Abstract
Ciliated hepatic foregut cyst (CHFC) is a rare foregut developmental malformation usually diagnosed in adulthood; however, rare cases have been reported in the pediatric population. CHFC can transform into a squamous cell carcinoma resulting in death despite surgical resection of the isolated malignancy. We report the presentation, evaluation, and surgical management of a symptomatic 17-year-old girl found to have a 6.5 × 4.5 centimeter CHFC and suggest that all patients with suspected CHFC undergo prompt evaluation and complete cyst excision.
Keywords: hepatic cyst excision, liver cyst, pediatric surgery, ciliated cyst
Introduction
Ciliated hepatic foregut cyst (CHFC) is a rare foregut developmental malformation first described by N. Fridrich in 1857. In more recent history, Wheeler and Edmondson histologically characterized CHFC as ciliated, pseudostratified, columnar epithelium, covered by connective tissue, a smooth muscle layer, and an outer fibrous capsule.1–3 Definitive diagnosis requires a biopsy of the cyst wall demonstrating these histologic features.
An estimated 90 cases of CHFC have been reported, predominantly in adults. However, there have been seven previously published reports of CHFC in children.3–9 To date, there have been three reported cases of malignant transformation from CHFC to squamous cell carcinoma resulting in death of two patients from recurrent malignancy within 9 months of complete tumor excision.10–12 As such, while malignant transformation occurs in approximately 3% of the cases, the survival rate of these patients with squamous cell carcinoma is poor.
Asymptomatic patients present with an incidentally identified, solitary, cystic hepatic lesion. Patients who present with symptoms usually complain of right upper quadrant and/or epigastric abdominal pain, or symptoms related to obstructive jaundice or portal hypertension.2, 4, 5 Herein, we describe the clinical course of a teenager who presented with a symptomatic CHFC, and examine the role of preemptive operative resection in the pediatric patient population.
Case
A seventeen-year-old African-American female presented to an outside medical center with a one month history of right upper quadrant abdominal pain, nausea, and frequent post-prandial emesis. She was morbidly obese (body mass index = 40.2 kg/m2); however, the remainder of physical examination was unremarkable. Electrolyte and hematologic panels were normal; the albumin was 3.8 g/dl (normal 3.9–4.9 g/dl) and the alkaline phosphatase was 96 U/L (normal 41–92 U/L). Other liver function tests and alpha-fetoprotein level were normal. The patient underwent an abdominal ultrasound, revealing a single hypoechoic mass in the left lobe of the liver measuring approximately 5 × 6 cm. Subsequent computed tomography (CT), magnetic-resonance imaging, and an ultrasound-guided biopsy all failed to diagnose the cyst or exclude malignancy. As such, she was referred to our medical center for further evaluation and treatment.
Repeat CT-imaging with triple-phase contrast confirmed the presence of a single 6.5 × 4.5 × 6.3 cm hepatic cyst in segment IV with extension into segment VIII (Figure 1). An ultrasound-guided biopsy demonstrated normal hepatic parenchyma with a thick fibrous band focally lined by pseudostratified, columnar, ciliated epithelium with mucoid material consistent with histologic diagnosis of CHFC. Due to the potential for malignant transformation and ongoing abdominal pain we recommended operative cyst excision.
