ABSTRACT
Examine the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) of an evidence-based physical activity and nutrition curriculum disseminated to after-school programs. Program components included nutrition, physical activity, and sustainability, adapted to after-school settings and disseminated across 4 years (2004–2008). The RE-AIM framework was used to evaluate dissemination quality through direct observations, surveys, and interviews. In the final year, the Fun 5 program was implemented in 90% (>22,000 students) of Hawai'i after-school sites. Despite substantial annual increases in program reach, implementation and adoption remained consistently effective, and students' physical activity levels during program activities peaked in the final year. Further, evaluations demonstrated strong long-term program sustainability potential. The Fun 5 program demonstrated promise for long-term maintenance with potential for a public health impact among Hawai`i after-school students. Future emphasis on wide-spread program dissemination is encouraged, bridging research and community efforts to improve our children's health and impact public health.
KEYWORDS: Dissemination, Children, Physical Activity, Nutrition, After-school, RE-AIM
INTRODUCTION
Physical activity and fruit and vegetable consumption contribute to the reduced risk of many chronic diseases. Physical activity promotion among children is a central public health concern due to its association with reduced body fatness, reduced risk for cardiovascular and metabolic diseases, enhanced bone health, and reduced symptoms of anxiety and depression [1]. Diets rich in fruit and vegetable consumption contribute to children's healthy growth and development (e.g., healthy bones, skin) and lower the risk of poor health conditions associated with malnutrition (e.g., vitamin/mineral deficiencies, eating disorders) [2]. Furthermore, fruit and vegetable consumption has been associated with decreases in children's fat and sugar intake [3] and has also aided in the prevention and treatment of childhood obesity [4, 5].
Unfortunately, most children are not meeting physical activity and fruit and vegetable consumption recommendations. Children are recommended to participate in at least 60 min of moderate-to-vigorous physical activity each day [6]. Only 49% of boys and 35% of girls (6 to 11 years) meet this standard [7]. Recommendations from the Dietary Guidelines for Americans [8] suggest that children (9 to 11 years) should consume 1.5 to 2 cups of fruit (3–4 servings) and 2 to 3 cups of vegetables (4–6 servings) each day. However, only a small percentage of children are meeting fruit and vegetable consumption recommendations (1.2% of boys, 3.6% of girls) [9]. In view of the numerous health benefits, low occurrence of these health behaviors among children needs to be addressed by researchers and practitioners.
Many in-school activities promote children's physical activity (e.g., physical education class, recess) [10] and facilitate healthy eating opportunities (e.g., dietary guidelines for school lunch) [11]; however, many children enter an unhealthy environment following release from school. The After-school Alliance [12] reported that 25% of children are left unsupervised when school ends, which has demonstrated the potential to facilitate sedentary behavior and excessive snacking [13–15]. Organized school settings like after-school programs are efficient vehicles to provide evidence-based physical activity and nutrition interventions [16–18].
Beyond development of evidence-based physical activity and fruit and vegetable consumption interventions, successful programs must be widely disseminated to facilitate broad and lasting impacts. To disseminate and sustain evidence-based programs in real-world settings, intervention components must complement and be flexible to the existing resources and staff within the delivering agency [19], which has demonstrated previous success [20].
A crucial principle underlying successful program dissemination and sustainment is active and compatible participation from multiple sources [21]. Specifically, both research and practice personnel provide important and distinct information that may determine the likelihood that a program is successfully implemented and sustained in practice [22]. For example, research teams provide an evidence-based program with training protocols and execution recommendations; however, these efforts are irrelevant without the child management and actual implementation provided by after-school personnel.
Additional characteristics of the program and the organization (i.e., delivering agency) impact the opportunity for program sustainability. Program characteristics that promote its use and increase chances of sustainability include evidence of population reach and effectiveness, ease of implementation, manageable participant and organizational costs, and local adaption. Optimal organizational characteristics include existence of a strong infrastructure, a mission that aligns with program goals, a sense of program benefits for staff, and organizational longevity [23].
One method of achieving a strong environment that facilitates successful implementation and sustainability is to integrate the program into the organization's mission, the staffs' job requirements, and the existing funding structure [22]. The purpose of the current paper is to present dissemination results from an evidence-based intervention (Fun 5) within the existing operations of state legislated elementary after-school programs (A+) in Hawai`i with the goal of promoting children's physical activity and fruit and vegetable consumption.
METHOD
Program and organizational setting
The Sports, Play, and Active Recreation for Kids Active Recreation (SPARK AR) curriculum, the foundation for the physical activity component of Fun 5, was initially piloted in 13 elementary after-school programs (evaluation grades 4–6, n = 533). Baseline data demonstrated that students were sedentary during the majority of time spent in the after-school program (87.1% of the time standing, sitting, and lying down) [24]. The intervention decreased time spent standing, sitting, and lying down by 21% and increased time spent in moderate and vigorous physical activity by 140% [24]. Limited effects were observed with lesson context and self-reported sedentary activities [24], and no nutrition component was included at that time. Following the successful pilot, the Hawai'i Medical Service Association funded the University of Hawai'i to incorporate the Fun 5 program into Hawai'i A + after-school programs, to develop a nutrition component for Fun 5, and to evaluate Fun 5 for state-wide dissemination. The A + after-school program was administered by private providers (i.e., Kama'aina Kids, Young Men's Christian Association (YMCA), Youth Community Services (YCS), or the Department of Education, beginning after the regular school-day and ending when students were picked up (approximately 2:00 p.m.–5:30 p.m.). The Fun 5 program was integrated within the after-school setting with targets of at least three times per week of 30 min of physical activity and daily consumption of at least five fruit and vegetable servings (which was added in the first dissemination year).
