Abstract
Hopelessness has become an increasingly important construct in palliative care research, yet concerns exist regarding the utility of existing measures when applied to patients with a terminal illness. This article describes a series of studies focused on the exploration, development, and analysis of a measure of hopelessness specifically intended for use with terminally ill cancer patients. The 1st stage of measure development involved interviews with 13 palliative care experts and 30 terminally ill patients. Qualitative analysis of the patient interviews culminated in the development of a set of potential questionnaire items. In the 2nd study phase, we evaluated these preliminary items with a sample of 314 participants, using item response theory and classical test theory to identify optimal items and response format. These analyses generated an 8-item measure that we tested in a final study phase, using a 3rd sample (n = 228) to assess reliability and concurrent validity. These analyses demonstrated strong support for the Hopelessness Assessment in Illness Questionnaire providing greater explanatory power than existing measures of hopelessness and found little evidence that this assessment was confounded by illness-related variables (e.g., prognosis). In summary, these 3 studies suggest that this brief measure of hopelessness is particularly useful for palliative care settings. Further research is needed to assess the applicability of the measure to other populations and contexts.
Keywords: hopelessness, terminal illness, cancer, psycho-oncology, suicide
Few topics have generated as much interest in end-of-life research as the construct of hopelessness. Long considered merely a symptom of depression, hopelessness has emerged as one of the strongest predictors of end-of-life decision making regarding issues such as physician-assisted suicide and desire for hastened death, advance directives, and use or requests for life-sustaining interventions. However, attempts to understand and measure hopelessness have lagged far behind this interest, with relatively little research focused on understanding and characterizing this construct in the context of terminal illness. Levine (2007) characterized hopelessness as an embittered, dark state that can lead to feelings of emptiness and despair. Sullivan (2003) conceptualized hopelessness as a form of anticipatory grief that can arise in response to one’s own inevitable death. However, such definitions have rarely informed measure development.
Although some writers conceptualize hopelessness as the absence or loss of hope, others view the constructs of hope and hopelessness as distinct, with hopelessness representing an attachment to goals or aspirations that have been lost. Hope, on the other hand, is typically conceptualized as an optimistic outlook on the future. Hence, in the context of terminal illness, hope is often intimately intertwined with one’s prognosis, whereas hopelessness need not be. However, some scholars have criticized this distinction, arguing that hope and hopelessness are merely two opposite poles along the same continuum. For example, on the basis of a qualitative study of patients with HIV/AIDS, Kylmä, Vehviläinen-Julkunen, and Lähdevirta (2001) concluded that hope is the belief that life is worth living in the present and the future, whereas hopelessness is the absence of this belief. Kylmä et al. argued that despair represents the border between hope and hopelessness, reflecting a desire to live longer and an awareness that it is not possible.
Regardless of how hopelessness is defined, research on hope and hopelessness has frequently demonstrated a significant impact on physical and emotional well-being. Several studies, such as Everson et al.’s (1996) longitudinal study of 2,428 middle-aged Finnish men, have demonstrated that individuals with high levels of hopelessness are slower to recover from medical interventions. Everson et al. found that men with high levels of hopelessness during an initial assessment were significantly more likely to die during the follow-up period than men with low or moderate levels of hopelessness, and this effect remained significant even after controlling for biological, socioeconomic, and behavioral risk factors (e.g., depression, perceived health). Anda et al. (1993) reported similar findings based on their epidemiological study of 2,832 American adults (ages 45–77). They found that moderate-to-severe hopelessness was associated with a 1.6-fold increase in the risk of fatal ischemic heart disease, even after controlling for demographic variables and other known risk factors. A number of other studies have found similar results, with elevated hopelessness corresponding to an elevated mortality rate (e.g., Barefoot et al., 2000; Chi, 2007; Davidson, Dracup, Phillips, Daly, & Padilla, 2007; Pedersen et al., 2007).
Yet, studies of hopelessness in the context of terminal illness have frequently been limited by reliance on a measure developed and validated on physically healthy, depressed individuals (Beck, Weissman, Lester, & Trexler, 1974). This measure, the Beck Hopelessness Scale (BHS), conceptualizes hopelessness largely as the presence of negative expectancies and a generally pessimistic attitude toward the future. However, in the context of severe illness, this conceptualization of hopelessness creates considerable confusion for clinicians, researchers, and theorists, many of whom assume that the presence of a terminal prognosis is synonymous with hopelessness and that the absence of hopelessness merely reflects a lack of insight into one’s prognosis (i.e., naïve optimism). Clinicians who work in palliative care settings often readily acknowledge that many patients retain considerable hope and are able to shift to more realistic albeit often short-term goals (e.g., adequate pain management, family reconciliations, participation in important family events). Thus, it has become increasingly clear that the construct of hopelessness requires careful analysis and revision if it is to be accurately applied to the context of terminal illness.
Problems with the BHS in the context of terminal illness are not simply theoretical. A growing literature has demonstrated that the BHS is confounded by the presence of items that are either inherently true or simply incomprehensible for terminally ill individuals. For example, a patient who endorses the item “I can’t imagine what my life would be like in ten years” may be expressing a realistic understanding of his or her prognosis rather than a hopeless attitude or pessimistic outlook. In fact, patients often respond to questions such as these with puzzlement or even irritation, and such interactions may actually jeopardize rapport with study participants. Abbey, Rosenfeld, Pessin, and Breitbart (2006) found several BHS items that were endorsed by the majority of terminally ill cancer patients and/or had very low item–total correlations with the remainder of the scale. Although Abbey et al. identified several abbreviated item sets (three, seven, and 13 items) that had reliability and validity comparable with the full scale, these abbreviated scales did not improve on the predictive validity of the full BHS.
The studies described here focused on the development and validation of a scale of hopelessness that was grounded in a revised conceptualization of the construct as it applies to individuals with terminal illness. In particular, we sought to develop a measure that would optimally measure the construct of hopelessness as it pertains to terminally ill patients, in hopes of disentangling the impact of prognosis itself, while minimizing the burden on patients (who often have limited ability or interest in completing lengthy assessment batteries). Such a measure has particular importance for the assessment of desire for hastened death and suicidal ideation, constructs that have particular importance for patients with a terminal illness. We used a three-step process to achieve these goals, beginning with a series of structured interviews with palliative care experts and terminally ill cancer patients and using qualitative analysis of the patient interview data to identify important and consistent themes. The themes and that emerged during this first stage were used to develop a pool of potential items, with initial item selection guided by feedback and input from palliative care experts (who reviewed the preliminary item set), that was administered to a large sample of terminally ill cancer patients. Classical test theory and item response theory analyses (Lord, 1980) were used to derive a subset of these initial items, and the final scale was administered to a third sample to establish reliability and concurrent validity.
Study 1
Method
During the first study phase, 13 palliative care experts (nine physicians, three psychologists, and one doctoral-level nurse) were interviewed to identify critical themes that should be explored in patient interviews. We selected experts who were leading scholars in the areas of palliative care, oncology, and psychological/ psychiatric functioning at the end of life. All experts were asked a series of open-ended questions (developed by the research team) related to their perceptions of hope and hopelessness at the end of life. These questions included the following examples: “How would you define hopelessness in the context of terminal illness?” “Is there a central defining feature of hopelessness?” “Are there different elements to hopelessness? If so, what are they?”
