Abstract
Study Design
Subgroup analysis of prospective, randomized cohort
Objective
To review the results of patients who received opioid pain medications during treatment compared to patients who did not receive opioid medications.
Summary of Background Data
The SPORT trial is a prospective, multicenter study of surgical treatment versus nonoperative treatment for lumbar intervertebral disk herniation (IDH).
Methods
The study population includes patients enrolled in SPORT for treatment of IDH in combined randomized and observational cohorts. Patients who received opioid medications at baseline (Opioid) were compared to those who did not. (No-Opioid)
Results
There were 520 patients in the Non-Opioid group and 542 patients in the Opioid group. Among the opioid medication group there were significantly (p<0.001) worse baseline scores in primary and secondary outcome measures. There was an increased percentage of patients in the opioid medication group with the perception of worsening symptoms and neurological deficit (p<0.001). A higher percentage of the opioid patients received surgery (p<0.001)
At four years follow-up, there were no significant differences in primary or secondary outcome measures or treatment effect of surgery between opioid and non-opioid medication patients. Opioid medications were associated with increased crossover to surgical treatment (p=0.005) and decreased surgical avoidance. (p=0.01)The incidence of opioid use at four years was 16% among patients who were using opioids at baseline and 5% among patients who were not using opioids at baseline.
Conclusion
Patients who were treated with opioids had significantly worse baseline pain and quality of life. At final follow-up, there was no long term difference in outcome associated with opioid pain medication use. Opioid medications were not associated with surgical avoidance. The majority of patients who use opioids during the study did not continue usage at four years.
Keywords: Disc herniation, lumbar, opioid, Outcomes
Introduction
The SPORT trial is a prospective, multicenter trial of surgical versus nonsurgical treatment of common lumbar degenerative conditions. Treatment options for lumbar intervertebral disk herniation includes medication, therapy, nonsurgical interventions, and/or surgery. Medical management of the symptoms of intervertebral disk herniation can include anti-inflammatory medications, muscle relaxants, or opioid medications.
First line medications recommended in the treatment of acute lumbar pain include acetaminophen and NSAIDS. Other options include muscle relaxants, membrane stabilizers, antidepressants and topical analgesics and counter irritants. Opioid analgesics are indicated in patients who have pain despite the aforementioned options that is severe and disabling.
Opioid medications are quite commonly used for treatment of both acute and chronic pain, despite the side effects. Acetaminophen/hydrocodone was the most prescribed drug in the United States in 2005. There have been large increases in the use of opioid medications in the United States. [1] Opioid use has increased significantly in the past decade and the cost of prescription opioid was estimated to be up to 8.6 billion dollars in 2001.[2, 3] Potential benefits of opioid use in patients with severe unremitting pain include decreased pain levels, functional improvement, improved mood and social function.
