ABSTRACT
While key components of the Patient-Centered Medical Home (PCMH) have been described, improved patient outcomes and efficiencies have yet to be conclusively demonstrated. We describe the rationale, conceptual framework, and progress to date as part of the VA Ann Arbor Patient-Aligned Care Team (PACT) Demonstration Laboratory, a clinical care-research partnership designed to implement and evaluate PCMH programs. Evidence and experience underlying this initiative is presented. Key components of this innovation are: (a) a population-based registry; (b) a navigator system that matches veterans to programs; and (c) a menu of self-management support programs designed to improve between-visit support and leverage the assistance of patient–peers and informal caregivers. This approach integrates PCMH principles with novel implementation tools allowing patients, caregivers, and clinicians to improve disease management and self-care. Making changes within a complex organization and integrating programmatic and research goals represent unique opportunities and challenges for evidence-based healthcare improvements in the VA.
KEYWORDS: Information technology, Access-to-care, Veterans, Chronic disease, Self-management, Telehealth, Health system change
OVERVIEW OF VA PATIENT-ALIGNED CARE TEAMS
Caring for the growing number of patients with complex chronic illnesses is increasingly challenging in the primary care setting [1–7]. Providers must follow multiple disparate guidelines [8] while supporting patients' efforts to adhere to complex self-management regimens in order to stay healthy and prevent complications [5, 9–11]. Meeting these challenges within constrained healthcare budgets requires models of care that are coordinated, comprehensive, innovative, and efficient.
The Patient-Centered Medical Home (PCMH) has been proposed as a model of efficient and comprehensive primary care that may improve health care quality as well as patient, family, and provider satisfaction [12, 13]. PCMH initiatives emphasize programs that: are patient-driven, accessible, continuous, efficient, coordinated, and team-based—including an emphasis on the patient and informal caregivers as key members of the team. PCMH seeks to enhance use of health information technologies and population-based registries for coordination and communication, and places a priority on addressing patients' own treatment goals [14–24]. A huge investment of resources is required to re-shape patient care according to PCMH principles, and it is still unclear whether this will improve treatment outcomes while controlling costs [25] (although some early findings are showing positive results) [26]. Nationally, several variants of the PCMH model are currently being implemented and evaluated [21, 27–32].
In 2010, the Department of Veterans Affairs (VA) launched its own national PCMH program, representing one of the largest initiatives of its kind. In addition to its size and scope, the VA PCMH initiative is important because VA treats a population of socioeconomically vulnerable patients with complex chronic illness management needs. These factors increase the importance of the care management principles at the heart of PCMH. VA medical homes are called Patient-Aligned Care Teams (PACT), and the national PACT program is coordinated through the VA Office of Primary Care [24]. The PACT redesign uses a team-based approach with patients viewed at the center of the team, supported by informal caregivers, primary care providers, nurse care managers, clinical associates, and administrative staff [24].
In addition to the PACT redesign affecting all VA primary care sites nationwide, the Office of Primary Care funded five Demonstration Laboratories charged with developing and evaluating innovations to facilitate the cost-effective implementation of PCMH principles. The PACT National Coordinating Center is conducting a national evaluation and facilitating collaboration among the Demonstration Labs. These laboratories allow clinical leaders and established VA health services researchers to work collaboratively in new ways that enhance services within the rubric of PACT goals. New partnerships foster rigorous and iterative evaluation of PCMH programs within “real-world” settings so that both effectiveness and scalability issues can be addressed simultaneously. By virtue of being the largest coordinated network of PCMH evaluations in the country, the VA PACT Demonstration Laboratories ensure that VA will have the best information possible about how to optimize PACT system redesign while generating knowledge that can inform the implementation of PCMH in other health systems nationally. This paper explains in detail the rationale and functioning of new programs being developed as part of the practice redesign in the VA Ann Arbor Healthcare System (VAAAHS), and how the Ann Arbor Demonstration Laboratory is evaluating these innovations to inform continuous service improvements and generate knowledge regarding the value of various initiatives.
THE VA ANN ARBOR HEALTHCARE SYSTEM PACT INITIATIVE
Overview
The VAAAHS, part of Veterans Integrated Service Network 11, was selected as one of the five sites to host a PACT Demonstration Laboratory. The VAAAHS is composed of a large tertiary medical center serving 16,100 veterans in primary care, plus three community-based outpatient clinics that serve a combined population of 16,000 additional patients. The VAAAHS has well-established collaborative relationships with the VA Center for Clinical Management Research, a Health Services Research and Development Center of Excellence located in Ann Arbor, Michigan. Additional relationships supporting the Laboratory include close ties with the Ann Arbor VA Geriatric Research Education and Clinical Center and other research programs within the VA and the University of Michigan.
The goal of the VAAAHS PACT program is to help veterans maintain health, decrease health risks, promote healthy behaviors, and manage stable chronic diseases as well as other health problems. Key features of the program include collaborative decision-making with veterans, services designed to improve access to in-person encounters plus between-visit care, and team-based service delivery with intensive coordination within the team. The primary care team central to the design includes the veteran along with clinical and administrative staff necessary to promote patient-centered outcomes.
The primary objective of the VAAAHS PACT Laboratory is to develop and evaluate innovative programs that facilitate cost-effective, patient-centered care consistent with PCMH goals. Key innovations developed in the VAAAHS PACT Laboratory include: (a) a population-based registry; (b) a navigator system to match veterans to programs based on their preferences and needs; and (c) a menu of technology facilitated self-management support (FSMS) programs that emphasize the use of patient-centered technologies to support self-management and increase the effective involvement of patient-peers and informal caregivers (Fig. 1). Services developed and implemented through the PACT Laboratory are in addition to the standard set of PACT initiatives being deployed within all VA's nationally, such as team-based coordinated care, telehealth, care management, and integration of PACT principles with other VA programs, such as Primary Care-Mental Health Integration, Health Promotion and Disease Prevention Programs, and the VA patient portal, My HealtheVet [33].
