16; in some rural areas of northern China, salt intake can be as high as 18 g/day. In order to achieve a substantial reduction in salt intake, salt substitution as well as reduction in the amount of salt used during food preparations is required, and the latter plays a crucial role.
The School-EduSalt study is to develop a new method to reduce salt intake in children and their families. During the study, we will not provide salt substitute to the participants; however, those in the intervention group will be given the information about the salt substitute and they could purchase it themselves if they wish.
Methods of measuring salt intake
Several methods have been used in previous studies to assess dietary intake of salt in children as well as adults. These include dietary methods (ie, dietary record, dietary recall, Food Frequency Questionnaires), and urine collections (ie, spot urine, overnight urine and 24 h urine).14 15 Most of these methods are unreliable in estimating salt intake. The dietary methods are well known to underestimate the actual amount of salt consumed, particularly as they do not include the salt added during cooking or at the table. In China, the majority of salt in the diet is added by consumers during cooking or in sauces; therefore, dietary methods are of little use under such circumstances. Among the urine collection methods, 24 h urine collection is the most reliable method for estimating salt intake and overnight urine collection is not as accurate as the 24 h urine collection, due to the diurnal variation in sodium excretion. Spot urinary sodium has been shown to have a poor agreement with the 24 h urinary sodium.23 In our study, we will use 24 h urinary sodium to assess salt intake throughout the study. The baseline 24 h urinary sodium could provide valuable data on the current salt intake in children and adults.
Methods and analysis
Study hypothesis
Children's salt intake can be reduced through an education programme.
Children, if taught properly, can deliver the salt reduction message home to their families, therefore the whole family's salt intake can be reduced.
Aim and objectives
The overall aim of the School-EduSalt study was to develop an innovative, feasible, affordable and sustainable education programme for school children to reduce the dietary intake of salt for children as well as their families. This programme will ultimately prevent or slow the rising BP that accompanies aging and thereby preventing the development of hypertension and CVD. There are four specific objectives:
To develop an education programme for school children to reduce their salt intake.
To empower children to educate their family members, particularly the person who does the cooking, on reducing the amount of salt used at home.
To test whether the education programme can lower salt intake in children and their families by carrying out a cluster randomised controlled trial.
To implement the education programme nationwide by incorporating it into the national school curriculum, although subsequent funding will be sought for the widespread implementation.
Study design
The study is designed as a cluster randomised controlled trial (figure 1). A total of 28 primary schools in urban Changzhi will be recruited into the study. The reason for excluding rural schools is to avoid contamination from school meals because some children in rural schools have lunch and dinner at school due to the long distance of their home from school, whereas in urban schools most children have lunch as well as dinner at home.
Figure 1.
Summary of the School-based Education Programme to Reduce Salt trial design.
Following baseline assessments, schools will be randomised to either the intervention or control group. The salt reduction education programme will be implemented in the intervention group. The duration of the intervention is one school term (≈4.5 months).
Participants and recruitment
In primary schools in Changzhi, there are six grades in total, with age ranging from 7 to 12 years. For practical reasons, the School-EduSalt study will be carried out in grade 5 children (age ≈11 years). It is considered that younger children may not be able to deliver the salt awareness education to their families and children in grade 6 are usually very busy with their final year examinations before entering high schools.
In total, there are 36 primary schools in urban Changzhi, among which three are special Muslim schools and will be excluded. Among the remaining 33 schools, we will recruit 28 schools whose headteachers agreed to take part in the study. To recruit schools, we will first contact the local education authority (ie, Changzhi Education Bureau) to gain their opinion, support and approval. The Changzhi Education Bureau will then send a letter to the headteachers of the schools encouraging them to take part in this project. Our research team members will then contact the headteachers asking for their participation in the study.
In most schools, there are more than one class in grade 5. In such schools, one class will be selected. We will discuss with the headteacher to choose a class whose teacher in charge is willing to collaborate with the researchers. From each class, we will randomly select 10 children for evaluation. Therefore, a total of 280 children from 28 schools will be recruited into the study for evaluation. Additionally, adult family members will be invited to take part in the study. We will recruit two adult members from each child's family, for example, grandparents, parents, uncles and aunties, who live and have meals at the child's home.
Inclusion/exclusion criteria
All children in grade 5 are eligible for the study; however, children who do not have lunch or dinner at their own home or who live far from the school (>3 km) will be excluded. All adult family members who share the same meals with the child are eligible for the study. If more than two adults in one family agree to take part in the study, we will select two of them (ie, one man and one woman) in the order of grandparents, parents, uncles and aunties.
