Abstract
Aim
Our aim is to use ultrasound to non-invasively detect differences in choroidal microarchitecture possibly related to ischaemia among normal eyes and those with wet and dry age-related macular degeneration (AMD).
Design
Prospective case series of subjects with dry AMD, wet AMD and age-matched controls.
Methods
Digitised 20 MHz B-scan radiofrequency ultrasound data of the region of the macula were segmented to extract the signal from the retina and choroid. This signal was processed by a wavelet transform, and statistical modelling was applied to the wavelet coefficients to examine differences among dry, wet and non-AMD eyes. Receiver operating characteristic (ROC) analysis was used to evaluate a multivariate classifier.
Results
In the 69 eyes of 52 patients, 18 did not have AMD, 23 had dry AMD and 28 had wet AMD. Multivariate models showed statistically significant differences between groups. Multiclass ROC analysis of the best model showed an excellent volume-under-curve of 0.892±0.17. The classifier is consistent with ischaemia in dry AMD.
Conclusions
Wavelet augmented ultrasound is sensitive to the organisational elements of choroidal microarchitecture relating to scatter and fluid tissue boundaries such as seen in ischaemia and inflammation, allowing statistically significant differentiation of dry, wet and non-AMD eyes. This study further supports the association of ischaemia with dry AMD and provides a rationale for treating dry AMD with pharmacological agents to increase choroidal perfusion.
ClinicalTrials.gov registration
Keywords: Choroid, Macula, Degeneration, Treatment Medical, Imaging
Introduction
It is well established that macular degeneration is a multifactorial disease related to age, genetics and a host of environmental factors such as light exposure and smoking. Choroidal ischaemia is also well accepted as a causative factor, but its severity and prevalence have not been well documented because of the difficulty in imaging the choroid due to light absorption by the overlying retinal pigment epithelium (RPE).
While reduced function of the RPE and Bruch's membrane are generally regarded as anatomic points of inception of age-related macular degeneration (AMD), the choroid also plays an important role in AMD pathogenesis1 with some investigators, such as Friedman and Oat2 and Grunwald and coworkers,3 suggesting a primary role. Significant choroidal vascular alterations, such as changes in choriocapillaris density and volume and choroidal vessel diameter, have been reported both in ageing and AMD.4–6 Local inflammatory activity in the RPE–Bruch's membrane–choriocapillaris complex has also been described.1 7 8 Since these microvascular and regional inflammatory changes are difficult to detect in vivo, clinicians and researchers have sought imaging characteristics predictive of AMD onset or severity. Researchers have used fluorescein angiography, indocyanine green angiography, pulsatile ocular blood flow tonometry and Doppler flowmetry.9–11 Observed anatomic modifications could be accompanied by or even preceded by localised ischaemia.1 If microarchitectural choroidal changes that occur concomitantly with early clinical signs of AMD could be detected and documented, then applying early therapy could possibly arrest or interdict AMD progression.
Although advances in optical coherence tomography (OCT)12 13 allow imaging of retinal structures in great detail, adequate visualisation of the choroid has been challenging.14–17 Although enhanced depth imaging (EDI)-OCT can obtain measurements of choroidal thickness, it does not provide data regarding choroidal function. Ultrasonography circumvents the RPE's optical barrier, and while resolution at even as high a frequency as 20 MHz (75 µm axially) is modest in comparison with OCT, ultrasound echo waveforms are affected by the size and spatial distribution of subresolvable scattering elements.18 Regional vascular and other changes in the choroidal interstitium would be expected to significantly alter the reflective interfaces within the ultrasound beam, leading to a complex alteration of the waveform that can be detected using wavelet analysis techniques.
We hypothesise that information from wavelet statistical models may serve as imaging surrogates for vessel diameter, vessel density and extraluminal fluid in the choroid. In this study, our primary objective was to determine if significant differences exist among wavelet parameters of eyes without AMD, with dry AMD and with wet AMD.