Fun 5 program content
Fun 5 contains physical activity, nutrition, and sustainability components. Fun 5 trainings included participation by the A + after-school staff in activities that they would implement with Fun 5 students. Full day trainings targeted skill development necessary to implement and maintain the program. Training sessions included program introduction, nutrition and physical activity components, and program evaluation. Furthermore, booster training sessions were held each semester (i.e., fall and spring) during the first 3 years and were adjusted into mini-trainings during the final year. Mini-trainings included two foci: one tailored specifically to previous A + staff and another to new A + staff. To facilitate ongoing improvements, evaluations were completed by all participants at the conclusion of all trainings. Table 1 summarizes the Fun 5 components which are detailed in the following.
Table 1.
Fun5 components by year of program implementation
| Fun5 components & description | Tailored to | Schedule | Program year | |||
|---|---|---|---|---|---|---|
| Fun5 nutritional component | 2004–2005 | 2005–2006 | 2006–2007 | 2007–2008 | ||
| Nutrition training: portion sizes, sugar intake, & various healthy nutrition tips | A + staff | ✓ | ✓ | ✓ | ✓ | |
| Role model: encourage staff to practice, promote, & reinforce FVC ( ≥5 per day) | A + staff | ✓ | ✓ | ✓ | ✓ | |
| Child nutrition activities: demonstrate various activities for Fun5 students | A + staff | ✓ | ✓ | ✓ | ||
| Super Size Me movie presentation: expose the American obesity epidemic during the lunch break of staff trainings with brief discussions | A + staff | Aug/Sept | ✓ | ✓ | ||
| Healthy lunch/snacks: provide to staff during Fun5 training | A + staff | ✓ | ✓ | |||
| Child nutrition booklets: fun presentation of FVC health benefits, including short stories & educational activities | Students | ✓^ | ✓ | ✓ | ||
| Fun5 physical activity component | ||||||
| SPARK AR training: management training: student grouping, equipment use, team formation & activity training: great games (e.g., tag & ball games), super sports (e.g., soccer, frisbee), dynamic dance, & extra (e.g., jump rope, relays) | A + staff | Aug/Sept | ✓ | ✓ | ✓ | ✓ |
| SPARK AR binders and equipment: word-for-word instructions and detailed diagrams of SPARK AR components. Equipment for PA promotion (e.g., balls, hula hoops, etc.) | A + sites | 59% ✓ | ✓ | ✓ | ✓ | |
| Fun5 sustainability component | ||||||
| Booster session/mini-training: demonstrated new activities, problem solving, & shared success and challenge experiences | A + staff | Fall/spring | ✓ | ✓ | ✓ | ✓ |
| Newsletters: creative ideas to keep the Fun5 students motivated & active | A + personnel | Bi-monthly | ✓ | ✓ | ✓ | ✓ |
| Site coordinators meeting: review of the Fun5 program & training; dispersed updated nutrition booklets; & updated contact information | Coordinators | Annual | ✓ | ✓ | ✓ | |
| Fun5 stakeholder meeting: acknowledge providers, discuss program updates, & collect feedback | Providers | ✓ | ✓ | ✓ | ✓ | |
| Fun5 Website: describe program components & goals | Fundraisers | Ongoing | ✓ | ✓ | ✓ | ✓ |
| Fun5 MyPyramid.gov posters: promote 5 days of PA a week & 5 servings of fruit and vegetables each day http://www.mypyramid.gov/kids/index.html | A + sites | Jan/Feb | ✓ | ✓ | ||
| Fun5 monthly planner: time management tool for: homework, snack, arts and crafts, and Fun5 activities | A + staff | Aug/Sept | ✓ | ✓ | ||
DOE Department of Education, ^ second half, HMSA Hawaii Medical Service Association, FVC fruit and vegetable consumption, PA physical activity
Fun 5 nutrition
The nutritional component was started in year 1 (2004–2005), underwent adjustments, and was fully incorporated during year 2 (2005–2006). In fall 2005, the nutritional component targeted A + after-school staff, included a training and follow-up program. Training was extensive and included nutrition intervention for the staff, both receiving negative feedback from the A + staff. An existing component (Deal Me In—http://www.dairycouncilofca.org/Educators/ClassroomPrograms/ProgramsDMI.aspx) was implemented instead. Again, feedback was negative, referring to inappropriate elimination games, unclear instructions, cumbersome set-up, and complicated delivery.