Randomisation procedures
Randomisation will be stratified by the level of schools (ie, belonging to city or district government) and the size of class. Among the schools in urban Changzhi, the size of the class varies from 13 children/class to ≈80 children/class. Usually, a larger class size indicates that the school is at the upper level of the league table in terms of examination results. Therefore, parents are more likely to send their child to such schools. Randomisation will be carried out using a computer-generated random number system by a researcher who is not involved in the study and is blind to the identity of the schools.
Intervention description
Our target is to lower salt intake by a minimum of 20% for children as well as their families. The intervention will be delivered to the whole class in spite of only 10 children being selected for evaluation. The salt reduction education includes two main components.
Classroom component: Children will be educated at 2-week intervals throughout the study. Education curriculum and materials will be developed around the following ‘key messages’: (1) harms of salt—‘More salt, less health; less salt, more health’; (2) recommended salt intake—’Less than 6 g/day’ and (3) methods of reducing salt intake—‘Add less salt in cooking and eat less pickles’. Our slogan is ‘Small hands leading big hands, together let’s reduce salt’.
Lessons will support other classroom disciplines and activities, and resources provided will be mapped to complement activities in the curriculum, in particular, health education lessons. Materials will be designed to provide a low-cost and sustainable intervention that could ultimately be used as a resource for teachers in the future. The material will consist of lesson plans, activity worksheets and homework assignments. Other teaching methods to engage students will include demonstrations, food-preparation activities, case studies and group projects. Programme materials will be developed around cartoon characters. Role plays and student presentations will be some of the activities included. Children will be encouraged to express their own ideas and initiatives on how to cut down the amount of salt. They will be invited to design their own programmes for their family. Essay competitions on salt or drawing competitions are other ways to actively involve children. Each lesson will build on what has been taught in the previous lessons to ensure that there is a clear progression in learning and understanding.
School teachers will be involved in all activities. They will coordinate all events and check students’ homework. Posters will be put up in the classroom.
Family component: Children will be empowered to persuade their family members, particularly the person who does the cooking and prepares food, to reduce the amount of salt used at home. Additionally, there needs to be a significant reduction in the amount of soy sauce and bean paste used, as well as a reduction in the consumption of pickles, salted eggs, salted peanuts, etc. Garlic, ginger and herbs will be recommended for enhancing food flavour. We will recommend replacing pickles with fresh vegetables, and replacing salted eggs and peanuts with unsalted ones. We will encourage participants to replace the usual salt with a mineral salt which is low in sodium and high in potassium. However, the important message is to reduce the total amount of salt used even with a salt substitute.
In view of the fact that the prevalence of stroke is very high in northern China and many people have witnessed the debilitating impact of a stroke on individuals and their families, our education materials will emphasise the effect of salt on stroke. For parents and grandparents, we will use their special love towards the only child in the family to persuade them to reduce the amount of salt used at home. The key message is ‘Do you know children who have high salt intake are more likely to develop hypertension and stroke when they grow up?’
To engage the family, some school activities will be organised with the family as a unit. Additionally, parents will be provided with educational materials in the form of a newsletter on a bi-weekly basis. The newsletter will cover topics such as salt and its effect on BP and CVD (particularly stroke), the major sources of salt in the diet and cooking with reduced salt. The newsletter will also have a question and answer column and a family quiz. Homework set for the students will be related to the newsletter.
Salt reduction target—minimum reduction 20%
To reduce salt intake from the current level of 12–14 g/day16 to the recommended 6 g/day, it is essential to implement a step-wise reduction in the amount of salt used, that is, 10–20% reduction and repeated at 1-year to 2-year intervals. Such reductions are not detectable by human salt taste receptors.24 In view of this, we have set a target of minimum 20% reduction which represents an important step towards achieving the overall goal and, importantly, this represents a realistic and achievable target.
Working towards 50% reduction in order to achieve the minimum 20% reduction in salt intake
From our previous experience of salt reduction trials, to ensure that a minimum of 20% reduction in salt intake can be achieved, a strategy towards a 50% reduction should be implemented. Based on the dietary data collected from northern China in the INTERMAP (INTERnational collaborative study of MAcronutrients, micronutrients and blood Pressure) study,25 we have developed a salt reduction strategy (table 1). Owing to a lack of such data in children, our strategy is based on the data in adults. However, in northern China, children's eating patterns are very similar to that of their parents and, therefore, this strategy also applies to children with a proportional reduction in all items.
Table 1.
