Abstract
Background
Identification of psychosocial correlates of health care utilization has become an important strategy in improving clinical care. The objective of the study was to examine the fit of the Information-Motivation-Behavioral Skills (IMB) model, applied to health care utilization among children with sickle cell disease (SCD).
Procedure
Participants were parents of 150 children, ages 1 to 17 years, receiving care in a sickle cell center. Parents completed questionnaires assessing information, motivation, adherence behaviors, and other factors with respect to SCD management. Data regarding health care utilization in the previous 12 months were obtained from parent report and electronic medical records. Stepwise multiple regression analysis was conducted to determine associations between IMB factors and health care use.
Results
Parents rated highly in the domains of information, motivation, and adherence behaviors for managing their child’s SCD. Children of parents reporting higher satisfaction with social supports had higher odds (OR 1.49, 95% CI 1.03–2.15) of 2 or more routine hematology visits in the previous 12 months. Neither information nor adherence behavior was associated with urgent or routine care use. Among other variables measured, high parental illness-related stress and child health status reported as fair/poor were the strongest predictors of urgent care use while private insurance type was the strongest predictor of routine care use.
Conclusions
Among IMB factors, social support was associated with routine health care utilization. Social support and parental illness-related stress may serve as important, modifiable targets in interventions to allocate needed resources to families and reduce unnecessary medical care.
Keywords: Sickle cell disease, Epidemiology, Outcomes research, Health Care Utilization
INTRODUCTION
Sickle cell disease (SCD) is an inherited hemoglobinopathy that occurs in 1 in every 500 African-American births and 1 in every 1000 to 1400 Hispanic American births.[1] Clinical manifestations include vaso-occlusive pain crises, anemic episodes, infections, and stroke.[2,3] The care of children with SCD is marked by substantial utilization of costly health care services.[4] Increasing concerns regarding the rising costs of health care have prompted researchers to identify modifiable psychosocial factors associated with health care utilization.[5–8] The premise behind such efforts is that certain patterns of health care utilization are influenced by psychosocial factors in addition to aspects of the medical condition. While health status functions as an important determinant of child health care use, it only accounts for a portion of the variance in use of medical services.[5]
A limited number of studies have explored the relationship between parental psychosocial factors and health care utilization among children with SCD.[9–13] In a study by Logan et al., parental illness-related stress was the strongest predictor of both urgent and routine service use.[12] Additionally, parental SCD knowledge was related to higher frequency of routine service use. Overall, these previous studies have revealed relatively few psychosocial factors associated with health care use among children with SCD. There is still a need to identify other variables that may more comprehensively explain health care utilization.
Conceptual Model
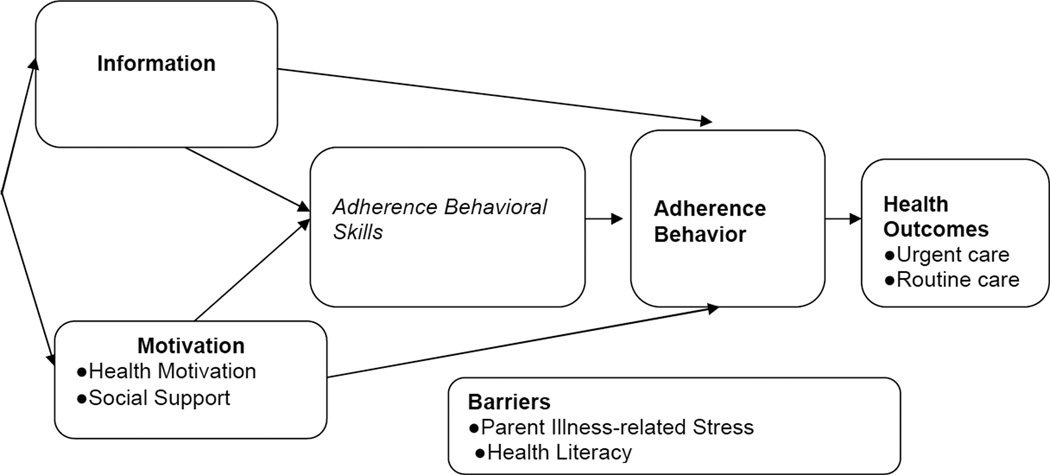
To further assess the relationship between parental variables and child health care utilization, we adopted the Information-Motivation-Behavioral Skills (IMB) model. The IMB model has been validated with a number of health-related behaviors.[14–20] This model postulates that information, motivation, and behavioral skills are fundamental determinants of health-related outcomes such as utilization. Information is comprised of one’s fund of accurate information concerning one’s specific plan of care. Motivation is comprised of components of personal and social motivation, including perceived social support. Behavioral skills describe the competencies necessary to implement information and motivation across various circumstances. Higher information and motivation facilitate effective behavioral skills to improve health-related behavior.[21] In turn, behavior influences health outcomes. We modified the model to assess health care utilization among children with SCD (Figure 1). The IMB model asserts that additional factors may also influence outcomes. We identified parent illness-related stress and health literacy as additional variables to assess based on prior literature.[12]
Figure 1. Adapted Information-Motivation-Behavioral Skills Model of Health Care Utilization for Children with Sickle Cell Disease.
