ABSTRACT
The objective of this study is to identify sociodemographics of older adults enrolled in a nationally disseminated evidence-based fall risk reduction program, describe different delivery sites, and examine personal and site characteristics associated with intervention adherence. Data were analyzed from 6,922 older adults enrolled in A Matter of Balance/Volunteer Lay Leader (AMOB/VLL) model between 2006 and 2009. Intervention dosage was measured by workshop attendance. Logistic regression analyses examined factors associated with attendance levels. Intervention dosage differed by sociodemographic and delivery site characteristics. Patterns of intervention dose significantly differed between Hispanic and non-Hispanic White participants. Those with less education and living in rural areas were more likely to receive adequate program doses. Although senior services agencies offered the most programs, intervention adherence was more likely in nonaging service sites. Findings may help program administrators better understand and minimize attrition issues within their AMOB/VLL workshops.
KEYWORDS: Fall prevention, Community-based interventions, Evidence-based programs, Older adults, Program adherence, Fall risk reduction program
INTRODUCTION
Falls are a major public health problem with severe physical, psychological, and economic consequences [1, 2]. And, with the rapid aging of the American population, falls will continue to be in the forefront of health issues facing older adults [3]. Falls are often the beginning of a downward trajectory among older adults with direct treatment costs estimated to reach over $50 billion annually by 2020 [4].
Currently, there is a greater attention to the importance of integrated models that address the multiple determinants of falls and the variety of intervention approaches which link clinical and community efforts [5]. In addition to better characterizing clinical, behavioral, and environmental risk factors for falling and fall-related injuries [2], recent research is demonstrating the preventability of falls. Also, there is a growing compendium of evidence-based fall prevention and fall risk reduction programs with proven efficacy for eliminating risk factors for older adults at risk for falling [6].
Despite the availability of evidence-based programs, there are often numerous factors that impact research to practice dissemination in the community [7]. An initial critical element in falls and fall risk reduction programs is building an infrastructure for delivering evidence-based programs that go beyond research studies to community settings where older adults reside, seek health care, and engage in recreational and social activities [8]. A second critical element to accelerating program implementation is recruiting older adults in evidence-based programs by addressing traditional stereotypes that older frail adults cannot benefit from health promotion/disease prevention programs [9]. In addition, program developers carefully consider the intervention dosage or number of programmatic sessions necessary to achieve hypothesized effects [10, 11]. Thus, a third critical element is retaining participants in the programs to ensure they are exposed to the essential elements of the program, thus increasing the likelihood of obtaining and retaining intended benefits [11]. Studies point to the importance of multiple intervention strategies coupled with adherence to essential programmatic activities for achieving optimal outcomes [12, 13]. Yet, from real world experience, we know that expecting participants to attend all recommended class sessions is often unrealistic, as “life happens.” What we do not know is who is likely to complete a fall prevention program and/or attend all offered sessions to receive the maximum intervention dose.
The implications of the effects of various delivery channels have also not been systematically studied, even though there is a growing training and delivery infrastructure for various community-based falls prevention/falls risk reduction programs for older adults [6, 14–16]. Understanding the delivery infrastructure of evidence-based program dissemination efforts in community settings can inform program developers and deliverers about issues with participant retention and attrition, which has implications for maximizing health outcomes, improving quality care, and saving scarce resources. The purposes of this study were to (1) identify sociodemographics of older adults who enrolled in A Matter of Balance/Lay Leader model (AMOB/VLL), a nationally delivered evidence-based fall risk reduction program, (2) describe characteristics of delivery site types in which program participants attended the community-based intervention, and (3) examine personal and delivery site characteristics associated with intervention intensity based on attendance levels: “inadequate intervention dose,” “adequate intervention dose,” and “complete intervention dose.”
METHODS
AMOB/VLL
A Matter of Balance, a group-based program built upon the application of social cognitive learning principles, is intended to reduce the fear of falling and improve health indicators associated with the risks of falling. The program also incorporated exercises appropriate for older adults of varying functioning levels. The effectiveness of A Matter of Balance was first documented in a randomized trial in which program content was delivered by health-care professionals [17]. A Matter of Balance has since been adapted to be widely disseminated in diverse community settings by lay leaders rather than professionals, and as a modified program, it is called, “A Matter of Balance/Volunteer Lay Leader model (AMOB/VLL)” [18]. AMOB/VLL has been recognized as an evidence-based fall risk reduction program for older adults [19, 20]. Hence, AMOB/VLL does not specifically target clinical outcomes such as falls; rather, it focuses on reducing fall-related risk factors by addressing attitudes and behaviors that predispose older adults to falls. This modified version of the program is the focus of the current study (see http://www.mmc.org/mh_body.cfm?id=432 for more information).
As indicated in Table 1, the program includes eight 2-hour sessions, which are typically held over an 8-week period. The program goal is to reduce fall-related disability by instilling greater confidence in one’s abilities to prevent or manage falls while simultaneously increasing physical activity to counterbalance and gait deficits [16]. Trained volunteer lay leaders facilitate each workshop using a uniform training manual and instructional videos [21]. Earlier workshop sessions are designed to diminish the fear of falling and promote the mentality that falls are preventable. Later workshop sessions encourage participants to modify their environments to reduce fall-related risk factors and increase strength and balance through structured exercises [21, 22]. The AMOB/VLL curriculum includes lectures, group discussions, problem-solving strategy planning and activities, role-play activities, physical activity training, assertiveness training, and home assignments [23].
Table 1.