Strategy for achieving ≈50% reduction in salt intake
| Source | Sodium* (g/day) | Salt (g/day) | Percentage contribution to total salt intake | Reduction needed (salt) |
|
|---|---|---|---|---|---|
| Reduction (%) | Reduction (g/day) | ||||
| Salt (added in cooking) | 3.614 | 9.04 | 76.4 | 50% reduction in the amount of salt used during food preparation | 4.52 |
| Soy sauce | 0.260 | 0.65 | 5.5 | 50% reduction in the amount of soy sauce used. Using garlic, herbs, ginger, 13 spices powder, vinegar | 0.33 |
| Mustard, pickles | 0.142 | 0.36 | 3.0 | 90% reduction in the amount of pickles eaten. Replacing pickles with fresh vegetables | 0.32 |
| Breads (eg, mantou) | 0.133 | 0.33 | 2.8 | No reduction | 0 |
| Noodles (homemade) | 0.131 | 0.33 | 2.8 | No reduction | 0 |
| Salted eggs, sausages | 0.049 | 0.12 | 1.0 | 100% reduction. Replacing salted eggs with unsalted eggs | 0.12 |
| Salted peanuts | 0.032 | 0.08 | 0.7 | 100% reduction. Using unsalted peanuts | 0.08 |
| Sodium bicarbonate | 0.147 | – | – | No reduction | 0 |
| Monosodium glutamate | 0.012 | – | – | No reduction | 0 |
| Others | 0.43 | 3.6 | No reduction | 0 | |
| Natural | 0.50 | 4.2 | No reduction | 0 | |
| Total | 4.733 | 11.83 | 100.0 | 45% reduction | 5.37 |
*Sources of sodium were taken from the INTERMAP study for northern China.25
From the sources of sodium reported in the INTERMAP study,25 we calculated the amount of salt (1 g sodium=2.5 g salt) and the percentage contribution of each food category to total salt intake. We then worked out the reduction needed for each food category in order to achieve a reduction of ≈50% in total salt intake (table 1). With this strategy, the total salt intake, on an average, will be reduced by 45%.
Monitoring family salt consumption
Each child will be given a salt container and a salt-control spoon (2 g salt) to take home. Parents are requested to put salt into the container provided and use salt in this container only. Parents are asked to use the salt-control spoon provided as well so that they know the approximate amount of salt used. Children will be asked to take the salt container to school every 2 weeks and the teacher will weigh it. The reduction in the weight will therefore indicate the amount of salt consumed by the household for those 2 weeks.
Children will also be asked to record whether they and their family members eat salted food weekly, including pickles, salted eggs, salted peanuts, processed meat, sauces, processed bean curd products, instant noodles, crisps or chips and salted fish or seafood.
The above data recorded along with the number of people in the household will be entered into a computer using specially designed software which will automatically give the information on how far each family’s salt consumption is different from the target level set. This information will be provided to the parents every 2 weeks in a format of a feedback letter to guide salt reduction in order to reach the target.
Control group
Children in the control schools will carry on with their usual health education lessons as in the curriculum. After the whole study is completed, participants in the control group will receive summary information on dietary salt intake and educational materials utilised in the intervention group.
Outcome evaluation
All outcome assessments will be carried out at baseline and at the end of follow-up in exactly the same way in all schools for all participants selected for evaluation, irrespective of their assignment to intervention or control group.
Two consecutive 24 h urine collections will be made for the measurement of urine volume, sodium, potassium and creatine. Participants will be carefully instructed on how to accurately collect 24 h urine by research staff. Twenty-four hour urinary creatine together with urine volume and participants’ report will be used to determine if the collection is likely to be complete. The biochemist who performs the measurements of urinary electrolytes will not be told to which group the participant is allocated.
BP and pulse rate will be measured using a validated automatic BP monitor (Omron HEM-7301-IT) with the appropriate size of the cuff. Three readings will be taken in the right arm at 2 min intervals at sitting position with arm supported at heart level, after the participant has had 10 min rest in a quiet room. The average of the last two measurements will be used for the analysis. Body weight and height will also be measured.
A brief interviewer-administered questionnaire will be completed to collect data on demographics, participants’ dietary habit such as frequency of eating out, knowledge and practices related to salt. For adults, disease history and medications will also be recorded. Additionally, a questionnaire on quality of life assessment (EQ5D)26 will be completed for all participants.
Outcomes
The primary outcome is the difference between the intervention and control group in the change in 24 h urinary sodium from baseline to the end of follow-up for children and for adults. The secondary outcome is the difference between the intervention and control group in the change of BP.