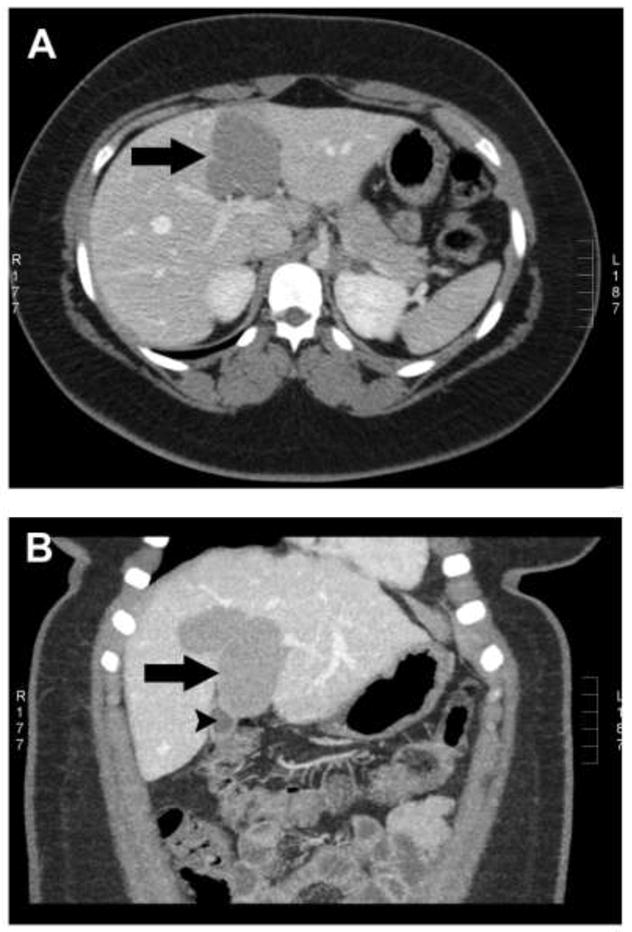
Figure 1.
Triple-phase CT scan with axial (Panel A) and coronal (Panel B) images of a large CHFC arising in segments IV and VIII (large arrow). The gallbladder is visible on the coronal view (panel B) and is marked by small arrowhead.
In the operating room, we laparoscopically decompressed the mucoid fluid cyst content. The cyst wall lining appeared smooth and uniform with no evidence of malignancy or bile ductule communication (Figure2). A portion of the cyst wall was sampled for frozen-section analysis. The preliminary histology was consistent with CHFC, confirmed by the presence of ciliated columnar cells with elements of smooth muscle capsule. Due to intrahepatic extension of the cyst, we converted to a laparotomy via a right subcostal incision. The CHFC and gallbladder shared a common thin-walled fibrous septum and a concomitant cholecystectomy was performed with complete cyst excision. Final histology confirmed diagnosis of CHFC (Figure 3). The immediate post-operative course was uneventful and the patient was discharged home on postoperative day #3. The patient has subsequently completed high school and started junior college with no recurrent symptoms.
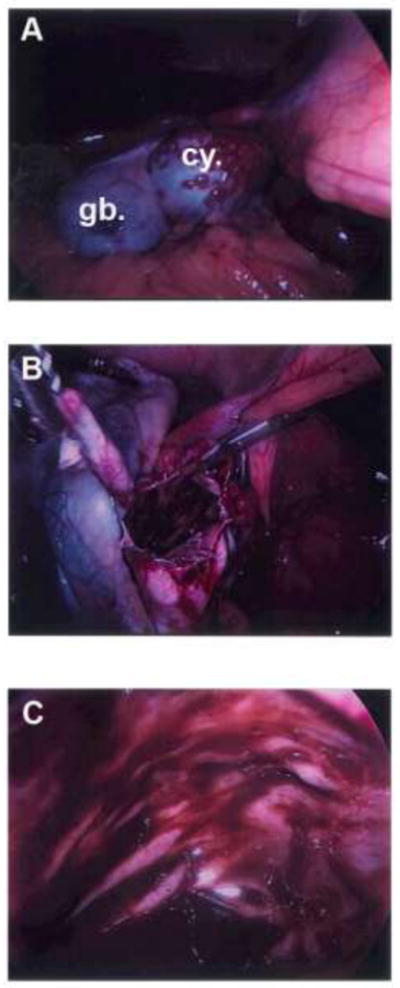
Figure 2.
Intra-operative photographs during laparoscopy showing an intact CHFC (Panel A), incised CHFC (Panel B) with portion of the wall sent for frozen section evaluation, and the inside view of the cyst (Panel C). gb=gallbladder; cy=CHFC.