The data generated from these expert interviews were used in two ways: First, they were used to develop a semistructured interview to be administered to 30 patients with advanced cancer. Second, they were a source of data to be integrated with patient responses. The patient interviews utilized cognitive interview techniques, such asking broad questions followed by inquiry into the thinking process that was used to answer these questions (a technique labeled verbal probing; DeMaio & Rothgeb, 1996; Willis, Royston, & Bercini, 1991). For example, patients were asked to rate their hopelessness on a scale from 0 to 10 and then were asked, “What were you thinking about when you came up with that number?” Similarly, patients were asked whether they had periods of extreme hopelessness, followed by questions such as “What was that like? What were your thoughts or feelings at that time?” All interviews (both expert and patient) were conducted by a clinical psychologist or psychology doctoral student.
Participants were recruited from two hospitals (15 from each site): a palliative care hospital for terminally ill cancer patients (Calvary Hospital [CH]) and a tertiary care cancer center (Memorial Sloan-Kettering Cancer Center [MH]). All participants were diagnosed with Stage IV cancer and had a life expectancy of less than one year, although participants recruited from the palliative care hospital typically had a life expectancy of less than 6 weeks, whereas those recruited from the cancer center typically had a life expectancy of 3 to 12 months. Prospective patients (N = 33; a 91% participation rate) were approached by study research assistants, either in their hospital room (for CH participants) or while waiting for an outpatient clinic appointment at an ambulatory care clinic (for MH participants). Participants were informed about the nature of the study and the risks and benefits of participation, and they provided written informed consent. Following informed consent, we interviewed participants with a structured interview that we developed (based on information provided by the expert participants), asking questions about participants’ current health status, their thoughts and goals for the future, and their emotional and spiritual well-being and overall quality of life. Interviews were audiotaped and transcribed for review by the research team.
The sample was equally divided across gender, with 16 (53%) women and 14 (47%) men. The majority were Caucasian (80%, n = 24), and 20% (n = 6) were Black; 86.7% (n = 26) were non-Hispanic, and 13% (n = 4) were Hispanic. Religious affiliation was also diverse, with 11 participants (36.7%) describing themselves as Catholic, 11 (36.7%) describing themselves as Jewish, seven describing themselves as other Christian faiths (23.3%), and one (3.3%) reporting no religious affiliation. The average age was 60.4 years (range = 30 to 80), and the average education level was 15.2 years (range = 9 to 17). All of the participants met criteria for advanced cancer (Stage IV disease) and included a variety of primary diagnoses (lung = 20.0%, n = 6; pancreatic = 16.7%, n = 5; ovarian = 13.3%, n = 4; prostate = 13.3%, n = 4; breast = 10.0%, n = 3; other cancer diagnoses = 23.3%, n = 8). Five participants (16.7%) were still alive at the conclusion of the study.
Transcribed interviews were analyzed with a two-stage open-coding process in which trained raters (clinical psychologists and psychology doctoral students) first identified critical passages and phrases used by the participants to describe their perceptions of and outlook for the future. This approach utilized a thematic content analysis framework (Walker & Avant, 2005) for data reduction, in which raters independently reviewed the transcripts to identify passages that conveyed unique aspects of hopes and aspirations as well as areas in which hope had been diminished or lost. In the second phase of coding, the core themes identified in the thematic content analysis were organized by each of the raters independently into a number of different categories that reflected the various aspects of hope and hopelessness articulated by the study participants. The data generated from this second phase of coding were discussed by the research team members, who made revisions and adjustments to the categories as well as to the elements contained within each category. This process continued until a consensus was reached on the different themes elicited, each of which was accompanied by patient-based descriptions or quotations.
Results
The single largest category of patient expressions pertained to goals and plans for the future or, in many instances, to the absence of such aspirations. Not surprisingly, hopes for the future were often short term or open ended and were framed in both positive (“There are still things I want to do” and “I enjoy making plans and having something to look forward to”) as well as negative terms (“I have stopped making any future plans” and “I have nothing to look forward to”). A subset of these responses targeted hopes specific to the illness and/or dying, with statements such as “I hope to be remembered after I’m gone” or “I hope my family won’t suffer” or, conversely, “I fear my suffering will never end.”
A second category of responses, more often directed at feelings of hopelessness rather than hope, conveyed a sense of futility or having given up on life. For example, items such as “There is no point in going on” or “I feel powerless over my life” reveal a sense of frustration with one’s inability to improve one’s situation and, in a subset of cases, revealed a cognitive rigidity that seemed to hinder patients in their attempts to improve their situation. A related theme of control also emerged but was distinguished from futility as being more cognitive in nature (vs. the affective tone of futility/giving up statements). For example, statements such as “There is nothing I can do to improve my situation” or “I can’t make anything good happen” were linked with statements such as “I feel a sense of control over my future.” A fourth category of responses revealed a will to live that was articulated in statements such as “I am still fighting to live” or, conversely, “I do not have the strength to go on.”
Many patients also expressed a more existential sense of futility, with statements such as “Life means nothing” or “My life has no value,” whereas other patients responded with precisely the opposite sentiment (“Despite my illness, my life is still important”). A sixth category of responses was predominantly affective in nature, with statements such as “I am demoralized,” “I dread every day,” and “Life is weighing heavily on me.” A more positive sentiment, also articulated by many patients, was one of acceptance (e.g., “I feel ready for whatever happens next”). Not surprisingly, patients anchored some of their statements to prognosis, either for the illness in general or for symptom management more specifically. For example, statements such as “I have lost confidence that the doctors can help me in any way” or, conversely, “Regardless of what the experts say, I still believe there is hope” communicate a sense of hope—or its absence—centered around treatment. Finally, a number of patients articulated a pervasive sense of optimism or pessimism that, although anchored to their current situation, appeared to reflect a more long-standing cognitive style (e.g., “in spite of my illness, I still have a positive outlook on life”), whereas other patients described changes in their cognitive style (e.g., “I used to be an optimistic person, but now that has changed”).
Summary
Terminally ill cancer patients described a wide range of hopes, fears, and concerns related to their illness, their families, and themselves. This diverse set of topics, elicited in response to structured interview questions regarding hope and hopelessness, demonstrates the range of issues encompassed by the construct of hopelessness at the end of life. Although some of the elements of hopelessness elicited through these qualitative analyses appeared to overlap with existing constructs (e.g., demoralization, desire for hastened death, depression), others appeared to be unique (e.g., short-term hopes and goals, the sense of futility that may accompany severe illness and dying). These findings suggest a number of aspects of hopelessness that should be assessed in a measure designed specifically for the context of terminal illness (in this case, cancer), although the centrality and relevance of each aspect clearly require further investigation and, thus, was addressed in our second study phase.
Study 2
Method
For Study 2, we recruited 328 patients from the same two study sites (CH and MH), using a sequential recruitment strategy in which all eligible patients were approached (N = 512; a 64% participation rate) and, if cognitively intact, were offered study participation. As in Study 1 (the qualitative phase), participants were recruited if they were diagnosed with Stage IV cancer, had a life expectancy of less than one year, and spoke English fluently. Participants were approached by a research assistant and informed about the nature of the study and the risks and benefits of participation. Participants then provided written informed consent. Following informed consent, participants were asked to complete a self-report inventory regarding hope and hopelessness developed on the basis of the first study phase (described later). Because many patients had significant fatigue and visual impairments (particularly among the more severely ill sample at CH), the items were read aloud to many participants rather than having them complete the measure independently.
