Abstract
This paper focuses on the process for adapting existing legacy computerized tailored intervention (CTI) programs and implications for future development of CTI to ensure that interventions can be disseminated and implemented in different settings. A significant amount of work is required to adapt existing CTI for new research applications and public health interventions. Most new CTI are still developed from scratch, with minimal re-use of software or message content, even when there are considerable overlaps in functionality. This is largely a function of the substantial technical, organizational, and content-based barriers to adapting and disseminating CTI. CTI developers should thus consider dissemination and re-use early in the design phase of their systems. This is not intended to be a step-by-step guide on how to adopt or disseminate research-tested CTI, but rather a discussion that highlights issues to be considered for adapting and disseminating evidence-based CTI.
Keywords: Computerized, Tailored, Research-tested, Evidence-based, Interventions, Dissemination, Implementation
BACKGROUND
The overarching goal of public health research and practice is to decrease the burden of diseases and improve population health. Chronic diseases such as cancer, diabetes, heart disease, and stroke are the leading cause of death and disability in the USA [18, 31]. The implementation of effective behavioral interventions represents a significant opportunity to prevent and control chronic diseases [9, 29]. Advances in preventing and controlling chronic diseases are currently limited by the failure to translate evidence-based behavioral interventions into practice [12]. Health promotion interventions are often designed and tested under “efficacy” conditions whereby investigators exert considerable control over factors such as intervention delivery and participant selection to minimize implementation variability and maximize internal validity [11, 13, 26]. Establishing efficacy is an important step in determining the potential public health value of an intervention. However, it is also necessary that the intervention has the potential for dissemination, adoption, implementation, and long-term maintenance (i.e., that the results be generalizable to other settings and populations), and that the intervention methods and strategies be compatible with stakeholder norms and system constraints so that interventions are maintained over time.
There is a substantial lag between discovery and adoption into practice due, in part, to the absence of effective systems to disseminate health innovations. Recognition of this limitation has been noted for many years [14, 15]. In 2000, Balas and Boren [1] reported that it takes about 17 years to apply/translate 14% of original, health-related research to the benefit of patient care. This limiting factor in controlling chronic diseases is compounded in racial-ethnic minorities, lower income, and underserved communities, which typically gain access to health-related innovations more slowly than other populations [32]. There has been insufficient attention to and resources for dissemination, especially for behavioral interventions. Unlike clinical or pharmaceutical interventions, there may often be a limited expectation that financial gain or cost savings can result from adoption of behavioral products and applications.
One category of behavioral interventions that has been found to be efficacious is tailored communication interventions. Tailored communications are formal individual communications in which the content and/or style of the materials have been created based on data specific to each individual and informed by health behavior theory. Computerized tailoring for health promotion (the focus of this paper) uses computer-based systems and algorithms to apply theories and principles of health behavior, communication, and social marketing to produce personally relevant health messages for participants. Providing individualized messages means the information can be particularly relevant, interesting, culturally appropriate, and credible to the message recipient [28].
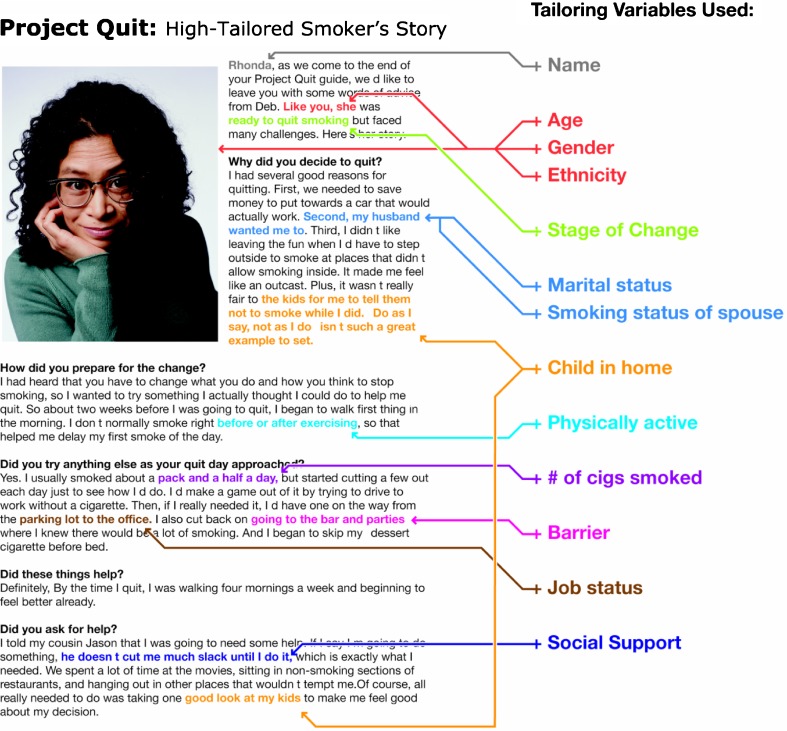
Review studies have concluded that tailored communications outperform generic communications for a variety of health behavior changes [6, 7, 22, 28]. The evidence demonstrates that computer-tailored interventions (CTI) are more likely to be effective than non-tailored communications because they provide personally relevant information that meets the needs of readers and largely excludes irrelevant or superfluous content [6, 27]. It follows that when these information needs are more closely met, an individual will be more likely to make desired changes in potential psychosocial indicators of behavior change. In most CTI, each individual’s data are used to match appropriate messages for an individual from a “library” of messages that can include text, graphics, photographs, audio or video information, or other formats. Each message is developed to address the demographic, health, behavioral, and/or psychosocial characteristics indicated by the presence of specific data values that have been chosen (based on formative research, previous studies, and/or clinical or behavioral science knowledge) as important for tailoring (i.e., potential mediators/moderators of behavior) [8, 17]. The messages are then turned into a single coherent communication by computer software that searches, selects, and assembles the messages based on matching rules (algorithms) (see Fig. 1).