However, there are significant concerns regarding dangers of opioids resulting from side effects, abuse, diversion to individuals who are not patients, and overdose. Also, the use of opioids on an ongoing basis would be expected to lead to tolerance and escalating doses of medication. Opioid- induced hyperalgesia [4] may result in a lowering of the pain threshold with escalating pain in the face of increasing opioid doses. [5] There are other serious medical complications of opioid use [6] including altered mental status, cognitive impairment, delirium, gastrointestinal, osteoporosis,[7] endocrine side effects,[8] and genitourinary side effects. Diversion of opioid medications is also a significant concern. [9] Nonmedical use of acetaminophen/hydrocodone and oxycodone was admitted by 9.5% and 5.5% of 12th graders, respectively, in 2005. Hospitalizations for poisoning by prescription opioids, sedatives, and tranquilizers increased 65% from 1999 to 2006.[10] Opioid analgesic poisoning resulted in more than 5,000 deaths in 2002, which was more than either heroin or cocaine. [11] Unintentional poisoning was second only to motor vehicle crashes as a cause of unintentional death in persons aged 35 to 54 years in 2005.[12] The rate of iatrogenic addiction is estimated at 0.27% in a meta-analysis of opioids for noncancer pain. [13] Despite these concerns, the incidence of opiate medication use has increased significantly compared to other nonpain-related medications in the Medicare population. [14]
The SPORT is a prospective study comparing surgical versus nonsurgical treatment of common lumbar degenerative conditions. In the SPORT lumbar disk herniation study, approximately 40–49% of patients were treated with opioid analgesics during the pre-enrollment period and 35–46% during the treatment period. [15–18] The purpose of this study was to determine the effect of opioid medication use on the outcome of surgical and nonsurgical treatment of lumbar disk herniation. Theoretically, palliation of pain with opioid medications may maximize participation in rehabilitation and nonoperative treatment while allowing for the favorable natural history of radiculopathy due to lumbar disc herniation to proceed, potentially leading to surgical avoidance. It may be expected that opioid medication treatment will result in improvement in pain control while the patient is being treated with the drug. However, in order to offset the risks of opioid use including dependence, hyperalgesia,[4] daytime sleepiness and lost productivity [19], and overdose [12], and incident long term use in 7% of opioid naïve patients at 2 years [20], it may be argued that a long term benefit in outcome should be present to offset the possible long term risks.
The specific questions to be answered in this study include: (1) Is there a sustained improvement in outcome associated with opioid pain medication use in surgically or nonsurgically treated patients?; (2) Are there more complications in surgically treated patients who are exposed to preoperative opioids?; (3) Does use of opioid pain medications lead to surgical avoidance?
Methods
Study Design
SPORT was conducted at thirteen multidisciplinary spine practices in eleven states across the United States. The details of methods have been reported previously. [15–18]
Patients
The human subject committees at each center approved the standardized protocol. Inclusion criteria for the study were patients over eighteen years of age with six weeks of radicular pain with positive nerve root tension sign and/or neurological deficit. The diagnosis of radiculopathy was confirmed by cross-sectional images that demonstrated intervertebral disc herniation at the level that corresponds to symptoms. Exclusion criteria included caudaequina syndrome, progressive neurologic deficit, malignancy, scoliosis of >15°, herniation cephalad to L2, prior back surgery, and other established contra indications to elective surgery. Patients were offered participation in either a randomized or observational cohort. Because of extensive crossover in the randomized cohort and similar baseline characteristics and outcome between randomized and observational patients when analyzed by treatment, the two groups were combined in this “as-treated” analysis. Patients were considered “surgically assigned” if they were randomized to surgery or chose surgical treatment in the observational cohort.
Study Interventions
The surgery patients were designated to receive lumbar diskectomy. The non operative protocol was “usual recommended care,” which included, at least, active physical therapy, education and counseling with instructions regarding home exercise, non-steroidal anti-inflammatory drugs, or opioid pain medications.
Study Measures
Data used in this study was obtained prospectively, and reviewed retrospectively from patient questionnaires completed at baseline, six weeks, three months, six months, one year, two years, three years, and four years following surgery. Primary outcome measures included the bodily pain (BP), physical function (PF), and mental component summary (MCS) domains of the SF-36 and the American Academy of Orthopaedic Surgeons version of the Oswestry Disability Index (ODI). Secondary measures included patient self-reported improvement, work status, and satisfaction with current symptoms. Symptom severity was measured by the low back pain bothersomeness scale (LBP), sciatica bothersomeness (SBI) and leg pain bothersomeness (LPI) indices. The SF-36 scales and the ODI range from 0 to 100, the SBI from 0 to 24, and the LBP scale from 0 to 6. Higher scores indicate more severe symptoms on the ODI, SBI, and low back pain bothersomeness scale, whereas higher scores indicate less severe symptoms on the SF-36.
Comparison
The change in primary and secondary outcome measures in patients who received opioid pain medication at enrollment in SPORT (Opioid) was compared to patients who did not receive opioid medication prior to enrollment in SPORT (Non-Opioid) (Figure 1). Opioid pain medications were defined as any medication containing hydrocodone, oxycodone, oxycontin, morphine, fentanyl, or hydromorphone. Tramadol and propoxyphene were excluded.