The primary goal of Fun 5 was to disseminate a program with high potential for long-term sustainability. Research staff remained flexible and developed a nutrition component that held value and credibility among the A + staff. Specifically, the training portion was adapted to focus on the students. Thus, the nutrition training incorporated brief nutrition education which included benefits of fruits and vegetables, managing portion sizes, and sugar intake. A + staff was also encouraged to be a good role model in terms of snacking during A + time and to reinforce when the children brought healthy snacks to A+. Supporting this, a booklet of child nutrition activities was created with activities tailored to student grade-level (K–2 and 3–6). These booklets included word searches, cross words, coloring pages, and word/picture matching activities addressing local culturally appropriate fruit and vegetables. They were created so that students could complete them if they finished their homework early or during rainy days. The booklets were delivered late in year 2 and completely integrated in year 3. Booklets were well received by the A + staff, owing to constructive communication between research and practice.
Fun 5 physical activity
The Fun 5 physical activity component was based on the Sports, Play, & Active Recreation for Kids Active Recreation (SPARK AR) [25]. The physical activity component developed students' physical activity skills and promoted positive physical activity and health attitudes, including motor skills (e.g., throwing, catching, kicking), positive social skills (e.g., sharing equipment, cooperative behavior), and increased levels of physical activity. Table 1 details the specific training foci. SPARK AR binders and physical activity promoting equipment were distributed to all A + sites (two sets for sites with > 200 students). In the first year, only 59% of the A + sites received equipment; however, from year 2 onward, all participating sites were provided equipment (Table 1). To ensure equipment maintenance, a tracking system recorded all purchases and updated equipment every 3 years.
Fun 5 sustainability components
Components were designed to encourage program commitment and maintenance. Booster sessions/mini-trainings were conducted each semester, providing continuous learning opportunities. Additional sustainability components included a Fun 5 website, bi-monthly newsletters, promotional posters, and time management planners (Table 1). Meetings with program coordinators and stakeholders promoted the Fun 5 program and fortified communication and partnership.
Program evaluation procedures and measurement
Evaluations of Fun 5 dissemination outcomes were guided by the Reach, Effectiveness, Adoption, Implementation, and Maintenance framework (RE-AIM). RE-AIM describes five dimensions to evaluate program dissemination and its potential to impact public health [26]. Reach is the proportion of the population that benefits from the program. Effectiveness refers to program impact on targeted outcomes. Adoption, Implementation, and Maintenance represent program implementation quality and likelihood for long-term sustainability.
Reach
Reach was evaluated as the proportion of A + after-school site implementing Fun 5 and the estimated number of students receiving the intervention. Specific goals for Reach were established prior to dissemination and used to evaluate yearly progress. Back-calculations were derived using the Department of Education data from the current year (2008–2009) for inaccessible data on the number of students during 2004–2008.
Effectiveness
Fun 5 effectiveness included process and program outcomes with 10% of randomly selected after-school sites. New sites were selected each year to minimize burden and maximize evaluation coverage. Process outcomes evaluated how effectively Fun 5 components were implemented. Program outcomes examined the program's impact on students' physical activity and fruit and vegetable consumption. Process outcomes were summarized each year (i.e., spring) from questionnaires distributed to A + staff at the randomly selected sites. Using a five-point Likert scale, staff responded to questions regarding the usefulness and quality of Fun 5 training, SPARK AR binders, and physical activity equipment. Additional comments and suggestions for program improvement were requested in an open-ended format, facilitating communication and continuous program improvement.
Program outcomes were examined each year in fall and spring among randomly selected Fun 5 student groups within the initially selected sites, allowing for annual longitudinal comparisons. Students randomly selected from all age groups (K–6th) were observed during SPARK AR activities using the System of Observation of Fitness Instruction Time (SOFIT). SOFIT uses momentary time sampling to measure student activity level [27]. SOFIT observations were completed by a trained Fun 5 research team member and summarized as the proportion of time students spent doing moderate-to-vigorous physical activity. Considering reading levels, the older grades (4th–6th) of the randomly selected sites self-reported daily moderate-to-vigorous physical activity minutes and daily servings of fruit and vegetable consumption.
Adoption, Implementation, and Maintenance
Successful sustainability was determined through interviews and observations. Adoption, or the decision to implement Fun 5, was evaluated from yearly structured interviews with all A + site coordinators conducted by Fun 5 research staff. Coordinators reported the incorporation of physical activity at least three times a week and the accessibility to nutritional materials, which were summarized as the percentage of sites attaining these goals. Implementation was the extent of consistency between program execution and research protocol, evaluated and summarized as a percentage for each semester during unscheduled visits by trained Fun 5 research staff at 10% of randomly selected sites. Lastly, program maintenance was indicated from yearly standardized interviews with higher-level organizational leaders (i.e., all A + administrators/providers) conducted by Fun 5 research staff, summarizing the leaders' familiarity (scale: 1—not familiar to 5—familiar) and evaluation (scale: 1—very poor to 5—very good) of the Fun 5 program. The methods were approved by the University of Hawai'i Committee of Human Subjects, and participants provided consent or parental consent in the case of the students.
RESULTS
Reach
Fun 5 reach is presented in Table 2. From dissemination years 1 to 4, the percentage of sites implementing Fun 5 increased by 48%. The largest yearly increase occurred between years 2 and 3 (34%). Pre-established reach goals were accomplished annually, surpassing expectations furthest in year 3 (+24%). Reach data from 1 year beyond the scope of this study (2008–2009) demonstrated another 4% increase. The number of students reached escalated by 12,645 from years 1 to 4 and an additional 1,416 during the supplemental year.