Fig 1.
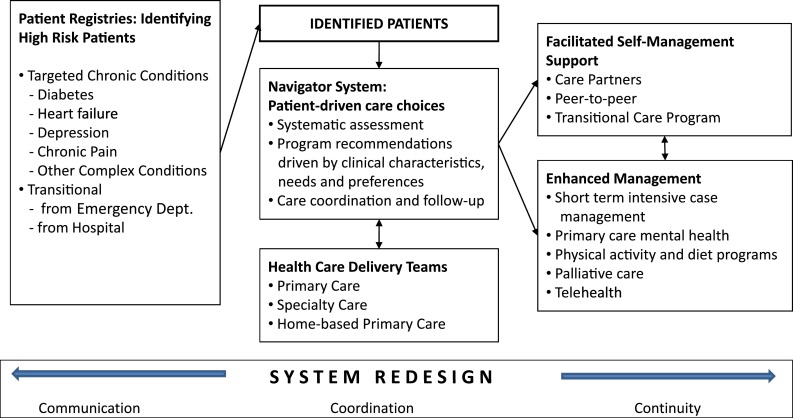
VA Ann Arbor Health System Patient-Aligned Care Team laboratory innovations
Emphasis on new partnerships between clinical operations and research
A major opportunity created by the PACT Demonstration Laboratory has been the development of new collaborative relationships between clinical leadership and the research service. Through this collaboration, the reach of both groups has expanded. The research team brings expertise in registry construction, patient assessments, and outcome measurement, while VAAAHS clinical leaders promote the implementation of new programs in a real-world clinical setting so that services can rapidly impact the care of thousands of patients. Input from clinical team members also ensures that immediate feedback regarding implementation barriers can inform program dissemination, and that the evaluation includes measures for outcomes useful to local decision-makers. Beyond the direct benefit of these relationships for the PACT evaluation, the emphasis on partnered research has had a much broader impact on the way in which investigators understand clinical challenges and how to design research initiatives in order to have the greatest impact on care.
The VAAAHS Laboratory's emphasis on patient-centered health technologies, peer-to-peer support, and support for informal caregivers all reflect clinical leadership priorities for new ways to promote cost-effective chronic illness care as well as researchers' knowledge about emerging evidence-based strategies for supporting self-management. Initiatives for self-care assistance that are being tested through the PACT Laboratory have been developed through studies funded by the VA Health Services Research and Development program, National Institutes of Health, and private foundations; as well as by non-research groups such as the national VA Office of Rural Health and Blue Cross and Blue Shield of Michigan.
VAAAHS PACT LABORATORY INNOVATION COMPONENTS
Registry of complex patients
The foundation of the PACT Laboratory is a patient registry for population-based health management of veterans with complex health problems. The registry targets groups of patients who are likely to benefit from additional assistance, including: (1) veterans transitioning from hospital to home; (2) veterans with priority chronic conditions such as diabetes, heart failure, and depression; and (3) veterans with additional vulnerabilities such as limited social support or low health literacy.
Registries are vital to the effective management of patients with chronic illnesses, and registry use has positive impacts on patient outcomes [34, 35]. Registries assist health care providers in identifying patients who can benefit from additional support, allow for provider feedback on the success of disease management efforts, and facilitate quality monitoring at the health system level [35–37]. A pilot test of the PCMH model using registry data to inform disease management was found to improve patient outcomes [38, 39]. The registry developed as part of the VAAAHS PACT Laboratory is designed to allow patient care teams to target patients at especially high risk for poor outcomes and link them with additional services using a navigator system described below.
The registry draws data from the local electronic medical record system (EMR) “Vista”, including information about patients' demographics, diagnoses, medications, and assignments to primary care and specialty teams. Patients with diabetes, heart failure, or depression are identified based on validated criteria using diagnosis codes and pharmacy records. The Laboratory has developed additional methods for using EMR data to identify patients at especially high risk, such as diabetes patients at high cardiovascular risk and depressed patients with a recent hospitalization. Additionally, the registry will incorporate risk classifications developed by others in VA [40].
The navigator system
Although navigator programs have been developed over many years [41–46], there is no standard definition of core structures or processes [47]. Goals identified as central to most programs include: coordination of patient care, continuous and proactive patient follow-up, and the use of the navigator's specialized knowledge to help patients successfully overcome administrative hurdles and access services [41, 45]. Prior research suggests that navigators can provide high quality evidence-based care, improve efficiency, and improve patient outcomes [42, 43, 48, 49].
Within the VAAAHS PACT program, a navigator service is being used for proactive outreach to patients identified by the registry. Navigator nurses conduct systematic assessments of patients' clinical characteristics, needs, and preferences in order to match patients to available programs. In this way, we hope to improve patients' access to services that are tailored not only based on data easily flagged in the EMR, but also on patient-reported factors that are poorly documented in medical records, such as their social resources. We have developed a computer-based navigator tool in order to allow for standardized patient assessments, goal setting, and shared decision-making about enrollment in programs facilitating self-management [17–19, 50].
Within the targetted chronic conditions identified by the registry, PACT navigators prioritize patients at high risk for adverse outcomes or care coordination problems. Navigators assess patients' needs, resources, and preferences via telephone or in person and using the specially designed software. The initial assessment covers 15 health domains, including patients' cognitive status, social support, functioning, and health literacy. Once the initial assessment is completed, navigators identify services that are appropriate and potentially of interest to the patient. These programs include the full suite of services available as part of the national PACT roll-out (e.g., home-based primary care and diabetes classes), and additional self-management support programs being implemented within the VAAAHS PACT Laboratory. The patient and navigator discuss the programs recommended, identify a treatment plan, and the navigator completes the patient referral. Navigators follow up with patients by phone at 2 weeks, 3 months, 6 months, 9 months, and 12 months after intake to determine if the patient is satisfied and benefiting from the assigned program.