Fig 1.
Example of computer-tailored intervention
The development of CTI can be resource intensive; however, once developed, they can be disseminated cost-effectively on a population basis. However, a significant amount of work is required to adapt a legacy CTI for a public health intervention or a new research application. This can present large barriers to dissemination. Because of the sizable effort involved in adapting a CTI at the technical, organizational, and intervention content levels, most new CTI are still developed from scratch, with little or no re-use of software or message content, even when there are considerable overlaps in functionality.
It is imperative for CTI developers to consider dissemination and re-use early in the system design phase. Table 1 presents the key challenges that should be addressed during CTI development to enhance their dissemination potential.
Table 1.
Challenges associated with dissemination of CTI
| Type of CTI | Challenges |
|---|---|
| Research-tested CTI | Not ready for dissemination without significant modifications |
| Reduce data collection | |
| Update/streamline software and user requirements | |
| Software no longer functional due to changes in technology and/or logistics | |
| Funding not provided in original grants for dissemination | |
| Funding difficult to obtain after research project has ended | |
| Proprietary CTI | Legal/ownership restrictions prevent broad dissemination/sharing |
| Designed to provide competitive advantage to company which inhibit sharing of technology | |
| Cost of CTI may prohibit broad adoption/dissemination |
Seeking partnerships with organizations that have an interest in disseminating CTI may help to mitigate this problem if the organizations are willing to invest in adaptation. In recent years, the National Institutes of Health and the Centers for Disease Control and Prevention and other agencies have awarded grants for dissemination and implementation research, representing a growing interest in dissemination and diffusion of evidence-based approaches and increased opportunities for developers of research-tested CTI.
One of the primary aims of this paper is to increase the dissemination of CTI by identifying the common processes necessary for modifying, recreating, and disseminating effective, research-tested CTI. The first section will focus on the process of adapting existing legacy programs. The second section focuses on development of CTI with an emphasis on designing for dissemination and implementation in diverse settings. This is not intended to be a step-by-step guide on how to adopt or disseminate research-tested CTI, but rather a discussion that highlights issues to be considered for adapting and disseminating evidence-based CTI.
PROCESS FOR ADAPTING LEGACY CTI
Research projects are designed and built to test various experimental conditions of an intervention for a specific audience. Dissemination of these interventions to larger, potentially more diverse populations offers both opportunities and challenges. Prior to broader dissemination of efficacious CTI, consideration should be given to a number of different factors (see Table 2).
Table 2.
Factors to consider when disseminating CTI
| 1. Characteristics of new target audience |
| 2. Program content modification/management |
| 3. Intervention implementation |
| 4. Data collection and ongoing program evaluation |
| 5. Ongoing operations and management |
Decisions regarding each of these factors will need to be sensitive to legal and regulatory issues that may apply differently in research vs. real-world settings.
Characteristics of the target audience
One of the first issues to examine when adapting CTI is the degree to which the participants in the original research trial resemble the new target audience in term of key behavioral, attitudinal, and socio-demographic characteristics. While by no means limited to CTI or behavioral health research, many efficacy trials are quite selective in their eligibility criteria, raising questions about the external validity of study findings. It is worth noting that CTI fare somewhat better in terms of external validity compared to generic or group-targeted behavioral interventions because, by definition, efficacious CTI are sensitive to individual characteristics that are related to successful behavior change. The process of individual tailoring should mitigate the potential impact of differences between the original study population and the new target audience as long as variables assessing these differences are part of the original tailoring algorithm. For example, if a CTI for smoking cessation provides feedback based upon an individual’s level of nicotine dependence, then differences in the level of nicotine dependence between the original study population and a new dissemination target audience likely would not pose as great a threat to the external validity of the intervention.
Content modification and management
Prior to dissemination of CTI, additional effort will also be needed to modify the health-related/health promotion message content in two main areas: (1) removal of research specific content, and (2) creation of new content to meet needs of the CTI adopter/provider and target audience.
Research-specific components of the message content perform functions for an efficacy trial, but may not be required when the CTI is later disseminated. Components to consider removing or modifying include study eligibility screening, informed consent, randomization, and content associated with the “control” condition in the original efficacy trial. If the original CTI tested multiple intervention factors (e.g., tailoring based upon different sets of important theoretical constructs), an optimized version of the CTI will need to be created for dissemination purposes. Effort needed to change underlying programming structure of the CTI to accommodate these changes should not be underappreciated.