Roughly half of the second sample was recruited from the inpatient palliative care hospital (CH, 45.7%, n = 150) with the remainder from the tertiary care cancer hospital (MH, 55.4%, n = 178); 14 participants withdrew from the study prior to completion and are not described later. The final sample included equal proportions of men (48.4%, n = 152) and women (51.5%, n = 162), with an average age of 61.0 years (SD = 13.8, range = 22 to 94). The majority were Caucasian (72.9%, n = 226), with 21.9% Black (n = 68) and 5.2% (n = 16) of other or mixed racial backgrounds (these data were missing for four participants); 11.9% (n = 37) were Hispanic, and 88.1% (n = 273) were non-Hispanic. Religious affiliation was also diverse, with 136 participants (44.0%) identifying as Catholic, 61 (19.7%) as Jewish, 54 as other Christian faiths (17.5%), 46 (14.9%) as other religions, and 12 (3.9%) as having no religious affiliation. Participants completed an average of 14.7 years of education (range = 2 to 23). All of the participants met criteria for advanced cancer (Stage IV disease) and included a variety of primary diagnoses (colon = 20.1%, n = 63; lung = 19.4%, n = 61; pancreatic = 11.8%, n = 37; breast = 7.0%, n = 22; sarcoma = 6.4%, n = 20; all other diagnoses accounted for less than 5% of the sample).
Instrument Development and Evaluation
Converting patient statements and expressions regarding hopelessness involved first identifying the optimal set of phrases, statements, and constructs to tap the range of dimensions identified in Study 1. The themes and quotations identified in the thematic content analysis (described earlier) were provided to the palliative experts, who were asked to identify those statements and constructs they believed best captured the construct of hopelessness in the context of terminal cancer. Those statements perceived by the team of palliative care experts as most useful were converted into a series of candidate items, either directly (e.g., retaining the statement in its entirety but associating a response format: true/ false or Likert type) or by generating alternative versions of the statement to reflect gradations of severity (for the anchored hierarchical statements).
We developed scale items with four different response formats: dichotomous choice (true/false), Likert-type items based on both frequency (never, rarely, sometimes, and often) and strength of agreement (strongly disagree, somewhat disagree, neutral, somewhat agree, and strongly agree), and anchored hierarchical statements (i.e., “I can put my illness out of my mind most of the time,” “Sometimes I can think about things other than my illness,” and “It is hard to think about anything besides my illness”). Finally, the potential scale items were reviewed by several of the palliative care experts, who helped refine content and improve item clarity. The resulting list of 30 items was initially pilot tested on several terminally ill cancer patients, many of whom complained that the measure was too long and repetitive and identified further wording issues and confusing questions. Following this initial feedback, the item pool was further trimmed to a set of 20 items, including 7 true/false items, 5 frequency items, 4 strength-of-agreement items, and 4 sets of anchored hierarchical statements.
The 20-item draft measure was administered to the study sample to generate preliminary data regarding item endorsement patterns as well as to identify items with stronger versus weaker psychometric properties, as described later. In addition, a secondary set of analyses focused on determining the optimal number of response options and response format to be used in the final version of the questionnaire. Data analysis included descriptive statistics regarding item endorsement as well as analyses grounded in both classical test theory (e.g., scale distribution, item-total correlations, coefficient alpha, and factor analysis) and item response theory (e.g., item information functioning, discrimination power, and differential item functioning). Because item response theory indices (e.g., slopes) are impacted by the number of item choices, we conducted these analyses using a series of steps in which the number of item response options was gradually reduced. In the first set of analyses, the items were analyzed with all possible response options (including items of the same response format in the same block), whereas in subsequent iterations, the Likert-type items were collapsed (i.e., strongly and somewhat agree were collapsed into a single response for items in which agreement reflected hopelessness; for items coded in the reverse manner, strongly disagree and disagree were collapsed), resulting in four levels for these items rather than five. This process was repeated twice more, first by collapsing both ends of the strength of agreement items, leaving disagree, neutral, and agree, as well as by collapsing often and sometimes, forming items with a maximum of three response options. Finally, all variables were collapsed into dichotomous variables in which the response choices reflected either no evidence/endorsement of hopelessness versus some evidence/endorsement (i.e., the neutral and the disagree items were collapsed together as were rarely, sometimes, and often, and the anchored statements reflecting no evidence of hopelessness were contrasted with those that reflected some evidence of hopelessness). The comparison of items within their original scaling helped identify stronger versus weaker items within each set of items, whereas by analyzing item information functions across these different iterations, the relative benefits of including more response options, as well as the relative utility of items using different response formats could be investigated.
Results
On the basis of the classical test theory and item response theory analyses, a number of items stood apart as having the strongest psychometric properties and were identified as potential candidates for the final scale. In general, the selected items were those that were relatively infrequently endorsed (Table 1) but not so rarely endorsed as to have unacceptably low item–total correlations (Table 1) or relatively poorer item characteristics (Table 2). Not surprisingly, there was considerable overlap between the items identified by the classical test theory and the item response theory analyses, with the same items emerging in both sets of analyses as the strongest (within their respective cohort of items using the same response scale).
Table 1.
Descriptive Statistics for the Original 20 Items
| Item | M | SD | Item total r |
|---|---|---|---|
| Four-level frequency items (scored 0–3) | |||
| 1 | 0.99 | 0.93 | .22 |
| 2 | 1.19 | 1.09 | .43 |
| 3 | 0.45 | 0.67 | .37 |
| 4 | 0.81 | 0.84 | .55 |
| 5 | 0.49 | 0.73 | .39 |
| Two-level true/false items (scored 0–1) | |||
| 6 | 0.12 | 0.32 | .38 |
| 7 | 0.14 | 0.35 | .29 |
| 8 | 0.12 | 0.33 | .43 |
| 9 | 0.11 | 0.31 | .34 |
| 10 | 0.26 | 0.44 | .47 |
| 11 | 0.03 | 0.17 | .23 |
| 12 | 0.19 | 0.39 | .46 |
| Five-level agreement items (scored 0–4) | |||
| 13 | 0.48 | 1.03 | .33 |
| 14 | 1.12 | 1.41 | .50 |
| 15 | 0.59 | 1.08 | .56 |
| 16 | 0.55 | 1.04 | .55 |
| Three-level anchored items (scored 0–2) | |||
| 17 | 0.41 | 0.58 | .53 |
| 18 | 0.81 | 0.61 | .49 |
| 19 | 0.60 | 0.64 | .43 |
| 20 | 0.56 | 0.62 | .59 |
Note. Italicized items were retained in the final sale. Some variables are reverse coded so higher scores reflect greater hopelessness for all items.
Table 2.