AMOB/VLL topics, objectives, and resources by session
| Session | Topics | Objectives | Resources |
|---|---|---|---|
| 1 | Introduction to the program | • Identify helpful and unhelpful fall beliefs | • Group meeting schedule |
| • Fall-related attitudes survey | |||
| • Video: fear of falling | |||
| 2 | Exploring thoughts and concerns about falling | • Recognize core beliefs about falls | • Evaluating thoughts about falling |
| • Challenge unhelpful thoughts through the use of cognitive restructuring | • Challenge your concerns about falling | ||
| 3 | Introduction to exercise and fall prevention | • Understand the role of exercise in fall prevention | • Age page: exercise: getting fit for life |
| • Identify barriers to exercise and exercises suited to preventing falls | • AMOB/VLL exercises | ||
| • Participate in the AMOB/VLL exercises | • Video: exercise it’s never too late | ||
| 4 | Assertiveness and fall prevention | • Identify physical risk factors for falls | • AMOB/VLL exercises |
| • Practice exercises that address physical risk factors | • Age page: preventing falls and fractures | ||
| • Relevance of assertive behavior and fall prevention | • Prevention of falls: some practical suggestions | ||
| • Resources for fall prevention | |||
| 5 | Managing concerns about falling | • Learn to use personal action planners | • AMOB/VLL exercises |
| • Recognize effect of thoughts about falls on feelings and action | • Personal action planner for exercise | ||
| • Improving your balance | |||
| • No fall-ty habits | |||
| 6 | Recognizing fall-ty habits | • Evaluate fall risk-taking behaviors | • AMOB/VLL exercises |
| • Prioritize risk-taking behaviors to be addressed | • Recognizing and changing fall-ty habits | ||
| • Identify thoughts that help to change behavior | • Home safety check list | ||
| • Learn ways to shift from negative to positive or helpful thinking | |||
| 7 | Recognizing fall hazards in the home and community | • Recognize potential fall hazards in home and community | • AMOB/VLL exercises |
| • Identify strategies to reduce physical hazards in the home and community | • Personal action planner for an environmental hazard | ||
| • Recognize relationship between assertive behavior and fall prevention | • Solutions to fall hazards in the home | ||
| • Getting up and down safely | |||
| 8 | Practicing no fall-ty habits and overview | • Recognize the benefits of a positive attitude toward fall prevention | • Personal action planner for behavior |
| All | Intervention formats | Video presentation, brain storming, guest therapist, individual survey, exercise routine, small group work, group discussion, problem solving, personal experience, group survey, role playing | |
AMOB/VLL has been shown to significantly improve health outcomes including fall-related efficacy, physical and mental health, and activity limitations [14, 24–28]. And, in a previous study in Texas, participants who received a complete dose of the program (i.e., attended all workshop sessions) reported more health-related improvements relative to their counterparts who attended fewer workshop sessions [25]. Compared to participants who attended between five and seven AMOB/VLL workshop sessions, those who attended all eight sessions reported significantly fewer days limited from usual activity and significantly greater falls efficacy scores [25].
Participants and procedures
Recognizing the rise in chronic disease rates impacting older adults in the United States (e.g., cardiovascular disease, diabetes, cancer, arthritis, and other musculoskeletal conditions), the U.S. Administration on Aging (AoA) began supporting the translation of Evidence-Based Disease and Disability Prevention (EBDDP) programs, including AMOB/VLL, by eldercare service providers in 2003. The success of these pilot results encouraged AoA to expand their initiative to award $22 million from 2006 to 2009. These funds were further leveraged with an additional $20 million to support the replication of evidence-based programs in 27 states. This funding stream supported delivery infrastructure development for AMOB/VLL and other evidence-based prevention programs, which serves older adults in a variety of venues (e.g., senior centers, senior housing, health-care, and faith-based organizations). AoA led this EBDDP initiative in partnership with the Centers for Disease Control and Prevention (CDC), Agency for Healthcare Research and Quality, Centers for Medicare and Medicaid Services, Health Resources and Services Administration, Substance Abuse and Mental Health Services Administration, and private foundations. The current study utilizes data from this nationwide dissemination of AMOB/VLL.
In the 3-year time period of EBDDP dissemination described above, AMOB/VLL was delivered in 14 states to 12,219 older adults nationwide. Participants were recruited to the program primary through local Area Agencies on Aging (AAA) and other community-based organizations. Each delivery site was responsible for collecting data using standardized forms to document participant-level data about sociodemographics, attendance (i.e., using attendance roster administrative forms utilized by the program deliverers), and AMOB delivery site information. Deidentified data from each state were then sent to Senior Services in Seattle. Senior Services personnel performed data quality checks and cleaned the data to ensure all data were complete, values were valid, and key fields crossmatched correctly. Data errors were shared with the state data managers for correction. Due to missing data for key sociodemographic variables, our analytic sample includes a total of 6,922 AMOB/VLL participants. Institutional Review Board approval was obtained at Texas A&M University for this secondary data analysis.
Measures
To assess factors associated with the intensity of intervention exposure to AMOB/VLL participants (i.e., program attendance), we included two types of variables: self-reported sociodemographics of the participants measured at program enrollment (i.e., measures required by the National Council on Aging for uniform interstate reporting purposes) and delivery site characteristics. Figure 1 highlights our conceptual framework linking personal and delivery site characteristics and intervention intensity indicators to program outcomes and public health impacts. Variables in the blackened boxes indicate those directly included in the current study. Intervention processes are designed to improve falls risk awareness, enhance behavioral skills, reduce environmental barriers, and provide opportunities to engage in classroom exercises. The short-term goals are to improve fall-related efficacy, increase physical activity, and reduce health interference, which lead to intermediate goals of reduced functional impairment, fall incidence, activity limitations, and disability with the ultimate goal of reducing health-care costs and improving population health.
Fig 1.