Adoption of the CTI in a new setting and dissemination to a new target audience may also require the creation and management of new content. Potential adopters of CTI (e.g., health systems, health plans, public health agencies or non-profits) may wish to include information about their organizations or provide links to relevant institutional or localized resources. For example, a health plan when adopting a CTI for smoking cessation may want to provide specific content to members regarding coverage for medications to treat nicotine dependence. New content may also be required if the new target audience differs substantially from the population of the original efficacy trial. For instance, a clinical health system may wish to take a smoking cessation CTI that was developed for individuals who all smoked ten or more cigarettes per day and use it for all of their smoking patients (some of whom may smoke less than ten cigarettes per day). Substantial effort, expert assessment, potential new content development, and testing would be needed to ascertain that the CTI provided appropriate feedback to these new segments of the population. In the example given, this could include development of new content regarding recommendations to use (or not to use) pharmacological therapy tailored to each individual’s daily smoking rate.
The ongoing provision of a high quality CTI program may also require updates to general content areas. For example, if the original CTI made reference to news, current events, or public figures these portions of the content will require updating. Links to external services or resources would need to be monitored and updated. Changes in associated treatments practices (e.g., new recommendations or guidelines for cancer screening practices) would likely need to be included as well. It is important for adopters of CTI to carefully consider how much and how often content will need to be updated and develop a plan for meeting these needs. The original CTI may be more or less amendable to these updates. Depending on their needs and resources, organizations adapting CTI could also consider integration or addition of a formal content management system to the original program.
Intervention implementation
For interventions originally developed as part of an efficacy trial, delivery of a disseminated program may require significant changes in operations based on factors such as the scale and delivery/communication modality of the new program, the cost per individual served by the program, need for modification of program content and characteristics, variation in available resources, infrastructure, operating procedures, or culture in adopting organizations, and conforming to new technology platforms or systems.
In terms of the scale of the intervention, efficacy trials of CTI are designed and funded to handle a specific number of participants determined by the research aims. When the number of individuals receiving the intervention is relatively small (e.g., a few hundred or a few thousand), many processes may be adequately handled manually (e.g., mailing of notifications) that would not be feasible during large-scale dissemination (e.g., tens to hundreds of thousands or more). The delivery of research interventions can typically be engineered to a smaller scale, requiring fewer or less expensive technical infrastructure (e.g., computers, servers) and fewer support staff. Large-scale dissemination of a CTI may require re-engineering of technical systems for greater efficiency (e.g., adding network bandwidth and new servers), developing new automated systems or processes, or partnership with appropriate external service providers to meet demands for higher volume (hosting services, video and audio streaming, etc.).
The mode of intervention delivery during dissemination is also an important consideration and can have substantial implications for the costs of operation. An example of this would be the adaption of a print-based CTI for broader dissemination via the web. While this change may appear fairly straight-forward and offer substantial cost savings, these sorts of changes may require substantial re-engineering efforts.
Cost or logistical concerns related to larger scale dissemination of CTI may lead to modification of other program characteristics as well. In efficacy trials, financial or other incentives may be used to encourage adherence or ongoing engagement with the program. Continued provision of incentives may not be feasible or desirable from an organizational perspective during broader dissemination. Decisions may also need to be made regarding whether or not to retain ancillary intervention components (e.g., mailings that accompany a tailored online program), particularly when these ancillary components have more substantial cost per case.
The need for delivery or integration into new technical environments may have profound impact on the dissemination of CTI. For example, the adaption of a stand-alone research CTI for delivery within an electronic health record (EHR) can pose substantial challenges. Re-developing a CTI for a different technical environment may require changes in programming language, system architecture, data storage, and networking standards. Dissemination efforts such as these will likely require the original CTI to conform to new standards for security and safety. Likewise, the need for delivery or integration into new clinical environments may require changes in format and procedures to fit differing clinical imperatives.
Data collection and program evaluation
By their very nature, CTI involve the collection of data from individuals. While some data collection is necessary in order to drive the creation of tailored feedback, in research settings a great deal of other data is often collected to meet scientific aims (e.g., establish efficacy, understand intervention mechanisms). In the context of dissemination of CTI, data collection will be governed by the rules of the adopting organization rather than the research organization. Several considerations will likely influence data collection practices during dissemination of CTI programs. These include the general desire to streamline the user experience by reducing the amount of data collected to make the program quicker and easier to use, potential need to modify data collection to meet new eligibility requirements (e.g., membership in a particular health plan), adherence to organizational rules for collecting and storing individual identifiers, and adherence to organizational rules for security and confidentiality of participant data. Substantial re-design and re-programming of data collection processes (login/authentication, surveys, database storage, etc.) may be required to meet needs of CTI dissemination.
Dissemination of CTI also raises important questions regarding the role and need for ongoing program evaluation. One of the advantages of CTI is their high degree of consistency and fidelity. However, adopting organizations may consider including ongoing program evaluation to ensure that implementation and maintenance of the CTI is optimal. Program evaluation may be particularly valuable when dissemination of CTI involves delivery to a new audience that may not have been part of the original efficacy trial (i.e., a change in program eligibility), when there was a change in mode of the CTI as part of dissemination (e.g., a switch from print to online delivery), or other modifications to program characteristics (e.g., reduction or removal of incentives for participation). It is important to point out that CTI may generate a great deal of paradata (i.e., data about participant use of the program) that can play an important role assessing program operations.