Item Response Theory Analyses of the Original 20-Item Scale
| Initial estimates |
Modified estimates |
|||||
|---|---|---|---|---|---|---|
| Item | Slope | Location | r | Slope | Location | r |
| Four-level frequency items | ||||||
| 1 | 0.17 | 1.83 | .38 | 0.22 | 0.31 | .42 |
| 2 | 0.27 | 0.68 | .59 | 0.33 | −0.17 | .59 |
| 3 | 0.44 | 2.21 | .55 | 0.48 | 1.58 | .54 |
| 4 | 0.75 | 1.07 | .71 | 0.92 | 0.48 | .70 |
| 5 | 0.41 | 2.27 | .59 | 0.51 | 1.46 | .60 |
| Two-level true/false items | ||||||
| 6 | 0.92 | 1.58 | .65 | 0.62 | 2.19 | .61 |
| 7 | 0.65 | 1.82 | .56 | 0.45 | 2.46 | .51 |
| 8 | 1.04 | 1.59 | .75 | 0.93 | 1.65 | .73 |
| 9 | 0.67 | 2.25 | .58 | 0.70 | 2.09 | .59 |
| 10 | 0.78 | 1.12 | .64 | 0.85 | 0.97 | .68 |
| 11 | 0.57 | 3.73 | .62 | 0.65 | 3.56 | .61 |
| 12 | 0.95 | 1.33 | .72 | 1.04 | 1.15 | .72 |
| Five-level agreement items | ||||||
| 13 | 0.22 | 2.84 | .57 | 0.11 | 8.85 | .44 |
| 14 | 0.27 | 1.30 | .70 | 0.14 | 3.46 | .66 |
| 15 | 0.46 | 1.59 | .85 | 0.43 | 2.59 | .84 |
| 16 | 0.36 | 2.02 | .81 | 0.32 | 3.65 | .74 |
| Three-level anchored items | ||||||
| 17 | 0.75 | 1.62 | .73 | 0.79 | 1.42 | .72 |
| 18 | 0.89 | 0.63 | .57 | 0.91 | 0.48 | .59 |
| 19 | 0.60 | 1.29 | .56 | 0.70 | 1.06 | .62 |
| 20 | 0.96 | 1.20 | .76 | 1.32 | 0.93 | .79 |
Note. Modified estimates reflect three-level variables for Items 1–5 and 13–20, two-level variables for Items 6–12; r corresponds to polyserial correlation. Italicized items were retained in the final scale.
Table 2 displays the results of the initial item response theory analyses based on a generalized partial credit model (using Parscale; Muraki & Bock, Version 4), broken down by item response format. Of note, we initially sought to apply a graded response model, but Parscale was not able to fit this model to these data. Moreover, the graded response and partial credit models generate highly similar results in terms of item response functions and estimated trait values, although the item parameters have very different meanings (Embretson & Reise, 2000). As is evident from the initial parameter estimates, which included each item in its original format, there was substantial variation in the slopes (discriminatory power) of the items. Because these estimates are impacted by the number of response options, comparisons are meaningful only within items of similar response format, limiting comparisons of the initial estimates across the different item sets. Although this process was conducted four times as described earlier (once using the original format for each item, a second time with a maximum of four alternatives, a third time collapsing the Likert-type items into three levels each, and a fourth time by collapsing all items into a yes/no response), only two sets of analyses are presented. The first analysis used each item in the response format originally developed, and the second analysis collapsed the frequency and strength-of-agreement items into three levels (which was ultimately deemed the optimal response format, as described later).
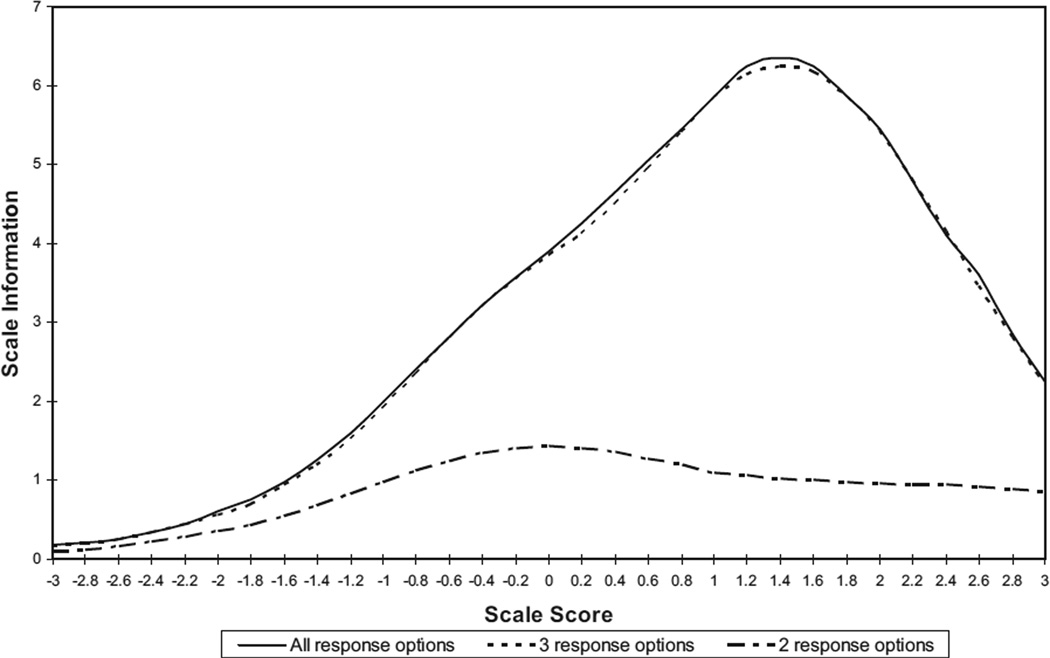
Once a tentative set of final items was identified, a second level of analyses focused on identifying the optimal number of response alternatives and response format for the final questionnaire (because integrating multiple questionnaire formats into a single scale might be confusing to participants and challenging for scoring and analysis). To determine the optimal response format and scaling, we used each of the four response formats described earlier to analyze the final eight-item scale. As is evident from Figure 1, there was virtually no loss of scale information by reducing the Likert-type items to three response levels (maximum scale information = 6.24 vs. 6.23), but when all items were reduced to a dichotomous choice, the drop in scale information was dramatic (maximum scale information = 1.41). These parameters, which are a function of the standard error of measurement of the underlying latent variable (see, generally, Lord & Novick, 1968), indicate substantially greater measurement precision for the original scoring and the three-alternative version of the scale compared with the version treating all items as dichotomous. Specifically, a maximum scale information value of 6.24 corresponds, roughly, to a minimum standard error of measurement of .40 (on the basis of a scale with a mean of 0 and standard deviation of 1), whereas a maximum scale information value of 1.41 corresponds to a minimum standard error of measurement of approximately .80. Thus, these findings suggest that three is the optimal number of response options and that little gain is evident from increasing the number of response options.
Figure 1.
Item information for the eight-item scale comparing two-response, three-response, and all response categories.
We also utilized an exploratory factor analysis (using a principal axis extraction) to evaluate the factor structure of the preliminary eight-item scale (based on the modified items with three response categories). An analysis of eigenvalues and the scree plot indicated that a one-factor model provided the best fit, accounting for 41.3% of the variance in item intercorrelations (eigenvalue = 4,330). Seven of the eight items had loadings of .5 or greater onto this factor (the remaining item loading was .48). The eigenvalue for a second factor was only 0.85, despite accounting for an additional 10.6% of the variance.
