Abstract
Objective
To determine the prevalence and mechanism of copying among ICU physicians using an electronic medical record.
Design
Retrospective cohort study
Setting
Medical intensive care unit of an urban, academic medical center
Participants
2,068 progress notes of 135 patients generated by 62 resident and 11 attending physicians between August 1 and December 31, 2009.
Interventions
None
Measurements and Main Results
82% of all resident and 74% of all attending notes contained ≥20% copied information (p=.001). Although residents authored more copied notes than attendings, residents copied less information between notes than attendings (55% vs. 61%, p<.001). Following ≥1 day off, residents copied less often from their own prior notes compared to attendings (66% vs. 94%, p < .001). Of the copied information following a day off, there was no difference in the amount of information copied into notes of residents (59%) or attendings (61%, p =.17). In a fixed effects regression model of attending notes, no patient factors were associated with copying. However, the levels of copying among attendings varied from 41% to 82% (p < .001).
Conclusions
Copying among attendings and residents was common in this ICU-based cohort, with residents copying more frequently and attendings copying more information per note. The only factor that was independently associated with attending copying was the attending. Further studies should focus on further elucidating the factors influencing copying in the ICU and the effects of copying on patient outcomes.
Keywords: Electronic Health Records, intensive care units, medical informatics, cohort study
BACKGROUND
Electronic health records have been touted to improve the accessibility, legibility, and completeness of medical documentation while reducing medical errors and mortality rates (1). Electronic clinician-generated progress notes may be more complete and demonstrate more appropriate clinical decisions compared to their paper equivalents (2). For these and other reasons, national implementation of electronic health records is expected to save the US healthcare system $77.8 billion annually (3). Not surprisingly, the Health Information Technology for Economic and Clinical Health Act of 2009 (HITECH) has encouraged the widespread and meaningful use of electronic health records within the next 5 years. Currently however, due in part to the steep cost of such systems, only 1.5% of hospitals currently have a comprehensive system and only 9.1% of hospitals have even a basic system (4).
While there are many advantages to electronic health record implementation, some have expressed concern regarding the development of “e-iatrogenesis”- a term used to describe patient harm resulting from health information technology (5, 6). One way electronic health records may adversely affect patients is by facilitating the copying of patient information between progress notes. Copying of information may impede clinician communication by perpetuating incorrect, unhelpful, or out of date clinical information, and subsequently diminish confidence in the accuracy of information provided (7). A recent study found that nearly 90% of electronic health record-using physicians admitted to copying and 80% planned to continue doing so, making the need for a comprehensive understanding of the pervasiveness of copying essential to ensuring thoughtful widespread electronic health record implementation (8). The concern regarding the increasing prevalence of copying in electronic health record progress notes has even prompted the publication of journal editorials (9, 10).
The intensive care unit is an ideal site to explore the extent of copying because of the high acuity of the patients, the frequent need for expeditious decision-making, the presence of complicated and technologically-advanced treatments, and the necessity for clear communication to facilitate multidisciplinary collaboration (11). Despite this, the characteristics of copying have not been described in the critical care setting. We sought to examine the frequency of copying among physicians in the medical intensive care unit to better understand what modifiable factors may be contributing. We hypothesized that copying would be infrequent in the intensive care unit, particularly in the notes of those patients with the highest severity of illness.
MATERIALS AND METHODS
Design and Setting
We performed a retrospective cohort study involving patients admitted to a 14-bed medical intensive care unit in an urban academic medical center between August 1, and December 31, 2009. Patients were eligible if they had stayed in the intensive care unit for at least 72 consecutive hours. Attending physicians rotated every 12 days with another attending covering the two days in between. Residents rotated every month and averaged one day off per week. The clinical team consisted of one attending, one critical care fellow, and four to five residents. The institutional review board of MetroHealth Medical Center, Cleveland, Ohio approved the study.
Data Collection
The assessment and plan portions of the progress notes of each patient (the portion of the note that contained the physician’s impression regarding the patient’s illness and plans for treatment) were extracted from the electronic medical record, EpicCare Inpatient Clinical System (EPIC Systems Corporation, Madison, WI) into a text file. We focused on the assessment and plan portion of the notes as we wanted the portion of the clinical record that most reflected physicians’ thoughts regarding each patient’s health status and treatment intentions. We were unable to separate the plan portion of the notes from the assessment as many authors had written them as one. All of the progress notes were typed into EpicCare directly by the physician. None of the clinicians dictated their notes.