Facilitated self-management programs
Patients with complex chronic conditions often need an enormous amount of support to make difficult behavioral changes and identify health problems in early, addressable stages. Unfortunately, even with the substantial investment associated with the PACT redesign, health care systems such as VA cannot provide this intensive monitoring and patient education during traditional face-to-face encounters or frequent telephone follow-up by nurse care managers. The Laboratory offers facilitated self-management programs designed to increase the quantity and quality of support for patients' disease management cost-effectively.
The CarePartner Program
The VA has a long history of using telehealth services to assess patients' status and provide self-care support between face-to-face encounters [51–57]. The CarePartner program builds on this institutional commitment to telehealth and is designed to enhance care managers' ability to follow patients between visits, providing patients with immediate feedback about health and self-care problems, and leveraging the support of informal caregivers or “CarePartners” (CPs).
The CarePartner Program consists of automated telephone monitoring and behavior change calls that are sent to participants' telephone once per week. During the calls, patients report information about their health and self-care, and receive tailored advice about how to manage their chronic diseases better. Feedback about patients requiring additional attention is sent to their PACT team automatically (via structured fax alerts), and to informal caregivers via structured emails and a specially designed voicemail service.
This program builds on more than 10 years of research on the use of automated telephone calls to improve self-management support for veterans with chronic diseases [55, 58–60]. In a pilot study [61], heart failure patients used proactive weekly automated calls to report information about their health and self-care and receive tailored feedback and education. Patients completed 90% of their assessments, and only 13% could not identify an informal caregiver willing to participate with them as their “CarePartner.” The service elicited self-care-specific communication between patients and their informal caregivers, and a high level of patient satisfaction. The content for the CarePartner program targeting veterans with diabetes, depression, and heart failure was developed with input from VA primary care providers, experts in health communication, and clinical specialists (e.g., cardiologists and psychiatrists). As part of the PACT, nurse navigators will offer this service to patients with these conditions. Early feedback suggests that a large number of veterans who have been offered the CarePartner program along with other innovations in the PACT choose the CarePartner program because of its convenience and involvement of informal caregivers.
Peer-to-peer support
As the number of people suffering with chronic conditions continues to rise, their service needs put an increasing strain on primary care resources. Peers living with a similar health problem can provide emotional support, self-care education, and assistance with solving real-world self-management problems [62, 63]. Peer support programs seek to improve patient self-care and outcomes, while reducing the number of provider visits through psychosocial support and disease self-management advice [64–66]. Peer support models are effective for patients with a variety of behavioral health needs, including patients with diabetes [66–69], depression [65], limitations in physical functioning [70], and heart failure [71].
Group visits are one important component of many peer-support programs [72], but VA patients often face the same barriers to accessing those services as they do to accessing one-on-one outpatient encounters. The peer-support program offered as part of the PACT combines group visits with a specially designed telephonic platform facilitating communication between veterans facing similar challenges. In a recently completed randomized trial, VA patients with diabetes and poor glycemic control were randomized to usual care management or care management plus the peer-support program [73]. Intervention patients experienced a substantial improvement in glycemic control after 12 months. Other data suggest that depressed veterans are willing and able to use the specialized telecommunication platform to talk regularly with a peer partner [74]. The PACT peer-to-peer program builds on this evidence and focuses initially on patients with diabetes or depression who are identified by the navigator using the registry.
Improving transitions from hospital to home
One in five hospitalized patients experiences a poor outcome in the first month following discharge [75, 76]. Appropriate self-care can prevent short-term readmissions, but many patients have difficulty understanding their post-hospitalization medication regimens or the signs of a worsening health problem [77, 78]. Due to inadequate clinical monitoring, such patients often are not assisted before they experience an adverse event [76, 79].
The transition support program offered by the PACT Laboratory is designed to facilitate a structured, coordinated effort between clinicians, patients, and family caregivers to assure transition quality and prevent acute events. The program builds on state-of-the-art models of transition support developed by Eric Coleman and others [80–83], which target patients with conditions associated with a high risk for preventable readmissions. Using the registry, PACT navigators identify hospitalized patients who are being discharged to the community and offer them the program as an enhancement to usual transitional care. The program promotes care processes that can prevent short-term readmission [81, 84], including: appropriate medication use, use of a patient-oriented health record, timely post-discharge follow-up in ambulatory care, and patient education about health status changes that signal the need for rapid clinical attention. A key program element is regular post-discharge telephone calls using an automated assessment and self-care education system that addresses risk factors for re-hospitalization. The calls also provide information about appointments, a way to connect immediately with VA telehealth nurses, and the opportunity for asynchronous communication between the patient and primary care team via voicemail or email using a secure patient portal. Based on patients' assessments during the automated calls, primary care teams receive follow-up reports about urgent problems, and informal caregivers use email and a specially designed voicemail service to receive updates about the patient's status along with advice about what they can do to help.
IMPLEMENTATION AND FORMATIVE EVALUATION METHODS
In order to develop an effective, sustainable implementation, we conducted an extensive baseline evaluation with key stakeholders. This baseline evaluation included a patient focus group; observations of the clinical environment; and semi-structured interviews with 65 health system managers, physicians, nurses, clerks, social workers, pharmacists, and dietitians. De-identified summaries of the interviews were provided to the clinical leadership as part of an ongoing dialog between the clinical and research teams. These evaluation results were then used to shape the implementation of the new programs and ensure they fit with operational goals.
To evaluate the impact of the PACT Laboratory programs on treatment quality, patient outcomes, staff experience, and resource use, we are using a quasi-experimental design that includes formative evaluation and mixed-methods [85]. Two “early innovation” sites will implement the registry and navigator systems along with the portfolio of technology facilitated self-management support programs described above. Two years later, the “later innovation” sites will implement these programs, while other programs are expanded to address additional patient groups, such as those with chronic pain. We will take advantage of the program's staged implementation to evaluate impacts using an interrupted time series design with historical as well as concurrent controls.