Operations and management
In transitioning from a research focused to a disseminated intervention, many of the operation and management functions performed and provided by the original intervention will likely need substantial modification. It is likely that decisions regarding operations and management of CTI during dissemination will be driven by the availability of resources and infrastructure, new management strategies to support large-scale delivery, new technical environments, and new business environments. These concerns will influence specific choices, such as central hosting services vs. stand-alone programs, the level of technical support (tools and staff) for CTI adopters and end users, and how to handle ongoing program development, improvement, and version management. A business plan or other funding mechanism will be needed for ongoing support of CTI dissemination and adaption of the CTI to meet the varied needs of potential adopters.
Legal and regulatory considerations
It is critical that efforts to disseminate CTI adhere to relevant legal and regulatory codes. From the perspective of research and research institutions, it is important that intellectual property be protected (copyrights, trademarks, software licenses, patents, etc.). It is highly advisable that all individuals who significantly contributed to the development of the original CTI are made aware of its expanded usage and that they have agreed to the use of content over which they may have ownership.
In addition, broader dissemination of CTI (depending on the setting) may need to adhere to a broader set of regulations and standards that govern the use of health-related information. These include:
▪ Health Insurance Portability and Accountability Act (HIPAA) http://www.hhs.gov/ocr/privacy/
▪ Federal Information Processing Standards (FIPS) http://www.itl.nist.gov/fipspubs/
▪ Federal Information Security Management Act (FISMA) http://csrc.nist.gov/groups/SMA/fisma/index.html
▪ California Information Practice Act http://www.oispp.ca.gov/consumer_privacy/default.asp
▪ Americans with Disabilities Act (ADA) http://www.ada.gov/
▪ Financial Modernization Act of 1999, also known as the “Gramm–Leach–Bliley Act” http://www.ftc.gov/privacy/privacyinitiatives/glbact.html
For example, integration of a formerly free standing research CTI into a health system EHR will require consideration of HIPAA rules that may not have applied to the original application.
IMPLICATIONS FOR DEVELOPERS OF NEW SYSTEMS
Many design and implementation methodologies and tools have been developed to enhance the re-usability of software that can be used in CTI to reduce the costs associated with their eventual dissemination and adaptation.
Existing software toolkits for building CTI
Tailored interventions, like the individual counseling sessions they often mimic, are inherently complex, and codifying even a small subset of a counselor’s expertise in software is not easy. However, the payoff for doing so has potential for large public health impacts. Several software toolkits have now been developed that allow CTI to be more efficiently created and adapted, greatly broadening the potential pool of adopters. Depending on an adopter’s baseline skills and the complexity of the CTI they wish to create, the nature and intensity of the support required will vary. Some of the toolkits have extensive online training and help that may be sufficient for adopters to develop certain interventions. More complex CTI may require consulting or even contracting by experienced professionals or the toolkit developers themselves. What follows are examples of existing toolkits for building CTI.
Michigan Tailoring System
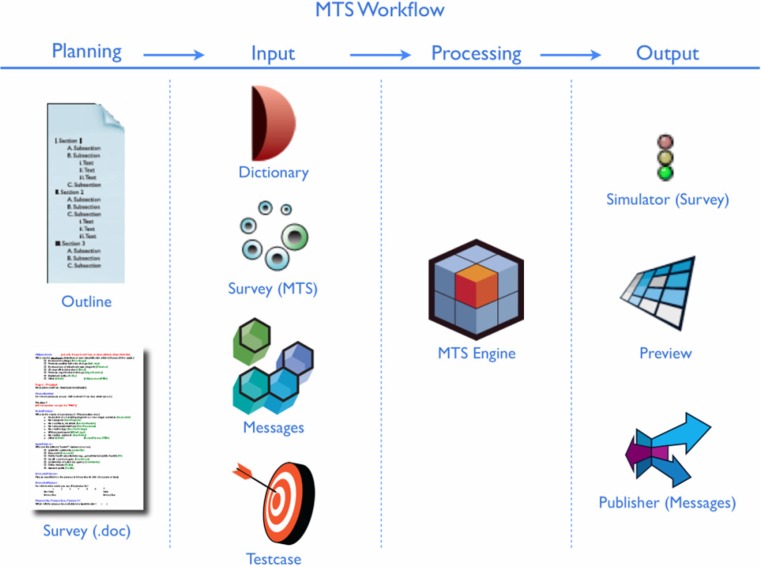
The Michigan Tailoring System (MTS) is an open-source software toolkit that enables the creation and delivery of tailored communications for print, web, mobile device, social networking application, or other delivery modes. The MTS Workbench design tool allows authors to write in-depth tailored messages, test them in real time, and see the results for a given individual, without the need for professional programmers. The MTS Engine runs behind the scenes and uses the logic defined by authors to select tailored text and media based on an individual’s characteristics. MTS comprises several key components (see Fig. 2).
Fig 2.