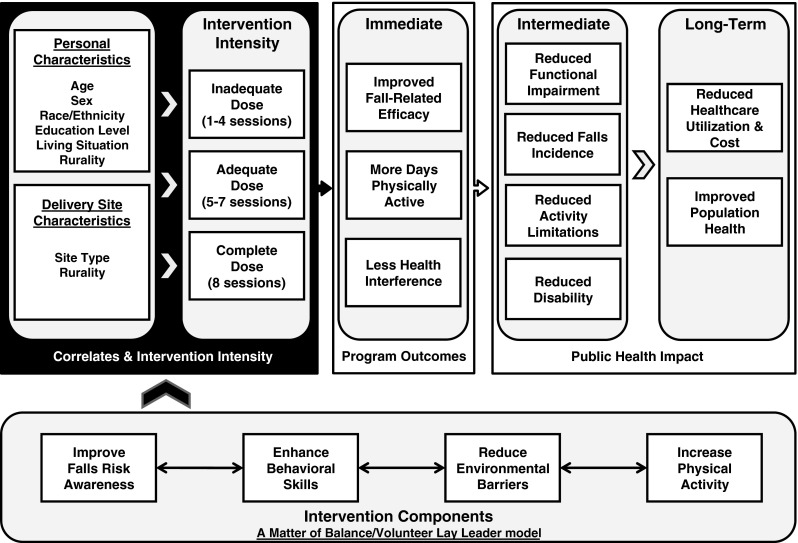
Conceptual framework linking correlates and intervention intensity to program outcomes and public health impacts
Dependent variables
AMOB/VLL attendance patterns were used as the dependent variables in this study. Program developers have defined the recommended attendance in which participants should receive intended program effects [16]. “Adequate dose” of the program is defined as attending five or more of the eight class sessions (i.e., attending fewer than five class sessions is defined as “inadequate dose”). This attendance recommendation is based on theoretical principles that have been translated to practitioner guidelines pertaining to the ideal intervention exposure needed for desired group dynamics and participant–lay leader interactions. A previous study examining the role of class attendance on health-related outcomes among AMOB/VLL participants reported a positive association between levels of program attendance and improvement in health-related outcomes [25]. As such, attendance was examined in two ways: inadequate dose compared to adequate dose (i.e., attended between one and four class sessions, attended between five and eight sessions) and complete dose among those who received an adequate dose (i.e., attended between five and seven class sessions, attended all eight sessions).
Sociodemographics
Participant sociodemographics included age group (i.e., 50–64, 65–74, 75–84, 85+ years), sex, race/ethnicity (i.e., non-Hispanic White, Hispanic, African-American, American Indian or Alaska Native, other/multiple races), the highest level of education received by the participant (i.e., less than high school, graduated high school, more than a high school education), and living situation (i.e., live alone, live with others). Using participants’ residential ZIP codes, geographic information system (GIS) software was used to generate neighborhood-level rurality categories for each participant (i.e., metro (urban) or nonmetro (rural) based on the Rural-Urban Commuting Area Codes (RUCA).
Delivery site characteristics
Data pertaining to AMOB/VLL delivery site types were gathered administratively, as previously described. Participant cases attending the six most prevalent delivery site types were compared in these analyses: senior centers or AAA, residential facilities, health-care organizations, community or multipurpose centers, faith-based organizations, and parks and recreation facilities. Participants attending AMOB/VLL at any other delivery site types were omitted because of the inadequate number of cases attending workshops at these site types. The following delivery site types were omitted from analyses: workplace settings (n = 70, 0.9 %) and municipal government (n = 17, 0.2 %). Further, delivery sites categorized as “other” (n = 366, 4.8 %) were omitted because of the potential difficulty to interpret findings associated with this delivery site type. Using organizational ZIP codes, GIS software was used to generate neighborhood-level rurality categories for each delivery site (i.e., metro (urban) or nonmetro (rural) based on the RUCA.
Statistical analyses
All statistical analyses were performed using SPSS (version 17). Frequencies were calculated for all major study variables, which were initially examined in relationship to participants’ receipt of an adequate intervention dose (i.e., yes, no) and participants’ receipt of a complete intervention dose among those who received an adequate dose (i.e., yes or no). Pearson’s chi-square tests were performed to assess the independence between dependent variable and categorized independent variables. Binary logistic regression analysis was used to identify sociodemographics and delivery site characteristics associated with receiving an adequate dose of the program (i.e., attending between one and four sessions served as the referent group). Then, after omitting those who received an inadequate dose, another binary logistic regression was conducted to examine how sociodemographics and delivery site characteristics were associated with receiving a complete intervention dose among those who attended five or more workshop sessions (i.e., attending between five and seven sessions served as the referent group).
RESULTS
Sample
Sample characteristics of study participants are presented in Table 2. Of the 6,922 study participants, 80.2 % of the AMOB/VLL participants attended five or more workshop sessions. Approximately 41 % of the participants attended workshops delivered at senior centers or AAA, 29.8 % at residential facilities, 11.1 % at community or multipurpose centers, 8.4 % at faith-based organizations, 6.1 % at health-care organizations, and 3.7 % at parks and recreation facilities. Approximately 88 % of the participants attended workshops delivered in urban areas. When examining participant sociodemographics, the majority of the participants was 75 years or older (66.3 %), female (82.2 %), non-Hispanic White (75.0 %), had more than a high school education (58.5 %), and resided alone (56.8 %). Over 86 % of the participants resided in urban areas.
Table 2.