Table 2.
Reach goals and attainment by year of program implementation
| Y1 (2004–2005) | Y2 (2005–2006) | Y3 (2006–2007) | Y4 (2007–2008) | Y5 (2008–2009) | |
|---|---|---|---|---|---|
| Reach goals | 30% | 50% | 60% | 70% | 80% |
| Implementation sites | 38% (n = 68) | 50% (n = 90) | 84% (n = 152) | 86% (n = 155) | 90% (n = 164) |
| # of studentsa | 8,548 | 11,975 | 20,898 | 21,193 | 22,609 |
aThe number of students includes non-public school sites, which were not included in percent of implementation site calculations
Effectiveness
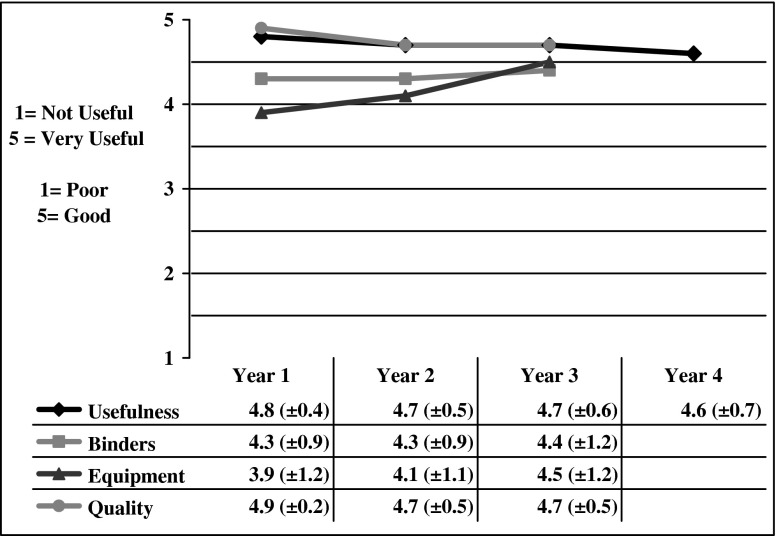
Figures 1 and 2 present process and program results, respectively, summarizing usefulness of the Fun 5 training, the SPARK AR binders, and the physical activity equipment (1 = not useful, 5 = very useful), as well as training quality (1 = poor, 5 = good). Unfortunately, a survey error limits year 4 training usefulness results as these components were inadvertently left off the survey. Training usefulness began high in year 1 (4.8), remaining consistent throughout dissemination. Reports of binder usefulness began high in year 1 (4.3) and remained high (4.4) in year 3. Staff reports of equipment usefulness began lowest during year 1 (3.9), but increased to 4.5 in year 3. Staff reports of training quality began high in year 1 (4.9) and remained consistently high through year 3 (4.7).
Fig 1.
Effectiveness process outcomes by year of program implementation
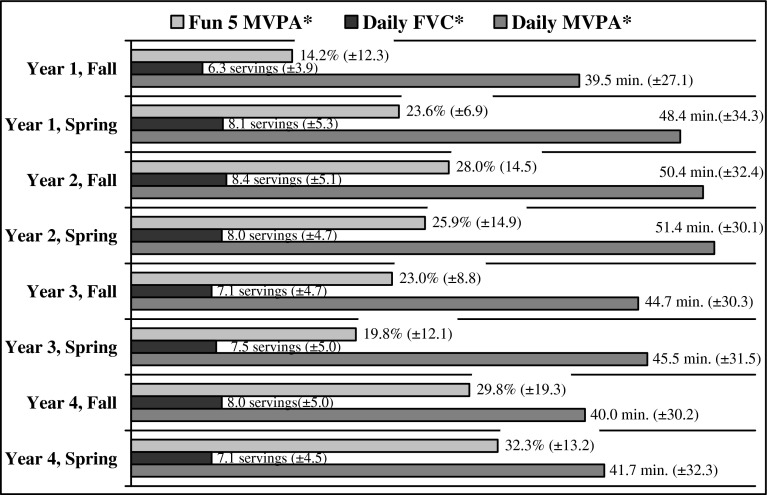
Fig 2.
Effectiveness program outcomes by year of program implementation. MVPA moderate-to-vigorous physical activity, min. minutes per day, FVC fruit and vegetable consumption, 1 serving 1 medium size fruit, ½-cup fruit or vegetable, 1-cup leafy vegetable, ¼-cup dried fruit per day
Figure 2 demonstrates program outcome results. SOFIT inter-rater reliability of 20% of the observations each year was excellent above the 80% recommendation (Y2 = 92.25%; Y3 = 92.75%; Y4 = 91.09%; Y1 inter-rater reliability was not collected due to staffing shortage) [26]. The lowest percent of moderate-to-vigorous physical activity occurred in the fall of year 1 (14.2%) and the highest during the spring of year 4 (32.3%). Percentages fluctuate minimally within each year; however, yearly averages demonstrate a progression over time. Specifically, the yearly average increased from 19% in year 1 to 27% in year 2, and although a slight decrease occurred in year 3 (-6%), percent of moderate-to-vigorous physical activity peaked during year 4 (31%). Regarding fruit and vegetable consumption, the grade 4–6 students report considerably high intake each semester, with the lowest in the fall of year 1 (6.3) and the highest in the fall of year 2 (8.4). Daily reported moderate-to-vigorous physical activity by the grade 4–6 students ranged from 39.5 min (fall, year 1) to 51.4 min (spring, year 2), resulting in a minimal range difference (11.9) over 4 years of dissemination. No reported fruit and vegetable consumption or reported moderate-to-vigorous physical activity was collected for the lower grades.