The decision regarding which question format to utilize (Likert-type frequency, strength-of-agreement items, or anchored statements) was somewhat more subjective than the selection of items or number of response categories, incorporating the observations of the research team and patient feedback into the analyses reported earlier. First, we observed that nearly half of the final scale items were drawn from the anchored statement format (which reflected all but one of the items generated using this format) and that the Likert-type items performed relatively poorly. Although this result might reflect the item content, it also appeared, to the research team, to reflect a greater ability of participants to understand and respond to the anchored question format. Indeed, patients often commented on the difficulties associated with both the multilevel Likert-type items as well as the overly restrictive response range for the dichotomous choice items. Study research assistants also noted a greater ease of comprehension of the anchored statements, as participants seemed better able to determine which option sounded best when hearing or reading the actual statement (perhaps because of the mild cognitive impairment that is common among terminally ill cancer patients). Given these observations, items that had been developed in a different response format (dichotomous, frequency, strength of agreement) were converted into the anchored statement format for the final stage of scale validation.
Finally, all of these analyses were repeated for each of the two subsamples (inpatient palliative care patients at CH and those receiving active treatment at a MH) to assess differential item functioning across levels of illness severity. These analyses revealed a virtually identical pattern of results across the two sub-samples, indicating that the optimal items and scale structure were not dependent on proximity to death (results are not presented here but are available on request).
Summary
Although explicit decision rules do not exist for combining scale development results based on classical test theory and item response theory, these analyses generated largely complementary results, identifying a subset of scale items that appeared superior to the remainder of the prospective items that were pilot tested. Perhaps surprisingly, of the four different scaling and response formats utilized in the pilot items, the three-choice anchored items appeared to be superior to dichotomous items and Likert-type items with more response options (whether frequency or strength of agreement). This may reflect the unique needs and characteristics of a terminally ill population, as anchored items are likely to require less cognitive effort or abstraction, and may therefore be easier for terminally ill patients to understand and respond to. Dichotomous items, on the other hand, although less complex, were often perceived as too black and white, failing to capture the nuances of the items and leaving no room for a neutral or ambivalent response. On the basis of these findings and observations, the anchored three-item format was utilized for the final version of the scale.
Study 3
Method
The third and final phase of scale development utilized a recruitment approach similar to the one used in Study 2, with another 255 end-stage cancer patients recruited from the same two study sites (CH and MH), representing 33.0% of patients who were approached (N = 772) and 41.0% of those who met the inclusion/ exclusion criteria described later (N = 622). As in the previous studies, participants were recruited if they were diagnosed with Stage IV cancer, had a life expectancy of less than one year, and spoke English fluently. Prospective participants were approached by a research assistant and informed about the nature of the study and the risks and benefits of participation. If willing, they provided written informed consent. Following informed consent, participants completed a series of self-report measures, although the questionnaires were read aloud to some participants who had excessive fatigue and visual impairments. The study measures administered included the eight-item Hopelessness Assessment in Illness (HAI), developed by the investigators and described earlier, as well as two additional measures of hopelessness, the BHS (Beck et al., 1974; analyzed as both a full scale and as the seven-item abbreviated scale developed by Abbey et al., 2006) and a clinical rating of hopelessness (CRH) using a 0 to 6 rating scale (based on Wilson et al.’s, 2004, brief structured interview). Additional measures administered included the depression module of the Structured Clinical Interview for DSM–IV (First, Spitzer, Gibbon, & Williams, 2001), the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983), the Functional Assessment of Cancer Therapy Spiritual Well-Being scale (Brady, Peterman, Fitchett, Mo, & Cella, 1999), the Life Orientation Test–Revised (Scheier, Carver, & Bridges, 1994), the Schedule of Attitudes Toward Hastened Death (SAHD; Rosenfeld et al., 1999), and the Duke–University of North Carolina Functional Social Support Questionnaire (FSSQ; Broadhead, Gehlbach, De Gruy, & Kaplan, 1988). A measure of prognostic awareness (PA; Chochinov, Tataryn, Wilson, Enns, & Lander, 2000) was added to the assessment battery after the first several months of data collection and was available for approximately two thirds of the sample. We anticipated that the HAI would be significantly correlated with all of these measures but that stronger correlations would be observed for other measures of hopelessness or psychological distress (e.g., the BHS, HADS, SAHD) than for measures of illness severity or social support (e.g., the FSSQ). We also anticipated somewhat weaker correlations between the HAI and measures of depression (e.g., HADS) or prognostic awareness (PA) compared with those observed for the BHS. Because a number of participants were too ill to complete testing (N = 27), the analyses reported here reflect only those participants who completed the HAI and at least some of the additional study measures (N = 228).
Just over half of the participants were recruited from the inpatient palliative care hospital (CH, 56.6%, n = 129), and the remainder were from the tertiary care cancer hospital (MH, 43.4%, n = 99). The sample included 104 men (45.6%) and 124 women (54.4%), with an average age of 62.9 years (SD = 13.0, range = 28 to 96). The majority were Caucasian (77.6%, n = 177), with 17.1% Black (n = 39) and 5.3% (n = 12) of other or mixed racial backgrounds; 11.0% (n = 25) were Hispanic, and 89.0% (n = 202) were non-Hispanic. The most common religious affiliations included Catholic (n = 94, 41.2%), Jewish (n = 46, 20.2%), and Protestant (n = 45, 19.8%), with 25 (11.0%) identifying as belonging to other religions, and 16 (7.0%) reporting no religious affiliation (religious affiliation was missing for two participants). Participants reported an average of 14.5 years of education (SD = 3.1, range = 5 to 24).
All of the participants met criteria for advanced cancer (Stage IV) and included a variety of primary diagnoses (lung = 15.8%, n = 36; pancreatic = 14.0%, n = 32; colon = 11.4%, n = 26; breast = 11.0%, n = 25; liver = 6.1%, n = 14; all other diagnoses accounted for less than 5% of the sample). When asked about their health, the majority were rated as having full awareness of their prognosis (n = 86, 53.1%), whereas 51 individuals (31.5%) were classified as having partial awareness, and 25 (15.4%) had no awareness of their terminal prognosis (these data were missing for 66 participants). Likewise, nearly half of the sample (n = 68, 44.4%) acknowledged that their illness was terminal, whereas 45 participants (29.4%) characterized their illness as incurable but not terminal, 36 participants (23.5%) believed their illness was curable, and 4 (2.6%) did not believe their illness was serious.
Results
Mean scores on the HAI, an eight-item hopelessness inventory (see the Appendix), were 4.32 (SD = 3.5), with a range of 0 to 15 (possible range = 0 to 16). HAI scores approximated a normal distribution (skew = 0.80, kurtosis = 0.70), despite 29 individuals (12.7%) obtaining the lowest possible score (0) on this measure. Coefficient alpha for the eight-item scale was .87, and each of the items had an item–total correlation exceeding .54; interitem correlations ranged from .269 to .638 with a mean of .48. None of the items resulted in an increased alpha coefficient if removed. However, a confirmatory factor analysis provided equivocal support for the one-factor model identified in the previous study. Although each of the eight items loaded significantly onto the latent factor, with standardized loadings between .60 and .78, the model generated a comparative fit index of .92 and a root-mean-square error of approximation index .12, both of which were somewhat poorer than anticipated. Examination of the residuals revealed large correlations between Item 7 and Items 2 and 4, likely causing the poorer than expected model fit (indeed, removal of Item 7 generated much improved fit indices; comparative fit index = .97 and root-mean-square error of approximation = .07). However, given the preliminary nature of these analyses and the finding that the mean interitem correlation was within the recommended range (.15 to .50; Clark & Watson, 1995), it appeared premature to delete this item on the basis of this analysis. As such, subsequent analysis included the full eight-item scale.