Delivery site and participant characteristics by AMOB/VLL attendance
| Total (n = 6,922) | 1 to 4 sessions (n = 1,372) | 5 to 8 sessions (n = 5,550) | χ2 | P value | 5 to 7 sessions (n = 3,274) | 8 sessions (n = 2,276) | χ2 | P value | |
|---|---|---|---|---|---|---|---|---|---|
| Delivery site characteristics | |||||||||
| Senior center/area agency on aging | 2,829 (40.9 %) | 588 (42.9 %) | 2,241 (40.4 %) | 29.94 | <0.001 | 1,308 (40.0 %) | 933 (41.0 %) | 16.77 | 0.005 |
| Residential facility | 2,066 (29.8 %) | 433 (31.6 %) | 1,633 (29.4 %) | 1,006 (30.7 %) | 627 (27.5 %) | ||||
| Health-care organization | 423 (6.1 %) | 63 (4.6 %) | 360 (6.5 %) | 202 (6.2 %) | 158 (6.9 %) | ||||
| Community/multipurpose center | 770 (11.1 %) | 152 (11.1 %) | 618 (11.1 %) | 336 (10.3 %) | 282 (12.4 %) | ||||
| Faith-based organization | 580 (8.4 %) | 75 (5.5 %) | 505 (9.1 %) | 293 (8.9 %) | 212 (9.3 %) | ||||
| Parks and recreation facility | 254 (3.7 %) | 61 (4.4 %) | 193 (3.5 %) | 129 (3.9 %) | 64 (2.8 %) | ||||
| Metro (delivery site) | 6,085 (87.9 %) | 1,236 (90.1 %) | 4,849 (87.4 %) | 7.65 | 0.006 | 2,849 (87.0 %) | 2,000 (87.9 %) | 0.89 | 0.346 |
| Nonmetro (delivery site) | 837 (12.1 %) | 136 (9.9 %) | 701 (12.6 %) | 425 (13.0 %) | 276 (12.1 %) | ||||
| Participant characteristics | |||||||||
| 50 to 64 years | 545 (7.9 %) | 123 (9.0 %) | 422 (7.6 %) | 6.08 | 0.108 | 241 (7.4 %) | 181 (8.0 %) | 5.10 | 0.165 |
| 65 to 74 years | 1,788 (25.8 %) | 376 (27.4 %) | 1,412 (25.4 %) | 837 (25.6 %) | 575 (25.3 %) | ||||
| 75 to 84 years | 3,053 (44.1 %) | 582 (42.4 %) | 2,471 (44.5 %) | 1,490 (45.5 %) | 981 (43.1 %) | ||||
| 85+ years | 1,536 (22.2 %) | 291 (21.2 %) | 1,245 (22.4 %) | 706 (21.6 %) | 539 (3.7 %) | ||||
| Male | 1,165 (16.8 %) | 245 (17.9 %) | 920 (16.6 %) | 1.29 | 0.256 | 504 (15.4 %) | 416 (18.3 % | 8.07 | 0.004 |
| Female | 5,757 (83.2 %) | 1,127 (82.1 %) | 4,630 (83.4 %) | 2,770 (84.6 %) | 1,860 (81.7 %) | ||||
| Less than high school | 963 (13.9 %) | 309 (22.5 %) | 654 (11.8 %) | 107.05 | <0.001 | 356 (10.9 %) | 298 (13.1 %) | 8.31 | 0.016 |
| Graduated high school | 1,908 (27.6 %) | 325 (23.7 %) | 1,583 (28.5 %) | 921 (28.1 %) | 662 (29.1 %) | ||||
| More than high school | 4,051 (58.5 %) | 738 (53.8 %) | 3,313 (59.7 %) | 1,997 (61.0 %) | 1,316 (57.8 %) | ||||
| Non-Hispanic White | 5,190 (75.0 %) | 914 (66.6 %) | 4276 (77.0 %) | 196.32 | <0.001 | 2,579 (78.8 %) | 1,697 (74.6 %) | 0.016 | 0.001 |
| Hispanic | 830 (12.0 %) | 312 (22.7 %) | 518 (9.3 %) | 293 (8.9 %) | 225 (9.9 %) | ||||
| African-American | 479 (6.9 %) | 64 (4.7 %) | 415 (7.5 %) | 224 (6.8 %) | 191 (8.4 %) | ||||
| Asian or Pacific islander | 96 (1.4 %) | 22 (1.6 %) | 74 (1.3 %) | 29 (0.9 %) | 45 (2.0 %) | ||||
| American Indian or Alaska Native | 164 (2.4 %) | 35 (2.6 %) | 129 (2.3 %) | 74 (2.3 %) | 55 (2.4 %) | ||||
| Other/multiple races | 163 (2.4 %) | 25 (1.8 %) | 138 (2.5 %) | 75 (2.3 %) | 63 (2.8 %) | ||||
| Lives with others | 2,991 (43.2 %) | 628 (45.8 %) | 2,363 (42.6 %) | 4.58 | 0.032 | 1,366 (41.7 %) | 997 (3.8 %) | 2.38 | 0.123 |
| Lives alone | 3,931 (56.8 %) | 744 (54.2 %) | 3,187 (57.4 %) | 1,908 (58.3 %) | 1,279 (56.2 %) | ||||
| Metro (participant) | 5,963 (86.1 %) | 1,196 (87.2 %) | 4,767 (85.9 %) | 1.51 | 0.219 | 2,797 (85.4 %) | 1,970 (86.6 %) | 1.40 | 0.236 |
| Nonmetro (participant) | 959 (13.9 %) | 176 (12.8 %) | 783 (14.1 %) | 477 (14.6 %) | 306 (13.4 %) | ||||
When comparing participant characteristics by attendance, a significantly larger proportion of participants who attended five or more AMOB/VLL sessions attended workshops offered in rural areas (χ2 = 7.65, P = 0.006). Significantly larger proportions of participants enrolled in workshops at community or multipurpose centers and faith-based organizations attended five or more sessions (χ2 = 29.94, P < 0.001). A significantly larger proportion of participants who attended five or more AMOB/VLL sessions were more educated (χ2 = 107.05, P < 0.001) and resided alone (χ2 = 4.58, P = 0.032). Significant workshop differences were observed by racial/ethnic category, with a larger proportion of non-Hispanic Whites attending five or more workshop sessions (χ2 = 196.32, P < 0.001).
Factors associated with receiving an adequate AMOB/VLL workshop dose
Table 3 displays the results of the binary logistic regression analysis examining factors associated with participants’ receipt of an adequate AMOB/VLL workshop dose (i.e., those attending between one and four sessions served as the referent group). Relative to those with less than a high school education, participants who graduated from high school were significantly less likely to receive an adequate AMOB/VLL workshop dose [odds ratio (OR) = 0.62, confidence interval (CI) (0.52, 0.75), P < 0.001]. African-American participants were significantly less likely to receive an adequate AMOB/VLL workshop dose compared to their non-Hispanic White counterparts [OR = 0.36, CI (0.23, 0.57), P < 0.001]. Relative to those who attended workshops at senior centers or AAA, participants who attended workshops at community or multipurpose centers [OR = 1.57, CI (1.05, 2.34), P = 0.028] and parks and recreation facilities [OR = 1.76, CI (1.20, 2.59), P = 0.004] were significantly more likely to receive an adequate AMOB/VLL workshop dose. Participants who attended workshops in rural areas were significantly more likely to receive an adequate dose compared to those attending workshops in urban areas [OR = 1.30, CI (1.06, 1.79), P = 0.016].
Table 3.