Adoption, Implementation, and Maintenance
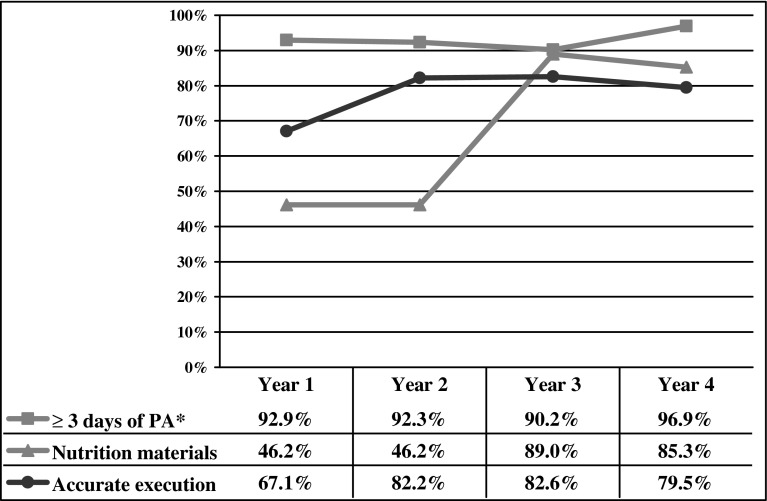
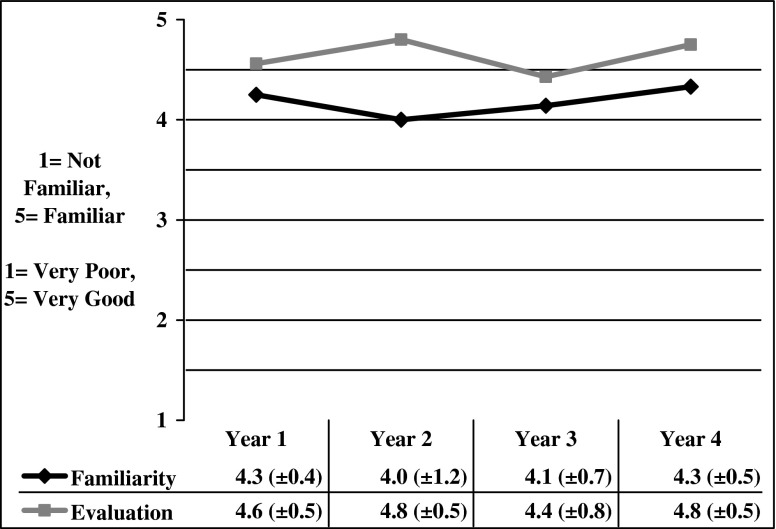
Figure 3 summarized program adoption outcomes and the percentage of successful implementation. The decision to execute physical activity at least three times per week remained consistently high throughout all 4 years (> 90%), demonstrating the highest percentage of adoption in year 4 (97%). Accessibility to nutritional materials was moderate during the first 2 years (46%), but improved in years 3 (89%) and 4 (85%). The percentage of proper program implementation was lowest in year 1 (67%), which improved in year 2 (+15%) and remained high through years 3 and 4 (≥ 80%). Figure 4 illustrates the maintenance results determined from administrator interviews. Fun 5 familiarity and evaluation scores remained high (≥ 4.0) during dissemination with the highest scores reported in year 4.
Fig 3.
Sustainability at site level by year of program implementation. PA physical activity
Fig 4.
Sustainability at organizational level by year of program implementation
DISCUSSION
The deficiency in children's physical activity and fruit and vegetable consumption is a national health concern. Members of Hawai'i Medical Service Association and University of Hawai'i, alongside after-school care providers, were able to successfully disseminate an evidence-based program (Fun 5) to promote physical activity and fruit and vegetable consumption. Four years of program dissemination evaluation demonstrated successful adaptability of Fun 5 within Hawai`i's A + after-school program. A constructive relationship between the Fun 5 research team, the state Department of Education, and the after-school personnel was instrumental. Results from RE-AIM evaluations suggest successful dissemination and program sustainability with potential to impact and improve the health of Hawai`i's child population.
Successful dissemination of Fun 5 was dependent on the sound relationship between research and practice to optimally adapt program components to A + after-school sites. Following continued responsiveness and adjustments, researchers developed a nutrition component effectively tailored to the A + staff and setting. Further flexibility was demonstrated by yearly booster trainings separately targeting previous A + staff and new hires. Awareness of program weaknesses and needed adjustments were achieved through ongoing evaluations, creating a constructive feedback loop for continuous improvement. Also, the recurrent communication components of Fun 5 (e.g., newsletters, website, meetings with A + personnel) generated rich relations between research and practice and improved the likelihood of program sustainability.