Methods
This study was performed under a protocol approved by the Institutional Review Board of Weill Cornell Medical College. Written informed consent was obtained from the subjects.
This is a prospective case series of 69 eyes of 52 patients. Patients with AMD and age-matched patients without AMD were recruited in an academic retina practice (DJC) for fundus photography, OCT and indocyanine green (ICG) (in some patients) and high-resolution ultrasound in all patients. OCT and rarely ICG were only performed as part of treatment decision-making in wet and dry AMD, and not at all in the normal group. These data were not used for correlation with wavelet data, but instead were used clinically to aid in confirming the distinction between wet and dry AMD. We performed 20 MHz ultrasound scans on each eye using a B-scan immersion technique with a prototype instrument of our own design. Normal saline was used as the coupling medium, and the eyelids were held open with a Barraquer wire lid speculum. Phase-resolved (radiofrequency) echo data were digitised at a sample rate of 250 MHz with 8-bit precision.
We used a wavelet analysis technique which produces a time–frequency representation of the echo data. This allows addition of the property of shift invariance and gives superior identification of subresolvable information within the waveforms.
The data analysis began with segmentation of the macular retinal–choroidal area from the denoised B-scan19 20 using semiautomated methods.21 Independent components analysis (ICA) was then performed on echo data from the segmented region to obtain waveforms consisting of speckle and baseband components.22 Wavelet analysis23–25 was then applied to the ICA-processed data and summary statistics were calculated.26 27 A multivariate statistical technique was then used to identify wavelet coefficients and statistical structures differentiating eyes without AMD from those with dry AMD and those with wet AMD.28 29
Results
In all, 69 eyes of 52 patients were studied. A total of 18 did not have AMD, 23 had dry AMD and 28 had wet AMD.
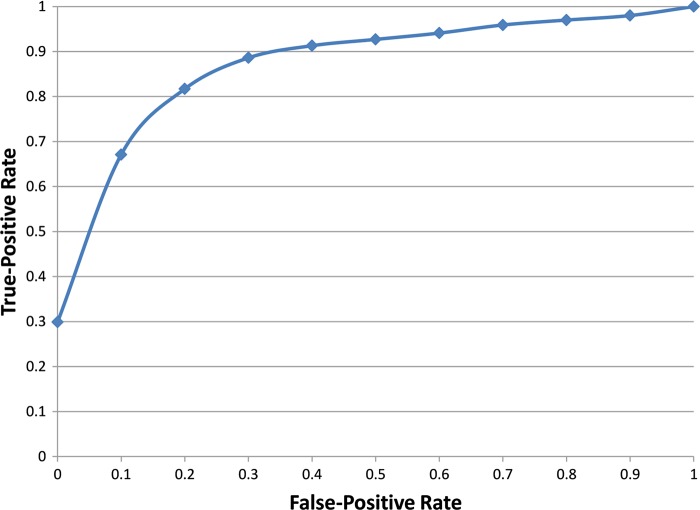
The multivariate model showed statistically significant differences for individual wavelet coefficients and wavelet covariance parameters between groups. One measure, interscale phase consistency, a parameter sensitive to tissue interfaces, separated the three subject groups by itself (figure 1). The optimal multivariate model included three wavelet parameters related to persistence and clustering of coefficients between scales and adjacent lateral B-scan line segments as well as the rate that coefficient magnitude decays over the scales. The model demonstrated excellent separation of the three classes and a volume under the multiclass receiver operating surface of 0.892±0.17 (figure 2).30 31
Figure 1.