On the BHS, participants obtained an average score of 5.18 (SD = 4.7), with a range of 0 to 19 (possible range: 0 to 20). Mean scores on the CRH were 1.21 (SD = 1.3), with a range of 0 to 5. Thirty-two participants (14.1%) were diagnosed with a major depressive episode on the basis of the Structured Clinical Interview for DSM-IV interviews, and 30 individuals (13.6%) acknowledged thoughts of suicide, although only two acknowledged having thought about a potential plan to commit suicide; these 30 individuals composed the suicidal ideation present group for the analyses described next. Mean scores on the 20-item SAHD were 2.87 (SD = 3.6), with 17 individuals (8.3%) obtaining scores of 10 or greater, indicating a strong desire for hastened death. Mean scores on the HADS were 5.44 (SD = 4.3) for the Anxiety subscale and 5.49 (SD = 4.2) for the Depression subscale, both of which indicated moderate levels of distress.
Correlations between the HAI and other measures of hopelessness, depression, and psychological distress are presented in Table 3; the vast majority of these coefficients were significant (p < .0001 for all coefficients exceeding .25), even with a conservative Bonferroni correction (Bonferroni corrected p < .05 for all coefficients exceeding .21). Although most of these correlations were roughly comparable across the hopelessness measures, associations were generally higher with the HAI and 20-item BHS compared with the CRH and the abbreviated seven-item BHS. As expected, the BHS was somewhat more strongly associated with the PA than was the HAI, as the latter measure was developed with the goal of minimizing the confounding impact of prognosis on the assessment of hopelessness.
Table 3.
Correlations Between the HAI and Relevant Measures of Concurrent Validity
| Variable | HAI | BHS | BHS-7 | CRH |
|---|---|---|---|---|
| BHS | .78 | 1.0 | ||
| BHS-7 | .70 | .92 | 1.0 | |
| CRH | .74 | .61 | .57 | 1.0 |
| LOT-R | −.63 | − .69 | − .62 | − .47 |
| Prognostic awareness | .22 | .28 | .27 | .11 |
| Illness severity | .25 | .34 | .26 | .05 |
| HADS Depression subscale | .65 | .62 | .57 | .52 |
| HADS Anxiety subscale | .61 | .58 | .53 | .58 |
| FACIT Spiritual Well-Being scale | −.64 | − .68 | − .59 | −.47 |
| SAHD | .60 | .60 | .53 | .44 |
| FSSQ | −.31 | − .32 | − .22 | −.24 |
Note. HAI =Hopelessness Assessment in Illness; BHS =Beck Hopelessness Scale; BHS-7 =abbreviated seven-item version of BHS; CRH =a clinical rating of hopelessness; LOT-R = Life Orientation Test–Revised; HADS =Hospital Anxiety and Depression Scale; FACIT =Functional Assessment of Cancer Therapy; SAHD =Schedule of Attitudes Toward Hastened Death; FSSQ =Duke–University of North Carolina Functional Social Support Questionnaire. p <.0001 for all coefficients exceeding .25.
Because a central focus of hopelessness research at the end of life centers around the unique contribution this construct makes in assessing important mental health outcomes, such as desire for hastened death and suicidal ideation, we analyzed the relative contributions of the HAI, BHS, and CRH after controlling for other potentially important predictors (depression, social support, prognostic awareness), using a series of hierarchical regression models. The first three predictors (HADS Depression subscale, FSSQ, and PA) were entered as a block and accounted for 41% of the variance in desire for hastened death (SAHD total scores). The four hopelessness variables were added, in individual regression models, to this block to estimate the unique contribution of each. The addition of the HAI explained another 13% of the variance, β = .46, t(136) = 5.71,p < .0001, when added to the first block of variables. The BHS also added significant explained variance to the first block of variables (depression, social support, and prognostic awareness) but added considerably less than the HAI, ΔR2 = .09, β = .42, t(136) = 4.93, p < .0001, and the abbreviated seven-item version of the BHS was weaker still when added to the first set of variables, ΔR2 = .06, β = .33, t(136) = 4.02, p < .0001. The CRH added the least amount of explained variance to predicting SAHD scores, ΔR2 = .05, β = .27, t(136) = 3.59, p = .001. A final hierarchical regression model included three measures of hopelessness, entered simultaneously, after the inclusion of the first block of variables (HADS Depression subscale, FSSQ, and PA). This analysis indicated that the HAI provided the largest contribution to the prediction of desire for hastened death, providing a significant contribution even after controlling for other measures of hopelessness, depression, prognostic awareness, and social support (see Table 4).
Table 4.
Multiple Regression Models Predicting Desire for Hastened Death and Suicidal Ideation
| SAHD total score |
Suicidal ideation |
|||||
|---|---|---|---|---|---|---|
| Variable | β | t | p | b | Wald | p |
| HADS Depression subscale | .22 | 2.67 | .009 | 0.08 | 0.49 | .48 |
| FSSQ | .05 | 0.79 | .43 | 0.57 | 1.28 | .26 |
| PA | .15 | 2.48 | .01 | 1.18 | 4.13 | .04 |
| HAI | .35 | 2.92 | .004 | 0.37 | 3.94 | .05 |
| BHS | .21 | 2.02 | .05 | −0.17 | 1.87 | .17 |
| CRH | .00 | 0.01 | .99 | 1.06 | 7.51 | .001 |
Note. SAHD = Schedule of Attitudes Toward Hastened Death; HADS = Hospital Anxiety and Depression Scale; FSSQ = Duke-University of North Carolina Functional Social Support Questionnaire; PA = a measure of prognostic awareness; HAI = Hopelessness Assessment in Illness; BHS = Beck Hopelessness Scale; CRH = a clinical rating of hopelessness.
Even more striking findings emerged when suicidal ideation was treated as the dependent variable (using a series of four logistic regression models rather than the four linear regression models used to predict desire for hastened death). The combination of depression (HADS Depression subscale), prognostic awareness (PA), and social support (FSSQ), when entered as a block, explained 28% of the variance (based on the Nagelkerke R2 statistic) in suicidal ideation, χ2(4) = 36.81, p < .0001, but the addition of the HAI to this model explained another 16% of the variance, Wald χ2(1) = 10.70, p < .0001, and each one-point increase in HAI scores increased the odds of suicidal ideation by 50% (odds ratio [OR] = 1.54). The addition of the BHS, on the other hand, resulted in a small increase in explained variance (4%) beyond the first block of variables (depression, prognostic awareness, and social support) that was not statistically significant, Wald χ2(1) = 3.58,p = .06, and each one-point increase in BHS scores increased the odds of suicidal ideation by 14% (OR = 1.14). Likewise, the abbreviated seven-item BHS added only 3% explained variance to the first block of variables, Wald χ2(1) = 2.66, p = .10. Each one-point increase in the abbreviated BHS increased the odds of suicidal ideation by 24% (OR = 1.24). Of interest, the CRH performed considerably better in predicting suicidal ideation, resulting in an additional 20% explained variance, Wald χ2(1) = 13.28, p < .0001, with each one-point increase in CRH scores increasing the odds of suicidal ideation threefold (OR = 3.22). A final logistic regression analysis, including each of the three measures of hopelessness (HAI, BHS, and CRH), indicated that the HAI provided a significant contribution to the prediction of suicidal ideation, even after inclusion of other measures of hopelessness (the BHS and CRH), as well as measures of depression, social support, and prognostic awareness (see Table 4).