MTS workflow
In the Dictionary, authors define variables (e.g., gender, ethnicity, outcome expectancies) that will be used for tailoring. Authors use the Survey Editor to create online questionnaires that can be highly tailored and include skip patterns. These surveys may be previewed and tested in the Simulator. The Message Editor lets authors specify both the text and multimedia elements (photos graphics, audio, video, animation) to be used in the tailored messages. The Tailoring Engine uses information from the Dictionary and Message Editor to create individually tailored health messages. Authors can create a suite of Testcases (i.e., a mock participant) and use Previewer to review tailored message output in real time. The Publisher provides formatted tailored message output that is ready to be incorporated into a range of media channels (print, online, etc.). The MTS software program contains a robust array of built-in user help features: automated spell checking, logic checking, helpful error messages, and auto-complete (to aid in writing tailoring logic). MTS is scalable, uses a common technical platform, and interoperates with standard programming languages and web tools, resulting in CTI that are more easily disseminated. MTS was developed by the University of Michigan Center for Health Communications Research and is freely available to noncommercial entities for noncommercial education and research purposes. The toolkit and more information are available at: http://chcr.umich.edu/mts.
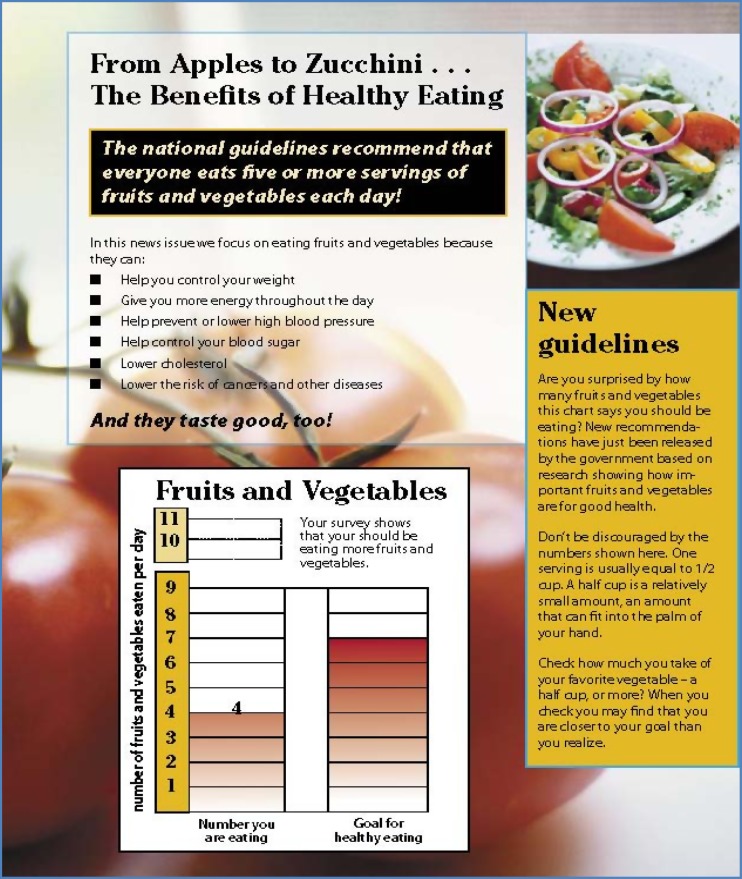
Tailortool
Tailortool is a software toolkit developed by the CHAI (Communications for Health Applications and Interventions) Core of the University of North Carolina at Chapel Hill. Tailortool enables the creation and delivery of tailored communications over the web that retains the integrity of print media for delivery in a newsletter format (see Fig. 3). This application generates intervention material such as individual feedback on targeted behavior(s) and uses variables such as relevant demographics, psychosocial factors, and barriers. Templates with various page lay-out possibilities allow individualization of the look and feel of the newsletters in terms of attributes such as format, graphics, colors, and story lengths. Messages are drawn from a library of text files of varying lengths depending on the needs of the intervention. Graphics can be imported into the various template pages. Newsletters can vary in length and can be personalized with names of participants. Following completion of an online survey, the newsletter(s) are dynamically and instantly created in pdf format for reading, printing, and/or saving by the participant. Each subsequent newsletter can be timed for release to fit the timeline of the intervention. From a technical perspective, the web application for the automated web-to-print system is programmed to run under a Windows operating system, using open-source software and a MS SQL database. The core of the system is a server-side application, with the website consisting of ASP pages (Active Server Pages), which interface with the application using XML. The backend application is heavily database-driven with everything from survey questions and skip patterns (i.e., which survey answers can cause later questions to be disabled, as described above; the actual disabling takes place client-side, with dynamically generated javascript code) to the newsletter content and tailoring logic stored in, and thus configurable via XML files. Participants’ survey-response data are stored in the database. The dynamic generation of the print newsletters in pdf format is done within the application using a dynamic-link library installed on the system.
Fig 3.
Example of print newsletter generated by TailorTool
The tool is available open source as a web application from Dr. Marci Campbell based at the University of North Carolina Chapel Hill (email—campbel7@email.unc.edu).