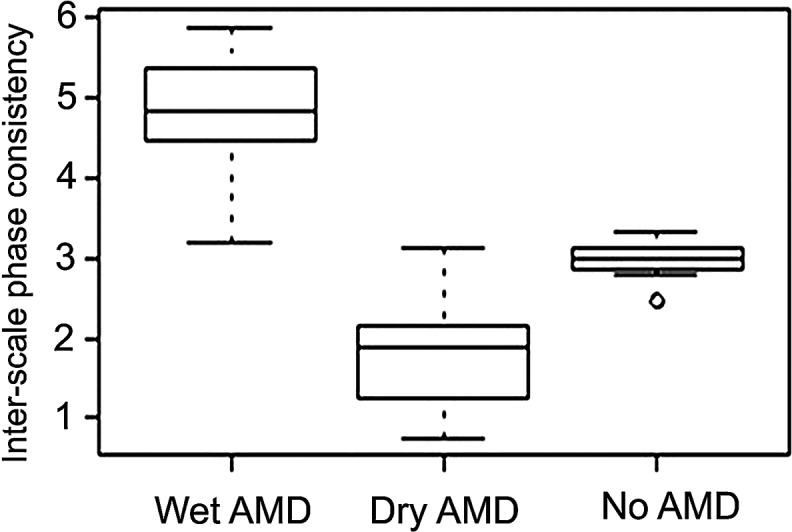
Boxplots showing distribution of interscale phase consistency, a wavelet-derived variable sensitive to fluid vessel wall boundaries, for non-age-related macular degeneration (AMD), dry AMD and wet AMD eyes. The relatively low value of this parameter in dry AMD indicates a reduction in the fluid wall boundaries (ischaemia) and an increase from normal in wet AMD.
Figure 2.
Multiclass receiver operating characteristic curve demonstrating performance of the multivariate classifier for separation of the three groups: normal, dry-age-related macular degeneration (AMD) and wet AMD. The volume under the surface was 0.892±0.17, indicative of excellent distinction among groups.
When applied to local echo data, the model can be used to produce wavelet images by performing successive and overlapping wavelet analyses centred on each pixel position using a sliding window. Such synthetic or hybrid ultrasound images show enhancement of contrast between fluid and tissue boundaries due to the differences in microarchitectural properties, as shown in figure 3. We term such images wavelet augmented ultrasound (WAU images) to differentiate them from conventional reflectance amplitude images. In figure 3, the hybrid image is superimposed on an ultrasound mid-band fit backscatter image which enhances boundary planes of the choroid, and like EDI-OCT studies, indicates thinning and irregularity of thickness in dry AMD eyes. These images demonstrate the data from which the interscale phase classifiers were derived.
Figure 3.
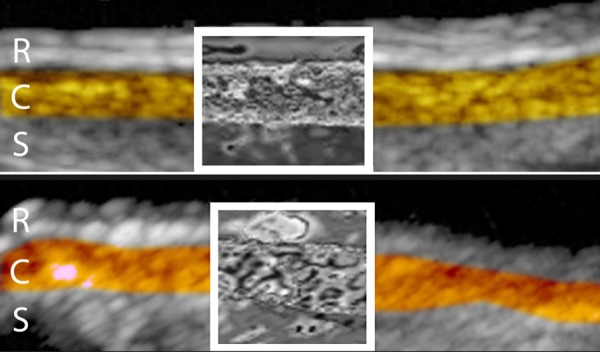
20 MHz ultrasound images of normal (top) and age-related macular degeneration (AMD) (bottom) eyes after semiautomated segmentation of retina (R), choroid (C) and sclera (S) as indicated by coloration. Wavelet processing was applied to the echo data encompassed by boxed regions. Note enhancement of druse in wavelet-processed area of AMD image. The choroid is more irregular in thickness in AMD than in normal eyes, as demonstrated here. These ‘hybrid’ or wavelet augmented ultrasound images demonstrate the use of classifiers such as interscale phase consistency.