The research team is conducting real-time formative evaluations to provide feedback to clinical operations about factors that may affect decisions about the PACT implementation. The evaluation includes information about patient enrollment in PACT programs, formation and function of new PACT clinical teams, and staff and patient experiences with newly implemented programs. Qualitative data collection will include direct observation of the nurse navigators and the post-hospitalization transition process. Our formative evaluation is guided by the Consolidated Framework for Implementation Research (CFIR) [86]. The CFIR was chosen because it draws on several other implementation models, such as the PARIHS [87], diffusion of innovation [88], and dimensions for strategic change [89], in order to take into account a diverse set of factors influencing and then influenced by practice changes (e.g., organizational culture, resource constraints, and provider satisfaction).
Additionally, implementation and evaluation of PACT redesign are influenced by our dialogs with clinical, operations, and research leaders throughout the VA nationally. For example, we are learning from other PACT Demonstration Laboratories, and coordinating our evaluations, through frequent contact directed by the PACT National Coordinating Center. This coordinated approach ensures that similar evaluation methods are being used across the labs and that programs found to be effective (or not) at one site can be considered for testing in other sites. National coordination also makes possible rapid dissemination of early products (e.g. the navigator tools) through clinical and operations leaders along with information about barriers and facilitators to implementation.
In the summative evaluation, we are focusing on measuring processes and outcomes that are most directly related to PACT Laboratory innovations and that follow along VA-identified PACT dimensions (See Table 1). For example, we will assess whether implementation of the between-visit self-care support programs results in an increase in patients' use of alternatives to face-to-face visits, as well as a decrease in readmissions. Resource use evaluations will focus on the extent to which care for chronic diseases such as depression or diabetes is consistent with VA treatment guidelines and will ensure that interventions do not lead to an over-use of treatments such as anti-hyperglycemic therapy. Because much of the focus in the PACT is on self-care behavior and other patient-centered outcomes; patient satisfaction, increased self-care self-efficacy, and specific behavior changes will be central to measuring the impact of the system redesign.
Table 1.
PACT laboratory innovations and selected evaluation measures
| VA PCMH principle | Innovation | Evaluation measures |
|---|---|---|
| Patient-driven | Navigators assess quality of life and risk for poor outcomes | HRQL and depressive symptoms |
| Self-care self-efficacy and behaviors | ||
| Service choices based on patient needs and goals | Patient experiences with care | |
| Team-based | Structures and processes promote coordination within and across teams | Clinician roles and responsibilities |
| Team functioning | ||
| Efficient | Registries identify complex patients | Registry timeliness and accuracy |
| Use of between-visit support and alternatives to face-to-face visits | ||
| Technology facilitated self-management support | Access to primary care and case management | |
| Personnel costs | ||
| Comprehensive | Integration between primary and specialty care | Technical quality of chronic disease care |
| Continuous | Improved transitions from hospital to home | Preventable readmissions |
| Timely post-discharge follow-up | ||
| Caregiver involvement | ||
| Coordinated | Navigator system and technology tools to support coordination | Timely navigator follow-up and coordination of care |
| Enhanced communication | Technology-based facilitated self-care programs for patients, clinicians, and caregivers | Use of technology |
| Communication with caregivers |
PACT Patient-Aligned Care Teams, PCMH Patient-Centered Medical Home, HRQL health-related quality of life
Cost analysis will focus on direct medical costs associated with inpatient and outpatient utilization [90]. We will determine the costs of core program components, including the tools and personnel required for implementing the registry and navigator system, and costs associated with the facilitated self-management programs. Developmental costs will be considered as part of our sensitivity analysis since these costs are likely to vary in the future depending on the extent to which additional development might be required. In addition to the evaluation of the overall initiative's effectiveness, we will evaluate the impact of individual PACT program components. A primary goal of the PACT Demonstration Laboratory evaluation is to provide new information regarding the effectiveness of these services as a portfolio of care management tools within the context of a real-world VA system. For example, potential changes in utilization among participants in the CarePartner program will be compared to wait-list controls and to utilization among program refusers. Since comparison groups will not be randomized, differences in baseline risk for various outcomes will need to be taken into account. However, in conjunction with ongoing qualitative feedback from patients and staff, these comparisons will inform efforts to continually improve program performance.
CHALLENGES AND UNANSWERED QUESTIONS
Evaluating fundamental changes to a complex healthcare system is inherently challenging. One challenge is coordinating quantitative and qualitative evaluation methods across the interrelated aspects of the innovations and PACT redesign. For example, the post-discharge transitions program and navigator service both create new nurse roles and responsibilities at the same time that nurses are adapting to working in teams. Evaluation must therefore look at many complex processes, including team functioning, role changes, and coordination of care across inpatient, outpatient, and facilitated self-management services. Qualitative assessments may shed light on how these functions jointly affect such diverse outcomes as re-hospitalization, efficiency, and patient quality of life. A more fundamental challenge is conducting an evaluation of new programs in a setting where the care organization is continually changing and responding to new directives and operational needs. Such evaluations are by their nature “messy.” Because change happens incrementally, we are unable to define a true baseline, and it will be impossible to attribute improvements in processes or outcomes definitively to individual program components. Rather, conclusions we draw will be about the collective innovations of PACT redesign in VAAAHS, and the qualitative and quantitative formative evaluations will help us understand which program elements may have been more or less influential.