Characteristics of both the Fun 5 program and the A + after-school context were predominant influences on program dissemination. Fun 5 was simple in its execution and low-cost in its dissemination (about $250,000 annually for year 4 and year 5, which translates to about $1 per child per month of the school year). Implementation was simplified using hands-on training that provided detailed instructions and diagrams (e.g., SPARK AR binders). Also, the pre-existing organizational structure of the A + after-schools offered an increasingly large student reach that made the dissemination of Fun 5 cost effective. The A + program communicated health promotion goals consistent with the program. Fun 5 was strategically integrated into after-school time, creating a sense of program benefit among A + after-school staff. Program implementation is a job responsibility with added opportunities for health education and supportive resources.
Following adaption efforts and 4 years of dissemination, RE-AIM evaluations suggest program success and likely sustainability. Reach of Fun 5 increased each year, more than doubling from dissemination years 1 to 4. This consistent increase suggests that the Fun 5 program adapted with promise of reaching a large after-school student population. Consistently high program effectiveness was illuminated by elevated reports of training quality and usefulness by A + staff and supporting the success of initial program adaptations. Equipment usefulness began slightly lower and increased each year, possibly reflecting the lack of equipment at the start of dissemination and/or progressive advancement in program training and staff experience. Considering rapid annual reach increases, the gradually increasing and/or consistently high process outcomes demonstrate strong and reliable Fun 5 training efficacy.
Fun 5 effectiveness was also supported by outcome evaluations specific to students' physical activity and fruit and vegetable consumption. The year 1 increase and subsequent maintenance of high percentages of students' moderate-to-vigorous physical activity during Fun 5 activities reflect ongoing efficacy of staff training to promote increased physical activity levels, as well as the capacity of Fun 5 components to encourage students' movement (e.g., effective games, management). Grade 4–6 students' daily reported moderate-to-vigorous physical activity minutes surpassed the Fun 5 goal of 30 min; however, values are still below the daily recommended 60 min [6]. It may be that students rely on after-school time for physical activity opportunities, suggesting the need to intervene within other contexts (e.g., school-day, home). Regarding reported fruit and vegetable consumption, grade 4–6 students' daily servings consistently surpassed the Fun 5 goal (≥ 5 servings daily), suggesting program effectiveness beyond the after-school context.
Sustainability outcomes demonstrated excellent implementation with strong potential for long-term maintenance. Demonstrating staff willingness to participate, the proportion of A + staff adopting the Fun 5 physical activity goal was consistently high (all years ≥90%). Adoption of nutritional material began low and nearly doubled during the final 2 years of dissemination, which is likely due to numerous adjustments, initial lack of resources, and the full integration of the nutrition booklets in year 3. Conversely, this profound increase of nutritional material adoption in year 3 supports the appropriateness of initial program adaptations, validating the value of a strong research to practice relationship.
Evaluations of Fun 5 implementation by A + staff evidenced high consistency with research protocol, increasing largely in year 2 and remaining considerably high. The Fun 5 research protocol was developed from theory and research, outlining the implementation procedures required. Although a comparison group was lacking, this points to a relationship between Fun 5 components and child-level behavioral outcomes. The continual implementation and adaptability of training protocol by A + staff is especially impressive considering the progressive and rapid increases in Fun 5 sites each year. Lastly, high reports of annual Fun 5 familiarity and evaluation by school administrators suggest promise for long-term program maintenance and advocacy for sustainment.
The sustainability plan put in motion during year 4 of dissemination is (a) create a comprehensive program operations manual (POM), (b) identify a community-based organization to adopt Fun 5 and fundraising required (approximately $150,000 annually for implementation and $100,000 for the comprehensive evaluation), (c) shift funds from the evaluation component to provide the community-based organization preliminary funding to implement Fun 5 in year 5, and (d) allow staff from the community organization to shadow Fun 5 implementation during year 4 of dissemination, then lead year 5 implementation with support from the dissemination team, and then completely take over Fun 5 implementation (and, if funds are raised, the evaluation) in subsequent years.
Dissemination lessons learned
The dissemination evaluation does not account for the intangibles or the factors that the researchers believe are the “magic ingredients” that made Fun 5 successful (others call this the lessons learned). Although this is inherently subjective, it is informed by our qualitative assessments, interviews, and countless interactions throughout the years of Fun 5.
Engaging, participatory, and fun trainings. We inherited this from the SPARK approach. Trainings were (and still are) fun. The participants looked forward to coming to our trainings, and we heard a lot of comments like “this was the most fun training I have ever had.” This was infectious and made new staff want to come too.
Make life easier for staff. We feel that this is probably one of the most important things for implementation. Practical examples are make the schedules for the staff, give them things they can do without adding extra work (games without paperwork), and provide the children something to do when it is raining (e.g., dancing or the nutrition booklets). The A + staff quickly realizes that we are on their side. We don't want to make them work more, but have more fun while working and make their work easier.