Adherence Behavioral Skills not measured due to lack of available instrument.
The overall purpose of this study was to conduct a preliminary investigation of the applicability of the IMB model to health care utilization among children with SCD. First, this study sought to utilize existing survey instruments to describe the levels of information, motivation, and adherence behavior among parents of children with SCD. Second, we evaluated those factors for their potential utility in predicting health care utilization among children with SCD. We hypothesized that greater parental information, motivation, and adherence behaviors would be associated with lower urgent care use and higher routine care use.
METHODS
Study Design and Participants
Data for this cross-sectional study were drawn from a survey conducted among parents of children with SCD at Texas Children’s Hospital (TCH). A questionnaire was utilized to collect demographic information, parent IMB ratings, and parent-reported health care utilization. The study was approved by the Institutional Review Board of Baylor College of Medicine, Houston, Texas. Written informed consent was obtained for all participants.
Participants were 150 parents of children ages 1 through 17 years with a diagnosis of SCD who had documented visits at the TCH sickle cell center for a minimum of 12 months prior to recruitment. Eligible parents had children with a diagnosis of either hemoglobin SS Disease or sickle beta zero thalassemia. These included parents of children receiving outpatient or inpatient care. Exclusion criteria included parental (1) inability to comprehend English or (2) severe cognitive impairment.
Procedures
Parents were recruited during outpatient visits at the sickle cell center or hospitalizations. Research staff were present in the sickle cell center or rounded with the inpatient hematology service daily from October 15, 2010 to May 4, 2011. Prospective study participants were initially informed of the study by their child’s provider (outpatient) or rounding team (inpatient) prior to recruitment. Prior to recruitment, all subjects were screened for eligibility. We attempted to recruit all subjects eligible for the study.
Measures
Urgent Care
The outcome measure of urgent health care utilization related to SCD in the past 12 months (aggregate of ED visits and hospitalizations) was measured using parent-report. Parent-reported visits to TCH were verified through comparison to the electronic medical record (EMR). Kendall’s τ coefficients were assessed to determine the correlation between parent-reported utilization at TCH and EMR documentation of utilization. These correlated moderately: for frequency of ER visits, r = 0.5, p<0.0001; for hospitalizations, r = 0.6, p<0.0001. Given the overall accuracy documented by correlations, we used parent report of overall visits for data analysis, since that would capture utilization at both TCH and outside facilities.
Routine Care
To assess use of routine hematology care, we used chart review given that all visits would occur at TCH. According to national guidelines, children with SCD are recommended to have at least 2 routine care visits with a hematology provider per year.[1] Therefore, we scored routine care use as a dichotomous variable – either meeting the recommended 2 routine visits per year in the past 12 months or not.
Demographic Questionnaire
Child variables consisted of age, gender, and insurance status. Parental variables consisted of relationship to child, parent age, gender, marital status, and education. As there is no fully validated scoring measure to assess SCD severity[22], we used reported health status as a proxy. To assess health status, we used a previously validated question asking parents, “In general, how would you rate [CHILD’S NAME] health?”[23] Families were given the following options: poor, fair, good, very good, or excellent. We a priori categorized health status as fair/poor versus excellent/very good/good.
Information
Parents completed the Sickle Cell Disease Transition Knowledge Questionnaire (SCDTKQ). This instrument contains 25 multiple choice questions assessing SCD knowledge. The SCDTKQ has been used in prior studies. However, psychometric properties have not been well described.[24]
Motivation
Parental health motivation was assessed using two instruments. The Value on Health Scale (VHS) is a 5-item self-report measure of health motivation.[25] Respondents rate their motivation regarding specific aspects of health on a 4 point Likert scale of “not important at all” to “very important.” The VHS has been used in prior studies.[26] For this study, the questions were modified to assess a parent’s motivation regarding their child’s health rather than their own. Given this modification, we examined internal consistency in our sample. The internal consistency was calculated as α >0 .99 (N = 150).