EpicCare offers two ways to copy notes. The first, called “copy and paste function” involves highlighting the desired text, selecting “Copy” from the “Edit” pull-down menu, and then moving to the new progress note and selecting “Paste” from the same “Edit” menu. This allows any text from any note to be copied. The second method of copying, called “copy forward”, involves opening a new, blank progress note and pushing the “Copy Text” button. This allows the entire last note created by the author to be copied into that author’s new progress note. We attempted to differentiate the two forms of copying by identifying the source of the copied information and calculating the proportion of information copied. If the copied proportion was high and the source of the copied information was the same physician’s last note, the “copy forward” method was most likely used. If the source of the copied information was another physician’s note the “copy and paste function” was likely employed.
The text file generated from the progress note was uploaded into CopyFind, a GNU General Pubic Use License program developed by Louis Bloomfield (12) and used in similar studies evaluating medical copying (13). CopyFind was created to help identify plagiarism in education. CopyFind performed pair-wise comparisons of all progress notes of each patient and searched for identical matching word sequences. When a physician took time off, we compared the note written on their return to the note written by another physician on the day prior as well as the note written by the same physician prior to leaving. CopyFind has user-modifiable settings for identifying copied segments. We set it to identify matching phrases of more than 4 words and 20 total characters and to only report copying of ≥20%. We chose ≥20% to reduce the false positives of copying due to long phrases that are commonly employed in the medical intensive care unit such as “acute respiratory distress syndrome” (Figure 1). CopyFind then created a Hypertext Markup Language (HTML) file revealing each pair of documents side by side with the matching words and phases underlined (Figures 1 and 2).
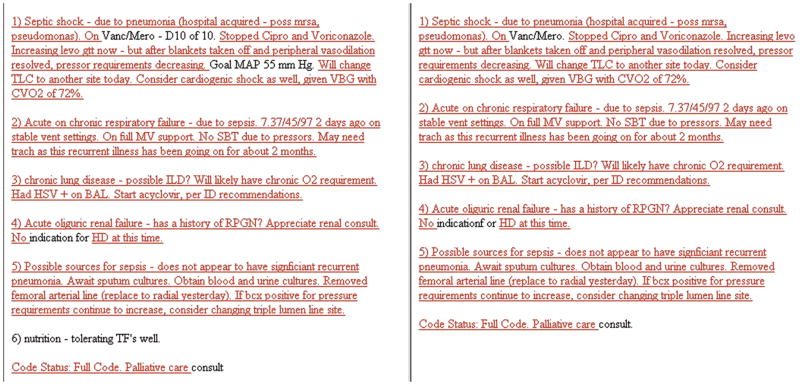
Figure 1.
Example of low copying proportion (11%) among two consecutive daily progress notes authored by one resident physician. The copied portions of text were underlined by the CopyFind software program.
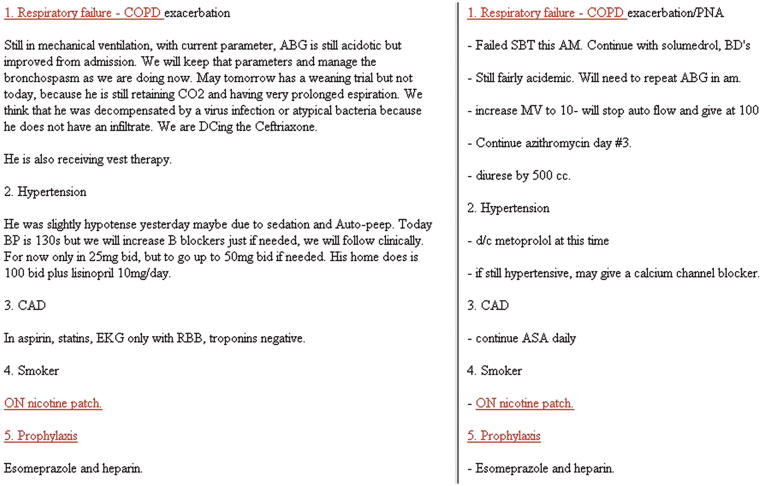
Figure 2.