Discussion
As demonstrated here, WAU tissue characterisation allowed distinction of the dry, wet, and non-AMD choroid. Our methodology used digitised raw ultrasound data32 which differs from standard ultrasound imaging by retaining phase information present in ultrasound waveforms, facilitating both Fourier and Wavelet signal processing. Wavelet analysis is advantageous compared with Fourier analysis as it localises functions in both time and frequency instead of frequency only and adds the property of shift invariance.25 33 These properties produce superior performance compared with Fourier methods in extraction of subresolvable information from echo waveforms.34 We conducted wavelet analysis of 20 MHz ultrasound data to determine and select descriptors most effective in distinguishing between normal eyes and wet and dry forms of AMD. Wavelet parameters were found to have significant classification power and may serve as biomarkers for assessing choroidal change in AMD.
Spectral-domain OCT allows choroidal thickness determination, as does ultrasound,35 and its representation of the choroidal microvasculature such in EDI-OCT12 is excellent. While OCT can now allow some visualisation of choroidal vasculature, no comparable analysis based on Wavelet or Fourier transforms has to-date been applied to OCT images of the choroid to differentiate wet, dry and non-AMD eyes. The methods described here may be applicable to such data as well. Our technique permits identification of a descriptor or classifier (ie, interscale phase consistency (ISCP)) that allows differentiation of wet, dry and non-AMD eyes based on choroidal ultrasound backscatter.
In dry AMD, the wavelet descriptors showed a reduction in boundary contrast (ie, decreased fluid to tissue ratio) when compared with the normal eye. This indicates choroidal ischaemia in dry AMD. In wet AMD, descriptors showed an increased boundary enhancement which could be caused by an enhanced blood supply or other causes such as inflammation or intrachoroidal microvascular anomalies.36 The ISCP clearly separated the normal, dry AMD and wet AMD eyes in this small series, based on the boundary ratios of fluid and tissue. The dry AMD separation can only be caused by ischaemia. The increased ratio of fluid to tissue in wet AMD could have many causes, including inflammation as suggested by Hageman et al8 or intrachoroidal microvascular anomalies as suggested by Fukushima et al36 and at this time can only be speculative. Future studies may be able to clarify the cause of the increased fluid to tissue ratio in wet AMD.
The genesis of RPE degeneration and choroidal neovascularisation in AMD is multifactorial, and is an open question. Is it primarily genetic or oxidative stress or ageing of the RPE itself or is it thickening of Bruch's membrane? Could all be related to ischaemia in the choriocapillaris and Sattler's layer of small arterioles? While the results of this study may not conclusively answer the question of causation of all AMD, and do not dispute genetics, oxidative stress or other factors, these results do confirm a principal correlation, if not causation, of dry AMD by choroidal dysfunction.
Our hypothesis, based on the results of this study and the findings of other investigators, is that ischaemia, primarily of Sattler's layer of the choroid, exists in all or nearly all cases of dry AMD. This smooth muscle endothelial dysfunction of the terminal arterioles would reduce the production of nitric oxide, a messenger molecule produced by the endothelium of the arterioles and choriocapillaris. This arteriolar damage may in turn be caused by parasympathetic neuronal deterioration37 38 as in erectile dysfunction and other arteriolar smooth muscle autonomic nerve-related diseases. Reiner and others39–42 have described the autonomic nerve relationship in the choroid in animal models. Fluid transfer between the choriocapillaris and the interstitial space of the retina would be based on the gradient of hydrostatic and osmotic pressure. Flower and coworkers43 have proposed that fluid transfer into the extracellular space around the RPE and removal of waste products may be governed by Starling's Law. These waste products (eg, drusen) and resultant toxic effects give rise to inflammation,11 7 vascular endothelial growth factor production and ultimately wet AMD. Our hypothesis would thus support a parasympathetic neuronal control of the terminal arterioles as a causative factor in reduced perfusion of the extracellular region surrounding the RPE. While other causes such as genetic predilection and/or oxidative stress are certainly present, RPE deterioration in AMD could thus be at least partly an effect rather than the sole direct cause of dry AMD, and ultimately wet AMD. The concept of parasympathetic choroidal perfusion regulation would relate pharmacological treatment of choroidal dysfunction to that of erectile dysfunction, another parasympathetic dystrophy for which a rich pharmacological data base is available.