As the result of the dedication of VA operations and clinical leaders to using the most innovative evidence-based care to enhance treatment quality, and the distinguished, long-established national VA HSR&D program that focuses on innovations for veteran-centric services, VA is in a unique position to enhance the way PCMH principles are translated to care. Indeed, a great strength of the VA is the ability to fund visionary programs like the PACT Laboratories, translate lessons from research into improvements in care, and evaluate the effect of such programs in an integrated healthcare system. While in many instances researchers and operations' leaders have been working together effectively for years, complex initiatives such as the PACT program still presents challenges, as the requirements for research, such as institutional review board (IRB) oversight and the need for controlled environments often collide with the realities of clinical operations (e.g., fast turnaround and the need to respond to new directives). Research and clinical leaders should continue to refine operating policies for the role of IRB in implementation evaluation, the efficient use of contracting, and the mechanisms to meet federal regulations such as those from the Office of Management and Budget, in order to fulfill the complete vision of research-operations partnerships.
CONCLUSIONS
The Patient-Centered Medical Home (PCMH) model represents an unprecedented effort to redesign health systems so that they better serve patients with chronic health care needs. As the largest single health system serving socioeconomically vulnerable and clinically complex patients, the VA's PACT program is investing substantial resources into re-shaping the services available to veterans in order to improve access to quality care within the framework of PCMH. Such a massive system restructuring within the context of a large, publically run healthcare system brings significant challenges. However, by providing a vehicle for linking researchers and clinical leadership, and encouraging the use of innovative programs that facilitate cost-effective self-care support, the PACT Laboratories can build on the unique resources of VA nationally, while fostering creative problem-solving that results from researchers and clinical leaders working closely together. The VAAAHS PACT Laboratory is evaluating a suite of innovative programs for identifying patients with complex needs and linking them with cost-effective services that emphasize self-care support. The investment in evaluation that is central to this effort will provide information that is useful for PCMH implementation not only within VA but also throughout the country.
Acknowledgments
Funding
Funding for the VAAAHS Demonstration Laboratory is through the Office of Primary Care, Veterans Health Administration, Department of Veterans Affairs. Additional support is derived from the VA Health Services Research and Development Service and the VA Quality Enhancement Research Initiative. John Piette is a VA Senior Research Career Scientist. Dr. Blaum is supported in part by the Ann Arbor VA Geriatric Research Education and Clinical Center. Drs. Piette, Krein, and Kerr are supported in part by the Michigan Diabetes Research and Training Center (NIH no. DK020572).
VAAAHS PACT Steering Committee
Caroline Blaum, MD, MS; Jane Forman, ScD, MHS; C. Leo Greenstone, MD; Cathy Kerr, MHSA; Eve Kerr, MD, MPH; Tom Kerr, MPH; Sarah Krein, PhD, RN; Wendy Morrish, BSN, RN; John Piette, PhD; Denny Ramsey, BSN, MSN; Darcy Saffar, MPH; and Adam Tremblay, MD
Additional VAAAHS PACT Advisors
Davoren Chick, MD; Jean Malouin, MD, MPH; Robert McDivitt, FACHE; Richard Moseley, MD; Alan Pawlow, MD; Sanjay Saint, MD, MPH; Connie Standiford, MD; Brent Williams, MD, MPH; Ronald Wuthrich; and Eric Young, MD, MS
Conflicts of interest
None of the authors has any conflicts of interest related to this study. The views expressed in this paper do not necessarily represent the official views of the Department of Veterans Affairs.
Footnotes
Implications
Practice: This portfolio of innovative services may improve the intensity and quality of self-management support without unacceptable increased demands on clinician time.
Policy: The VA PACT Demonstration Laboratories will not only provide evidence regarding specific innovations for improving chronic illness care, but more generally will provide evidence about the impacts of Patient-Centered Medical Home principles.
Research: The VA PACT program provides unprecedented opportunities to evaluate novel care management interventions in real-world primary care settings.
References
- 1.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood) 2009;28:175–185. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen E, Thorn D, Hessler D, et al. Using the teamlet model to improve chronic care in an academic primary care practice. Journal of General Internal Medicine. 2010;25(Suppl. 4):610–614. doi: 10.1007/s11606-010-1390-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ostbye T, Yarnall K, Krause K, Pollack K, Gradison M, Michener J. Is there time for management of patients with chronic disease in primary care? Annals of Family Medicine. 2005;3:209–214. doi: 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yarnall K, Pollack K, Ostby T, Krause K, Michener J. Prmary care: Is there enough time for prevention? American Journal of Public Health. 2003;93(4):635–641. doi: 10.2105/AJPH.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patient with chronic illness: The chronic care model, part 2. Journal of the American Medical Association . 2002;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 6.McGlynn E, Asch S, Adams J, Kessesy J. The quaity of health care delivered to adults in the United States. The New England Journal of Medicine. 2003;348(26):2635–2646. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. Journal of the American Medical Association . 2003;289(19):2560–2571. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 8.Boyd CM, Darer J, Boult C, Fried L, Boult L, Wu A. Clinical practice guidelines and quality of care for older patients with multiple comorbid disease. Journal of the American Medical Association . 2005;294(6):716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- 9.Glasgow RE, Funnell MM, Bonomi A, Davis C, Beckham V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough. Annals of Behavioral Medicine. 2002;24(2):80–87. doi: 10.1207/S15324796ABM2402_04. [DOI] [PubMed] [Google Scholar]
- 10.Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling. 2002;48(2):177–187. doi: 10.1016/S0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 11.Holman H, Lorig K. Patient self-management: A key to effectiveness and efficiency in care of chronic disease. Public Health Reports. 2004;119(3):239–243. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American College of Physicians (2007) Joint principles of a patient-centered medical home released by organizations representing more than 300,000 physicians. http://www.acponline.org/pressroom/pcmh.htm. Accessed September 2, 2008.
- 13.Barr M, Ginsburg J (2008) The advanced medical home: A patient-centered, physician-guided model of health care. www.acponline.org/running_practice/pcmh. Accessed 5 December 2008.