Example of high copying proportion (90%) among two consecutive daily progress notes authored by one attending physician. The copied portions of text were underlined by the CopyFind software program.
Detailed patient information was obtained from the electronic record and included baseline demographics, admission diagnoses, primary insurance, severity of illness, and lengths of stay. Patients were followed for the entirety of their ICU stay. Patient deaths during the hospitalization were determined using the electronic record. Physician demographics were obtained through interview.
Statistical Analysis
For each patient, we determined the proportion of resident and attending progress notes containing ≥20% copied information. Patients were the unit of analysis. The t test was used to compare the mean copying proportion between attending and resident physicians and the mean copying proportion between notes on consecutive days compared to days following a physician hiatus. We then constructed a linear mixed model for repeated observations over time by patient and clustering of patients within physicians (intraclass correlation coefficient = .31). The effects of physicians on the primary response variable in this model (percent of copied information in attending notes) was assessed in several ways. In the initial model, physicians were included as a fixed categorical effect using dummy variables. For this model we generated the least square mean effects by physicians and tested pairwise differences with Tukey adjustment for multiple comparisons. In a second model, characteristics of attending physicians (gender, race, and years since fellowship) were included and assessed individually without an indicator for physicians. In addition, we constructed a model with characteristics of the interaction of demographics (race and gender) between patient and attending (i.e. both patients and attending the same or different gender or race). Only the final model was included in the results as the findings did not change. Similar models for resident physicians could not be constructed due to the large number of residents enrolled in the study.
Patient characteristics were determined a priori and included age, sex, race, ethnicity, insurance status, primary admission diagnosis, Acute physiology and Chronic Health Evaluation II (APACHE II) score at ICU admission and again 72 hours later, Sequential Organ Failure Assessment (SOFA) score at ICU admission and again 72 hours later, days of mechanical ventilation, and days in the ICU. The SOFA score at admission and 72 hours later were used in final models in place of APACHE II as it has been demonstrated to be a good indicator of prognosis (14) and no difference in the two was noted during model fitting. The unit of analysis for the regressions was the patient. Analyses were performed using SAS v.9.2 (Cary, NC). All p values represent 2-side hypothesis tests, and the significance level was .05.
RESULTS
Patient characteristics are found in Table 1. One hundred thirty five patients were admitted to the medical intensive care unit and had stays of longer than 3 days. The average age was 57 ± 16 years, 44% were men, and 16% of patients died during their hospitalization.
Table 1.
Patient Characteristics
| Patients (N = 135) | |
|---|---|
| Age, mean (SD), y | 57 (16) |
| Sex, no. of men (%) | 59 (44%) |
| Race and Ethnicity, no. (%) | |
| White, Not Hispanic | 87 (65%) |
| Black, Not Hispanic | 33 (24%) |
| Hispanic | 12 (9%) |
| Other | 3 (2%) |
| Insurance, no. (%) | |
| Uninsured | 12 (10%) |
| Medicaid | 49 (36%) |
| Medicare | 60 (44%) |
| Private | 13 (10%) |
| Primary admission category, no (%) | |
| Acute respiratory failure | 80 (59%) |
| Cardiovascular | 5 (4%) |
| Gastrointestinal Hemorrhage | 56 (4%) |
| Metabolic | 5 (4%) |
| Neurologic | 27 (20%) |
| Sepsis | 12 (9%) |
| APACHE II on ICU admit, mean (SD) | 20 (8) |
| APACHE II 72 hours following ICU admit, mean (SD) | 16 (8) |
| SOFA on ICU admit, mean (SD) | 8 (3) |
| SOFA 72 hours following ICU admit, mean (SD) | 7 (3) |
| Mechanical ventilation, mean days (SD) | 7 (5) |
| ICU length of stay, mean days (SD) | 7 (5) |
| Hospital length of stay, mean days (SD) | 14 (9) |
| In-hospital death, no (%) | 22 (16%) |
APACHE, Acute Physiology and Chronic Health Evaluation
ICU, intensive care unit
SOFA, Sequential Organ Failure Assessment
Physician characteristics and information regarding their progress notes are found in Table 2. Seventy-three physicians (62 residents and 11 attendings) cared for the 135 enrolled patients. Each patient had an average of 5 physicians caring for them during their intensive care unit stay. Patients stayed in the intensive care unit for an average of 7 ± 5 days and generated an average of 16 notes (8 by residents and 8 by attendings). Over the entire cohort, 2,068 notes (1047 resident and 1021 attending) were generated.