Economic evaluation
An economic evaluation will be performed to assess the cost-effectiveness of the intervention. The perspective to be adopted will be societal. Costs to be assessed will include costs in establishing and running the programme including the costs incurred by the educational authorities and teachers involved in the programme, but excluding protocol-driven costs associated with conducting research. These data will be extracted from financial statements from the project and partner organisations (eg, the education bureau and schools). Cost effectiveness will be assessed initially in terms of incremental cost per unit reduction in urinary sodium and BP, but modelled to estimate cost per life year saved and cost per Disability Adjusted Life Year averted.27 These estimates will be based on evidence from the literature of disease progression and long-term effects of salt reduction. Extensive sensitivity analyses will be carried out to estimate uncertainty about the primary findings associated with varying key parameters.
Sample size
Children
We anticipate that there will be a difference in salt intake between the intervention and control group at the end of the follow-up. A 20% difference would be considered significant from a population viewpoint. This is equivalent to a reduction in salt intake of 1 g/day from ≈5 g/day. To detect this difference with a power of 90% and α=0.05, we would require a sample size of 196 children, given an SD of 2.15 (from a pilot study, unpublished data). Taking into account the clustering (cluster size=10 and intraclass correlation coefficient=0.01) and allowing a 10% drop-out rate,19 the sample size would be 235 children from 24 schools. To ensure that the study has a sufficient power, we will recruit a total of 280 children from 28 schools (ie, 14 schools with 140 children in the intervention group and 14 schools with 140 children in the control group).
Adults
We will recruit two adult family members per child and therefore a total of 560 adults will be recruited into the study. With this sample size, we would have a power of greater than 95% and α=0.05 to detect a difference in salt intake of 2 g/day (ie, 20% reduction from 10 g/day, SD=3.528). With a sample size of 560, we would also have a power of 80% and α=0.05 to detect a difference of 2.6 mm Hg in systolic BP (SD=1028) in adults.
For children as well as adults, we will recruit equal number of male and female participants.
Data analysis
Data analyses will be performed according to the intention-to-treat approach. Statistical comparisons between intervention and control groups for 24 h urinary sodium and other continuous variables will be made using regression analysis with robust SEs accounting for clustering.
Adjusting for potential confounding factors
Our study is a school-based cluster randomised trial and schools will be randomised to either intervention or control group. For children, it is anticipated that the two groups will be comparable in baseline characteristics. For adults, however, there is a possibility for a difference between the two groups in factors that predict our secondary outcome, that is, BP. For example, age and baseline BP level have been shown to be important factors predicting the change in BP with salt reduction. If there is a difference between the intervention and control group in such factors, statistical adjustment will be made when analysing the data.
Project timelines
Recruitment of schools and participants started on 21 May 2013. Baseline assessments are underway and scheduled to complete in early July, that is, before the school examinations begin. Randomisation will take place during summer holiday in August. Intervention will start at the beginning of September when the new school term begins. Final follow-up assessments will be carried out at the end of the school term in January 2014.
Ethics and dissemination
Ethics
Written consent was obtained from all participants according to well-established practices. For children, written consent from parent/guardian as well as child was obtained. All participants were free to discontinue their participation at any time with no explanation required.
Dissemination
The findings of this study will be disseminated widely through conference presentations and peer-reviewed publications. Furthermore, the results will be disseminated worldwide through World Action on Salt and Health29 which is a global non-profit organisation of 527 members from 98 countries with the mission to improve the health of populations throughout the world by achieving a gradual reduction in salt intake.
Discussion
The School-EduSalt study offers a unique approach towards the prevention and control of hypertension. The approach of using the primary school education system rather than the healthcare system has the potential to achieve the greatest long-term benefit as it prevents hypertension from its roots (ie, starting from childhood). Although the study will be carried out in China, the method could be adapted by many other LMICs where the majority of salt in the diet is added by consumers. A modest reduction in salt intake across the whole population even by a small amount could have major beneficial effects on health along with major cost-savings.
It is important that the reduction in salt intake achieved during the trial is sustained over the years after the study. Furthermore, our ultimate aim is to incorporate the education programme into the national school curriculum which all schools will follow. A key to success for such a large-scale implementation is to monitor the progress. Repeated measurements of 24 h urinary sodium at 3-year to 4-year interval are essential to this process. Further funding will be sought for the widespread implementation and for the monitoring programme.
Supplementary Material
Acknowledgments
We acknowledge the independent supervision provided by the Trial Steering Committee (TSC) which is comprised of the independent Chairman (Peter Sever) and members (Francesco Cappuccio, Kiang Liu, Dong Zhao) and three investigators (Feng He, Yangfeng Wu and Graham MacGregor).