Factors associated with receiving an adequate AMOB/VLL dose
| P value | OR | 95 % CI | ||
|---|---|---|---|---|
| Lower | Upper | |||
| 50 to 64 years | – | 1.00 | – | – |
| 65 to 74 years | 0.112 | 0.82 | 0.63 | 1.05 |
| 75 to 84 years | 0.316 | 0.91 | 0.76 | 1.09 |
| 85+ years | 0.984 | 1.00 | 0.76 | 1.18 |
| Male | – | 1.00 | – | – |
| Female | 0.498 | 1.06 | 0.90 | 1.25 |
| Less than high school | – | 1.00 | – | – |
| Graduated high school | <0.001 | 0.62 | 0.52 | 0.75 |
| More than high school | 0.182 | 1.11 | 0.95 | 1.28 |
| Non-Hispanic White | – | 1.00 | – | – |
| Hispanic | 0.241 | 0.77 | 0.50 | 1.19 |
| African-American | <0.001 | 0.36 | 0.23 | 0.57 |
| Asian or Pacific islander | 0.407 | 1.24 | 0.75 | 2.06 |
| American Indian or Alaska Native | 0.121 | 0.60 | 0.32 | 1.14 |
| Other/multiple races | 0.096 | 0.62 | 0.35 | 1.09 |
| Lives with others | – | 1.00 | – | – |
| Lives alone | 0.058 | 1.13 | 1.00 | 1.29 |
| Metro (participant) | – | 1.00 | – | – |
| Nonmetro (participant) | 0.310 | 0.88 | 0.70 | 1.12 |
| Senior center/area agency on aging | – | 1.00 | – | – |
| Residential facility | 0.267 | 1.19 | 0.88 | 1.62 |
| Health-care organization | 0.682 | 1.07 | 0.78 | 1.47 |
| Community/multipurpose center | 0.028 | 1.57 | 1.05 | 2.34 |
| Faith-based organization | 0.451 | 1.14 | 0.81 | 1.62 |
| Parks and recreation facility | 0.004 | 1.76 | 1.20 | 2.59 |
| Metro (delivery site) | – | 1.00 | – | – |
| Nonmetro (delivery site) | 0.016 | 1.38 | 1.06 | 1.79 |
Referent group: attending one to four sessions
Factors associated with receiving a complete AMOB/VLL workshop dose
As seen in the bivariate analyses presented in Table 2, significant differences were identified based on whether or not those who received an adequate dose of the program attended all eight workshop sessions (i.e., complete dose). Of the 5,550 study participants who attended five or more AMOB/VLL workshops, 41.0 % received the complete dose. When comparing participant characteristics by this level of attendance, a significantly larger proportion of males (χ2 = 8.07, P = 0.004) and those who were less educated (χ2 = 8.31, P = 0.016) attended all eight AMOB/VLL workshops. Significant differences were also observed by racial/ethnic category (χ2 = 22.03, P = 0.001) and delivery site type (χ2 = 16.77, P = 0.005).
Table 4 displays the results of the binary logistic regression analysis explaining factors associated with participants’ receipt of a complete AMOB/VLL workshop dose among only those attending five or more sessions (i.e., those attending between five and seven sessions served as the referent group). Compared to participants aged 50 to 64 years, those aged 85 years and older were significantly less likely to receive a complete AMOB/VLL workshop dose [OR = 0.83, CI (0.72, 0.96), P = 0.011]. Female participants were significantly less likely to receive a complete AMOB/VLL workshop dose compared to their male counterparts [OR = 0.81, CI (0.70, 0.94), P = 0.006]. Relative to those with less than a high school education, participants who graduated from high school were significantly more likely to receive a complete AMOB/VLL workshop dose [OR = 1.22, CI (1.01, 1.47), P = 0.035]. American Indian and Alaska Native participants were significantly more likely to receive a complete AMOB/VLL workshop dose compared to their non-Hispanic White counterparts [OR = 1.87, CI (1.05, 3.33), P = 0.034]. Relative to those who attended workshops at senior centers or AAA, participants who attended workshops at residential facilities [OR = 1.41, CI (1.03, 1.93), P = 0.031], community or multipurpose centers [OR = 1.62, CI (1.12, 2.34), P = 0.010], faith-based organizations [OR = 1.65, CI (1.17, 2.33), P = 0.004], and parks and recreation facilities [OR = 1.45, CI (1.02, 2.06), P = 0.040] were significantly more likely to receive a complete AMOB/VLL workshop dose.
Table 4.
Factors associated with receiving a complete AMOB/VLL dose
| P value | OR | 95 % CI | ||
|---|---|---|---|---|
| Lower | Upper | |||
| 50 to 64 years | – | 1.00 | – | – |
| 65 to 74 years | 0.432 | 0.91 | 0.72 | 1.15 |
| 75 to 84 years | 0.044 | 0.85 | 0.72 | 1.00 |
| 85+ years | 0.011 | 0.83 | 0.72 | 0.96 |
| Male | – | 1.00 | – | – |
| Female | 0.006 | 0.81 | 0.70 | 0.94 |
| Less than high school | – | 1.00 | – | – |
| Graduated high school | 0.035 | 1.22 | 1.01 | 1.47 |
| More than high school | 0.085 | 1.12 | 0.99 | 1.26 |
| Non-Hispanic White | – | 1.00 | – | – |
| Hispanic | 0.173 | 0.79 | 0.56 | 1.11 |
| African-American | 0.580 | 0.90 | 0.61 | 1.32 |
| Asian or Pacific islander | 0.818 | 0.96 | 0.65 | 1.41 |
| American Indian or Alaska Native | 0.034 | 1.87 | 1.05 | 3.33 |
| Other/multiple races | 0.559 | 0.87 | 0.53 | 1.41 |
| Lives with others | – | 1.00 | – | – |
| Lives alone | 0.598 | 0.97 | 0.86 | 1.09 |
| Metro (participant) | – | 1.00 | – | – |
| Nonmetro (participant) | 0.462 | 0.92 | 0.74 | 1.15 |
| Senior center/area agency on aging | – | 1.00 | – | – |
| Residential facility | 0.031 | 1.41 | 1.03 | 1.93 |
| Health-care organization | 0.232 | 1.22 | 0.88 | 1.68 |
| Community/multipurpose center | 0.010 | 1.62 | 1.12 | 2.34 |
| Faith-based organization | 0.004 | 1.65 | 1.17 | 2.33 |
| Parks and recreation facility | 0.040 | 1.45 | 1.02 | 2.06 |
| Metro (delivery site) | – | 1.00 | – | – |
| Nonmetro (delivery site) | 0.808 | 0.97 | 0.77 | 1.22 |
Referent group: attending five to seven sessions
DISCUSSION
The national rollout of AMOB/VLL provides an excellent example of closing the research to practice gap through the widespread dissemination of an evidence-based falls reduction program for seniors. This was accomplished through a variety of delivery channels including the aging services network, residential facilities, community centers, faith-based organizations, health-care organizations, and parks and recreation facilities. And, although there were missing data for analytical purposes, it is clear that AMOB/VLL is a highly salient program to older adults regardless of location—more than 12,000 older adults participated across 14 states.