Summary
Preliminary validation analyses using the eight-item scale demonstrated considerable evidence for the internal consistency and concurrent validity of the measure. Despite the relative brevity of the scale, coefficient alpha was strong, and each of the eight items was at least moderately correlated with the total score; factor analysis supported a one-factor model with each variable loading substantially on the central factor (although raising questions about the utility of one of the eight items). Preliminary validation analyses also revealed substantial correlations with other measures of hopelessness and expected correlates (e.g., depression, desire for hastened death, suicidal ideation). Although the magnitude of these correlations was only slightly higher for the HAI compared with other measures of hopelessness, the association with prognostic awareness was also somewhat lower, suggesting that this measure is less likely to be confounded by factors related to advanced illness. Of importance, regression analyses indicated that the HAI accounted for more variance in end-of-life despair measures (desire for hastened death and suicidal ideation) than other measures of hopelessness. In summary, this brief measure demonstrated adequate, albeit preliminary, reliability (internal consistency) and concurrent validity and appears to be less confounded by awareness of one’s prognosis.
Discussion
The three studies reported in this article represent the first attempt to develop a measure of hopelessness that is appropriate for use in patients with a terminal illness. Although theorists have only recently begun to focus on hopelessness as a critical construct for understanding adjustment and despair at the end of life, an ever-growing literature has highlighted the critical importance of this construct. However, measurement has lagged behind this interest, with most researchers relying on measures developed for use with physically healthy, depressed individuals (i.e., the BHS). Having identified a number of problems with this measure in our own research (e.g., Abbey et al., 2006; Rosenfeld, Gibson, Kramer, & Breitbart, 2004), we sought to develop a measure that would be appropriate for this important context.
As expected, the research described here demonstrates that hopelessness is a construct that encompasses a number of different elements, most of which are clearly distinct from one’s awareness of a terminal prognosis. Hopelessness appears to reflect a broad assessment of one’s potential to achieve important goals in a wide range of areas, including the physical, emotional, and interpersonal. Qualitative analysis of patient interviews revealed a number of different aspects of hopelessness, most of which were represented in the final eight-item questionnaire (e.g., affective elements of despair, will to live, sense of futility, cognitive rigidity). The ability to distinguish hopelessness from prognostic awareness is particularly noteworthy given the limited empirical research that has addressed prognostic awareness. Few researchers have systematically studied patient perceptions of their illness, and both scholars and lay people frequently question the ability to distinguish these two constructs.
In addition to helping distinguish hopelessness from prognosis, the HAI demonstrated considerable, unique explanatory power in predicting important psychosocial outcome variables, such as desire for hastened death and suicidal ideation. Although the incremental benefit of the HAI relative to other measures of hopelessness might appear modest, its improved reliability and concurrent validity are more striking given the relative brevity of this measure. Internal consistency (coefficient alpha) was extremely high despite inclusion of only eight items, and the HAI demonstrated substantially greater utility in predicting important psychosocial outcomes (i.e., desire for hastened death and suicidal ideation) than did the lengthier, 20-item BHS. Even more striking improvements were observed when the HAI was compared with the abbreviated, seven-item BHS. In short, the HAI provides a brief index of hopelessness in the context of terminal illness that is only minimally confounded by illness-related factors.
The importance of brevity in the HAI cannot be overstated. As any researcher studying palliative care populations already understands, patient burden is a critical element of conducting end-of-life research. Patients are rarely able to complete lengthy batteries of study instruments, and physical deterioration often limits the feasibility of dividing assessments into smaller, less burdensome units. Thus, developing brief, yet reliable and valid assessment tools for this population can have critical benefits for researchers. Although the use of anchored statements (rather than dichotomous or Likert-type items) may negate some of the brevity (particularly if items and response options are read aloud), our experience administering these items to terminally ill patients suggests that the ease of comprehension for these anchored statements results in a measure that retains the benefits of a brief questionnaire. Clinicians, too, benefit from the availability of brief screening instruments. Although interventions specifically targeting hopelessness do not yet exist (though some interventions have been developed that may have particular utility for such individuals; see Breitbart et al., 2010), the HAI could provide a valuable screening function by identifying patients for whom a more thorough psychological or psychiatric evaluation is warranted (e.g., determining the optimal cutoff for identifying high levels of hopelessness). Clearly, further research is needed to determine how and when the HAI should be used for clinical evaluations.
An important strength in the present study is the use of a multistage approach to measure development. This approach enabled both a broad understanding of the construct of hopelessness as well as a focused assessment of the most critical elements needed to measure the construct. By beginning with a detailed exploration of the construct and applying two large samples to assess the initial item pool and evaluate the preliminary measure, this study provides a comprehensive assessment of hopelessness. The use of multiple independent samples also provides support for the utility of the HAI, because the measure demonstrated strong evidence of concurrent validity with a sample on which item selection was not based.
However, the present study is not without limitations. Although participants were drawn from two separate sites, representing a range of illness severity, both settings provide state-of-the-art treatment. Thus, not only might higher levels of hopelessness emerge in samples drawn from less optimal treatment settings, but stronger associations might exist between hopelessness and psychological distress (i.e., because of greater variance in both hopelessness and distress). In addition, because the present sample was limited to patients diagnosed with advanced cancer, the majority of whom were Caucasian and relatively well-educated, the applicability of the HAI to patients diagnosed with other terminal illnesses, or of disenfranchised ethnic backgrounds is unknown. Although we anticipate that this measure will be no less useful in other palliative care populations (e.g., end-stage dialysis patients, those with Parkinson’s disease, etc.) with varying ethnic and cultural backgrounds (as is common, e.g., in HIV/AIDS research), future research must explore this question.
These limitations notwithstanding, the present study suggests that hopelessness can be quantified using this brief, eight-item measure. Given the emerging evidence for the important role played by hopelessness at the end of life, the development of the HAI has considerable potential for helping assess important outcomes, such as the effectiveness of interventions designed to improve psychological adjustment or the impact of psychological states on end-of-life decisions. Only by developing and validating measures that are tailored specifically for the context of advanced illness can researchers maximize the relevance of their research and best address the clinical needs of patients at this important stage of life.
Acknowledgments
This study was supported by a grant from the National Cancer Institute (Barry Rosenfeld, principal investigator, R01 CA101940). We are indebted to the staff and patients of Memorial Sloan-Kettering Cancer Center, as well as a number of colleagues who helped facilitate this research, including Simon Wein, Steven Passik, David Kissane, Jimmie Holland, Anne Kosinski, Maryann Santasario, James Cimino, Joanna Fava, and Leah Newkirk.
Appendix
Hopelessness Assessment in Illness Questionnaire
| 1. | 0 | I don’t feel discouraged about my future. |
| 1 | I sometimes feel discouraged about my future. | |
| 2 | I often feel discouraged about my future. | |
| 2. | 0 | I don’t have the inner strength to keep fighting this illness. |
| 1 | I don’t know if I have the inner strength to keep fighting this illness. | |
| 2 | I have the inner strength to keep fighting this illness. | |
| 3. | 0 | It is hard to think about anything besides my illness. |
| 1 | Sometimes I can think about things other than my illness. | |
| 2 | I can put my illness out of my mind most of the time. | |
| 4. | 0 | I don’t let myself feel hopeless. |
| 1 | I try to stay hopeful but sometimes I can’t. | |
| 2 | I can’t help feeling hopeless much of the time. | |
| 5. | 0 | I dread every day. |
| 1 | Sometimes it’s hard for me to face the day. | |
| 2 | I usually look forward to each day. | |
| 6. | 0 | I feel a sense of control over my life. |
| 1 | I feel in control of some parts of my life. | |
| 2 | I have no control over my life. | |
| 7. | 0 | I have nothing to look forward to. |
| 1 | I am looking forward to some things | |
| 2 | I am looking forward to many things. | |
| 8. | 0 | I almost always feel hopeful. |
| 1 | Sometimes I feel hopeless but then it passes. | |
| 2 | I almost always feel hopeless. |
Contributor Information
Barry Rosenfeld, Department of Psychology, Fordham University.