Figure 1.
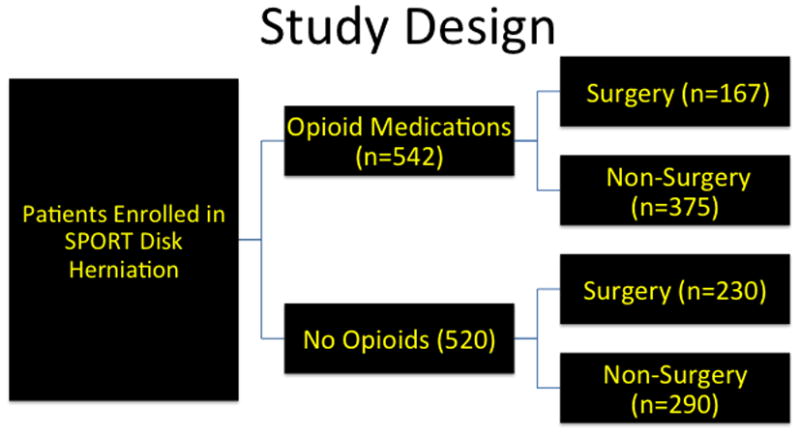
Diagram displaying the enrollment and study design.
Statistical Analysis
Baseline characteristics between the groups were compared using a chi-square test for categorical variables and a t-test for continuous variables. Outcomes were analyzed using longitudinal mixed effect models with random individual effect to account for repeated individual observations over time. Covariate adjustment predicted missing data, treatment received, baseline differences, and outcomes included in the model. In addition, outcome, center, age and gender were included in all longitudinal outcome models. All analyses are as-treated, and treatment is considered a time-varying covariate. Therefore, patients categorized at each time-point either received or did not receive surgical treatment. Follow-up times were measured from the beginning of treatment, and baseline covariates were updated at the time of surgery. All observations prior to surgery are considered in the non-operative estimate with follow-up time measured from enrollment. All observations following surgery contribute to the surgical estimate with follow-up time measured from time of surgery. Secondary and binary outcomes were analyzed using generalized estimation equations (GEE) that assumed a compound symmetry working correlation structure. Outcome comparisons between the opioid and No-opioid groups are made at each time-point with multiple degrees of freedom using Wald tests. Across the four-year follow-up, overall comparisons of area-under-the-curve were made by using a Wald test. Analyses were performed with the SAS PROC MIXED and PROC GENMOD procedures (SAS version 9.2, Windows ZP Pro, Cary, NC). Statistical significance is defined as p<0.05 based on a two-sided hypothesis with no adjustment made for multiple comparisons.
Results
There were 520 patients in the Non-Opioid group and 542 patients in the Opioid group (Figure 1). Demographic characteristics are displayed in Table 1. At baseline, there was significantly increased disability (18% vs 9% p<0.001), compensation claims (Opioid 24% vs Non-Opioid 13%, p<0.001), and smoking (29% vs 19%, p<0.001) among the opioid medication patients (542/1244 IDH patients). There was a lower rate of college education in the Opioid patients (Opioid 71% vs Non-Opioid 78%, p=0.009). There was a difference in body mass index in the Opioid group (Opioid 28.6 vs Non-Opioid 27.4, p<0.001) and Other unlisted comorbidities (Opioid 50% vs Non-Opioid 40%, p=0.001).
Table 1.
