Abstract
Objective
The objective of this study was to assess the predictive value of body mass index (BMI) at earlier ages on risk of overweight/obesity at age of 11 years.
Study Design
This is a longitudinal study of 907 children from birth to age of 11 years. Predictors include BMI at earlier ages and outcome is overweight/obesity status at age of 11 years. Analyses were adjusted for covariates known to affect BMI.
Result
At 11 years, 17% were overweight and 25% were obese. Children whose BMI was measured as percentile once at preschool age had a twofold risk for overweight/obesity at 11 years of age. Risk increased by 11-fold if a child's BMI measured was noted more than once during this age. During early elementary years, if a child's BMI was>85th percentile once, risk for overweight/obesity at 11 years was fivefold and increased by 72-fold if noted more than two times. During late elementary years, if a child's BMI was>85th percentile once, risk for overweight/obesity was 26-fold and increased by 351-fold if noted more than two times. Risk of overweight/obesity at 11 years was noted with higher maternal prepregnancy weight, higher birth weight, female gender and increased television viewing.
Conclusion
Children in higher BMI categories at young ages have a higher risk of overweight/obesity at 11 years of age. Effect size was greater for measurements taken closer to 11 years of age. Pediatricians need to identify children at-risk for adolescent obesity and initiate counseling and intervention at earlier ages.
Keywords: overweight, obesity, preschool, early elementary, late elementary
Introduction
Obesity is recognized as a major cause of health problems in childhood.1 Obesity persists from childhood to adolescence and into adulthood.2,3 Among children in the United States, the prevalence of obesity has increased from approximately 5% in 1963 to 1972 to 17% in 2003 to 2004.4
The health risk of overweight and obesity status in childhood is that the body mass index (BMI) predicts cardiovascular changes in adulthood,1,5,6 early onset of Type II diabetes,7,8 asthma,9 obstructive sleep apnea8 and psychological distress.10–12 Recommendations for the assessment, prevention and treatment of child and adolescent overweight and obesity status have recently been reviewed.1,13,14,15 It is imperative, therefore that obesity be recognized as early as possible in childhood. However, perinatologists and neonatologists are also interested in obesity because there is an emerging hypothesis that obesity may be due to maternal and fetal (developmental) nutrition, developmental exposure to environmental chemicals or the interaction of nutrition and environmental exposures during development.16,17
The National Institute of Child Health and Human Development Study of Early Child Care and Youth Development demonstrated that children with a BMI of>85th percentile as well as a BMI in the high-reference ranges are more likely than children with a BMI <50th percentile to continue to gain weight and reach overweight status by adolescence.18 The sample studied was drawn from middle class families that were predominantly White. The objective of our study was to estimate the predictive value of earlier levels of BMI on later risk of overweight status (≥ the 85th percentile) and obesity (≥ the 95th percentile) during early adolescence in an urban, low socioeconomic status sample while controlling for variables that effect obesity and overweight status. The multi-site longitudinal study evaluating the effect of maternal lifestyle during pregnancy on childhood and adolescent outcome (Maternal Lifestyle Study) offered an opportunity to study risk for obesity in early childhood in this at-risk population.