The results demonstrated variability in program completion rates and reveal the nuances distinguishing participant and site characteristics associated with intervention dose. Although a significantly larger proportion of non-Hispanic Whites received an adequate workshop dose, significantly fewer received the complete dose. Opposite trends were seen among Hispanic participants, where significantly smaller proportions received an adequate workshop dose, but a significantly larger proportion received the complete dose (among those attending five or more workshop sessions). Similar trends were also seen among other minority groups, with the exception of African-American participants who had larger proportions receiving adequate and complete workshop doses.
These results confirm the importance of attending to ethnic/minority variations in intervention dissemination research [29, 30]. The reasons why Hispanics were less likely to attend more program sessions are unclear, although there was anecdotal evidence that Hispanic participants were dropping out of the classes to go back to their homelands for extended visits. While AMOB/VLL workshops are currently offered in Spanish, such workshops were not widely available during the early years of this national initiative. Consequently, enrollment in Spanish language AMOB/VLL workshops could not be specifically examined in this study; however, the Spanish language version of AMOB/VLL may help to attract and retain less acculturated Hispanics who prefer programs in their native language [31]. We need to better understand the reasons different Hispanic populations stop attending workshop sessions and how to best formulate strategies to keep Hispanic participants in the program until they receive adequate exposure to the intervention so that they can achieve maximum benefits.
Contrary to the body of research suggesting that advanced education leads to greater program adherence and outcomes [32, 33], those who graduated high school were less likely to receive an adequate dose of the intervention. This documents that less educated older adults can attend the majority of workshop sessions but may experience difficulties when attempting to attend all eight of the AMOB/VLL sessions. However, similar to ethnicity trends for Hispanics, those with higher education were more likely to receive the complete intervention dose, relative to those without high school diplomas (Tables 3 and 4).
Those attending programs offered in rural areas were significantly more likely to attend five or more workshop sessions (Table 2). This may show the need or “thirst” for services in rural areas, thus reflecting the commitment of such participants to receive benefits and utilize limited health-related offerings in their areas [34, 35]. We were unable to ascertain the exact distance in which participants had to travel to attend classes, but it has been shown that delivering programs in close proximity to participants residence (and in familiar settings) can boost program attendance [36]. Travel-related issues may also differ based on the rurality of participants’ residence or delivery sites. For example, in rural areas, transportation is often carpooled or specially coordinated, which makes these populations more of a “captive audience” based on the prearranged and limited travel options. Further, research is needed to unveil the practical implications of travel issues on attendance levels for these evidence-based programs for older adults.
Although the majority of participants attended sessions at senior centers/AAA, other types of delivery sites were associated with better attendance (Tables 3 and 4) (e.g., community/multipurpose facilities, parks/recreation facilities, residential facilities, faith-based organizations). A better understanding of the dynamics and characteristics of those attending each type of delivery site is needed for tailoring recruitment/retention strategies to keep participants enrolled for the maximum intervention exposure. It would be valuable in future research to understand systematic delivery biases by examining whether there are only particular delivery systems available to persons in different locations and varying backgrounds, as well as specific participants most likely to register for evidence-based programs in different settings. These findings about program attendance may also be related to the types of programs that choose to adopt and deliver AMOB/VLL; many of which may not traditionally serve aging populations as their typical participant. Such organizations and institutions may benefit from additional communication with their local AAA about appropriate and successful strategies for participant recruitment and retention, as well as program fidelity during implementation.
Limitations
This study had limitations that must be acknowledged. First, there was considerable missing data for participants’ personal characteristics. This missing data may be attributed to the unwillingness of the participants to share sociodemographic data with program developers and/or a limited data collection and reporting infrastructure in earlier years of the national dissemination. Data collection of personal characteristics took place on site and during workshop time. To minimize missing data in future program dissemination efforts, it is important to establish data-related expectations for program implementers and reduce the time and resource-related burdens on workshop leaders and program participants. This study was also limited to the use of administrative data; thus, information about the program’s effectiveness was not available. While outcome data were not available for this study, prior research has shown that attending all eight AMOB/VLL workshop sessions is associated with a greater program impact on health-related behaviors and other indicators [25].
Additionally, there were no education- or health literacy-related requirements to enroll in the program, which ensures that high-risk and disadvantaged seniors are eligible for program participation. Although basic self-management skills were taught during group discussion, data were not collected to assess participants’ level of health literacy. Future disseminations of AMOB/VLL may examine health literacy levels because participants with high versus low levels of health literacy may have better program completion rates or greater health-related benefits.
Another acknowledged limitation is the nature of the AMOB/VLL course itself, which does not fully address the lack of coordination across different sectors of care. In addition to a primary focus on improving psychosocial attitudes, physical activity, and environmental risk factors, AMOB/VLL briefly covers aspects of vision and medication (physician interaction), which are important fall-related risk factors. To address these health care-related issues comprehensively, there is a need for multicomponent interventions that focus on integrated clinical and behavioral fall prevention programs that assist primary care providers to perform standardized fall prevention screenings and refer patients to community-based resources. The newly funded States Fall Prevention Program Initiative supported by the Centers for Disease Control and Prevention builds upon prior work to explore strategies for better connecting clinical and community efforts [37].