Patient Baseline Demographic Characteristics, Comorbid Conditions, Clinical Findings, and Health Status Measures.
| Characteristics IDH (RCT & OBS) |
Non-Opioid (n=520) | Opioid (n=542)* | p-value |
|---|---|---|---|
| Mean Age (SD) | 41.8 (11.5) | 41.8 (10.9) | 0.97 |
| Female - no.(%) | 212 (41%) | 245 (45%) | 0.16 |
| Ethnicity: Not Hispanic† | 497 (96%) | 518 (96%) | 0.88 |
| Race - White† | 446 (86%) | 479 (88%) | 0.24 |
| Education - At least some college | 406 (78%) | 384 (71%) | 0.009 |
| Income - Under $50,000 | 224 (43%) | 252 (46%) | 0.29 |
| Marital Status - Married | 366 (70%) | 385 (71%) | 0.87 |
| Work Status | <0.001 | ||
| Full or part time | 352 (68%) | 283 (52%) | |
| Disabled | 49 (9%) | 100 (18%) | |
| Other | 119 (23%) | 158 (29%) | |
| Compensation - Any‡ | 66 (13%) | 129 (24%) | <0.001 |
| Mean Body Mass Index (BMI), (SD)§ | 27.4 (5.2) | 28.6 (5.8) | <0.001 |
| Smoker | 99 (19%) | 158 (29%) | <0.001 |
| Comorbidities - no.(%) | |||
| Depression | 60 (12%) | 72 (13%) | 0.44 |
| Joint Problem | 95 (18%) | 106 (20%) | 0.65 |
| Diabetes | 19 (4%) | 25 (5%) | 0.53 |
| Other¶ | 208 (40%) | 271 (50%) | 0.001 |
| Time since recent episode < 6 months | 403 (78%) | 431 (80%) | 0.47 |
| SF-36 scores, mean (SD)†† | |||
| Bodily Pain (BP) | 32.8 (21.1) | 19.5 (15.1) | <0.001 |
| Physical Functioning (PF) | 44.6 (25) | 28.9 (22.8) | <0.001 |
| Mental Component Summary (MCS) | 46.6 (11.5) | 43 (11.3) | <0.001 |
| Physical Component Summary (PCS) | 32.6 (8.5) | 27.8 (7.3) | <0.001 |
| Oswestry (ODI) (SD)‡‡ | 43 (20.3) | 58.5 (18.5) | <0.001 |
| Sciatica Frequency Index (0–24) (SD)§§ | 14.5 (5.4) | 17.4 (4.8) | <0.001 |
| Sciatica Bothersome Index (0–24) (SD)§§ | 14.4 (5.2) | 17.1 (4.8) | <0.001 |
| Back Pain Bothersomeness (0–6)(SD)¶¶ | 3.7 (1.9) | 4.2 (1.9) | <0.001 |
| Satisfaction with symptoms - very dissatisfied | 391 (75%) | 480 (89%) | <0.001 |
| Patient self-assessed health trend - no.(%) | <0.001 | ||
| Getting better | 92 (18%) | 64 (12%) | |
| Staying about the same | 249 (48%) | 222 (41%) | |
| Getting worse | 178 (34%) | 251 (46%) | |
| Treatment preference at baseline - no.(%) | <0.001 | ||
| Preference for non-surg | 209 (40%) | 132 (24%) | |
| Not sure | 93 (18%) | 82 (15%) | |
| Preference for surgery | 217 (42%) | 326 (60%) | |
| Pain Radiation | 506 (97%) | 530 (98%) | 0.76 |
| Straight Leg Raise Test - Ipsilateral | 311 (60%) | 365 (67%) | 0.013 |
| Straight Leg Raise Test - Contralateral/Both | 79 (15%) | 90 (17%) | 0.59 |
| Any Neurological Deficit | 366 (70%) | 439 (81%) | <0.001 |
| Reflexes - Asymmetric Depressed | 195 (38%) | 227 (42%) | 0.16 |
| Sensory - Asymmetric Decrease | 234 (45%) | 307 (57%) | <0.001 |
| Motor - Asymmetric Weakness | 198 (38%) | 251 (46%) | 0.008 |
| Herniation Level | 0.36 | ||
| L2–L3/L3–L4 | 31 (6%) | 43 (8%) | |
| L4–L5 | 194 (37%) | 209 (39%) | |
| L5–S1 | 294 (57%) | 290 (54%) | |
| Herniation Type | 0.002 | ||
| Protruding | 162 (31%) | 123 (23%) | |
| Extruded | 328 (63%) | 370 (68%) | |
| Sequestered | 29 (6%) | 49 (9%) | |
| Posterolateral herniation | 400 (77%) | 423 (78%) | 0.72 |
| Received surgery** | 306 (59%) | 407 (75%) | <0.001 |
Race or ethnic group was self-assessed. Whites and blacks could be either Hispanic or non-Hispanic.