Methods
The Maternal Lifestyle Study is performed at four sites (Brown University, University of Miami, University of Tennessee at Memphis and Wayne State University) in The Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network with additional support from the National Institute on Drug Abuse. The study was approved by the Institutional Review Board at each of the participating clinical centers and informed consent was obtained before study initiation. The recruitment and selection procedures have been described previously.19 The children were born between May of 1993 and May of 1995. The study groups consisted of 658 cocaine-exposed infants (diagnosed by maternal self-report and meconium analysis of cocaine metabolites by gas chromatography/mass spectroscopy) and 730 comparison group infants matched on race, gender and gestational age. Confidentiality regarding maternal substance use was assured through each center's National Institute on Drug Abuse Certificate of Confidentiality. Children were evaluated on an annual basis from birth to the 11 year visit (to 2006). At each clinic visit, height was measured with the child standing without shoes, feet together on a stadiometer. Weight was measured using a 2-Beam scale with children wearing light clothing (no shoes, no outer clothing and no items that could add weight such as keys, belts or watches). The BMI was determined separately for boys and girls at the Centers for Disease Control and Prevention, and National Center for Health Statistics Growth charts designed for use for children from 2 to 20 years of age.20
Statistical analyses
Children who were present for the 11 year visit and had at least two previous visits at ages 1 through 11 years were included in the study. Odds ratios and 95% confidence intervals for risk for overweight and obesity at 11 years were examined comparing the frequency with which children did reach versus did not reach specific BMI percentiles during the preschool year (2 to 4 years), early elementary (5 to 7 years) and late elementary (8 to 10 years) visit to the clinic. Logistic regression analysis controlled for predefined perinatal, childhood and sociodemographic variables known to affect BMI. The maternal variables included maternal substance use, prepregnancy height and weight and race.4,21,22 The infant variables included birth weight and gender.22 From the age of 6 years, information on physical activity, including hours of exercise, days of exercise in the past week and sport activities from the child and parental interview were obtained using the Child Health and Illness Profile. Information on the hours of watching television (reflecting physical inactivity) was also obtained from the interview of the child at 11 years. Information on diet was obtained from a 3-day food diary using the Nutri-Pro Data System. The sociodemographic variables included assessment of socioeconomic status, education, annual income, occupation and whether the family was living at the Federal Poverty Level.23,24 Only perinatal and neonatal variables were used at birth, whereas variables evaluating physical activity, inactivity, blood pressure and diet were examined at the annual visits between 6 and 11 years of age. Family history and parental blood pressure was available only at the 11 year visit.
Two sets of logistic regression models were conducted. The first set of models predicted whether children were overweight or obese at 11 years of age, based on whether they were 85th to 95th percentile or>95th percentile for weight at earlier ages. Models were developed separately for boys and girls. The second set of models predicted overweight or obese at 11 years, based on BMI at earlier ages. These analyses were conducted for the combined sample. The analyses accounted for clustering of children at the site level using the SUDAAN software (Research Triangle Institute 2008, Research Triangle Park, NC, USA) for cluster-correlated data.
Results
The study sample included 907 children seen at the 11 year visit. Approximately, 42% of the children were overweight or obese, 17% of the entire group was overweight and 25% were obese (Table 1). The clinical characteristics of the sample are shown in Table 2. At 11 years, the mean±s.d. for weight for the boys was 44±13 kg, whereas that of the girls was 48±16 kg. The mean height for the boys was 145±7 cm, whereas that of the girls was 148±8 cm. The BMI for the boys was 21±5, whereas that of the girls was 22±6. Approximately, 14% of the boys were overweight and 24% were obese at 11 years of age. Among the girls, 20% were overweight and 26% were obese.
Table 1.