- Cultivate relationships. This is true in general, but especially important in the multicultural environment of Hawai'i. Allow the first part of any meeting for the participants to “talk story,” and let them get to know each other, you, and topics in life important that day—we are all people first and foremost. Work needs to get done, but if it is not done in a fun and engaging way, others will not want to continue coming.
- Champions within partner organizations. These are your best allies. Communicate with them often. We feel that talking to them (not just email) is very important to cultivate this relationship. Promptly answer their requests, and provide them with materials that could be useful for their organization, above and beyond your project. The champions are usually the gatekeepers to their entire organization's commitment.
- Recognize them. The individuals from other organizations that are working with your project usually do not get paid, so we feel that one of the reasons they continued their involvement with us is that we recognized them. This is not just general thanks to all (that can actually backfire) but acknowledgement for specific things they did or contributed. In Hawai'i, the tradition is to provide a lei; it is not an expensive gift, but a very important gesture of respect.
Build local capacity—Fun 5/SPARK trainers for all counties—ambassadors. We were fortunate to work with SPARK, who recognized the benefits of having local capacity. This was important for us financially, so we did not have to fly in SPARK trainers every time. Much more important was the local pride and ownership this facilitated. Each A + provider recommended motivated and committed individuals to become SPARK trainers for Hawai'i. We have trainers on every county, which speaks volumes that this effort is a true collaboration and not the University bringing in “outsiders” to tell the local people what to do.
Early champions. One of the main reasons for our successful recruitment was to include the three major providers from the start—during the conceptualization discussions and in the pilot. Thus, the organizations knew what would be involved. Those early successes showed the value added by implementing Fun 5, motivated a private provider and a couple of DOE districts in the first year to implement across their sites. This early confidence opened other's curiosity.
Effective program. The second piece contributing to our successful dissemination was having an effective program. The fact that SPARK was evidence based provided a level of confidence for organizations to partake in the pilot. The successful pilot, in turn, provided everyone the confidence that this works in Hawai'i too. Finally, the substantial increase in participating sites and continued success in our first dissemination year, combined with being recognized nationally (United States Department of Health and Human Services 2005 Innovation in Prevention Award and the 2005 Gold Star Rank in the Cooper Institute's Children's Healthy Bodies Initiative) facilitated recruitment so much so that after dissemination year 2, we stopped active recruitment and let it grow on its own.
CONCLUSION
The chronic disease preventative nature of physical activity and fruit and vegetable consumption is well established and evidence-based programs promoting these health behaviors are numerous. It is now necessary for research to disseminate effective programs, evaluating program sustainability and potential public health impacts. The first 4 years of Fun 5 exceeded dissemination expectations, demonstrating high quality each year despite dramatic yearly increases in reach. For instance, even with a 34% increase in participating sites from years 2 to 3, the program demonstrated consistently high adoption, implementation accuracy, and maintenance likelihood. Minimal decreases observed in percent moderate-to-vigorous physical activity during year 3 may be attributable to rapid increased reach; however, the program adapted and recovered with even more sites and the highest percent of moderate-to-vigorous physical activity in year 4.
Evaluation of Fun 5 dissemination within Hawai`i's after-school program is novel. Unlike most program evaluations, the current results advance intervention research to a wide-spread dissemination. Strengths of the current study include its large sample size and multiple method approach to measurement. Noted limitations are the non-experimental design that limited casual conclusions of Fun 5 effectiveness, along with subjective student self-reports of daily moderate-to-vigorous physical activity and fruit and vegetable consumption which was limited to grade 4–6 students. It should also be clarified that unlike the physical activity component, the nutrition component had not been formally tested for efficacy. Although the data on grade 4–6 students on fruit and vegetable intake are encouraging, the design and data are insufficient to describe the nutrition component of the program as efficacious at this time. However, effectiveness was evident among several measures that determined successful dissemination.
Acknowledgments
This project was funded by the Hawai`i Medical Service Association, an Independent Licensee of the Blue Cross and Blue Shield Association. We would like to thank the valuable contributions of Cary Koike, Roberta Pang, Marisa Yamashita, Jo Ann Chang, Jackie Battista, Megan Inada, Crystalyn Hottenstein, Nicole Kerr, Kelley McGee, and Kevin Kuroda; the private providers (Kama'aina Kids, YMCA); the Hawai`i State Department of Education; and the participating sites.
Conflict of interest
All of the authors of this manuscript are individually without conflicts of interest, including specific financial interests, relationships, and affiliations relevant to the subject of this manuscript.
Footnotes
Implications
Research: Community-based dissemination research involves many components at various levels which need to be periodically assessed so that adjustments can be made to maintain implementation quality.
Practice: Continuous refreshers of program components and fostering motivation among staff are key to delivering a high quality program.
Policy: Evidence-based physical activity and nutrition programs targeted at children are available and should be supported to be implemented.