Table 2.
Characteristics of the physicians and their progress notes
| Number (%) | |
|---|---|
| Physicians, no. (%) | 73 |
| Residents | 62 (85%) |
| Attendings | 11 (15%) |
| Progress notes written, no. (%) | 2,068 |
| Resident notes | 1047 (51%) |
| Attending notes | 1021 (49%) |
| Notes per patient, mean (SD) | 15 (9) |
| Resident notes | 8 (4) |
| Attending notes | 8 (4) |
| Physicians per patient, mean (SD) | 5 (2) |
| Residents | 2 (1) |
| Attendings | 2 (1) |
The assessment and plan portion of the progress notes were on average 92 words longer for residents compared to attendings (208 ± 99 vs. 116 ± 61, p <.001, Table 3). Copying was found in 82% of all resident notes and 74% of all attending notes. Residents copied less information between notes than attendings (55 ± 23% vs. 61 ± 21%, p <.001). The source of copying following at least one day off varied between residents and attendings. Residents were less likely to copy information from their own notes from prior to the day off than attendings were (66% vs. 94%, p <.001). However, whether information was obtained from their own notes prior to a day off or from a colleague’s note on the day prior, both residents and attendings copied the same amount of information (59% vs. 61%, p = .17 and 52% vs. 49%, p = .48). Less than 20% of information was copied from attendings’ notes to residents’ notes and <20% of information was copied from residents’ notes to attendings’ notes. Similarly, we found <20% of information was copied from critical care physicians’ notes into consultants’ (residents’ or attendings’) notes.
Table 3.
Prevalence of progress note copying by ICU physicians
| Resident (773 Notes) | Attending (773 Notes) | p* | |
|---|---|---|---|
| Word count, mean (SD) | 208 (99) | 116 (61) | <0.001 |
| Percent of notes with ≥20% copying | 82% | 74% | 0.001 |
| Percent of information copied per note**, mean (SD) | 55% (23%) | 61% (21%) | <0.001 |
| Following ≥ 1 day off: | |||
| Percent of information copied from same author’s note**, mean (SD) | 59% (21%) | 61% (21%) | 0.17 |
| Percent of information copied from colleague’s note**, mean (SD) | 52% (24%) | 49% (22%) | 0.48 |
p-value based on mixed models with patient admissions considered a random effect to account for within-patient clustering of observations
among notes with at least 20% copying
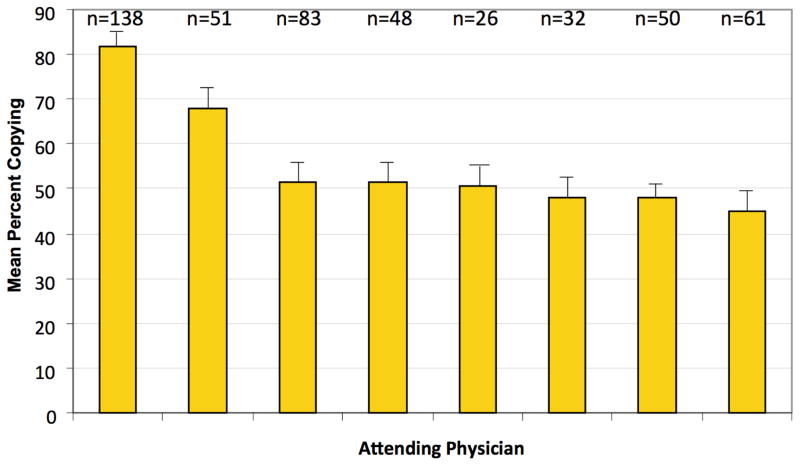
There was significant variation in the average amount of copying among both attendings and residents. In a regression model adjusting for the clustered effect of patients by physicians, there was significant variation in mean copying amongst attendings ranging from 41% to 82% (Figure 3) However, no patient factors were associated with copying, including ICU length of stay (p = .34), patient age (p = .23), patient gender (p = .61), patient race/ethnicity (p = .94), patient insurance (p = .48), patient SOFA score at admission (p = .36), change in SOFA score after 72 hours (p = .66), admission diagnosis (p = .38), and days on mechanical ventilation (p = .44, Table 4). . There was no significant association between attending gender, race/ethnicity, or years following fellowship and mean copying. There was also no effect of racial concordance between provider and patient on copying.