DTask and LiteBody
DTask is an open-source toolkit for building CTI deployed as dialogue systems, in which users have interactive “conversations” with the system [3, 10]. Telephone-based Interactive Voice Response (IVR) systems are one example of how DTask can be used. DTask is a dialogue planner designed to model and execute system-directed dialogue (for example, between health-related counselors and their patients), with multiple-choice user input. Dialogue is specified declaratively, as a hierarchical task decomposition, using a public standard task specification language [10, 25]. CTI for physical activity (walking) and fruit & vegetable promotion have been developed using this toolkit and are being released open source along with the toolkit. An example of a task specification is shown in Table 3, in which the high-level steps for conducting a counseling conversation are specified.
Table 3.
Example of task specification
| Task: conversation |
|---|
| Input parameters: behavior |
| Precondition: (applicable when session >1) |
| Steps: |
| 1. Opening |
| 2. RitualSocial |
| 3. ReviewTasks |
| 4. Assess |
| 5. Counseling |
| 6. Assign Tasks |
| 7. PreClosing |
| 8. Closing |
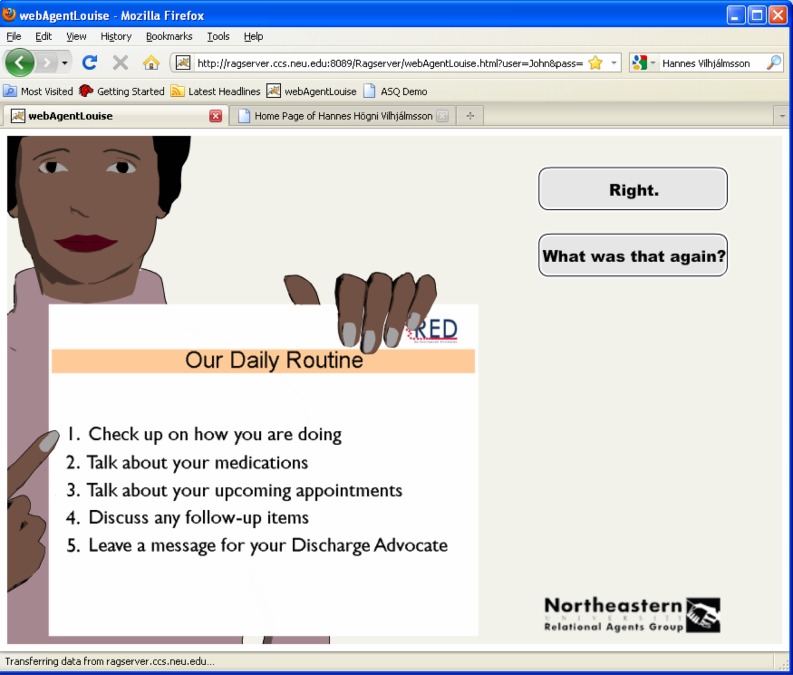
These include: (1) opening the conversation with a greeting; (2) conducting ritualized social dialogue, including small talk (e.g., about the weather) and inquiries into the patient’s general emotional and physical state (e.g., “how are you?”); (3) reviewing previously assigned behavioral tasks and goals (such as homework assignments or exercise goals); (4) assessing the patient’s current state in the intervention, such as stage of change and attitude toward the behavior; (5) conducting counseling based on the assessment (e.g., using Motivational Interviewing techniques); (6) negotiating new behavioral goals and tasks; (7) preparing to close the conversation (e.g., reviewing assignments and negotiating a next meeting time); and (8) delivering a farewell. There may be many such task decompositions specified for a given goal (e.g., counseling conversation templates such as the one in Fig. 4), and DTask decides moment-to-moment which to use based on many factors, such as tailoring parameters, patient characteristics, and what was said previously in the conversation.
Fig 4.
Screen shot of LiteBody user interface
DTask interoperates with LiteBody, a web-enabled user interface that presents users with an animated character they can converse with. LiteBody only requires that the Adobe Flash plug-in be installed on users’ computers (pre-installed on most contemporary browsers). The character speaks using synthetic speech and provides a range of conversational nonverbal behavior synchronized to speech, including: visemes, eyebrow raises, head nods, facial displays of emotion, posture shifts, gazing at and away from the user, and idle behavior (blinking, etc.). More information is available at: http://relationalagents.com/litebody.html.
VoiceXML
VoiceXML is a public standard specification language for defining telephone-based Interactive Voice Response (IVR) systems (see http://www.w3.org/TR/voicexml20/). Although there are no CTI-specific toolkits available, several commercial vendors provide general purpose toolkits that allow conversations to be defined and tested using visual design tools and minimal programming. Several vendors also provide IVR hosting services that can significantly simplify the deployment of IVR-based CTI.
Software development methodologies for developing new CTI
The field of software engineering has concerned itself with issues of software migration and adaptation as part of software maintenance, as well as software reusability, which in the context of CTI involves expending effort at the time a CTI system is first constructed so as to reduce the effort and cost of migration and adaptation to new settings.
Developers should follow standard practices in software engineering to address reusability, including:
- Cross-platform languages (e.g., Java)—these support rapid migration across supported platforms.
- ○ Modularity—support re-use of modules at different levels of abstraction: Parameterization, Functional abstraction, Object-Oriented Abstraction, Well-defined interfaces.
Public standard Application Programming Interfaces (APIs), and data and knowledge representation languages.
Quality documentation and good naming practices. This reduces time required for recipients of a system to understand how to modify it.