Descriptive statistics for weight, height and BMI by gender
| Gender/age |
Weight, kg
|
Height, cm
|
BMI
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | s.d. | N | Mean | s.d. | N | Mean | s.d. | 85–94% | ||
| Boys | |||||||||||
| 24 months | 385 | 12 | 2 | 385 | 85 | 3 | 379 | 17 | 1 | 17 | 6 |
| 36 months | 379 | 15 | 2 | 374 | 95 | 4 | 372 | 16 | 1 | 12 | 9 |
| 4 years | 376 | 17 | 2 | 375 | 103 | 5 | 375 | 16 | 2 | 13 | 11 |
| 5 years | 366 | 20 | 3 | 365 | 110 | 5 | 364 | 16 | 2 | 11 | 13 |
| 6 years | 385 | 23 | 4 | 384 | 117 | 5 | 384 | 16 | 2 | 14 | 14 |
| 7 years | 393 | 26 | 6 | 393 | 123 | 5 | 392 | 17 | 3 | 13 | 18 |
| 8 years | 431 | 29 | 7 | 430 | 128 | 6 | 430 | 18 | 3 | 13 | 19 |
| 9 years | 426 | 34 | 9 | 428 | 134 | 6 | 423 | 18 | 4 | 13 | 20 |
| 10 years | 426 | 38 | 11 | 432 | 140 | 7 | 425 | 19 | 5 | 14 | 22 |
| 11 years | 466 | 44 | 13 | 466 | 145 | 7 | 466 | 21 | 5 | 14 | 24 |
| Girls | |||||||||||
| 24 months | 351 | 12 | 2 | 349 | 85 | 4 | 347 | 17 | 2 | 12 | 7 |
| 36 months | 349 | 14 | 2 | 347 | 94 | 4 | 345 | 16 | 2 | 12 | 10 |
| 4 years | 330 | 17 | 3 | 333 | 102 | 5 | 330 | 16 | 2 | 13 | 12 |
| 5 years | 333 | 20 | 5 | 334 | 109 | 5 | 332 | 16 | 3 | 13 | 12 |
| 6 years | 363 | 22 | 6 | 362 | 116 | 6 | 362 | 17 | 3 | 12 | 14 |
| 7 years | 385 | 26 | 8 | 383 | 122 | 6 | 382 | 17 | 4 | 14 | 19 |
| 8 years | 398 | 30 | 10 | 399 | 128 | 7 | 396 | 18 | 4 | 11 | 20 |
| 9 years | 409 | 35 | 12 | 411 | 135 | 7 | 409 | 19 | 5 | 17 | 21 |
| 10 years | 417 | 41 | 14 | 420 | 141 | 8 | 417 | 20 | 5 | 16 | 23 |
| 11 years | 441 | 48 | 16 | 441 | 148 | 8 | 441 | 22 | 6 | 20 | 26 |
Abbreviation: BMI, body mass index.
Table 2.
Logistic regression model predicting BMI>85th percentile at 11 years
| Variable | N | % | Adjusted OR | 95% CI | P-value |
|---|---|---|---|---|---|
| Prenatal/neonatal | |||||
| Male | 466 | 51 | 0.66 | 0.46, 0.96 | 0.029 |
| Race | |||||
| Black | 739 | 81 | 0.78 | 0.46, 1.33 | 0.365 |
| White | 110 | 12 | REF | ||
| Other | 58 | 6 | 1.32 | 0.55, 3.16 | 0.535 |
| Maternal education | |||||
| Less than high school | 352 | 39 | 0.61 | 0.40, 0.93 | 0.021 |
| High school | 369 | 41 | REF | ||
| More than high school | 184 | 20 | 0.98 | 0.61, 1.56 | 0.923 |
| Mother's weight before pregnancy | 147 | 39 | 4.07 | 2.29, 7.22 | <0.001 |
| Birth weight | 2606 | 831 | 1.62 | 1.12, 2.35 | 0.011 |
| SGA | 199 | 22 | 0.91 | 0.51, 1.63 | 0.761 |
| Preterm | 390 | 43 | 1.01 | 0.63, 1.63 | 0.951 |
| Breast fed at 1 month | 92 | 11 | 0.54 | 0.31, 0.95 | 0.031 |
| Cocaine exposure | 381 | 42 | 1.00 | 0.64, 1.55 | 1.000 |
| Opiate exposure | 66 | 8 | 0.83 | 0.40, 1.74 | 0.630 |
| Marijuana exposure | 210 | 23 | 1.01 | 0.67, 1.54 | 0.952 |
| Alcohol exposure | 554 | 61 | 0.86 | 0.59, 1.25 | 0.425 |
| Tobacco exposure | 484 | 53 | 0.87 | 0.54, 1.40 | 0.562 |
| 7 Years | |||||
| Watch TV on school days(Hours) | |||||
| 3 or more hours | 309 | 39 | 1.77 | 1.08, 2.90 | 0.023 |
| 1–2 h | 253 | 32 | 1.15 | 0.72, 1.83 | 0.563 |
| <1 h | 224 | 29 | REF | ||