Figure 3. Adjusted mean percent copying by attending.
Bars represent adjusted mean levels with standard error bars. The number of patients evaluated by each physician is listed above each bar. Three attending physicians with a small number of observations not displayed. Overall effect of attendings (p<0.001); pairwise differences between the first attending and all other attendings was significant (p<0.05); pairwise differences between attending two and all other attendings was significant (p<0.05); pairwise differences between the third and last attendings was significant (p<0.05).
Table 4.
Patient characteristics independently-associated with increasing proportion of attending copying using multivariate regression
| Patient Characteristic | Regression Coefficient | p | 95% CI |
|---|---|---|---|
| Age | .08 | .23 | −.05 – .21 |
| Women | −.91 | .61 | −4.4 – 2.6 |
| Race and Ethnicity (White = referent) | |||
| Black | −1.3 | .58 | −6.1 – 3.4 |
| Hispanic | −.41 | .9 | −7.1 – 6.2 |
| Other | 1.5 | .82 | −12 – 15 |
| Insurance Status (Uninsured = referent) | |||
| Medicaid | −1.5 | .66 | −8.2 – 5.2 |
| Medicare | −3.3 | .33 | −10 – 3.4 |
| Private | .91 | .83 | −7.4 – 9.2 |
| Admission category (Sepsis = referent) | |||
| Acute Respiratory Failure | .08 | .98 | −6.1 – 6.3 |
| Cardiovascular | 6.4 | .25 | −4.6 – 17 |
| Gastrointestinal Hemorrhage | −.51 | .92 | −11 – 9.9 |
| Metabolic | 4.7 | .33 | −4.8 – 14 |
| Neurologic | −3.2 | .36 | −9.8 – 3.6 |
| SOFA on ICU admit | .28 | .35 | −.32 – .9 |
| SOFA change 72 hours following ICU admit | .14 | .66 | −.49 – .78 |
| Duration of mechanical ventilation | −.16 | .43 | −.57 – .24 |
| ICU length of stay | .49 | .34 | −.55 – 1.5 |
| Attending Physicians | |||
| Attending 1 | −10 | .06 | −20 – .39 |
| Attending 2 | −3.3 | .4 | −11 – 4.4 |
| Attending 3 | 30 | <.001 | 25 – 35 |
| Attending 4 | 16 | <.001 | 9.1 – 24 |
| Attending 5 | .13 | .97 | −7.2 – 7.5 |
| Attending 6 | −.94 | .83 | −9.6 – 7.7 |
| Attending 7 | −3.4 | .31 | −10 – 3.2 |
| Attending 8 | −6.5 | .04 | −13 – −.29 |
| Attending-Patient racial concordance | −1.3 | .57 | −6.0 – 3.3 |
Includes attendings who wrote notes on greater than 25 enrolled patients.
SOFA, Sequential Organ Failure Assessment
ICU, intensive care unit
DISCUSSION
In this cohort study conducted in the medical intensive care unit of an urban, academic medical center, copying of information in the assessment and plan portion of daily progress notes was prevalent among both resident and attending physicians. While residents copied more frequently than attendings, attendings copied more information between notes compared to residents. The majority of attending copying was from their own prior notes, both on consecutive days and following a day off. Attending physician was the only variable associated with copying.
Our finding of 74% copying among attendings, and 82% among all physicians in the medical intensive care unit is comparable to the prevalence of copying found in prior studies conducted outside of the medical intensive care unit. A study from the Utah VA hospital found an overall prevalence of 20% copying of patient notes (7). However, when they examined 60 patient records more closely, they found that 43 (72%) had at least one copied note. In another VA study, over 167,076 notes were analyzed for 1,479 patients (13, 15). Using the Copyfind software used in this study, the authors found 90,702 instances when “pairs of documents contained identical forty-word sentences.” This amounts to a copy rate of 54%. The copy rates were greatest in the physical exam (25% of patient records), but the assessment portion of notes was fourth most common. Over the 7.5 years of analyzed data, the copy rates significantly increased with 2 notes with copied text in 1995 and 867 in 2001.