The Social Support Questionnaire (SSQ) is a 27-item self-report measure used to quantify the availability and satisfaction with social support that an individual has.[27] Each item involves two parts: respondents are asked to list individuals that are available to them for help in individual situational circumstances, and how satisfied they are with the support available. Each circumstance allows a subject to list up to nine individuals. A six point rating scale (from “very satisfied to “very unsatisfied”) is used to rate the individual’s satisfaction with his/her support across all individuals for a particular item. A support score for each item is calculated by the number of individuals the subject lists (number score). The overall support score (SSQN) is calculated by the mean of the number score across items. The overall satisfaction score (SSQS) is calculated by the mean of the satisfaction scores for the 27 items. The SSQ shows both validity and reliability.[27]
Adherence Behavior
The Self Care Inventory – Sickle Cell (SCI-SC) is a parent report measure of adherence behaviors for SCD.[28] Respondents rate how well their child follows physician advice for 13 specific behaviors on a 5 point Likert scale. A validated instrument, the SCI-SC has been used previously in several cross-sectional studies.[24]
Additional Factors
The Pediatric Inventory for Parents (PIP) is a 42-item self-report that measures parental illness-related stress.[29] Each item is rated on two 5-point Likert scales assessing 1) frequency of each stressor and 2) how difficult the issue has been for the parent. Frequency and difficulty scores are determined for the overall total score. The PIP has been validated in previous studies.[29] Health literacy was assessed with the Short Test of Functional Health Literacy for Adults (S-TOFHLA).[30] The 36-point scoring scale of the S-TOFHLA is divided into three categories of functional literacy: inadequate (0–16), adequate (17–22) and functional (23–36). The S-TOFHLA has demonstrated adequate validity and reliability.[31]
Statistical Analysis
Descriptive statistics were generated to characterize the levels of information, motivation, and adherence behaviors among the study sample. The associations between IMB variables, demographics, self-reported health status, and health care utilization were preliminarily assessed using Pearson’s zero-order correlations. Variables with associations p<0.25 were selected to be entered into regression models.
For the purposes of the current analyses, the urgent and routine care variables were transformed. Urgent care utilization was calculated by aggregating the number of ED encounters and hospitalizations. Given the skewed distribution of urgent care events, a square root transformation was performed to establish a near-normal distribution and to reduce the influence of outliers. Routine care use was transformed into a dichotomous variable, 2 or more visits versus not. A series of stepwise multiple regression models were constructed to examine the relative contribution of IMB variables to health care utilization while controlling for demographic variables and child health status. For urgent care, linear regression was conducted, assigning the square root of aggregated encounters as the dependent variable. For routine care use, logistic regression was performed. Statistical analyses were performed using SAS® 9.2 (SAS Institute Inc, Cary, NC).
RESULTS
Descriptive Data
There were 150 children recruited. Of the total population, 137 children were recruited from the sickle cell center and 13 children were recruited from the inpatient service. No statistically significant differences were found between the groups in demographics or parent ratings of IMB variables. The participation rate among eligible families approached for the study was 77% (150/196). Demographics of the 46 families who refused participation showed no statistically significant differences with participating families (data not shown). The characteristics of the 150 parents and their children are shown in Table I.
Table I.
Study Population Demographics and Family Characteristicsa
| Variable | No. (%) N=150 |
|---|---|
| Child Characteristics | |
| Age | |
| 1–5 | 39 (26.0) |
| >5–9 | 46 (30.6) |
| >9–13 | 37 (24.7) |
| >13–17 | 28 (18.7) |
| Gender | |
| Male | 79 (52.7) |
| Female | 71 (47.3) |
| Insurance | |
| Public | 94 (66.7) |
| Private | 47 (33.3) |
| Health Status | |
| Fair/Poor | 32 (22.2) |
| Excellent/Very Good/Good |
112 (77.8) |
| Caregiver Characteristics | |
| Relationship to Child | |
| Parent | 136 (93.2) |
| Other | 10 (6.9) |
| Gender | |
| Female | 133 (91.7) |
| Male | 12 (8.3) |
| Marital Status | |
| Married | 60 (41.1)) |
| Other | 86 (58.9) |
| Education | |
| High school or less | 35 (24.0) |
| More than high school | 58 (39.7) |
| College degree | 53 (36.3) |
Individual categories may not add to 150 due to missing responses.
IMB Factors
Table II provides descriptive information on each predictor variable. Parents reported high levels of SCD knowledge. The Sickle Cell Disease Transition Knowledge Questionnaire mean score for the sample was 21.4 (range 13–25). Parents also showed high levels of health motivation for managing their child’s SCD. The mean score for the Value on Health Scale was 19.6 (range 15–20). For social support, the mean score for SSQN was 2.7 and the mean score for SSQS was 5.4. For the Self Care Inventory-Sickle Cell, the mean score was 4.3 (range 2–5).
Table II.