Based on our results of ultrasonographic evidence of choroidal ischaemia in AMD and the results of EDI-OCT,44 45 we, like others,3 46 feel that pharmacological agents such as sildenafil, tadalafil, niacin or other agents that increase choroidal perfusion could have a beneficial effect on delaying or interdicting AMD. Choroidal perfusion measurements with swept scan ultrasound and OCT measurements of thickness offer a means of measuring and monitoring pharmacological therapy.44 45
Ultimately, longitudinal studies, including swept scan quantitative measurement of choroidal perfusion coupled with OCT, will be required to determine if reversing or moderating choroidal ischaemia will stabilise or interdict AMD. Such studies will also provide increased insight into the sequence of RPE change relative to the other parts of the tunica ruyschiana and more definitively determine not only the role of ischaemia as a primary causative factor of AMD but allow us to determine the role of pharmacological agents that could have a beneficial effect on the development and progression of AMD.
Footnotes
Contributors: Design and conduct of the study: DJC, RHS and RVPC; collection, management, analysis, and interpretation of the data: DJC, RHS, MJR, HOL and AAK; and preparation and review of the manuscript: DJC, RHS, MJR and HOL.
Funding: This study was supported in part by NIH grant 1R01EB000238, the Dyson Foundation, the St. Giles Foundation and Research to Prevent Blindness.
Competing interests: None.
Ethics approval: The study and data accumulation were carried out with prospective approval from the Weill Cornell Medical Center Institutional Review Board (IRB) (#0508008050) and was conducted in compliance with the tenets of the Declaration of Helsinki. Informed Consent for the research was obtained from the patients and the study is in accordance with HIPAA regulations.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zarbin MA. Current concepts in the pathogenesis of age-related macular degeneration. Arch Ophthalmol 2004;122:598–614 [DOI] [PubMed] [Google Scholar]
- 2.Friedman E, Oak SM. Choroidal microcirculation in vivo. Bibl Anat 1965;7:129–32 [PubMed] [Google Scholar]
- 3.Grunwald JE, Siu KK, Jacob SS, et al. Effect of sildenafil citrate (Viagra) on the ocular circulation. Am J Ophthalmol 2001;131:751–5 [DOI] [PubMed] [Google Scholar]
- 4.Ramrattan RS, van der Schaft TL, Mooy CM, et al. Morphometric analysis of Bruch's membrane, the choriocapillaris, and the choroid in aging. Invest Ophthalmol Vis Sci 1994;35:2857–64 [PubMed] [Google Scholar]
- 5.McLeod DS, Lutty GA. High-resolution histologic analysis of the human choroidal vasculature. Invest Ophthalmol Vis Sci 1994;35:3799–811 [PubMed] [Google Scholar]
- 6.Spraul CW, Lang GE, Grossniklaus HE. Morphometric analysis of the choroid, Bruch's membrane, and retinal pigment epithelium in eyes with age-related macular degeneration. Invest Ophthalmol Vis Sci 1996;37:2724–35 [PubMed] [Google Scholar]
- 7.Anderson DH, Mullins RF, Hageman GS, et al. A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol 2002;134:411–31 [DOI] [PubMed] [Google Scholar]
- 8.Hageman GS, Luthert PJ, Victor Chong NH, et al. An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-Bruch's membrane interface in aging and age-related macular degeneration. Prog Retin Eye Res 2001;20:705–32 [DOI] [PubMed] [Google Scholar]
- 9.Pauleikhoff D, Spital G, Radermacher M, et al. A fluorescein and indocyanine green angiographic study of choriocapillaris in age-related macular disease. Arch Ophthalmol 1999;117:1353–8 [DOI] [PubMed] [Google Scholar]