This category includes patients who were receiving or had applications pending for workers compensation, Social Security compensation, or other compensation.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Other indicates problems related to stroke, diabetes, osteoporosis, cancer, fibromyalgia, chronic fatigue syndrome (CFS), post traumatic stress disorder (PTSD), alcohol, drug dependence, heart, lung, liver, kidney, blood vessel, nervous system, hypertension, migraine, anxiety, stomach or bowel.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Sciatica Bothersomeness index range from 0 to 24, with lower scores indicating less severe symptoms.
The Low Back Pain Bothersomness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms.
Among total of 1244 IDH patients, 541 did not use opioid at enrollment (Non-Opioid group), 567 used opioid at enrollment (Opioid group), and 136 had no information. 520 out of 541 Non-Opioid patients and 542 out of 567 Opioid patients had at least one follow-up through 4 years and were included in the current analysis dataset.
Received surgical treatment during the first 4 years of enrollment.
Differences between groups in primary and secondary outcome measures are reviewed in Table 1. In the Opioid group, there was significantly worse baseline SF36 BP (Opioid 19.5 vs Non-Opioid 32.8, p<0.001), SF36 PF (Opioid 28.9 vs Non-Opioid 44.6, p<0.001), SF36 MCS (Opioid 43 vs Non-Opioid 46.6, p<0.001), SF36 PCS (Opioid 27.8 vs Non-Opioid 32.6, p<0.001), ODI (Opioid 58.5 vs Non-Opioid 43, p<0.001), Sciatica Frequency Index (Opioid 17.4 vs Non-Opioid 14.5, p<0.001), Sciatica Bothersomeness Index (Opioid 17.1 vs Non-Opioid 14.4, p<0.001), Back Pain Bothersomeness Index (Opioid 4.2 vs Non-Opioid 3.7, p<0.001), and percent dissatisfaction with current symptoms (Opioid 89% vs Non-Opioid 75%, p<0.001). There was an increased percentage of patients in the Opioid medication group with the perception of worsening symptoms (Opioid 46% vs Non-Opioid 34%, p<0.001). There was an increased preference for surgery among the Opioid patients (Opioid 60% vs Non-Opioid 42%, p<0.001).
Baseline differences in symptom severity and clinical presentation are reviewed in Table 1. There was an increased percentage of any neurological deficit (Opioid 81% vs Non-Opioid 70%, p<0.001), motor weakness (Opioid 46% vs Non-Opioid 38%, p<0.008), decreased sensation (Opioid 57% vs Non-Opioid 45%, p<0.001), protruding herniation (Opioid 23% vs Non-Opioid 31% p=0.002) and received surgery in the opioid medication group.
Operative treatments, complications, and events are compared between Opioid and Non- Opioid groups in Table 2. There were no significant differences in procedure details discectomy level between groups. There was an increased percentage of L23 Diskectomy in the opioid group (Opioid 2% vs Non-Opioid 0%, p=0.048). There were no significant differences in operative time, blood loss, blood replacement, intraoperative replacement, post operative transfusion, length of stay, intraoperative complications (including dural tear), length of stay, mortality, or postoperative complications (hematoma, infection), or additional surgeries between groups..
Table 2.