Parental Scores for IMB Factors
| Measure | Sample Mean (SD) | Sample Range | Possible Score Range |
|---|---|---|---|
| Information | |||
| SCDTKQa | 21.4 (2.9) | 13–25 | 0–25 |
| Motivation | |||
| VHSb | 19.6 (0.9) | 15–20 | 4–20 |
| SSQ Numberc | 2.7 (1.7) | 0–9 | N/A |
| SSQ Satisfaction | 5.4 (1.1) | 1–6 | 1–6 |
| Adherence Behaviors | |||
| SCI-SCd | 4.3 (4.0) | 2–5 | 1–5 |
| Barriers | |||
| PIP total frequencye | 109.2 (31.0) | 42–192 | N/A |
| PIP total difficulty | 97.3 (34.1) | 42–193 | N/A |
| S-TOFHLAf | 34.9 (1.5) | 26–36 | 0–36 |
Sickle Cell Disease Transition Knowledge Questionnaire -Higher scores indicate greater knowledge
Value of Health Scale- Higher scores indicate higher health motivation
Social Support Questionnaire- Higher scores indicate greater support
Self Care Inventory – Sickle Cell - Higher scores indicate greater adherence behaviors
Pediatric Inventory for Parents- Higher scores indicate increased illness-related stress
Test of Functional Health Literacy for Adults- Higher scores indicate greater health literacy; N/A – Due to scoring methodology, possible score range cannot be calculated
For additional factors, the S-TOFHLA mean score was 34.8 (range 26–36) with all subjects meeting criteria for functional health literacy. For the Pediatric Inventory for Parents, there was a very strong relationship between the frequency and difficulty of stress total scores (r=0.9). The research literature on stress and coping demonstrates that frequency of stressors is more important than intensity in adaptive outcomes.[32] Therefore, frequency of illness-related stress variable was retained in subsequent multivariate analyses.
Health care utilization
Analysis of ED use showed that 35% of children (n=51) had no reported visits, while the majority (n=99) had 1 or more visits. The median number of reported ED visits was 2 encounters among children who had any visits (range 1 to 22 visits). Almost half of the children (n= 72) had no reported hospitalizations, while the remainder (n=78) had 1 or more. The median number of reported hospitalizations was 2 inpatient encounters among children who had any hospitalizations (range 1–12 hospitalizations). Overall, the number of events (ED and hospitalizations) was 465 encounters. Twenty percent of ED encounters and 8% of hospitalizations were reported to occur outside TCH. One-fifth of children (n=31) had no reported routine visits to hematology. Sixty-five percent of children (n=98) met the requirement of at least 2 routine visits to hematology in 12 months.
Associations between Parental Psychosocial Measures and Health Care Utilization
Urgent Care
According to Pearson’s correlations, younger child age, public insurance status, younger parent age, and single marital status all demonstrated associations with higher urgent care use with p values <0.25 (Table III). Higher levels of urgent health care use were significantly associated with fair/poor child health status. Among additional factors, higher frequency of parent illness-related stress was also associated with greater urgent care use. No IMB factors were associated with urgent care use.
Table III.
Zero-order Correlations between IMB Factors and Health Care Utilization
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | ||||||||||||||||
| 1. Child age | --- | |||||||||||||||
| 2. Child gender | 0.03 | --- | ||||||||||||||
| 3. Insurance type | −0.1 | −0.06 | --- | |||||||||||||
| 4. Health status | −0.06 | −0.06 | −0.01 | --- | ||||||||||||
| 5. Parent age | 0.35*** | −0.01 | 0.13 | 0.04 | --- | |||||||||||
| 6. Marital status | −0.02 | −0.17** | 0.35*** | −0.09 | 0.03 | --- | ||||||||||
| 7. Education | 0.05 | −0.15 | 0.43*** | 0.1 | 0.19** | 0.25*** | --- | |||||||||
| Additional Factors | ||||||||||||||||
| 8. Health Literacy | −0.1 | −0.06 | 0.07 | 0.09 | −0.02 | 0.15 | 0.28*** | --- | ||||||||
| 9. Parental tress | −0.03 | 0.01 | −0.11 | −0.07 | −0.07 | −0.18** | 0.01 | −0.03 | --- | |||||||
| Information | ||||||||||||||||
| 10. SCD Knowledge | 0.05 | −0.03 | 0.24*** | 0.06 | −0.02 | 0.25*** | 0.43*** | 0.41*** | −0.09 | --- | ||||||
| Motivation | ||||||||||||||||
| 11. Social Support Number | −0.21** | −0.02 | 0.15 | 0.20** | −0.11 | 0.04 | 0.07 | 0.16** | −0.1 | 0.17** | --- | |||||
| 12. Social Support Satisfaction | −0.08 | 0.02 | 0.08 | 0.08 | −0.1 | 0.22** | 0.04 | 0.1 | −0.15 | 0.05 | 0.30*** | --- | ||||
| 13. Health Motivation | −0.05 | −0.02 | −0.01 | −0.03 | 0.08 | −0.02 | 0.05 | −0.05 | −0.15 | 0.04 | 0.01 | −0.01 | --- | |||
| Behavior | ||||||||||||||||
| 14. SCD Adherence Behavior | 0.04 | −0.07 | −0.06 | 0.03 | −0.06 | −0.07 | −0.03 | −0.03 | 0.09 | −0.02 | −0.06 | 0.07 | 0.04 | --- | ||
| 15. Urgent care | −0.15* | 0.02 | −0.10* | −0.27** | −0.13* | −0.15* | 0.03 | 0.08 | 0.36** | 0.04 | 0.04 | 0.03 | −0.1 | −0.09 | --- | |
| 16. Routine care | −0.10* | −0.03 | 0.17** | −0.07 | −0.05 | 0.06 | 0.03 | 0.16* | 0.03 | 0.04 | 0.18** | 0.16* | 0.11* | −0.13* | 0.34 | --- |
p<0.25
p<0.05
p<0.005
In the first step of the linear regression model for urgent care use, demographic variables (child age, insurance type, parent marital status) were entered (See Table IV). Given collinearity between child age and parent age, we chose to omit parent age from the model. The first step of the model demonstrated that younger child age was the only demographic variable that was a significant predictor of urgent care utilization (β=−0.20, p<0.05). The second step of the model investigated the relative contribution of parent-reported child health status when added to the model. Results of the second step revealed that child health status was a significant predictor of health care utilization (R2 Change 0.09, p<0.005). Health status reported as fair/poor was associated with higher urgent care utilization (β=0.84, p<0.005). In the third step of the model, parent illness-related stress was added. Results of the third step demonstrated that parent illness-related stress was a significant predictor of utilization (R2 Change 0.13, p<0.005) and accounted for the largest portion of variance in the model. Higher frequency parental illness-related stress was associated with higher urgent health care utilization (β=0.12, p<0.005).