Footnotes
Contributors: FJH, YW and GAM conceived the project and designed the study. FJH wrote the first draft of the manuscript. JM, HW and YY designed the education materials. LLY and SJ contributed to the economic evaluation. All authors contributed to the refinement of the study protocol and approved the final manuscript.
Funding: This work was supported by Medical Research Council, UK (grant number: MR/J015903/1).
Competing interests: None.
Ethics approval: The study has been approved by The Queen Mary Research Ethics Committee (QMREC2012/81) and Peking University Health Science Centre IRB (IRB00001052-12072).
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513–18 [DOI] [PubMed] [Google Scholar]
- 2.World Health Report Reducing risks, promoting healthy life. Geneva, Switzerland: World Health Organisation, 2002. http://www.who.int/whr/2002 (accessed 3 Jun 2013) [Google Scholar]
- 3.Intersalt Cooperative Research Group Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 1988;297:319–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis 2010;52:363–82 [DOI] [PubMed] [Google Scholar]
- 5.He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta-analysis of randomised trials. BMJ 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 6.Aburto NJ, Ziolkovska A, Hooper L, et al. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He FJ, MacGregor GA. Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials. Lancet 2011;378:380–2 [DOI] [PubMed] [Google Scholar]
- 8.Asaria P, Chisholm D, Mathers C, et al. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet 2007;370:2044–53 [DOI] [PubMed] [Google Scholar]
- 9.Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010;362:590–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute for Health and Clinical Excellence (NICE) Guidance on the prevention of cardiovascular disease at the population level. http://guidance.nice.org.uk/PH25 (accessed 3 Jun 2013)
- 11.Lauer RM, Clarke WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics 1989;84:633–41 [PubMed] [Google Scholar]
- 12.He FJ, Macgregor GA. Importance of salt in determining blood pressure in children. Meta-analysis of controlled trials. Hypertension 2006;48:861–9 [DOI] [PubMed] [Google Scholar]
- 13.He FJ, Marrero NM, MacGregor GA. Salt intake is related to soft drink consumption in children and adolescents: a link to obesity? Hypertension 2008;51:629–34 [DOI] [PubMed] [Google Scholar]
- 14.Simons-Morton DG, Obarzanek E. Diet and blood pressure in children and adolescents. Pediatr Nephrol 1997;11:244–9 [DOI] [PubMed] [Google Scholar]
- 15.Brown IJ, Tzoulaki I, Candeias V, et al. Salt intakes around the world: implications for public health. Int J Epidemiol 2009;38:791–813 [DOI] [PubMed] [Google Scholar]
- 16.Zhou BF, Stamler J, Dennis B, et al. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens 2003;17:623–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He J, Gu D, Chen J, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet 2009;374:1765–72 [DOI] [PubMed] [Google Scholar]
- 18.Beaglehole R, Bonita R, Horton R, et al. Priority actions for the non-communicable disease crisis. Lancet 2011;377:1438–47 [DOI] [PubMed] [Google Scholar]
- 19.Wu Y, Cai R, Zhou B, et al. Effects of genetic factors and dietary electrolytes on blood pressure of rural secondary school students in Hanzhong. Chin Med Sci J 1991;6:148–52 [PubMed] [Google Scholar]
- 20.Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008;118:2679–86 [DOI] [PubMed] [Google Scholar]
- 21.The China Salt Substitute Study Collaborative Group Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens 2007;25:2011–18 [DOI] [PubMed] [Google Scholar]
- 22.Chang HY, Hu YW, Yue CS, et al. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr 2006;83:1289–96 [DOI] [PubMed] [Google Scholar]
- 23.Ji C, Miller MA, Cappuccio FP. Comparisons of spot v 24 h urine samples for population estimates of salt intake. J Human Hypertens 2011;25:S5 [Google Scholar]
- 24.Girgis S, Neal B, Prescott J, et al. A one-quarter reduction in the salt content of bread can be made without detection. Eur J Clin Nutr 2003;57:616–20 [DOI] [PubMed] [Google Scholar]
- 25.Anderson CA, Appel LJ, Okuda N, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc 2010;110:736–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.EQ-5D. http://www.euroqol.org/ (accessed 3 Jun 2013)
- 27.Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. Oxford: Oxford University Press, 2006 [Google Scholar]
- 28.He FJ, Marciniak M, Visagie E, et al. Effect of modest salt reduction on blood pressure, urinary albumin, and pulse wave velocity in white, black, and Asian mild hypertensives. Hypertension 2009;54:482–8 [DOI] [PubMed] [Google Scholar]
- 29.World Action on Salt and Health. http://www.worldactiononsalt.com (accessed 3 Jun 2013)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.