Future technologies to support CTI dissemination
Most software developers start from scratch when building new applications and designing unique data representations and this also holds true for most CTI systems developed to date. Unfortunately, this practice leads to significant problems in reusing, adapting, and disseminating CTI software across different settings and behaviors. For instance, the manner in which users are identified may vary significantly between systems, with one system using first and last name, another using a study-assigned identifier, and a third based on a user-specified account name. If each of these data structures could be tagged as “types” of user identification representations, then automatic translation among the various representations could be performed if the systems needed to exchange data, or if the system was originally based on first and last name and subsequently needed to be used in an environment in which user privacy protocols were important.
Computational ontologies represent one solution to these problems, by encouraging different developers (say, one who initially develops a CTI and one who wishes to adapt it for a new intervention) to use the same representations in their systems, or at least have a principled way to relate the representations in one system to the other.
An ontology is a formal representation of a set of concepts within a domain (such as “user” and “user identifier”), possibly including relationships among those concepts. Ontologies vary not only in their content but also in their structure and implementation. The level of description of a domain can range from lexicons or controlled vocabularies, to taxonomies where terms are related hierarchically and can be given distinguishing properties, to full-blown ontologies where these properties can define new concepts and where concepts have named relationships with other concepts [24, 30]. Although there has been a significant amount of work in the development of computational ontologies for biomedicine, e.g., the UMLS Metathesaurus and Semantic Network [20], there has been very little work on the development of public ontologies which encompass concepts in behavioral medicine or health communication. There are a few early efforts in this area; one of the more innovative being the National Cancer Institute’s Grid Enabled Measures (GEM) Database, which is essentially a social experiment on harnessing community intelligence to support the development of common behavioral science constructs and measures [2, 4, 19, 21, 23].
Future media
There is a wide range of new media that is currently being explored as deployment channels for CTI based on their potential to communicate with patients and consumers, including:
Computer Games (e.g., Wii Fit)
Mobile devices (messaging through email/SMS/Twitter)
Social Media (e.g., “Patients Like Me”)
Social Robots [16]
As new technologies emerge, the relevant factors related to adapting and disseminating research-tested CTI into practice will change.
CONCLUSION
Dissemination of efficacious CTI has a great potential to reduce the morbidity and mortality related to chronic diseases. While several aspects of CTI inherently lend themselves to effective dissemination (e.g., standardization, fidelity, relatively low incremental cost), adoption and implementation of CTI is not without significant challenges. Substantial planning, effort, and resources are often needed to transform an efficacious research CTI into a program that can be successfully disseminated. This process requires careful consideration of health behavior, technical, organization, business/financial, and legal and regulatory issues. Developers of new CTI for research and practice settings can simplify this process by planning for dissemination in the design of the original program. A variety of technical resources are now available to assist in the development of CTI. The potential of CTI to benefit the public health is highly likely to increase with the development of new technologies and systems to support dissemination of CTI and changing population norms and expectations regarding availability, access, and use of health individuals personal health information.
Footnotes
Implications
Practice: Computerized tailored interventions have been shown to be effective for preventing and controlling chronic disease, yet there has been a failure to translate these interventions from research into practice. This article describes a methodology for adapting these interventions for practice settings.
Policy: Resources should be directed toward efforts that directly address dissemination of computerized tailored interventions. These interventions should also be designed from the outset with eventual dissemination and re-usability in mind.
Research: Further research is needed to develop tools, methodologies, and shared resources, such as computational ontologies, to promote dissemination and re-use of computerized tailored interventions.
This paper is being submitted to TBM for the special section on “Information Technology and Evidence Implementation”.
Contributor Information
Cynthia Vinson, Email: cvinson@mail.nih.gov.
Timothy Bickmore, Email: bickmore@ccs.neu.edu.
David Farrell, Email: davidfarrellmail@peopledesigns.com.
Marci Campbell, campbel7@email.unc.edu.
Larry An, Email: lcan@umich.edu.
Ed Saunders, Email: saunders@umich.edu.
Mike Nowak, Email: mnowak@umich.edu.
Betsy Fowler, Email: beth_fowler@unc.edu.
Abdul R Shaikh, Email: shaikhab@mail.nih.gov.