When interviewed, many physicians have acknowledged copying frequently in their electronic notes. In one study conducted at two academic medical centers, 90% of 253 physicians reported copying when writing progress notes (8). The majority (70%) reported copying almost always or most of the time when writing their notes. Residents were three times more likely to report high copying rates compared to attendings. Interestingly, the majority of the physicians who reported copying did so using the “copy and paste function”. In this study, however, attending physicians were more likely to copy from their own notes than the notes of colleagues, suggesting use of the “copy forward” method. Intensivists in this study may have exhibited a lack of trust in the information found in the notes of colleagues, who were generally covering patients over the weekend, and therefore less often chose to copy information from their colleagues’ notes.
The fact that copying prevalence in this intensive care unit-based study was not appreciably different from that of studies involving the notes of patients with lower severity of illness suggests that despite the need for intensive monitoring and therapies, physicians may not feel obligated to convey new or changing information from day to day. Alternatively, the intensive care unit environment may make physicians feel more compelled to reduce their workload. Electronic health records have been demonstrated to slow the speed at which clinicians carry out clinical documentation and ordering processes (16). The addition a “copy forward” button to the electronic health record may provide physicians with an easy means to reduce workload. Another explanation for the high rate of copying in the intensive care unit may be a change in the perception of the utility of the medical record. Some authors have suggested that the primary purpose of writing progress notes has shifted from the transfer of knowledge to documentation for billing (11). As a result, physicians may be less invested in spending the time and effort necessary to convey new information and may prefer copying of existing information as a means to quickly completing an onerous task. We found no patient characteristics that were associated with copying among attendings. We also found that there was great variability in attending copying. These findings suggest that copying occurs at the whim of the intensivist regardless of the patient.
There are limitations of this study. We examined progress notes involving patients of a medical intensive care unit in a single hospital. The results may not be generalizable to other settings. The study was conducted during a time of year when the medical intensive care unit census is generally low. However, it is difficult to envision how an increased physician workload would be associated with less copying. Physicians in this study used EpicCare and while it is one of the most utilized electronic health records in the country, other electronic health records may be used differently. We did not directly observe the physicians in this study writing notes nor did we interview them to better understand their behavior. We chose to report a copying rate of greater than 20% to minimize the risk of false positives. In doing so, the reported copying prevalence was likely artificially low. However, with over 75% of the examined notes having some form of copying, even this prevalence is quite elevated.
Data continues to emerge demonstrating benefits to using electronic health records. In the ambulatory setting, diabetes care is significantly better at facilities using electronic compared to paper records (17). In inpatient settings, electronic records with physician order entry have been demonstrated to reduce medical errors and mortality (18, 19). They have also been shown to reduce time spent for daily activities, reduce costs and are positively regarded by nurses and clinicians (20–23). However, with the relative ease of copying information into progress notes, the possibility of inaccurate of diluted information exists in which true patient assessments and treatment plans may be missed and adverse patient outcomes may result (11). Copying may also lead to less independent thought thereby hampering the development of alternative diagnoses and treatments (9). This is of particular concern in training the next generation of doctors. As we transition to electronic health records we need to continue to focus on their strengths while being careful not to embrace their limitations.
Acknowledgments
Supported by grant 1-P60MD002265-01 from the National Center on Minority Health and Health Disparities, and from the Robert Wood Johnson Harold Amos Medical Faculty Development Program.
Footnotes
The authors report no commercial associations that might pose a conflict of interest in connection with this manuscript.