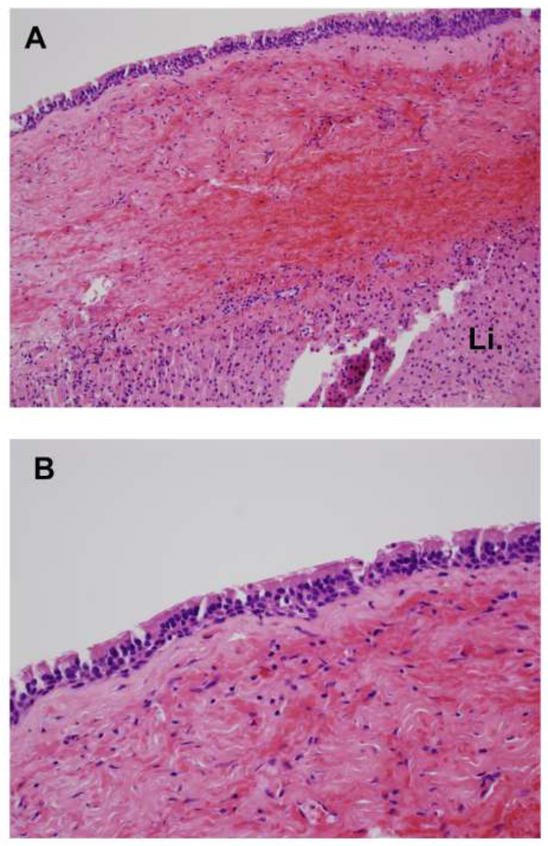
Figure 3.
Hematoxylin and eosin stained permanent sections of cyst wall (Panel A - 200x magnification) showing pseudostratified epithelium lining, connective tissue, smooth muscle layer, an outer fibrous capsule cyst wall and underlying liver parenchyma with the closer view (Panel B - 400x magnification) highlighting the ciliated, columnar, pseudostratified epithelial lining. Li=liver parenchyma.
Discussion
Solitary liver cysts in children are rare and span a range of diagnoses. A recent study identified a number of cyst-related diagnoses: simple cyst, intrahepatic choledochal cyst, complex biliary cyst, cystic mesenchymal hamartoma, hydatid cyst, and ciliated hepatic foregut cyst.13 The authors reviewed twenty-one children and noted prenatal diagnosis with a median gestational age of 22 weeks in 11/21 (52%), and antenatal diagnosis with a mean age of 7.5 years in the remaining 48% of the children. Approximately half of the patients in both groups required surgical resection attributed either to symptomatic presentation or concerning histopathology. CHFC was diagnosed in only one of the twenty-one patients and was treated by excisison.3, 13
While choledochal cyst is the most common pediatric hepatobiliary cystic anomaly, it can usually be excluded with radiologic imaging. The majority of choledochal cysts present with either extrahepatic manifestations or multiple intrahepatic components. Unlike the solitary intrahepatic CHFCs that have not been shown to communicate with the biliary tree, choledochal cysts arise within the bile duct and have an anomalous union of the pancreatic and common bile ducts proximal to the sphincter of Oddi. When radiologic diagnosis is uncertain, a percutaneous biopsy will confirm pathognomonic histopathologic features of CHFC.
Including this report, there are only 8 cases of CHFC described in the pediatric population. Half of the children were diagnosed before 6 years of age (two boys and two girls), while the other four children (all female) were diagnosed as teenagers. Demography, clinical presentation, and treatment of this pediatric cohort are summarized in Table 1. Symptomatic abdominal distention resulting from a very large cyst (10 × 7.5 × 5 cm) necessitated a surgical intervention in one of the four children presenting before 6 years of age. The infant was diagnosed prenatally and underwent multiple surgical interventions including: (1) cyst aspiration with rapid bilious reaccumulation, (2) two attempts at internal drainage via cystojejunostomy, and (3) definitive left trisegmentectomy.3 The other three children were diagnosed during prenatal screening or later during evaluation for unrelated illness. Two of these children underwent surgical resection for definitive diagnosis and treatment 6, 7, while the other was treated with cyst aspiration alone.8
Table 1.