Finally, attendance was based solely on the number of sessions attended, and criteria for obtaining adequate dosage of the program did not differ based on which of the eight sessions was attended. We recommend future research efforts be performed to determine if attendance rates and/or health-related outcomes are influenced by which of the eight sessions is missed (i.e., to identify if some sessions contain content that is more critical to participant success or benefit). Additionally, we were unable to determine the preferred delivery site types in which participants would select, if given the opportunity. In grand-scale dissemination efforts of community-based interventions, the programs are offered by those organizations and facilities that adopt the intervention. Thus, the participant is limited to attend sessions only where they are offered, not necessarily where they are preferred. This has implications for program attendance and associated barriers. These study findings would be better understood if augmented by qualitative data collected to query program participants about the factors impacting their program attendance.
CONCLUSION
This study provides insight into the participant and delivery site characteristics associated with AMOB/VLL workshop attendance, which is linked to intervention dose. As previously determined, receiving an adequate AMOB/VLL workshop dose is correlated with improvements in health indicators, but significantly greater improvements are seen when all eight sessions are attended [25]. For this reason, program deliverers must realize that while situational circumstances arise in participants’ lives, which may impede their attendance of all workshop sessions, they must nevertheless seek out ways of making it easier for older adults to enroll in and fully complete evidence-based falls and fall risk reduction programs.
Programmatically, it is desirable to have a menu of evidence-based options delivered on a regular basis in a variety of settings that will appeal to the rapidly growing but heterogeneous population of seniors. Our findings showed that a variety of nonsenior service community agencies had higher rates of program completion than senior services agencies. Perhaps, the participants were younger, healthier, or were better able to handle transportation or other daily life challenges to in order to attend sessions. Or perhaps there was something different about the quality of the program instruction and delivery across the different sites. To understand better why some sites are more successful than others, more research is needed to determine effective agency-based strategies used to overcome attendance barriers and promote more complete programmatic adherence [38]. While much more research is needed, our findings may help program administrators to better understand and potentially minimize issues of attrition based on the participant and delivery site characteristics of their AMOB/VLL workshops. And, while it remains important to keep participants enrolling in evidence-based programs like AMOB/VLL and attend as many sessions as possible once enrolled, it is equally important to investigate issues of sustainability in terms of what program delivery sites require to continue offering programs to seniors in times of tight fiscal resources [39].
Acknowledgments
The national dissemination of A Matter of Balance/Volunteer Lay Leader model was supported as part of the United States Administration on Aging’s Evidence-Based Disease and Disability Prevention program (EBDDP) initiative. In addition to the AoA, this initiative was made possible by partnerships with the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality (AHRQ), Centers for Medicare and Medicaid Services (CMMS), Health Resources and Services Administration (HRSA), Substance Abuse and Mental Health Services Administration (SAMHSA), and over 30 private foundations. We recognize the support from the AoA with assistance from the National Council on Aging for the evaluation of the EBDDP initiative under cooperative agreement number 90OP0001/01, as well as the Healthy Aging Research Network, funded through the Centers for Disease Control and Prevention Prevention Research Centers. The findings and conclusions in this article are those of the author(s) and do not necessarily represent the official position of AoA, National Council on Aging, or any other agency. The authors specifically acknowledge the contributions of Nancy Whitelaw, Don Grantt, Wendy Zenker, Kelly Horton, Meghan Thompson, Ashley Wilson, and Linnae Hutchison.
Footnotes
Implications
Practice: Understanding the delivery infrastructure of evidence-based program dissemination efforts in community settings can inform program developers and deliverers about issues with participant retention and attrition, which has implications for maximizing health outcomes, improving quality care, and saving scarce resources.
Policy: While it remains important to keep participants enrolling in evidence-based programs like AMOB/VLL (and attend as many sessions as possible once enrolled), it is equally important to investigate issues of sustainability in terms of what program delivery sites require to continue offering programs to seniors in times of tight fiscal resources.
Research: Research is needed to determine effective agency-based strategies used to overcome attendance barriers and promote more complete programmatic adherence.
References
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Falls Among Older Adults: An Overview. Retrieved June 19, 2009, 2009 from http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html
- 2.Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev. 2005;11:115–119. doi: 10.1136/ip.2004.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Census Bureau. Federal interagency forum on aging related statistics. Older Americans 2008: key indicators of well-being. 2008.
- 4.Englander F, Hodson TJ, Terregrossa RA. Economic dimensions of slip and fall injuries. J Forensic Sci. 1996;41:733–746. [PubMed] [Google Scholar]
- 5.Preventing falls in older patients: a provider toolkit. Atlanta, GA: National Center for Injury Prevention and Control; 2012. [Google Scholar]
- 6.Centers for Disease Control and Prevention. What works: a CDC compendium of effective community-based interventions from around the world. Retrieved April 22, 2009 from http://www.cdc.gov/ncipc/preventingfalls/CDCCompendium_030508.pdf
- 7.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 8.Ory MG, Smith ML, Mier N, Wernicke MM. The science of sustaining health behavior change: the health maintenance consortium. Am J Health Behav. 2010;34:647–659. doi: 10.5993/AJHB.34.6.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ory MG, Hoffman M, Hawkins M, Sanner B, Mockenhaupt R. Challenging aging stereotypes: designing and evaluating physical activity programs. Am J Prev Med. 2003;25:164–171. doi: 10.1016/S0749-3797(03)00181-8. [DOI] [PubMed] [Google Scholar]
- 10.Schulz R, Belle SH, Czaja SJ, et al. Introduction to the special section on Resources for Enhancing Alzheimer’s Caregiver Health (REACH) Psychol Aging. 2003;18:357–360. doi: 10.1037/0882-7974.18.3.357. [DOI] [PubMed] [Google Scholar]
- 11.Seymour RB, Hughes SL, Ory MG, et al. A lexicon for measuring maintenance of behavior change. Am J Health Behav. 2010;34:660–668. doi: 10.5993/AJHB.34.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ory MG, Jordan PJ, Bazzarre T. The behavior change consortium: setting the stage for a new century of health behavior-change research. Health Educ Res. 2002;17:500–511. doi: 10.1093/her/17.5.500. [DOI] [PubMed] [Google Scholar]
- 13.Hughes S, Seymour R, Ory MG. Behavioral risk factors and evidence-based interventions. In: Prohaska TR, Anderson LA, Binstock RH, editors. Public Health in an Aging Society. Baltimore, MD: The Johns Hopkins Press; 2012. [Google Scholar]
- 14.Ory MG, Smith ML, Wade A, et al. Implementing and disseminating an evidence-based program to prevent falls in older adults, Texas, 2007–2009. Preventing Chronic Disease. 2010:http://www.cdc.gov/pcd/issues/2010/nov/2009_0224.htm. [PMC free article] [PubMed]
- 15.Ory MG, Smith ML, Wade AF, et al. Falls prevention as a pathway to healthy aging: statewide implementation and dissemination of an evidence-based program. College Station, TX: Texas A&M Health Science Center; 2009. [Google Scholar]
- 16.Partnership for Healthy Aging. A Matter of Balance replication report. Retrieved April 22, 2009 from http://www.healthyagingprograms.org
- 17.Tennstedt S. A randomized, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B Psychol Sci Soc Sci. 1998:P384–392. [DOI] [PubMed]
- 18.Healy TC. The feasibility and effectiveness of translating a matter of balance into a volunteer lay leader model. J Appl Gerontol. 2008;27:34–51. doi: 10.1177/0733464807308620. [DOI] [Google Scholar]
- 19.National Council on the Aging. Issue brief: evidence-based health promotion series. Using the evidence base to promote healthy aging (Vol. November 2006), 2006.