Table IV.
Stepwise Multiple Regression Analysis to Predict Urgent Care Utilization
| Predictor variables | β (SE)a | R2 | R2 Change | F Change |
|---|---|---|---|---|
| Step 1 – Demographics | 0.04 | 0.04 | 2.13 | |
| Child’s age | −0.20 (0.11)* | |||
| Insurance Type | 0.19 (0.22) | |||
| (Private v. Public) | ||||
| Relationship Status | 0.27 (0.21) | |||
| (Not married v. Married) | ||||
| Step 2 – Illness severity | 0.13 | 0.09 | 5.16** | |
| Health Status | 0.84 (0.23)** | |||
| (Poor/Fair v. Good/VG/EX) | ||||
| Step 3 – Additiona Factors | 0.26 | 0.13 | 8.31** | |
| Illness-related Stress | 0.12 (0.03)** |
p<0.05
p<0.005
Estimates are specific to the step that each variable was first entered
Routine care
According to Pearson’s correlations, lower child age and private insurance demonstrated associations with higher routine care use with p values <0.25 (See Table V). Among parental IMB factors, social support, health motivation, and adherence behaviors were associated with routine health care use with p values <0.25. Health literacy was also associated with routine care use.
Table V.
Stepwise Multiple Regression Analysis to Predict Routine Care Utilization
| Predictor variables | OR (95%CI)a | AIC | AIC Change | c-statistic |
|---|---|---|---|---|
|
Step 1 – Demographics/Additional Factors |
180.30 | 180.30 | 0.64 | |
| Child’s age | 0.80 (0.53–1.22) | |||
| Insurance Type | ||||
| (Private v. Public) | 2.98 (1.29–6.90) * | |||
| Health Literacy | 1.10 (0.87–1.40) | |||
| Step 2 – Behaviors | 177.69 | −2.61 | 0.63 | |
| Adherence Behaviors | 0.94 (0.81–1.10) | |||
| Step 3 – Motivation | 170.95 | −6.74 | 0.70 | |
| Social Support Number | 1.13 (0.86–1.44) | |||
| Social Support Satisfaction | 1.49(1.03–2.15) * | |||
| Health Motivation | 1.35 (0.91–2.01) |
p<0.05
Estimates are specific to the step that each variable was first entered
In the first step of the logistic regression model, child age, insurance type, and health literacy were entered. Only insurance type was found to be associated with routine care use. Children with private insurance had higher odds of 2 or more routine visits (OR 2.98, 95%CI 1.29–6.90). In the second step, adherence behavior was added. Adherence behavior was not associated with routine care visits. In the third step, social support and health motivation were added. Higher satisfaction with social supports was associated with higher odds of having 2 or more routine visits (OR 1.49, 95% CI 1.03–2.15). The increase in the c-statistic across steps of the regression showed improved model discrimination with social support included.
DISCUSSION
The primary aims of this study were to apply the IMB model to SCD and investigate relationships between IMB factors and child health care utilization. We conducted the study with the instruments currently available to measure IMB variables. Of the IMB factors, motivation in the form of satisfaction with social supports was the sole measure to show a relationship with routine health care use. Higher satisfaction with social supports was associated with higher odds of having 2 or more routine visits.