Demographic and clinical description of the 8 pediatric patients treated for CHFC. Patients arranged by age at diagnosis.
| Study | Age†/Gender | Size (cm) | Symptoms | Detection | Operation |
|---|---|---|---|---|---|
| Stringer et al.3 | Prenatal/M | 10 × 7.5 × 5 | Yes | Ultrasound | 1. Percutaneous drainage |
| 2. Failed cystojejunostomy (x2) | |||||
| 3. Right trisegmentectomy | |||||
| Betalli et al.6 | Prenatal/F | 4 × 5 | No | Ultrasound | Cyst resection |
| Kim et al.7 | 3 years/M | 2 × 1.5 | No | CT | Cyst resection |
| Carnicer et al.8 | 5 years/F | 2 × 1.3 | No | Ultrasound | Aspiration |
| Vick et al.5 | 14 years/F | 6 (diameter) | Yes | Unknown‡ | Unknown‡ |
| Young et al.9 | 16 years/F | 6 × 3.5 × 3 | Yes | CT | 1. Percutaneous drainage |
| 2. Sclerotherapy | |||||
| 3. Cyst resection | |||||
| Harty et al.4 | 17 years/F | 8 (diameter) | Yes | Ultrasound | Cyst resection |
| Zaydfudim et al.* | 17 years/F | 6.5 × 4.5 × 6.3 | Yes | Ultrasound | Cyst resection |
Present study
Age at the time of diagnosis
Patient derived from pathology series. Information on diagnosis and treatment is unknown
M (Male)
F (Female)
CT (computed tomography)
cm (centimeters)
Interestingly, all four of the teenage girls initially presented with complaints of right upper quadrant pain, jaundice, or portal obstruction.4, 5, 9 At the time of cyst excision, in the three patients that underwent an operation, the average cyst dimensions exceeded 6 cm. In the fourth teenager, non-operative management consisting of cyst aspiration combined with sclerotherapy was unsuccessful and cyst excision was subsequently performed due to fluid reaccumulation.9
There are three reported cases (two males and one female) of malignant transformation from CHFC to squamous cell carcinoma. All patients were diagnosed between 21 and 51 years of age, and presented with either epigastric or right upper quadrant pain.10–12 Although one report lacked clinical follow-up, the other two cases noted aggressive tumor behavior with widespread disease recurrence and progression. One patient was diagnosed with a “hepatic cyst” in childhood, which was observed, and was later surgically treated for CHFC and squamous cell carcinoma at 21 years of age. At operation, the patient had contiguous spread of the squamous cell carcinoma to the transverse mesocolon, stomach, and right colon. He underwent a right hepatectomy with en block resection of the tumor including a right hemicolectomy and partial gastrectomy. Unfortunately, he succumbed to metastatic disease 9 months after surgical resection.11 The other patient was a 51 year-old male who was treated at the time of diagnosis. At operation, he was noted to have contiguous tumor extension to the mesentery, gastrohepatic ligament, and duodenum. A non-anatomic en block resection specimen included CHFC, gallbladder, part of the right hepatic lobe and duodenal wall involved by squamous cell carcinoma. The patient died of disease recurrence two months after the operation.10
In summary, there are an estimated 90 reported cases of CHFC. Eight reports involve children, and 3 reports describe progression to squamous cell carcinoma at various ages. At present, there are no evidence-based recommendations for routine surveillance for either cyst recurrence or progression to malignancy following complete cyst excision. Although these lesions are rare and sometimes difficult to diagnose, there is a poor prognosis once malignant transformation has occurred. Thus, we favor timely radiologic and, if needed, histologic evaluation when a child presents with a hepatic cyst. If CHFC is suspected or diagnosed, prompt cyst excision should be performed.
Acknowledgments
We would like to thank Aaron Shaver, MD (Department of Pathology) for providing the histopathology photographs. This study was supported in part by the National Research Service Award T32HS013833 (VZ) from the Agency of Healthcare Research and Quality, and by the National Institute of Diabetes and Digestive and Kidney Disease Training Grant 2T32DK007673-13 (MR); both from the National Institutes of Health and US Department of Health and Human Services.