References
- 1.Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearbook of medical informatics. Stuttgart: Schattauer; 2000. pp. 65–70. [PubMed] [Google Scholar]
- 2.Beveridge M, Fox J. Automatic generation of spoken dialogue from medical plans and ontologies. J Biomed Inform. 2006;39:482–499. doi: 10.1016/j.jbi.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Bickmore T, Giorgino T. Health dialog systems for patients and consumers. J Biomed Inform. 2006;39:556–571. doi: 10.1016/j.jbi.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Bickmore T, Sidner CL (2006) Towards plan-based health behavior change counseling systems. AAAI Spring Symposium on Argumentation for Consumers of Healthcare, Stanford, CA
- 5.Bickmore T, Gruber A, Picard R. Establishing the computer–patient working alliance in automated health behavior change interventions. Patient Educ Couns. 2005;59:21–30. doi: 10.1016/j.pec.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Brug J, Glanz K, Van Assema P, Kok G, van Breukelen GJP. The impact of computer-tailored feedback and iterative feedback on fat, fruit, and vegetable intake. Health Educ Behav. 1998;25:517–531. doi: 10.1177/109019819802500409. [DOI] [PubMed] [Google Scholar]
- 7.Brug J, Oenema A, Campbell M. Past, present, and future of computer-tailored nutrition education. Am J Clin Nutr. 2003;77:1028S–1034S. doi: 10.1093/ajcn/77.4.1028S. [DOI] [PubMed] [Google Scholar]
- 8.Campbell MK, DeVellis BM, Strecher VJ, Ammerman AS, DeVellis RF, Sandler RS. Improving dietary behavior: the effectiveness of tailored messages in primary care settings. Am J Public Health. 1994;84:783–787. doi: 10.2105/AJPH.84.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doll R, Peto R. The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States. JNCI. 1981;66:1191–1308. [PubMed] [Google Scholar]
- 10.DTask and LiteBody Open source, standards-based tools for building web-deployed embodied conversational agents. Lect Notes Artif Intell. 2009;5773:425–431. [Google Scholar]
- 11.Flay BR. Efficacy and effectiveness trials (and other phases of research) in the development of health promotion programs. Prev Med. 1986;15:451–474. doi: 10.1016/0091-7435(86)90024-1. [DOI] [PubMed] [Google Scholar]
- 12.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 13.Greenwald P, Cullen JW. The scientific approach to cancer control. CA Cancer J Clin. 1984;34:328–332. doi: 10.3322/canjclin.34.6.328. [DOI] [PubMed] [Google Scholar]
- 14.Harris JK, Luke DA, Zuckerman RB, Shelton SC. Forty years of secondhand smoke research the gap between discovery and delivery. Am J Prev Med. 2009;36:538–548. doi: 10.1016/j.amepre.2009.01.039. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine (2003) Crossing the quality chasm: a new health system for the 21st century. National Academy Press, Washington. Available at http://library.georgetown.edu/search/t?-Crossing+the+quality+chasm; http://0-site.ebrary.com.library.lausys.georgetown.edu/lib/georgetown/Doc?id-10056947
- 16.Kidd CD. Engagement in long-term human–robot interaction. Cambridge: MIT; 2007. [Google Scholar]
- 17.Kreuter MW, Oswald DL, Bull FC, Clark EM. Are tailored health education materials always more effective than non-tailored materials? Health Educ Res. 2000;15:305–315. doi: 10.1093/her/15.3.305. [DOI] [PubMed] [Google Scholar]
- 18.Kung HC, Hoyert DL, Xu JQ, Murphy SL (2008) Deaths: final data for 2005, vol. 56, no. 10. Centers for Disease Control and Prevention, Atlanta. Available at http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.pdf
- 19.Lenert L, Norman GJ, Mailhot M, Patrick K. A framework for modeling health behavior protocols and their linkage to behavioral theory. J Biomed Inform. 2005;38:270–280. doi: 10.1016/j.jbi.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Medicine NLo. MLS KNOWLEDGE SOURCES. 2004
- 21.Moser R, Hesse B, Shaikh AR, Courtney P, Morgan G, Augustson E (2010) The grid-enabled measures (GEM) database: a science 2.0 tool to facilitate the use of standardized measures and sharing harmonized data. AJPM (in press) [DOI] [PMC free article] [PubMed]
- 22.Neville LM, O’Hara B, Milat AJ. Computer-tailored dietary behaviour change interventions: a systematic review. Health Educ Res. 2009;24:699–720. doi: 10.1093/her/cyp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piazza M, Giorgino T, Azzini I, Stefanelli M, Luo R. Cognitive human factors for telemedicine systems. Stud Health Technol Inform. 2004;107:974–978. [PubMed] [Google Scholar]
- 24.Reviewing the design of {DAML+OIL} (2002) An ontology language for the semantic web
- 25.Rich C. Building task-based user interfaces with ANSI/CEA-2018. IEEE Computer. 2009;42:20–27. [Google Scholar]
- 26.Sallis J, Owen N, Fotheringham M. Behavioral epidemiology: a systematic framework to classify phases of research on health promotion and disease prevention. Ann Behav Med. 2000;22:294–298. doi: 10.1007/BF02895665. [DOI] [PubMed] [Google Scholar]
- 27.Skinner CS, Strecher VJ, Hospers H. Physicians’ recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1994;84:43–49. doi: 10.2105/AJPH.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Skinner C, Campbell M, Rimer B, Curry S, Prochaska J. How effective is tailored print communication? Ann Behav Med. 1999;21:290–298. doi: 10.1007/BF02895960. [DOI] [PubMed] [Google Scholar]
- 29.Straub RO. Health psychology. New York: Worth; 2002. [Google Scholar]
- 30.w3c. Web Ontology Language (OWL). Available at http://www.w3.org/2004/OWL
- 31.Wu SY, Green A. Projection of chronic illness prevalence and cost inflation. Santa Monica: RAND Health; 2000. [Google Scholar]
- 32.Young WWS, Marks SM, Kohler SA, Hsu AY. Dissemination of clinical results: mastectomy versus lumpectomy and radiation therapy. Med Care. 1996;34:1003–1017. doi: 10.1097/00005650-199610000-00003. [DOI] [PubMed] [Google Scholar]