The results regarding the relationship between social support and routine hematology visits represent a novel finding among parents of children with SCD. According to the IMB model, social support may act a proxy for motivation. Perceived social support from others is a social factor that increases internal motivation, which in turn facilitates engagement in behavioral skills. When a patient perceives that significant others (e.g., family, friends) support them, he or she will enact specific adherence-related behavioral skills. The performance of these skills results in adherence behavior, which in turn, produces favorable health outcomes. Previous studies among parents of children with SCD have demonstrated social support as an effective coping mechanism and influential factor during stressful disease-related events.[33] However, no prior studies have documented a relationship between social support and health care use. Our results suggest that interventions based on increasing perceived social support[34] may provide a new strategy toward improving routine care use for children with SCD. Different types of support (e.g., emotional support, social support, physician support) have been shown to influence health related behaviors.[35] A recent study on social support among parents of children with SCD reported that mothers, physicians, the Internet, and books were important sources of support.[36] These specific factors may serve as potential targets in developing evidence-based social support inventions which do not currently exist for this population.
Contrary to our hypotheses, other parental psychosocial factors of our adapted IMB model did not demonstrate a relationship with child health care utilization. Parental information was not associated with routine hematology clinic visits, contradicting a prior study showing more accurate parental information to be associated with increased routine health care use.[12] Additionally, measures of parental health motivation and adherence behaviors did not show relationships with child health care utilization. There are several potential explanations as to why these components did not predict health care use. First, all families were recruited from a sickle cell center. Care in such a setting may especially emphasize parental education and motivation such that scores on the survey instrument would be positively skewed.
Second, our selected psychosocial instruments may be inadequate measures of their intended concepts. In previous studies, parental information has been measured with the Sickle Cell Disease Transition Knowledge Questionnaire, Sickle Cell Disease Knowledge Questionnaire, and a single-question rating of the parent’s comfort with their knowledge of SCD.[12,24,37] The psychometric properties of these instruments are inadequately described in the literature. For health motivation, there are no instruments that assess this concept among parents of children with SCD. While the internal consistency of our modified VHS was excellent, 5 items with a Cronbach α > 0.99 suggest overlapping and potential redundancy in instrument items. For adherence behaviors, we used the Self Care Inventory-SC, which may be biased by social desirability. Biases in self-reporting may also serve as an explanation for the contrary findings with respect to IMB factors. While information was objectively measured, motivation and adherence behavior were assessed with subjective instruments where caregivers could rate themselves favorably. Such biases in self-report may have positively skewed ratings for caregivers such that associations between IMB factors and health care utilization could not be adequately assessed.
It is possible that we did not include some potentially influential factors which would have strengthened our model.[38] Use of active coping by parents and children has been associated with less health service use. Coping strategies as a measure of behavioral skills may have increased the predictive capability of our adapted IMB model for health care utilization.[39] Lastly, it is possible that IMB factors are not the most robust predictors of health care use among children with SCD and other models are more appropriate.[13]
Our findings are consistent with previous studies demonstrating that children of parents with high parenting stress use health care services more frequently.[40,41] In a previous study, parental illness related stress experienced in raising an adolescent with SCD was the most robust predictor of health service use.[12] A small number of qualitative studies among adults with SCD also suggest that stress influences use.[42,43] In other studies, parents who have more illness-related stress tend to self-report fair or poor mental health status.[40] These linkages may allow for consideration of pharmacological or behavioral treatments to address these factors.
Several limitations of the study should be noted. First, information used to determine health status and health care utilization were primarily derived from parent report rather than clinical sources. While parental recall is potentially subject to recall bias, EMR review will not capture utilization at outside institutions. In future studies, administrative record review through payer databases should be utilized. A second limitation was that this study was conducted in a large tertiary center with variable attendance at routine care. We only recruited caregivers of children who had documented visits to the sickle cell center in the past 12 months. Caregivers who do not regularly access care for their children may be fundamentally different from the caregivers in the current study. Third, the structure of the SSQ may introduce response bias by first asking for a list of supportive individuals and then asking about satisfaction. It may be difficult for respondents to provide names and subsequently state they are not satisfied. Finally, as this was a cross-sectional study, causality could not be established. We could not determine whether parental psychosocial factors influenced or were influenced by child health care utilization. Longitudinal, prospective studies will provide more reliable data on the relationship between parental psychosocial factors and child health care utilization.
Conclusions
While specific components of the IMB model may hold promise in identifying parental psychosocial factors influencing SCD health care utilization, the model as a whole was not supported despite adequate sample size and survey instruments. Future work should focus on identifying or constructing more applicable conceptual models to understand how psychosocial factors influence health care use for children with SCD.
Acknowledgements
This study was funded by grants to Dr. Raphael from the Pilot Research Award, Department of Pediatrics, Baylor College of Medicine/Texas Children's Hospital and NIH Grant Number 1K23 HL105568-01A1.
Footnotes
Conflict of Interest Statement
The authors declared no financial interests related to this work.