| Hours exercise or play sports on school days | |||||
| 3 or more hours | 139 | 18 | 0.97 | 0.59, 1.61 | 0.917 |
| 1–2 h | 219 | 28 | 1.09 | 0.70, 1.69 | 0.700 |
| <1 h | 423 | 54 | REF | ||
| 11 years | |||||
| Caloric intake | 2223 | 735 | 0.86 | 0.59, 1.26 | 0.448 |
| Sugar intake | 134 | 57 | 1.10 | 0.69, 1.75 | 0.684 |
| Watch TV per day (Hours) | |||||
| 3 or more hours | 427 | 48 | 1.14 | 0.62, 2.09 | 0.684 |
| 1–2 h | 361 | 40 | 1.51 | 0.84, 2.71 | 0.168 |
| <1 h | 107 | 12 | REF | ||
| Days play active games or sports | |||||
| Almost every day/everyday | 197 | 24 | 0.61 | 0.36, 1.03 | 0.064 |
| Some days | 83 | 10 | 0.70 | 0.39, 1.23 | 0.214 |
| None/very few days | 538 | 66 | REF | ||
Abbreviations: BMI, body mass index; CI, confidence interval; OR, odds ratio; REF, reference category; SGA, small for gestational age.
Note: Model accounts for clustering of children by site. Units for the following variables were modified for the logistic regression model to allow for easier interpretation of odds ratios: maternal weight (pounds/100), birth weight (kg), caloric intake (calories/1000) and sugar intake (sugar/100).
The logistic regression model predicting BMI greater than 85th percentile based on prenatal, neonatal, 7 and 11 year factors is shown in Table 2. Higher maternal prepregnancy weight, higher birth weight and watching 3 h or more of television at 7 years of age was associated with a higher risk of BMI>85th percentile at 11 years of age, whereas male gender and less than a high school maternal education were associated with a lower odds of being overweight or obese at 11 years of age.
The risk of being overweight or obese at 11 years of age, given the number of times the BMI exceeded the 85th percentile or 50th percentile during the preschool, early elementary or late elementary years is shown in Table 3, following adjustment for maternal, neonatal and childhood variables listed in the Table. Children who were percentile at one time between 2 to 4 years of age had twice the risk for overweight status at 11 years. If BMI was measured at percentile for more than two times during this age, the risk increased 11 times. Between 5 and 7 years of age, if BMI percentile was noted once, the risk for becoming percentile at 11 years was fivefold. The risk increased by 72-fold if BMI was measured percentile for more than two times. Between 8 and 10 years of age, if BMI percentile occurred once, the risk for overweight status at 11 years was increased by 26-fold. The risk increased by 352-fold if BMI was measured percentile for more than two times. After controlling for covariates, being overweight at previous visits was associated with increased odds of being overweight at 11 years. Overweight status at 2 years was associated with odds ratio 4.5 (1.7 to 11.8) for overweight status at 11 years. Overweight status at 6, 8 and 10 years was associated with odds ratio of 26.8 (14.2 to 50.3), 86.7 (40.9 to 183.7) and 239.2 (12.1 to 560.5), respectively, of becoming overweight at 11 years.
Table 3.