- 14.Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. Journal of General Internal Medicine. 2010;25(6):601–612. doi: 10.1007/s11606-010-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paulus R, Davis K, Steele G. Continuous innovation in health care: Implications of the Geisinger Experience. Health Affairs. 2008;27(5):1235–1245. doi: 10.1377/hlthaff.27.5.1235. [DOI] [PubMed] [Google Scholar]
- 16.Reid R, Fishman P, Yu O, et al. Patient-centered medical home demonstration: A prospective, quasi-experimental before and after evaluation. The American Journal of Managed Care. 2009;15(9):e71–e87. [PubMed] [Google Scholar]
- 17.Bitton A, Martin C, Landon BE. A nationwide survey of patient centered medical home demonstration projects. Journal of General Internal Medicine. 2010;25:584–592. doi: 10.1007/s11606-010-1262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crabtree BF, Chase SM, Wise CG, et al. Evaluation of patient centered medical home practice transformation initiatives. Medical Care. 2011;49(1):10–16. doi: 10.1097/MLR.0b013e3181f80766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crabtree BF, Nutting PA, Miller WL, Stange KC, Stewart EE, Jaen CR. Summary of the National Demonstration Project and recommendations for the patient-centered medical home. Annals of Family Medicine. 2010;8(Suppl 1):S80–S90. doi: 10.1370/afm.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedberg MW, Safran DG, Coltin KL, Dresser M, Schneider EC. Readiness for the patient-centered medical home: Structural capabilities of Massachusetts primary care practices. Journal of General Internal Medicine. 2009;24(2):162–169. doi: 10.1007/s11606-008-0856-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller WL, Crabtree BF, Nutting PA, Stange KC, Jaen CR. Primary care practice development: A relationship-centered approach. Annals of Family Medicine. 2010;8(Suppl 1):S68–S79. doi: 10.1370/afm.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association (2007) Joint Principles of the Patient-Centered Medical Home. http://www.medicalhomeinfo.org/downloads/pdfs/jointstatement.pdf. Accessibility verified 2011.
- 23.American College of Physicians (2006) The advanced medical home: A patient-centered, physician-guided model of health care. http://www.hhs.gov/healthit/ahic/materials/meeting03/cc/ACP_Initiative.pdf.
- 24.Affairs USDoV. Patient-Centered Medical Home Concept Paper. Patient Aligned Care Team (PACT) [2010; http://www.va.gov/PrimaryCare/docs/pcmh_ConceptPaper.doc. Accessed March 22, 2011.
- 25.Homer CJ, Baron RJ. How to scale up primary care transformation: What we know and what we need to know? Journal of General Internal Medicine. 2010;25(6):625–629. doi: 10.1007/s11606-010-1260-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takach M. Reinventing Medicaid: State innovations to qualify and pay for patient-centered medical homes show promising results. Health Affairs (Millwood) 2011;30(7):1325–1334. doi: 10.1377/hlthaff.2011.0170. [DOI] [PubMed] [Google Scholar]
- 27.Jaen CR, Crabtree BF, Palmer RF, et al. Methods for evaluating practice change toward a patient-centered medical home. Annals of Family Medicine. 2010;8(Suppl 1):S9–S20. doi: 10.1370/afm.1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jaen CR, Ferrer RL, Miller WL, et al. Patient outcomes at 26 months in the patient-centered medical home National Demonstration Project. Annals of Family Medicine. 2010;8(Suppl 1):S57–S67, S92. doi: 10.1370/afm.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaen CR. Journey to the patient-centered medical home: A qualitative analysis of the experiences of practices in the National Demonstration Project. Annals of Family Medicine. 2010;8(Suppl 1):S45–S56. doi: 10.1370/afm.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stange KC, Miller WL, Nutting PA, Crabtree BF, Stewart EE, Jaen CR. Context for understanding the National Demonstration Project and the patient-centered medical home. Annals of Family Medicine. 2010;8(Suppl 1):S2–8. doi: 10.1370/afm.1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stewart EE, Nutting PA, Crabtree BF, Stange KC, Miller WL, Jaen CR. Implementing the patient-centered medical home: observation and description of the National Demonstration Project. Annals of Family Medicine. 2010;8(Suppl 1):S21–S32. doi: 10.1370/afm.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bojadzievski T, Gabbay RA. The patient-centered medical home and diabetes care. Diabetes Care. 2011;34(4):1047–1053. doi: 10.2337/dc10-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nazi KM, Hogan TP, Wagner TH, McInnes DK, et al. Embracing a health services research perspective on personal health records: Lessons learned from the VA My HealtheVet system. Journal of General Internal Medicine. 2010;25(Suppl 25):62–67. doi: 10.1007/s11606-009-1114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kilbourne A, Schulberg H, Post E, Rollman B, Herbeck Belnap B, Pincus H. Translating evidence-based depression management services to community-based primary care practices. The Milbank Quarterly. 2004;82(4):631–659. doi: 10.1111/j.0887-378X.2004.00326.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nobel JJ, Norman GK. Emerging information management technologies and the future of disease management. Disease Management. 2003;6(4):219–231. doi: 10.1089/109350703322682531. [DOI] [PubMed] [Google Scholar]
- 36.Wagner E, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: Translating evidence into action. Health Affairs. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 37.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. The Milbank Quarterly. 1996;74(4):511–544. doi: 10.2307/3350391. [DOI] [PubMed] [Google Scholar]
- 38.Rice K, Dewan N, Bloomfield H, et al. Disease management program for chronic obstructive plumonary disease: A randomized controlled trail. American Journal of Respiratory and Critical Care Medicine. 2010;182(7):890–896. doi: 10.1164/rccm.200910-1579OC. [DOI] [PubMed] [Google Scholar]
- 39.Grumbach K, Grundy P (2010). Outcomes of implemented patient centered medical home interventions: A review of the evidence from prospective evaluation studies in the United States. Patient-Centered Primary Care Collaborative.http://www.pcpcc.net/content/pchm-outcome-evidence-quality. Accessed 5 April 2011.