Operative treatments, complications and events.
| Characteristics IDH (RCT & OBS) |
Non-Opioid (n=304) | Opioid (n=406)* | p-value |
|---|---|---|---|
| Discectomy Level | |||
| L2–L3 | 1 (0%) | 10 (2%) | 0.048 |
| L3–L4 | 9 (3%) | 15 (4%) | 0.73 |
| L4–L5 | 113 (37%) | 162 (40%) | 0.47 |
| L5–S1 | 186 (62%) | 224 (56%) | 0.15 |
| Operation time | 75.5 (33.9) | 77.1 (37.9) | 0.56 |
| Blood loss | 63.7 (95.1) | 63.2 (103.4) | 0.94 |
| Blood Replacement | |||
| Intraoperative replacement | 2 (1%) | 3 (1%) | 0.74 |
| Post-operative transfusion | 0 (0%) | 0 (0%) | |
| No. of days in hospital (SD) | 0.94 (0.8) | 0.96 (0.9) | 0.86 |
| Intraoperative complications§ | |||
| Dural tear/spinal fluid leak | 10 (3%) | 10 (2%) | 0.67 |
| Nerve root injury | 0 (0%) | 2 (0%) | 0.61 |
| Other | 2 (1%) | 1 (0%) | 0.80 |
| None | 293 (96%) | 393 (97%) | 0.93 |
| Postoperative complications/events¶ | |||
| Nerve root injury3 | 1 (0%) | 0 (0%) | 0.88 |
| Wound hematoma | 1 (0%) | 2 (0%) | 0.80 |
| Wound Infection | 7 (2%) | 10 (2%) | 0.90 |
| Other4 | 10 (3%) | 14 (3%) | 0.91 |
| None5 | 284 (94%) | 381 (94%) | 0.96 |
| Post-operative mortality (death within 6 weeks of surgery) | 0 (0%) | 0 (0%) | |
| Post-operative mortality (death within 3 months of surgery) | 0 (0%) | 1 (0.1%)‡ | |
| Additional surgeries (1-year rate)|| | 16 (5%) | 26 (6%) | 0.512 |
| Additional surgeries (2-year rate)|| | 19 (6%) | 41 (10%) | 0.069 |
| Additional surgeries (3-year rate)|| | 25 (8%) | 42 (10%) | 0.318 |
| Additional surgeries (4-year rate)|| | 31 (10%) | 47 (12%) | 0.515 |
| Recurrent disc herniation | 16 (5%) | 29 (7%) | |
| Complication or Other | 7 (2%) | 13 (3%) | |
| New condition | 5 (2%) | 4 (1%) |
Surgical information was available for 304 Non-Opioid patients and 406 Opioid patients.
None of the following were reported: aspiration, operation at wrong level, vascular injury.
Patient died after heart surgery at another hospital, the death was judged unrelated to spine surgery.
Any reported complications up to 8 weeks post operation. None of the following were reported: bone graft complication, CSF leak, paralysis, caudaequina injury, wound dehiscence, pseudarthrosis.
One-, two-, three- and four-year post-surgical re-operation rates are Kaplan Meier estimates and p-values are based on the log-rank test. Numbers and percentages are based on the first additional surgery if more than one additional surgery.
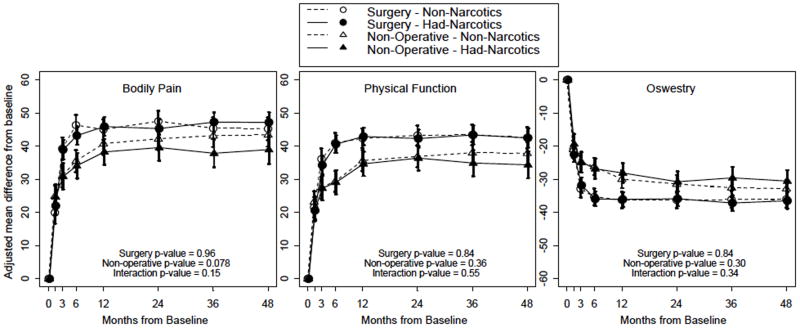
Adjusted changes in outcome measures after surgery are displayed in Table 3. At four years follow-up, there were no significant differences in primary or secondary outcome measures or treatment effect of surgery between Opioid and Non-Opioid medication patients (Table 3). Averaged over four years, there was no significant difference in primary or secondary outcome measures or treatment effect of surgery between groups (Table 4, Figure 2).