- 20.National Council on the Aging. Evidence-based programs: 2006 & 2007 AoA evidence-based disease prevention grantees and their programs. Retrieved June 29, 2009 from http://healthyagingprograms.org/content.asp?sectionid=32&ElementID=589
- 21.Area Agency on Aging of the Capital Area. A Matter of Balance: managing concerns about falls. Retrieved June 29, 2009 from http://www.aaacap.org/falls.html
- 22.Graafmans WC, Ooms ME, Hofstee HMA, et al. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143:1129–1136. doi: 10.1093/oxfordjournals.aje.a008690. [DOI] [PubMed] [Google Scholar]
- 23.Ory MG, Smith ML, Wade AF, Wright JC, Parrish R. Addressing falls in Texas: evidence-based fall prevention programming for older adults. Tex Public Health Assoc J. 2010;62:15–20. [Google Scholar]
- 24.Smith ML, Ahn S, Sharkey JR, et al. Successful falls prevention programming for older adults in Texas: rural-urban variations. J Appl Gerontol. 2010; doi:10.1177/0733464810378407.
- 25.Smith ML, Hochhalter AK, Cheng Y, Wang S, Ory MG. Programmatic influences on outcomes of an evidence-based falls program for older adults: a translational assessment. Transl Behav Med: Pract, Policy Res. 2011;1:384–393. doi: 10.1007/s13142-011-0058-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith ML, Jiang L, Ory MG. Falls efficacy among older adults enrolled in an evidence-based program to reduce fall-related risk: sustainability of individual benefits over time. Fam Community Health. 2012; 35:in press. [DOI] [PubMed]
- 27.Smith ML, Ory MG, Ahn S, Bazzarre TL, Resnick B. Older adult’s participation in a community-based falls prevention exercise program: relationships between the EASY tool, program attendance, and health outcomes. Gerontologist. 2011;51:809–821. doi: 10.1093/geront/gnr084. [DOI] [PubMed] [Google Scholar]
- 28.Smith ML, Ory MG, Larsen RAA. Older women in a statewide evidence-based falls prevention program: who enrolls and what benefits are obtained? Womens Health Issues. 2010;20:427–434. doi: 10.1016/j.whi.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Mier N, Ory MG, Toobert D, et al. A qualitative case study examining intervention tailoring for minorities. Am J Health Behav. 2011;34:822–832. [PMC free article] [PubMed] [Google Scholar]
- 30.Mier N, Ory MG, Medina AA. Anatomy of culturally sensitive interventions promoting nutrition and exercise in Hispanics: a critical examination of existing literature. Health Promot Pract 2009; doi:10.1177/1524839908328991. [DOI] [PMC free article] [PubMed]
- 31.Smith ML, Ahn S, Mier N, Jiang L, Ory MG. An evidence-based program to reduce fall-related risk among older adults: a comparison of program efficacy by ethnicity. California Journal of Health Promotion. 2012; in press.
- 32.Delamater AM. Improving patient adherence. Clin Diabetes. 2006;24:71–77. doi: 10.2337/diaclin.24.2.71. [DOI] [Google Scholar]
- 33.Stineman MG, Strumpf N, Kurichi JE, et al. Attempts to reach the oldest and frailest: recruitment, adherence, and retention of urban elderly persons to a falls reduction exercise program. Gerontologist. 2011;51:S59–S72. doi: 10.1093/geront/gnr012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith ML, Quinn C, Gipson R, Wilson AD, Ory MG. Serving rural communities for falls prevention: the dissemination of a matter of balance in the Brazos Valley region of Texas. Tex Public Health Assoc J. 2011;63:54–58. [Google Scholar]
- 35.Gipson R, Quinn C. Local perspectives on the implementation of an evidence-based falls prevention program: the Brazos Valley experience. Tex Public Health Assoc J. 2010;62:21. [Google Scholar]
- 36.Salazar CI, Smith ML, Perez AG, Ahn S, Ory MG. Geospatial characteristics of the Chronic Disease Self-Management Program: reaching diverse ethnic populations in San Antonio, Texas. Tex Public Health Assoc J. 2011;63:16–20. [Google Scholar]
- 37.Centers for Disease Control and Prevention. CDC falls prevention activities. Accessed from http://www.cdc.gov/HomeandRecreationalSafety/Falls/FallsPreventionActivity.html
- 38.Goins RT, Krout JA, editors. Service Delivery to Rural Older Adults. New York, NY: Springer Publishing Company; 2006. [Google Scholar]
- 39.Estabrooks PA, Smith-Ray RL, Dzewaltowski DA, et al. Sustainability of evidence-based community-based physical activity programs for older adults: lessons from Active for Life. Transl Behav Med: Pract, Policy Res. 2011;1:208–215. doi: 10.1007/s13142-011-0039-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