- 40.Fihn SD, McDonell M, Martin D, et al. Risk factors for complications of chronic anticoagulation: A multicenter study. Annals of Internal Medicine. 1993;118(7):511–520. doi: 10.7326/0003-4819-118-7-199304010-00005. [DOI] [PubMed] [Google Scholar]
- 41.Brooks F, Kendall S, Bunn F, Bindler R, Bruya M. The school nurse as navigator of the school health journey: Developing the theory and evidence for policy. Primary Health Care Research and Development. 2007;8:226–234. doi: 10.1017/S1463423607000278. [DOI] [Google Scholar]
- 42.Carroll JK, Humiston SG, Meldrum SC, et al. Patients' experiences with navigation for cancer care. Patient Education and Counseling. 2010;80:241–247. doi: 10.1016/j.pec.2009.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Druss BG, Marcus SC, Olfson M, Tanielian T, Pincus HA. Trends in care by nonphysician clinicians in the United States. The New England Journal of Medicine. 2003;348(2):130–137. doi: 10.1056/NEJMsa020993. [DOI] [PubMed] [Google Scholar]
- 44.Freeman H, Muth B, Kerner J. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Practice. 1995;3(1):19–30. [PubMed] [Google Scholar]
- 45.Robinson-White S, Conroy B, Slavish K, Rosenzweig M. Patient navigator in breast cancer: A systematic review. Cancer Nursing. 2010;33(2):127–140. doi: 10.1097/NCC.0b013e3181c40401. [DOI] [PubMed] [Google Scholar]
- 46.Unutzer J, Rubenstein L, Katon WJ, et al. Two-year effects of quality improvement programs on medication management for depression. Archives of General Psychiatry. 2001;58(10):935–942. doi: 10.1001/archpsyc.58.10.935. [DOI] [PubMed] [Google Scholar]
- 47.Dohan D, Schrag D. Using navigators to improve care of underserved patients: current practices and approaches. Cancer. 2005;104:848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 48.Seek A, Hogle W. Modeling a better way: Navigating the healthcare system for patients with lung cancer. Clinical Journal of Oncology Nursing. 2007;11(1):81–85. doi: 10.1188/07.CJON.81-85. [DOI] [PubMed] [Google Scholar]
- 49.Shockney L. Becoming a breast cancer nurse navigator. Sudbury: Jones and Barlett; 2011. [Google Scholar]
- 50.Ruland CM, Holte HH, Røislien J, et al. Effects of a computer-supported interactive tailored patient assessment tool on patient care, symptom distress, and patients' need for symptom management support: A randomized clinical trial. Journal of the American Medical Informatics Association. 2010;17(4):403–410. doi: 10.1136/jamia.2010.005660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bosworth H, Powers B, Oddone E. Patient self-management support: Novel strategies in hypertension and heart disease. Cardiology Clinic. 2010;28:655–663. doi: 10.1016/j.ccl.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Darkins A. Remote patient monitoring in home healthcare: Lessons learned from advanced users. Journal of Management and Marketing in Healthcare. 2009;2:238–252. [Google Scholar]
- 53.Darkins A. Care coordination/home telehealth: The systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemedicine Journal and e-Health. 2009;14:1118–1126. doi: 10.1089/tmj.2008.0021. [DOI] [PubMed] [Google Scholar]
- 54.Inglis, S., Clark, R., McAlister, G., et al. (2010). Structured telephone support or telemonitoring programs for patients with chornic heart failure. Cochrane Database Syst Rev. doi:10.1002/14651858.CD007228.pub2. [DOI] [PubMed]
- 55.Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: A randomized controlled trial. Diabetes Care. 2001;24(2):202–208. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 56.Wasson J, Gaudette C, Whaley F, Sauvigne A, Baribeau P, Welch H. Telephone care as a substitute for routine clinic follow-up. Journal of the American Medical Association . 1992;267(13):1788–1793. doi: 10.1001/jama.1992.03480130104033. [DOI] [PubMed] [Google Scholar]
- 57.Darkins A, Ryan P, Kobb R, et al. Care coordination/Home telehealth: The systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemedicine Journal and e-Health. 2009;14(10):1118–1126. doi: 10.1089/tmj.2008.0021. [DOI] [PubMed] [Google Scholar]
- 58.Piette JD, Weinberger M, McPhee SJ. The effect of automated calls with telephone nurse follow-up on patient-centered outcomes of diabetes care: a randomized, controlled trial. Medical Care. 2000;38(2):218–230. doi: 10.1097/00005650-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 59.Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? The American Journal of Medicine. 2000;108(1):20–27. doi: 10.1016/S0002-9343(99)00298-3. [DOI] [PubMed] [Google Scholar]
- 60.Piette J, Beard A. Automated telephone monitoring and behavior change calls (IVR). Interactive Health Communication Technologies: Promising strategies for health behavior change. (in press)
- 61.Piette J, Gregor MA, Share D, Heisler M, Bernstein S, Koelling T, Chan P. Improving heart failure self-management support by actively engaging out-of-home caregivers: results of a feasibility study. Congestive Heart Failure. 2008;14(1):12–18. doi: 10.1111/j.1751-7133.2008.07474.x. [DOI] [PubMed] [Google Scholar]
- 62.Heisler M (2006). Building peer support programs to manage chronic disease: seven models for success. pp. 1–41. http://www.chcf.org/topics/chronicdisease/index.cfm?itemID=127997. Accessed 4 May 2011.