Adjusted odds ratios of overweight/obese (BMI percentile) at 11 years of age given number of times BMI percentile or BMI percentile during preschool, early elementary or late elementary years
| Age/BMI | Adjusted OR | 95% CI | P-value |
|---|---|---|---|
| Preschool (2–4 years) | |||
| BMI percentile | |||
| Two or more times | 10.58 | 5.25, 21.32 | <0.001 |
| One time | 2.12 | 1.10, 4.09 | 0.024 |
| BMI percentile | |||
| Two or more times | 4.82 | 2.48, 9.37 | <0.001 |
| One time | 1.31 | 0.51, 3.37 | 0.570 |
| Early elementary (5–7 years) | |||
| BMI percentile | |||
| Two or more times | 71.65 | 30.94, 165.96 | <0.001 |
| One time | 5.56 | 2.70, 11.47 | <0.001 |
| BMI percentile | |||
| Two or more times | 17.78 | 8.27, 38.23 | <0.001 |
| One time | 0.61 | 0.15, 2.57 | 0.505 |
| Late elementary (8–10 years) | |||
| BMI percentile | |||
| Two or more times | 351.05 | 126.26, 976.07 | <0.001 |
| One time | 25.82 | 9.97, 66.87 | <0.001 |
| BMI percentile | |||
| Two or more times | 292.82 | 36.53, 2347.06 | <0.001 |
| One time | 5.21 | 0.44, 61.65 | 0.190 |
Abbreviations: BMI, body mass index; CI, confidence interval; OR, odds ratio. Note: Odds ratios account for clustering of children with site and are adjusted for gender, maternal race and education, maternal weight before delivery, SGA, preterm, cocaine, opiate, tobacco, alcohol, marijuana, breast fed at 1 month, birth weight, hours of TV watching at ages 7 and 11, hours of exercise at age 7, days spent doing active games or sports at age 11 and sugar and caloric intake at age 11.
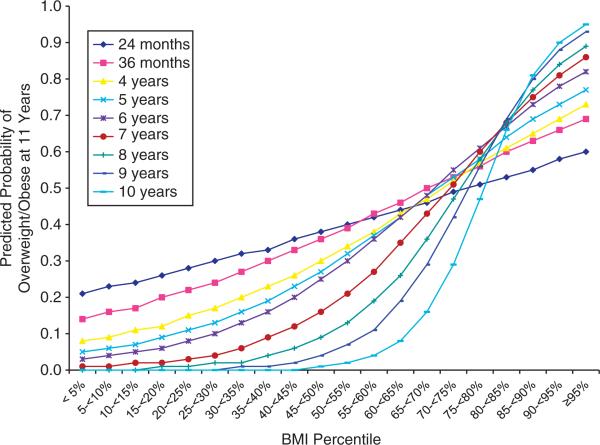
The relationship between being overweight or obese at 11 years of age and BMI at earlier ages is demonstrated in Figure 1. For each age, children were divided into 20 groups, based on their BMI percentiles. The sample sizes across the categories ranged from a low of 3% to a high of 20% of the sample. Logistic regression models were computed to predict the probability of being overweight or obese at 11 years of age for each of the 20 groups at earlier ages. As noted in the figure, children in the higher BMI categories at younger ages had consistently higher probability of being overweight or obese at 11 years of age. This relationship is strongest for the later ages as illustrated by the steepness of the curves.
Figure 1.
Predicted probabilities of overweight/obese (BMI percentile at 11 years by BMI percentiles during earlier years (ages 2 to 10 years)).
Discussion
In this longitudinal secondary analysis of preexisting data involving 907 at-risk children aged 11 years we found an alarmingly high rate (42%) of overweight and obesity. The effect size was greater for BMI measurements taken closer to 11 years. This effect persisted after controlling for perinatal, childhood and sociodemographic variables that contribute to the risk of obesity and overweight status.
In the National Health and Nutrition Examination Study, among 6- to 11-year-old children, the prevalence of obesity was 18.5%.4 In our study we found that 25% of our 11-year-old children were obese. This high rate may reflect the predominately inner city, low socioeconomic status of the children in our study.23,24 Our finding that higher BMI was associated with a higher maternal weight before pregnancy, higher birth weight, female gender and more hours of watching television have been documented by other investigators.1,22,25 In our study we found there was a trend that participation in physical activity could be protective against overweight status (P = 0.09), a finding noted by other investigators.1 We did find a relationship between low maternal education and low child BMI. Recently, van Rossem et al.26 evaluated 2954 Dutch children and found that relative to children from mothers with the highest educational level, mean BMI s.d. scores was lower at 2 years in children with low, mid-low and mid-high educational level, and in the mid-low group at 3 years. They conclude that the inverse relationship between socioeconomic status and childhood overweight presumably emerges after age 3 years.