REFERENCES
- 1.The Management of Sickle Cell Disease: National Institutes of Health: National Heart, Lung, and Blood Institute. 2002 Report. [Google Scholar]
- 2.Frank NC, Allison SM, Cant MEC. Sickle cell disease. In: Brown RT, editor. Cognitive Aspects of Chronic Illness in Children. New York: Guilford Press; 1999. pp. 172–189. [Google Scholar]
- 3.Smith JA. The natural history of sickle cell disease. Ann N Y Acad Sci. 1989;565:104–108. doi: 10.1111/j.1749-6632.1989.tb24156.x. [DOI] [PubMed] [Google Scholar]
- 4.Kauf TL, Coates TD, Huazhi L, et al. The cost of health care for children and adults with sickle cell disease. Am J Hematol. 2009;84(6):323–327. doi: 10.1002/ajh.21408. [DOI] [PubMed] [Google Scholar]
- 5.Loiselle KA, Lee JL, Gilleland J, et al. Factors Associated With Healthcare Utilization Among Children With Noncardiac Chest Pain and Innocent Heart Murmurs. J Pediatr Psychol. 2012;37(7):817–825. doi: 10.1093/jpepsy/jss055. [DOI] [PubMed] [Google Scholar]
- 6.Janicke DM, Finney JW, Riley AW. Children's health care use: a prospective investigation of factors related to care-seeking. Med Care. 2001;39(9):990–1001. doi: 10.1097/00005650-200109000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Richardson LP, Russo JE, Lozano P, et al. The effect of comorbid anxiety and depressive disorders on health care utilization and costs among adolescents with asthma. Gen Hosp Psychiatry. 2008;30(5):398–406. doi: 10.1016/j.genhosppsych.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernal P, Estroff DB, Aboudarham JF, et al. Psychosocial morbidity: the economic burden in a pediatric health maintenance organization sample. Arch Pediatr Adolesc Med. 2000;154(3):261–266. doi: 10.1001/archpedi.154.3.261. [DOI] [PubMed] [Google Scholar]
- 9.Gil KM, Abrams MR, Phillips G, et al. Sickle cell disease pain: 2. Predicting health care use and activity level at 9-month follow-up. J Consult Clin Psychol. 1992;60(2):267–273. doi: 10.1037//0022-006x.60.2.267. [DOI] [PubMed] [Google Scholar]
- 10.Bush PJ, Iannotti RJ. A Children's Health Belief Model. Med Care. 1990;28(1):69–86. doi: 10.1097/00005650-199001000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Kunkel N, Rackoff WR, Katolik L, et al. Utilization of a pediatric emergency department by patients with sickle cell disease. Pediatr Emerg Care. 1994;10(2):79–82. doi: 10.1097/00006565-199404000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Logan DE, Radcliffe J, Smith-Whitley K. Parent factors and adolescent sickle cell disease: associations with patterns of health service use. J Pediatr Psychol. 2002;27(5):475–484. doi: 10.1093/jpepsy/27.5.475. [DOI] [PubMed] [Google Scholar]
- 13.Reese FL, Smith WR. Psychosocial determinants of health care utilization in sickle cell disease patients. Ann Behav Med. 1997;19(2):171–178. doi: 10.1007/BF02883334. [DOI] [PubMed] [Google Scholar]
- 14.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 15.Fisher JD, Fisher WA, Misovich SJ, et al. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996;15(2):114–123. doi: 10.1037//0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- 16.Jaworski BC, Carey MP. Effects of a brief, theory-based STD-prevention program for female college students. J Adolesc Health. 2001;29(6):417–425. doi: 10.1016/s1054-139x(01)00271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher JD, Fisher WA, Amico KR, et al. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462–473. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- 18.Kelly S, Melnyk BM, Belyea M. Predicting physical activity and fruit and vegetable intake in adolescents: a test of the information, motivation, behavioral skills model. Res Nurs Health. 2012;35(2):146–163. doi: 10.1002/nur.21462. [DOI] [PubMed] [Google Scholar]
- 19.Goodell LS, Pierce MB, Amico KR, et al. Parental information, motivation, and behavioral skills correlate with child sweetened beverage consumption. J Nutr Educ Behav. 2012;44(3):240–245. doi: 10.1016/j.jneb.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 20.Pepper JK, Carpenter DM, DeVellis RF. Does adherence-related support from physicians and partners predict medication adherence for vasculitis patients? J Behav Med. 2012;35(2):115–123. doi: 10.1007/s10865-012-9405-5. [DOI] [PubMed] [Google Scholar]
- 21.Amico KR, Barta W, Konkle-Parker DJ, et al. The Information-Motivation-Behavioral Skills Model of ART Adherence in a Deep South HIV+ Clinic Sample. AIDS Behav. 2009;13(1):66–75. doi: 10.1007/s10461-007-9311-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van den Tweel XW, van der Lee JH, Heijboer H, et al. Development and validation of a pediatric severity index for sickle cell patients. Am J Hematol. 2010;85(10):746–751. doi: 10.1002/ajh.21846. [DOI] [PubMed] [Google Scholar]
- 23.National Survey of Children's Health. [Accessed February 3rd, 2012]; < http://www.nschdata.org/Content/LearnAboutTheSurvey.aspx>.