References
- 1.Healthy People 2010. Washington, DC: U.S. Government Printing Office; 2001. [Google Scholar]
- 2.Mirmiran P, Noori N, Zavareh MB, Azizi F. Fruit and vegetable consumption and risk factors for cardiovascular disease. Metabolism. 2009;58(4):460–468. doi: 10.1016/j.metabol.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes Res. 2001;9(3):171–178. doi: 10.1038/oby.2001.18. [DOI] [PubMed] [Google Scholar]
- 4.Epstein LH, Paluch RA, Beecher MD, Roemmich JN. Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity (Silver Spring) 2008;16(2):318–326. doi: 10.1038/oby.2007.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rolls BJ, Ello-Martin JA, Tohill BC. What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutr Rev. 2004;62(1):1–17. doi: 10.1111/j.1753-4887.2004.tb00001.x. [DOI] [PubMed] [Google Scholar]
- 6.Strong WB, Malina RM, Blimkie CJ, et al. Evidence based physical activity for school-age youth. J Pediatr. 2005;146(6):732–737. doi: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 7.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 8.Revised dietary guidelines to help Americans live healthier lives. FDA Consumer. 2005; 39(2):18–19. [PubMed]
- 9.Guenther PM, Dodd KW, Reedy J, Krebs-Smith SM. Most Americans eat much less than recommended amounts of fruits and vegetables. J Am Diet Assoc. 2006;106(9):1371–1379. doi: 10.1016/j.jada.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Wechsler H, Devereaux RS, Davis M, Collins J. Using the school environment to promote physical activity and healthy eating. Prev Med. 2000;31(2):S121–S137. doi: 10.1006/pmed.2000.0649. [DOI] [Google Scholar]
- 11.Centers for Disease Control and Prevention Guidelines for school and community programs to promote lifelong physical activity among young people. MMWR Recomm Rep. 1997;46(RR-6):1–36. [PubMed] [Google Scholar]
- 12.Health Utilisation Research Alliance (HURA). Ethnicity, socioeconomic deprivation and consultation rates in New Zealand general practice. J Health Serv Res Po. 2006; 11(3):141-149. [DOI] [PubMed]
- 13.Atkin AJ, Gorely T, Biddle SJ, Marshall SJ, Cameron N. Critical hours: physical activity and sedentary behavior of adolescents after school. Pediatr Exerc Sci. 2008;20(4):446–456. doi: 10.1123/pes.20.4.446. [DOI] [PubMed] [Google Scholar]
- 14.Pratt C, Webber LS, Baggett CD, et al. Sedentary activity and body composition of middle school girls: the trial of activity for adolescent girls. Res Q Exerc Sport. 2008;79(4):458–467. doi: 10.5641/193250308X13086832906517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Savige G, Macfarlane A, Ball K, Worsley A, Crawford D. Snacking behaviours of adolescents and their association with skipping meals. Int J of Behav Nutr Phys. 2007;4:36. doi: 10.1186/1479-5868-4-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coleman KJ, Geller KS, Rosenkranz RR, Dzewaltowski DA. Physical activity and healthy eating in the after-school environment. J Sch Health. 2008;78(12):633–640. doi: 10.1111/j.1746-1561.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 17.Pate RR, Davis MG, Robinson TN, Stone EJ, McKenzie TL, Young JC. Promoting physical activity in children and youth: a leadership role for schools: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Physical Activity Committee) in collaboration with the Councils on Cardiovascular Disease in the Young and Cardiovascular Nursing. Circulation. 2006;114(11):1214–1224. doi: 10.1161/CIRCULATIONAHA.106.177052. [DOI] [PubMed] [Google Scholar]
- 18.Optimal calcium intake. NIH Consens Statement Online. 1994; 12(4): 1–31. http://consensus.nih.gov/1994/1994OptimalCalcium097html.htm [PubMed]
- 19.Fawcett J, Aber C, Weiss M, et al. Adaptation to cesarean birth: implementation of an international multisite study. Nurs Sci Q. 2005;18(3):204–210. doi: 10.1177/0894318405277609. [DOI] [PubMed] [Google Scholar]
- 20.Rogers EM. Diffusion of innovations. 5. New York: The Free Press; 2003. [Google Scholar]
- 21.Minkler M, Wallerstein N. Introduction to community based participatory research. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health. San Francisco, CA: Jossey-Bass; 2003. pp. 3–26. [Google Scholar]
- 22.Estabrooks PA, Glasgow RE. Translating effective clinic-based physical activity interventions into practice. Am J Prev Med. 2006;31(4):S45–S56. doi: 10.1016/j.amepre.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 23.Scheirer MA. Is sustainability possible? A review and commentary on empirical studies of program sustainability. Am J Eval. 2005;26(3):320–347. doi: 10.1177/1098214005278752. [DOI] [Google Scholar]
- 24.Nigg CR, Battista J, Chang JA, Yamashita M, Chung RS. Physical activity outcomes of a pilot intervention using SPARK Active Recreation in elementary after school programs. J Sports Exerc Psychol. 2004;26:S144–S145. [Google Scholar]
- 25.Sallis JF, McKenzie TL, Alcaraz JE. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Sports, play and active recreation for kids. Am J Public Health. 1997;87(8):1328–1334. doi: 10.2105/AJPH.87.8.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/AJPH.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKenzie TL, Sallis JF, Nader PR, et al. BEACHES: an observational system for assessing children's eating and physical activity behaviors and associated events. J Appl Behav Anal. 1991;24(1):141–151. doi: 10.1901/jaba.1991.24-141. [DOI] [PMC free article] [PubMed] [Google Scholar]