We evaluated the affect of prenatal substance abuse on the child's BMI at 11 years of age and did not find any relationship. Alcohol use during pregnancy is associated with a negative affect on height, weight and head circumference, whereas cocaine exposure has been associated with impaired growth in childhood.27,28,29 Smoking during pregnancy has been associated with an increase BMI during early childhood as well as adolescence.30,31
The findings of our study parallel those that of the Early Childcare and Youth Development longitudinal study in which it is was shown that children with a BMI>85th percentile are more likely than children whose BMI <50th percentile to continue to gain weight and reach overweight status by adolescence.18 However, our study specifically focuses on high-risk urban, low socioeconomic status children, including those whose mothers had used cocaine, alcohol and tobacco during the pregnancy. Another difference between our study and the Early Childcare Youth Development Study is that our study included preterm infants and our study measured growth at more time points. Lastly, in our study we evaluated the affect of variables known to influence BMI including maternal, child and sociodemographic variables.
The strengths of our study include the large number of children who were evaluated, the prospective nature of the evaluation and the assessment of confounding variables that effect BMI. The drawback of the study is that we did not have assessments of skin fold thickness, measurements of the waist-to-hip ratio or the waist-to-height ratio at 11 years of age.32,33
The clinical implication of this study is that overweight and obesity in adolescence is preceded by increasing BMI in the preschool years. We emphasize that obesity in children is a huge problem. An increase in the percentage of overweight status among non-Hispanic Black adolescents has been noted by other investigators.4 Our findings address this high-risk group because our study population included a high percentage of Black children. Parents and pediatricians need to recognize the early onset of childhood obesity, and efforts to reduce overweight status needs to be initiated in the preschool period. It is possible to prevent as well as treat obesity.1 Our study highlights this association by demonstrating a trend for increased physical activity to be protective, whereas sedentary habits such as television watching increased the risk of obesity. The perinatal period and the period of adiposity rebound 16,17 have been identified as critical periods that effect weight gain for pediatric patients: in our study we have identified the preschool years also as a time when rapid weight gain can affect adolescent obesity.
Acknowledgments
The National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Institute on Drug Abuse (NIDA), the Administration on Children, Youth, and Families and the Center for Substance Abuse and Treatment provided grant support for recruiting subjects into the Maternal Lifestyle Study from 1993 to 1995. NIDA and NICHD provided funding to conduct follow-up examinations in three phases: at 1, 4, 8, 10, 12, 18, 24 and 36 months corrected age (Phase I); at 3½, 4, 4½, 5, 5½, 6, and 7 years of age (Phase II); and at 8, 9, 10 and 11 years of age (Phase III). The funding agencies provided overall oversight of study conduct, but all data analyses and interpretation were completed independent of the funding agencies. We are indebted to our medical and nursing colleagues, the infants and their parents who agreed to take part in this study. Data collected at participating sites of the NICHD Neonatal Research Network (NRN) were transmitted to RTI International, the data coordinating center (DCC) for the network, which stored, managed and analyzed the data for this study. On behalf of the NRN, Dr Abhik Das (DCC Principal Investigator) and Dr Sylvia Tan (DCC Statistician) had full access to all the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. The following investigators, in addition to those listed as authors, participated in this study: Steering Committee Chair: Barry M Lester, PhD, Brown University. Brown University Warren Alpert Medical School Women & Infants Hospital of Rhode Island (U10 HD27904, N01 HD23159): Barry M Lester, PhD, Cynthia Miller-Loncar, PhD; Linda L. LaGasse, PhD; Jean Twomey, PhD. Eunice Kennedy Shriver National Institute of Child Health and Human Development: Rosemary D Higgins, MD. National Institute on Drug Abuse: Vincent L Smeriglio, PhD; Nicolette Borek, PhD. RTI International (U10 HD36790): W Kenneth Poole, PhD; Abhik Das, PhD; Jane Hammond, PhD; Debra Fleischmann, BS. University of Miami Holtz Children's Hospital (GCRC M01 RR16587, U10 HD21397): Charles R Bauer, MD; Ann L Graziotti, MSN, ARNP; Rafael Guzman, MSW; Carmel Azemar, MSW. University of Tennessee (U10 HD42638): Henrietta S Bada, MD; Toni Whitaker, MD; Charlotte Bursi, MSSW; Pamela Lenoue, RN Wayne State University Hutzel Women's Hospital and Children's Hospital of Michigan (U10 HD21385)FSeetha Shankaran, MD; Eunice Woldt, RN MSN; Jay Ann Nelson, BSN. Supported by the Eunice Kennedy Shriver. The National Institute of Child Health and Human Development. Grant Numbers: U10HD21385 (S Shankaran) 10HD36790( C Bann) U10HD27904 (B Lester), U10HD42638 (H Bada) and U10HD21397 (CR Bauer).