- 10.Chen SJ, Cheng CY, Lee AF, et al. Pulsatile ocular blood flow in asymmetric exudative age related macular degeneration. Br J Ophthalmol 2001;85:1411–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Metelitsina TI, Grunwald JE, DuPont JC, et al. Foveolar choroidal circulation and choroidal neovascularization in age-related macular degeneration. Invest Ophthalmol Vis Sci 2008;49:358–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spaide RF, Koizumi H, Pozonni MC. Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol 2008;146:496–500 [DOI] [PubMed] [Google Scholar]
- 13.Povazay B, Hermann B, Hofer B, et al. Wide field optical coherence tomography of the choroid in vivo. Invest Ophthalmol Vis Sci 2009;50:1856–63 [DOI] [PubMed] [Google Scholar]
- 14.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science 1991;254:1178–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drexler W, Morgner U, Ghanta RK, et al. Ultrahigh-resolution ophthalmic optical coherence tomography. Nat Med 2001;7:502–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wojtkowski M, Leitgeb R, Kowalczyk A, et al. In vivo human retinal imaging by Fourier domain optical coherence tomography. J Biomed Opt 2002;7:457–63 [DOI] [PubMed] [Google Scholar]
- 17.Khanifar AA, Koreishi AF, Izatt JA, et al. Drusen ultrastructure imaging with spectral domain optical coherence tomography in age-related macular degeneration. Ophthalmology 2008;115:1883–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coleman DJ, Silverman RH, Lizzi FL, et al. Ultrasonography of the eye and orbit. 2nd edn.: Philadelphia: Lippincott Williams & Wilkins, 2005 [Google Scholar]
- 19.Pan J, Guo Q, Jiang B. Spectra denoising based on the dual-tree complex wavelet transform. International Conference Audio, Language Image Proceedings; 2008:1121–5 [Google Scholar]
- 20.Serbes G, Aydin N. Denoising embolic Doppler ultrasound signals using dual tree complex discrete wavelet transform. Conference proceedings:... Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference; 2010:1840–3 [DOI] [PubMed] [Google Scholar]
- 21.Ben Salah M, Mitiche A, Ben Ayed I. Effective level set image segmentation with a kernel induced data term. IEEE Trans Image Proc 2010;19:220–32 [DOI] [PubMed] [Google Scholar]
- 22.Di L, Rao N, Kuo CH, et al. Independent component analysis applied to ultrasound speckle texture analysis and tissue characterization. Conference proceedings:... Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference; 2007:6524–7 [DOI] [PubMed] [Google Scholar]
- 23.Chaux C, Duval L, Pesquet J-C. Image analysis using Dual-Tree M-Band Wavelet Transform. IEEE Trans Image Proc 2006;15:2397–412 [DOI] [PubMed] [Google Scholar]
- 24.Bayram I, Selesnick W. A simple construction for the M-Band Dual-Tree Complex Wavelet Transform. 12th IEEE Digestive Sig Proceeding Workshop 2006:596–601 [Google Scholar]
- 25.Selesnick IW, Baraniuk RG, Kingsbury NC. The dual-tree complex wavelet transform. Sig Proc Mag, IEEE 2005;22:123–51 [Google Scholar]
- 26.Chaux C, Pesquet J-C, Duval L. Noise covariance properties in dual-tree wavelet decompositions. IEEE Trans Inf Theory 2007;53:4680–700 [Google Scholar]
- 27.Rakvongthai Y, An Vo, Oraintara S. Complex Gaussian scale mixtures of complex wavelet coefficients . IEEE Trans Sig Proc 2010;58:3545–56 [Google Scholar]
- 28.Akaike H. A new look at the statistical model identification. IEEE Trans Auto Contr 1974;19:716–23 [Google Scholar]
- 29.Rindskopf D. Fitting multinomial models in R: A Program Based on Bock’s Multinomial Response Relation Model. In: Vinod HD, ed. Advances in Social Science Research Using R. New York: Springer, 2010:167–77. [Google Scholar]