- 63.Boothroyd RI, Fisher EB. Peers for progress: Promoting peer support for health around the world. Family Practice. 2010;27(Suppl 1):i62–i68. doi: 10.1093/fampra/cmq017. [DOI] [PubMed] [Google Scholar]
- 64.Fisher EB, Brownson CA, O'Toole ML, Anwuri VV. Ongoing follow-up and support for chronic disease management in the Robert Wood Johnson Foundation Diabetes Initiative. The Diabetes Educator. 2007;33(Suppl 6):201S–207S. doi: 10.1177/0145721707304189. [DOI] [PubMed] [Google Scholar]
- 65.Greden JF, Valenstein M, Spinner J, et al. Buddy-to-Buddy, a citizen soldier peer support program to counteract stigma, PTSD, depression, and suicide. Annals of the New York Academy of Sciences. 2010;1208:90–97. doi: 10.1111/j.1749-6632.2010.05719.x. [DOI] [PubMed] [Google Scholar]
- 66.Heisler M, Vijan S, Makki F, Piette JD. Diabetes control with reciprocal peer support versus nurse care management: A randomized trial. Annals of Internal Medicine. 2010;153(8):507–515. doi: 10.7326/0003-4819-153-8-201010190-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baksi AK. Experiences in peer-to-peer training in diabetes mellitus: challenges and implications. Family Practice. 2010;27(Suppl 1):i40–45. doi: 10.1093/fampra/cmp014. [DOI] [PubMed] [Google Scholar]
- 68.Travis J, Roeder K, Walters H, et al. Telephone-based mutual peer support for depression: A pilot study. Chronic Illness. 2010;6(3):183–191. doi: 10.1177/1742395310369570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Davis KL, O'Toole ML, Brownson CA, Llanos P, Fisher EB. Teaching how, not what: The contributions of community health workers to diabetes self-management. The Diabetes Educator. 2007;33(Suppl 6):208S–215S. doi: 10.1177/0145721707304133. [DOI] [PubMed] [Google Scholar]
- 70.Schopp LH, Hales JW, Quetsch JL, Hauan MJ, Brown GD. Design of a peer-to-peer telerehabilitation model. Telemedicine Journal and e-Health. 2004;10(2):243–251. doi: 10.1089/tmj.2004.10.243. [DOI] [PubMed] [Google Scholar]
- 71.Heisler M, Halasyamani L, Resnicow K, et al. “I am not alone”: The feasibility and acceptability of interactive voice response-facilitated telephone peer support among older adults with heart failure. Congestive Heart Failure. 2007;13(3):149–157. doi: 10.1111/j.1527-5299.2007.06412.x. [DOI] [PubMed] [Google Scholar]
- 72.Levine MD, Ross TR, Balderson BH, Phelan EA. Implementing group medical visits for older adults at group health cooperative. Journal of the American Geriatrics Society. 2010;58(1):168–172. doi: 10.1111/j.1532-5415.2009.02628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Heisler M, Piette JD. “I help you, and you help me”: Facilitated telephone peer support among patients with diabetes. Diabetes Educator. 2005;31(6):869–879. doi: 10.1177/0145721705283247. [DOI] [PubMed] [Google Scholar]
- 74.Kilbourne A, Flanders McGinnis G, Herbeck Belnap B, Klinkman M, Thomas M. The role of clinical information technology in depression care management. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33(1):54–64. doi: 10.1007/s10488-005-4236-0. [DOI] [PubMed] [Google Scholar]
- 75.Forster AJ, Clark HD, Menard A. Adverse events affecting medical patients following discharge from hospital. Canadian Medical Association Journal. 2004;170:3345–3349. [PMC free article] [PubMed] [Google Scholar]
- 76.Forster AJ, Murff HJ, Peterson JF, Ghandi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Annals of Internal Medicine. 2003;138:3161–3167. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 77.Gonseth J, Guallar-Castillon P, Banegas JR, Rodriguez-Artalejo F. The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: A systematic review and meta-analysis of published reports. European Heart Journal. 2004;25(18):1570–1595. doi: 10.1016/j.ehj.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 78.Kasper E, Gerstenblith G, Hefter G, et al. A randomized trial of the efficacy of multidisciplinary care in heart failure outpatients at high risk of hospital readmission. Journal of the American College of Cardiology. 2002;2002(39):471–480. doi: 10.1016/S0735-1097(01)01761-2. [DOI] [PubMed] [Google Scholar]
- 79.Forster AJ, Boyle L, Shojania KG, Feasby TE, Van Walraven C. Identifying patients with post-discharge care problems using an interactive voice response system. Journal of General Internal Medicine. 2009;24(4):520–525. doi: 10.1007/s11606-009-0910-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Boyd CM, Boult C, Shadmi E, et al. Guided care for multimorbid older adults. Gerontologist. 2007;47:697–704. doi: 10.1093/geront/47.5.697. [DOI] [PubMed] [Google Scholar]
- 81.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine. 2006;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 82.Corrigan JM, Martin JB. Identification of factors associated with hospital readmission and development of a predictive model. Health Services Research. 1992;27(1):81–101. [PMC free article] [PubMed] [Google Scholar]
- 83.Weissman JS, Ayanian JZ, Chasan-Taber S, Sherwood MJ, Roth C, Epstein AM. Hospital readmissions and quality of care. Medical Care. 1999;37(5):490–501. doi: 10.1097/00005650-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 84.Blaum CS, Cigolle CT, Boyd CM, Wolffe JL, Tian Z, Langa KM, Weir DR. Clinical complexity in middle aged and older adults with diabetes: The Health and Retirement Study. Medical Care. 2010;48(4):327–334. doi: 10.1097/MLR.0b013e3181ca4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Creswell JW, Clark VLP. Designing and conducting mixed methods research. Thousand Oaks: Sage Publications, Inc.; 2007. [Google Scholar]
- 86.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: A conceptual framework. Quality in Health Care. 1998;7(3):149–158. doi: 10.1136/qshc.7.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rogers E. Diffusion of innovations. 5. New York: Free Press; 2003. [Google Scholar]
- 89.Pettigrew A, Whipp R. Managing change and corporate performance. In: Cool K, Neven D, Walter I, editors. European industrial restructuring in the 1990s. New York: New York University Press; 1992. [Google Scholar]
- 90.Barnett P. Determination of VA health care costs. Medical Care Research and Review. 2003;60(Suppl. 3):124S–141S. doi: 10.1177/1077558703256483. [DOI] [PubMed] [Google Scholar]