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 2.Sun SS, Liang R, Huang TT, Daniels SR, Arslanian S, Liu K, et al. Childhood obesity predicts adult metabolic syndrome: the Fels Longitudinal Study. J Pediatr. 2008;152:191–200. doi: 10.1016/j.jpeds.2007.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hannon ST, Rao G, Arslanian AS. Childhood obesity and type 2 diabetes mellitus. Pediatrics. 2005;116:473–480. doi: 10.1542/peds.2004-2536. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999 to 2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 5.Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: The Bogalusa Heart Study. JAMA. 2003;290:2271–2276. doi: 10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 6.Baker JL, Olsen LW, Søresen TIA. Childhood body mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329–2337. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhargava SK, Sachdev HS, Fall CH, Osmond C, Lakshmy R, Barker DJ, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med. 2004;350:865–875. doi: 10.1056/NEJMoa035698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flint J, Kothare SV, Zihlif M, Suarez E, Adams R, Legido A, et al. Association between inadequate sleep and insulin resistance in obese children. J Pediatr. 2007;150:364–369. doi: 10.1016/j.jpeds.2006.08.063. [DOI] [PubMed] [Google Scholar]
- 9.Ford ES. The epidemiology of obesity and asthma. J Allergy Clin Immunol. 2005;115:897–909. doi: 10.1016/j.jaci.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 10.Franklin J, Denyer G, Steinback KS, Caterson ID, Hill AJ. Obesity and risk of low self esteem: a statewide survey of Australian children. Pediatrics. 2006;118:2481–2486. doi: 10.1542/peds.2006-0511. [DOI] [PubMed] [Google Scholar]
- 11.Jassen I, Craig WM, Boyce WF, Pickett W. Associations between overweight and obesity with bullying behaviors in school age children. Pediatrics. 2004;113:1187–1194. doi: 10.1542/peds.113.5.1187. [DOI] [PubMed] [Google Scholar]
- 12.Williams J, Wake M, Hesketh K, Maher E, Waters E. Health related quality of life of overweight and obese children. JAMA. 2005;293:70–76. doi: 10.1001/jama.293.1.70. [DOI] [PubMed] [Google Scholar]
- 13.Wilfley DE, Stein RI, Saelens BE, Mockus DS, Matt GE, Hayden-Wade HA, et al. Efficacy of maintenance treatment approaches for childhood overweight: a randomized controlled trial. JAMA. 2007;298:1661–1673. doi: 10.1001/jama.298.14.1661. [DOI] [PubMed] [Google Scholar]
- 14.Collins CE, Warren J, Neve M, McCoy P, Stokes BJ. Measuring effectiveness of dietetic interventions in child obesity: a systematic review of randomized trials. Arch Pediatr Adolesc Med. 2006;160:906–922. doi: 10.1001/archpedi.160.9.906. [DOI] [PubMed] [Google Scholar]
- 15.Wunsch R, de Sousa G, Toschke AM, Reinehr T. Intima-media thickness in obese children before and after weight loss. Pediatrics. 2006;118:2334–2340. doi: 10.1542/peds.2006-0302. [DOI] [PubMed] [Google Scholar]
- 16.Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early life conditions on adult health and disease. N Engl J Med. 2008;359:621–673. doi: 10.1056/NEJMra0708473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heindel JJ, vom Saal FS. Role of nutrition and environmental endocrine disrupting chemicals during the perinatal period on the aetiology of obesity. Mol Cell Endocrinol. 2009;304:90–96. doi: 10.1016/j.mce.2009.02.025. [DOI] [PubMed] [Google Scholar]