Footnotes
Presented at the 2009 Southeastern Surgical Congress, February 7-10 2009; Atlanta, Georgia
References
- 1.Wheeler DA, Edmondson HA. Ciliated hepatic foregut cyst. Am J Surg Pathol. 1984;8:467–70. doi: 10.1097/00000478-198406000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Sharma S, Corn A, Kohli V, Wright HI, Sebastian A, Jabbour N. Ciliated hepatic foregut cyst: an increasingly diagnosed condition. Dig Dis Sci. 2008;53:2818–21. doi: 10.1007/s10620-008-0203-4. [DOI] [PubMed] [Google Scholar]
- 3.Stringer MD, Jones MO, Woodley H, Wyatt J. Ciliated hepatic foregut cyst. J Pediatr Surg. 2006;41:1180–3. doi: 10.1016/j.jpedsurg.2006.01.068. [DOI] [PubMed] [Google Scholar]
- 4.Harty MP, Hebra A, Ruchelli ED, Schnaufer L. Ciliated hepatic foregut cyst causing portal hypertension in an adolescent. AJR Am J Roentgenol. 1998;170:688–90. doi: 10.2214/ajr.170.3.9490954. [DOI] [PubMed] [Google Scholar]
- 5.Vick DJ, Goodman ZD, Deavers MT, Cain J, Ishak KG. Ciliated hepatic foregut cyst: a study of six cases and review of the literature. Am J Surg Pathol. 1999;23:671–7. doi: 10.1097/00000478-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Betalli P, Gobbi D, Talenti E, Alaggio R, Gamba P, Zanon GF. Ciliated hepatic foregut cyst: from antenatal diagnosis to surgery. Pediatr Radiol. 2008;38:230–2. doi: 10.1007/s00247-007-0648-1. [DOI] [PubMed] [Google Scholar]
- 7.Kim S, White FV, McAlister W, Shepherd R, Mychaliska G. Ciliated hepatic foregut cyst in a young child. J Pediatr Surg. 2005;40:e51–3. doi: 10.1016/j.jpedsurg.2005.07.061. [DOI] [PubMed] [Google Scholar]
- 8.Carnicer J, Duran C, Donoso L, Saez A, Lopez A. Ciliated hepatic foregut cyst. J Pediatr Gastroenterol Nutr. 1996;23:191–3. doi: 10.1097/00005176-199608000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Young AS, Nicol KK, Teich S, Ii WE. Catheter-based drainage and agitation for definitive cytological diagnosis of a ciliated hepatic foregut cyst in a child. Pediatr Dev Pathol. 2007;10:153–6. doi: 10.2350/06-06-114.1. [DOI] [PubMed] [Google Scholar]
- 10.Vick DJ, Goodman ZD, Ishak KG. Squamous cell carcinoma arising in a ciliated hepatic foregut cyst. Arch Pathol Lab Med. 1999;123:1115–7. doi: 10.5858/1999-123-1115-SCCAIA. [DOI] [PubMed] [Google Scholar]
- 11.Furlanetto A, Dei Tos AP. Squamous cell carcinoma arising in a ciliated hepatic foregut cyst. Virchows Arch. 2002;441:296–8. doi: 10.1007/s00428-002-0668-z. [DOI] [PubMed] [Google Scholar]
- 12.de Lajarte-Thirouard AS, Rioux-Leclercq N, Boudjema K, Gandon Y, Ramee MP, Turlin B. Squamous cell carcinoma arising in a hepatic foregut cyst. Pathol Res Pract. 2002;198:697–700. doi: 10.1078/0344-0338-00323. [DOI] [PubMed] [Google Scholar]
- 13.Rogers TN, Woodley H, Ramsden W, Wyatt JI, Stringer MD. Solitary liver cysts in children: not always so simple. J Pediatr Surg. 2007;42:333–9. doi: 10.1016/j.jpedsurg.2006.10.024. [DOI] [PubMed] [Google Scholar]