- 30.Nakas CT, Yiannoutsos CT. Ordered multiple-class ROC analysis with continuous measurements. Statist Med 2004;23:3437–49 [DOI] [PubMed] [Google Scholar]
- 31.Everson R, Fieldsend J. Multi-class ROC analysis from a multi-objective optimisation perspective. Pattern Recog Lett 2006;27:918–27 [Google Scholar]
- 32.Coleman DJ, Silverman RH, Chabi A, et al. High-resolution ultrasonic imaging of the posterior segment. Ophthalmology 2004;111:1344–51 [DOI] [PubMed] [Google Scholar]
- 33.Kingsbury N. Complex wavelets for shift invariant analysis and filtering of signals. J Appl Comp Harm Anal 2001;10:234–53 [Google Scholar]
- 34.Zhang GM, Braden DR, Harvey DM, et al. Acoustic time-frequency domain imaging. J Acoust Soc Am 2010;128:EL323–8 [DOI] [PubMed] [Google Scholar]
- 35.Coleman DJ, Lizzi FL. In vivo choroidal thickness measurement. Am J Ophthalmol 1979;88:369–75 [DOI] [PubMed] [Google Scholar]
- 36.Fukushima I, McLeod DS, Lutty GA. Intrachoroidal microvascular abnormality: a previously unrecognized form of choroidal neovascularization. Am J Ophthalmol 1997;124:473–87 [DOI] [PubMed] [Google Scholar]
- 37.Hodos W, Miller RF, Ghim MM, et al. Visual acuity losses in pigeons with lesions of the nucleus of Edinger-Westphal that disrupt the adaptive regulation of choroidal blood flow. Vis Neurosci 1998;15:273–87 [DOI] [PubMed] [Google Scholar]
- 38.Fitzgerald MEC, Jackson B, Cuthbertson SL, et al. Anatomical and functional evidence for progressive age-related decline in parasympathetic control of choroidal blood flow in pigeons. Exp Eye Res 2005;81:478–91 [DOI] [PubMed] [Google Scholar]
- 39.Reiner A, Li C, Del Mar N, et al. Choroidal blood flow compensation in rats for arterial blood pressure decreases is neuronal nitric oxide-dependent but compensation for arterial blood pressure increases is not. Exp Eye Res 2010;90:734–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fitzgerald MEC, Tolley E, Frase S, et al. Functional and morphological assessment of age-related changes in the choroid and outer retina in pigeons. Visual Neurosci 2001;18:299–317 [DOI] [PubMed] [Google Scholar]
- 41.Jablonski MM, Iannaccone A, Reynolds DH, et al. Age-related decline in VIP-positive parasympathetic nerve fibers in the human submacular choroid. Invest Ophthalmol Vis Sci 2007;48:479–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fitzgerald MEC, Cuthbertson SL, Hodos W, et al. Anatomical and functional evidence for progressive age-related decline in parasympathetic control of choroidal blood flow in pigeons. Exp Eye Res 2005;81:478–91 [DOI] [PubMed] [Google Scholar]
- 43.Flower RW, von Kerczek C, Zhu L, et al. Theoretical investigation of the role of choriocapillaris blood flow in treatment of subfoveal choroidal neovascularization associated with age-related macular degeneration. Am J Ophthalmol 2001;132: 85–93 [DOI] [PubMed] [Google Scholar]
- 44.Vance SK, Imamura Y, Freund KB. The effects of sildenafil citrate on choroidal thickness as determined by enhanced depth imaging optical coherence tomography. Retina 2011;31:332–5 [DOI] [PubMed] [Google Scholar]
- 45.Kim DY, Silverman RH, Chan RVP, et al. Measurement of choroidal perfusion and thickness following systemic sildenafil (Viagra®). Acta Ophthalmologica 2012;10:1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berenberg TL, Metelitsina TI, Madow B, et al. The association between drusen extent and foveolar choroidal blood flow in age-related macular degeneration. Retina 2012;32:25–31 [DOI] [PMC free article] [PubMed] [Google Scholar]