- 24.Jensen S, Elkin T, Hilker K, et al. Caregiver knowledge and adherence in children with sickle cell disease: knowing is not doing. Journal of Clinical Psychology in Medical Settings. 2005;12(4):333–337. [Google Scholar]
- 25.Costa FM, Jessor R, Donovan JE. Value on health and adolescent conventionality: a construct validation of a new measure in problem-behavior theory. Journal of Applied Social Psychology. 1998;19:841–861. [Google Scholar]
- 26.Tucker CM, Butler AM, Loyuk IS, et al. Predictors of a health-promoting lifestyle and behaviors among low-income African American mothers and white mothers of chronically ill children. J Natl Med Assoc. 2009;101(2):103–110. doi: 10.1016/s0027-9684(15)30821-x. [DOI] [PubMed] [Google Scholar]
- 27.Sarason IG, Levine HM, Basham RB, et al. Assessing social support: the social support questionnaire. Journal of Personality and Social Psychology. 1983;44(1):127–139. [Google Scholar]
- 28.Hilker KA, Jordan SS, Jensen S, et al. Development of a screening instrument of adherence in pediatric sickle cell disease. Children'sHealth Care. 2006;35(3):235–246. [Google Scholar]
- 29.Streisand R, Braniecki S, Tercyak KP, et al. Childhood illness-related parenting stress: the pediatric inventory for parents. J Pediatr Psychol. 2001;26(3):155–162. doi: 10.1093/jpepsy/26.3.155. [DOI] [PubMed] [Google Scholar]
- 30.Parker RM, Baker DW, Williams MV, et al. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 31.Baker DW, Williams MV, Parker RM, et al. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 32.Kanner AD, Coyne JC, Schaefer C, et al. Comparison of two modes of stress measurement: daily hassles and uplifts versus major life events. J Behav Med. 1981;4(1):1–39. doi: 10.1007/BF00844845. [DOI] [PubMed] [Google Scholar]
- 33.Barbarin OA, Whitten CF, Bond S. The social and cultural context of coping with sickle cell disease: III. stress, coping tasks, family functioning and children's adjustment. J Black Psychol. 1999;25(3):356–377. [Google Scholar]
- 34.Teri L, McCurry SM, Logsdon R, et al. Training community consultants to help family members improve dementia care: a randomized controlled trial. Gerontologist. 2005;45(6):802–811. doi: 10.1093/geront/45.6.802. [DOI] [PubMed] [Google Scholar]
- 35.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 36.Vaughn LM, McLinden D, Jacquez F, et al. Understanding the social networks of parents of children with sickle cell disease. J Health Care Poor Underserved. 2012;22(3):1014–1029. doi: 10.1353/hpu.2011.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barakat L, Smith-Whitley K, Ohene-Frempong K. Treatment adherence in children with sickle cell disease: disease-related risk and psychosocial resistance factors. Journal of Clinical Psychology in Medical Settings. 2002;9:201–209. [Google Scholar]
- 38.Brown RT, Lambert R, Devine D, et al. Risk-resistance adaptation model for caregivers and their children with sickle cell syndromes. Ann Behav Med. 2000;22(2):158–169. doi: 10.1007/BF02895780. [DOI] [PubMed] [Google Scholar]
- 39.Gil KM, Williams DA, Thompson RJ, Jr., et al. Sickle cell disease in children and adolescents: the relation of child and parent pain coping strategies to adjustment. J Pediatr Psychol. 1991;16(5):643–663. doi: 10.1093/jpepsy/16.5.643. [DOI] [PubMed] [Google Scholar]
- 40.Raphael JL, Zhang Y, Liu H, et al. Parenting stress in US families: implications for paediatric healthcare utilization. Child Care Health Dev. 2010;36(2):216–224. doi: 10.1111/j.1365-2214.2009.01052.x. [DOI] [PubMed] [Google Scholar]
- 41.Barakat LP, Patterson CA, Weinberger BS, et al. A prospective study of the role of coping and family functioning in health outcomes for adolescents with sickle cell disease. J Pediatr Hematol Oncol. 2007;29(11):752–760. doi: 10.1097/MPH.0b013e318157fdac. [DOI] [PubMed] [Google Scholar]
- 42.Leavell SR, Ford CV. Psychopathology in patients with sickle cell disease. Psychosomatics. 1983;24(1):23–25. doi: 10.1016/S0033-3182(83)73256-1. 28–29, 32, 37. [DOI] [PubMed] [Google Scholar]
- 43.Nadel C, Portadin G. Psychological factors associated with onset. New York State Journal of Medicine. 1977;77:1075–1078. [PubMed] [Google Scholar]