- 18.Nader PR, O'Brien M, Houts R, Bradley R, Belsky J, Crosnoe R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118:e594–e601. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- 19.Lester BM, Tronick EZ, LaGasse L, Seifer R, Bauer CR, Shankaran S, et al. The Maternal Lifestyle Study: effects of substance exposure during pregnancy on neurodevelopmental outcome in 1-month old infants. Pediatrics. 2002;110:1182–1192. doi: 10.1542/peds.110.6.1182. [DOI] [PubMed] [Google Scholar]
- 20.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Adv Data. 2000;314:1–25. [PubMed] [Google Scholar]
- 21.Whitaker RC. Predicting preschool obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics. 2004;114:e29–e36. doi: 10.1542/peds.114.1.e29. [DOI] [PubMed] [Google Scholar]
- 22.Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: a prospective study for birth to 9.5 years. J Pediatr. 2004;145:20–25. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 23.McKay CM, Bell-Ellison BA, Wallace K, Ferron JM. A multilevel study of the association between economic and social context, stage of adolescence, and physical activity and body mass index. Pediatrics. 2007;119:s84–s91. doi: 10.1542/peds.2006-2089M. [DOI] [PubMed] [Google Scholar]
- 24.Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among US adolescents 1971 to 2004. JAMA. 2006;295:2385–2593. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- 25.Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school age children. Pediatrics. 2004;113:475–482. doi: 10.1542/peds.113.3.475. [DOI] [PubMed] [Google Scholar]
- 26.van Rossem L, Silva LM, Hokken-Koelega A, Arends LR, Moll HA, Jaddoe VWV, et al. Socioeconomic status is not inversely associated with overweight in preschool children. J Pediatr. 2010;157:929–935. doi: 10.1016/j.jpeds.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Hill SY, Shen S, Locke Wellman J, Rickin E, Lowers L. Offspring from families at high risk for alcohol dependence: increased body mass index in association with prenatal exposure to cigarettes but not alcohol. Psychiatry Res. 2005;135:203–216. doi: 10.1016/j.psychres.2005.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Richardson G, Goldschmidt L, Larkby C. Effects of prenatal cocaine exposure on growth. A longitudinal analysis. Pediatrics. 2007;120:e1017–e1027. doi: 10.1542/peds.2006-3482. [DOI] [PubMed] [Google Scholar]
- 29.Lumeng JC, Cabral HJ, Gannon K, Heeren T, Frank DA. Pre-natal exposures to cocaine and alcohol and physical growth patterns to age 8 years. Neurotoxicol Teratol. 2007;29:446–457. doi: 10.1016/j.ntt.2007.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Widerøe M, Vik T, Jacobsen G, Bakketeig LS. Does maternal smoking during pregnancy cause childhood overweight? Paediatr Perinat Epidemiol. 2003;17:171–179. doi: 10.1046/j.1365-3016.2003.00481.x. [DOI] [PubMed] [Google Scholar]
- 31.Leary SD, Smith DG, Rogers IS, Reilly JJ, Wells JCK, Ness AR. Smoking during pregnancy and offspring fat and lean mass in childhood. Obesity. 2006;14:2284–2293. doi: 10.1038/oby.2006.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maffeis C, Banzato C, Talamini G. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr. 2008;152:207–213. doi: 10.1016/j.jpeds.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 33.Lee S, Bacha F, Arslanaian SA. Waist circumference, blood pressure, and lipid components of the metabolic syndrome. J Pediatr. 2006;149:809–816. doi: 10.1016/j.jpeds.2006.08.075. [DOI] [PubMed] [Google Scholar]