Dr. Thornton had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author Contributions:
Conception and design: JDT, LV
Analysis and interpretation: JDT, JS, LV, BL
Drafting of the manuscript for important intellectual content: JDT, JS, LV, BL
The authors have not disclosed any potential conflicts of interest
References
- 1.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 2.Tang PC, LaRosa MP, Gorden SM. Use of computer-based records, completeness of documentation, and appropriateness of documented clinical decisions. J Am Med Inform Assoc. 1999;6:245–251. doi: 10.1136/jamia.1999.0060245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baron RJ, Fabens EL, Schiffman M, et al. Electronic health records: just around the corner? Or over the cliff? Ann Intern Med. 2005;143:222–226. doi: 10.7326/0003-4819-143-3-200508020-00008. [DOI] [PubMed] [Google Scholar]
- 4.Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360:1628–1638. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 5.Weiner JP, Kfuri T, Chan K, et al. “e-Iatrogenesis”: the most critical unintended consequence of CPOE and other HIT. J Am Med Inform Assoc. 2007;14:387–8. doi: 10.1197/jamia.M2338. discussion 389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell EM, Sittig DF, Ash JS, et al. In reply to: “e-Iatrogenesis: The most critical consequence of CPOE and other HIT”. J Am Med Inform Assoc. 2007 doi: 10.1197/jamia.M2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weir CR, Hurdle JF, Felgar MA, et al. Direct text entry in electronic progress notes. An evaluation of input errors. Methods Inf Med. 2003;42:61–67. [PubMed] [Google Scholar]
- 8.O’Donnell HC, Kaushal R, Barrón Y, et al. Physicians’ attitudes towards copy and pasting in electronic note writing. J Gen Intern Med. 2009;24:63–68. doi: 10.1007/s11606-008-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartzband P, Groopman J. Off the record--avoiding the pitfalls of going electronic. N Engl J Med. 2008;358:1656–1658. doi: 10.1056/NEJMp0802221. [DOI] [PubMed] [Google Scholar]
- 10.Hirschtick RE. A piece of my mind. Copy-and-paste. JAMA. 2006;295:2335–2336. doi: 10.1001/jama.295.20.2335. [DOI] [PubMed] [Google Scholar]
- 11.Gajic O, Herasevich V, Hubmayr RD. Will the electronic medical record live up to its promise? Am J Respir Crit Care Med. 2010;182:585–586. doi: 10.1164/rccm.201004-0677ED. [DOI] [PubMed] [Google Scholar]
- 12.The Plagiarism Resource Site [Internet] [cited 2012 Apr. 23] Available from: http://plagiarism.bloomfieldmedia.com/z-wordpress/
- 13.Hammond KW, Helbig ST, Benson CC, et al. Are electronic medical records trustworthy? Observations on copying, pasting and duplication. AMIA Annual Symposium proceedings / AMIA Symposium AMIA Symposium; 2003. pp. 269–273. [PMC free article] [PubMed] [Google Scholar]
- 14.Ferreira FL, Bota DP, Bross A, et al. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–1758. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 15.Thielke S, Hammond K, Helbig S. Copying and pasting of examinations within the electronic medical record. International Journal of Medical Informatics. 2007;76 (Suppl 1):S122–8. doi: 10.1016/j.ijmedinf.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Poissant L, Pereira J, Tamblyn R, et al. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;12:505–516. doi: 10.1197/jamia.M1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cebul RD, Love TE, Jain AK, et al. Electronic health records and quality of diabetes care. N Engl J Med. 2011;365:825–833. doi: 10.1056/NEJMsa1102519. [DOI] [PubMed] [Google Scholar]
- 18.Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280:1311–1316. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- 19.Amarasingham R, Plantinga L, Diener-West M, et al. Clinical information technologies and inpatient outcomes: a multiple hospital study. Arch Intern Med. 2009;169:108–114. doi: 10.1001/archinternmed.2008.520. [DOI] [PubMed] [Google Scholar]
- 20.Kari A, Ruokonen E, Takala J. Comparison of acceptance and performance of automated and manual data management systems in intensive care. Int J Clin Monit Comput. 1990;7:157–162. doi: 10.1007/BF02915580. [DOI] [PubMed] [Google Scholar]
- 21.Menke JA, Broner CW, Campbell DY, et al. Computerized clinical documentation system in the pediatric intensive care unit. BMC Med Inform Decis Mak. 2001;1:3. doi: 10.1186/1472-6947-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med. 2008;359:50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 23.Donati A, Gabbanelli V, Pantanetti S, et al. The Impact of a Clinical Information System in an Intensive Care Unit. J Clin Monit Comput. 2008;22:31–36. doi: 10.1007/s10877-007-9104-x. [DOI] [PubMed] [Google Scholar]