Hayley Pessin, Department of Psychiatry and Behavioral Sciences, Memorial Sloan-Kettering Cancer Center, New York.
Charles Lewis, Department of Psychology, Fordham University.
Jennifer Abbey, Department of Psychology, Fordham University.
Megan Olden, Department of Psychology, Fordham University.
Emily Sachs, Department of Psychology, Fordham University.
Lia Amakawa, Department of Psychology, Fordham University.
Elissa Kolva, Department of Psychology, Fordham University.
Robert Brescia, Palliative Care Institute, Calvary Hospital, Bronx, New York.
William Breitbart, Department of Psychiatry and Behavioral Sciences, Memorial Sloan-Kettering Cancer Center, New York.
References
- Abbey JG, Rosenfeld B, Pessin H, Breitbart W. Hopelessness at the end of life: An analysis of the Beck Hopelessness Scale. British Journal of Health Psychology. 2006;11:173–183. doi: 10.1348/135910705X36749. [DOI] [PubMed] [Google Scholar]
- Anda R, Williamson D, Jones D, Macera C, Eaker E, Glassman A, Marks J. Depressed affect, hopelessness, and the risk of ischemic heart disease in a cohort of U.S. adults. Epidemiology. 1993;4:285–294. doi: 10.1097/00001648-199307000-00003. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Brummett BH, Helms MJ, Mark DB, Siegler JC, Williams RB. Depressive symptoms and survival of patients with coronary artery disease. Psychosomatic Medicine. 2000;62:790–795. doi: 10.1097/00006842-200011000-00008. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: The Beck Hopelessness Scale. Journal Consulting and Clinical Psychology. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D. A case of including spirituality in quality of life measurement in oncology. Psycho-oncology. 1999;8:417–428. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Breitbart W, Rosenfeld B, Gibson C, Pessin H, Nelson C, Poppito S, Olden M. Meaning-centered group psychotherapy for patients with advanced cancer: A pilot randomized controlled trial. Psycho-oncology. 2010;19:21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadhead WE, Gehlbach SH, De Gruy FV, Kaplan PH. The Duke–UNC Functional Social Support Questionnaire: Measurement of social support in family medicine patients. Medical Care. 1988;26:709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- Chi GC. The role of hope in patients with cancer. Oncology Nursing Forum. 2007;34:415–424. doi: 10.1188/07.ONF.415-424. [DOI] [PubMed] [Google Scholar]
- Chochinov HM, Tataryn DJ, Wilson KG, Enns M, Lander S. Prognostic awareness in the terminally ill. Psychosomatics. 2000;41:500–504. doi: 10.1176/appi.psy.41.6.500. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Constructing validity: Basic issues in objective scale development. Psychological Assessment. 1995;7:309–319. doi: 10.1037/pas0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson PM, Dracup K, Phillips J, Daly J, Padilla G. Preparing for the worst while hoping for the best: The relevance of hope in the heart failure illness trajectory. Journal of Cardiovascular Nursing. 2007;22:159–161. doi: 10.1097/01.JCN.0000267821.74084.72. [DOI] [PubMed] [Google Scholar]
- DeMaio TJ, Rothgeb JM. Cognitive interviewing techniques: In the lab and in the field. In: Schwartz N, Sudman S, editors. Answering questions: Methodology for determining cognitive and communication processes in survey research. San Francisco, CA: Jossey-Bass; 1996. pp. 177–195. [Google Scholar]
- Embretson SE, Reise SP. Item response theory for psychologists. Mahwah, NJ: Erlbaum; 2000. [Google Scholar]
- Everson SA, Goldberg DE, Kaplan GA, Cohen RD, Tuomilehto J, Salonen JT. Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosomatic Medicine. 1996;58:113–121. doi: 10.1097/00006842-199603000-00003. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM–IV–TR Axis I Disorders. New York, NY: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Kylma¨ J, Vehvila¨inen-Julkunen K, La¨hdevirta J. Hope, despair, and hopelessness in living with HIV/AIDS: A grounded theory study. Journal of Advanced Nursing. 2001;33:764–775. doi: 10.1046/j.1365-2648.2001.01712.x. [DOI] [PubMed] [Google Scholar]
- Levine R. Treating idealized hope and hopelessness. International Journal of Group Psychotherapy. 2007;57:297–317. doi: 10.1521/ijgp.2007.57.3.297. [DOI] [PubMed] [Google Scholar]
- Lord FM. Applications of item response theory to practical testing problems. Mahwah, NJ: Erlbaum; 1980. [Google Scholar]
- Lord FM, Novick MR. Statistical theories of mental test scores (with contributions by Allan Birnbaum) Reading, MA: Addison-Wesley; 1968. [Google Scholar]
- Muraki E, Bock D. Parscale (Version 4) [Computer software] Lin-colnwood, IL: Scientific Software International; [Google Scholar]
- Pedersen SS, Denollet J, Daemen J, van de Sande M, de Jaegere PT, Serruys PW, van Domburg RT. Fatigue, depressive symptoms, and hopelessness as predictors of adverse clinical events following percutaneous coronary intervention with paclitaxel-eluting stents. Journal of Psychosomatic Research. 2007;62:455–461. doi: 10.1016/j.jpsychores.2006.12.018. [DOI] [PubMed] [Google Scholar]
- Rosenfeld B, Breitbart W, Stein K, Funesti-Esch J, Kaim M, Krivo S, Galietta M. Measuring desire for death among patients with HIV/AIDS. American Journal of Psychiatry. 1999;156:94–100. doi: 10.1176/ajp.156.1.94. [DOI] [PubMed] [Google Scholar]
- Rosenfeld B, Gibson C, Kramer M, Breitbart W. Hopelessness and terminal illness: The construct of hopelessness in patients with advanced AIDS. Palliative and Supportive Care. 2004;2:43–53. doi: 10.1017/s1478951504040064. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Sullivan MD. Hope and hopelessness at the end of life. American Journal of Geriatric Psychiatry. 2003;11:393–405. [PubMed] [Google Scholar]
- Walker LO, Avant KC. Strategies for theory construction in nursing. 4th ed. Upper Saddle River, NJ: Prentice Hall; 2005. [Google Scholar]
- Willis GB, Royston P, Bercini D. The use of verbal report methods in the development and testing of survey questionnaires. Applied Cognitive Psychology. 1991;5:251–267. [Google Scholar]
- Wilson KG, Graham ID, Viola RA, Chater S, de Faye BJ, Weaver LA, Lachance JA. Structured interview assessment of symptoms and concerns in palliative care. Canadian Journal of Psychiatry. 2004;49:350–358. doi: 10.1177/070674370404900603. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]