Table 3.
| Outcome | Narcotics use at baseline | 1-Year | 2-Year | 3-Year | 4-Year | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||
| IDH | Surgical | Non-operative | Treatment Effect† (95% CI) | Surgical | Non-operative | Treatment Effect† (95% CI) | Surgical | Non-operative | Treatment Effect† (95% CI) | Surgical | Non-operative | Treatment Effect† (95% CI) | |
| SF-36 Bodily Pain (BP) (0–100) (SE)†† | Non-Opioid | 45 (1.6) | 40.7 (1.7) | 4.2 (−0.5, 9) | 47.5 (1.6) | 42.2 (1.7) | 5.3 (0.5, 10.1) | 45.4 (1.7) | 43.1 (1.7) | 2.3 (−2.7, 7.2) | 45.2 (1.8) | 43.4 (1.8) | 1.9 (−3.2, 6.9) |
| Opioid | 45.9 (1.4) | 38.2 (2) | 7.6 (2.7, 12.6) | 45.3 (1.5) | 39.6 (2) | 5.7 (0.7, 10.8) | 47.2 (1.5) | 37.8 (2.2) | 9.4 (4.1, 14.8) | 47.1 (1.6) | 38.9 (2.2) | 8.2 (2.7, 13.7) | |
|
| |||||||||||||
| pvalue | 0.66 | 0.30 | 0.28 | 0.29 | 0.30 | 0.89 | 0.38 | 0.043 | 0.032 | 0.41 | 0.094 | 0.066 | |
|
| |||||||||||||
| SF-36 Physical Function (PF) (0–100) (SE)†† | Non-Opioid | 42.3 (1.5) | 35.6 (1.6) | 6.7 (2.2, 11.3) | 43.2 (1.5) | 36.9 (1.6) | 6.4 (1.8, 10.9) | 43.4 (1.6) | 38 (1.7) | 5.4 (0.8, 10.1) | 42.5 (1.6) | 37.8 (1.7) | 4.7 (−0.1, 9.5) |
| Opioid | 42.9 (1.4) | 34.6 (1.9) | 8.3 (3.5, 13) | 42.3 (1.4) | 36.4 (1.9) | 5.9 (1.1, 10.7) | 43.3 (1.4) | 34.9 (2) | 8.5 (3.4, 13.5) | 42.5 (1.5) | 34.4 (2) | 8.1 (2.9, 13.3) | |
|
| |||||||||||||
| pvalue | 0.77 | 0.67 | 0.60 | 0.64 | 0.83 | 0.89 | 0.98 | 0.20 | 0.33 | 0.99 | 0.16 | 0.29 | |
|
| |||||||||||||
| Mental Component Summary (MCS) (0–100) (SE) †† | Non-Opioid | 8 (0.7) | 5.4 (0.7) | 2.5 (0.6, 4.5) | 5.7 (0.7) | 6.1 (0.7) | −0.4 (−2.3, 1.6) | 6.2 (0.7) | 5.6 (0.7) | 0.6 (−1.4, 2.6) | 6.3 (0.7) | 6 (0.7) | 0.3 (−1.7, 2.4) |
| Opioid | 7.3 (0.6) | 5.8 (0.8) | 1.5 (−0.5, 3.5) | 6.3 (0.6) | 5.7 (0.8) | 0.6 (−1.5, 2.6) | 6.1 (0.6) | 4.7 (0.9) | 1.4 (−0.8, 3.6) | 5.6 (0.6) | 6.2 (0.9) | −0.6 (−2.9, 1.6) | |
|
| |||||||||||||
| pvalue | 0.44 | 0.69 | 0.42 | 0.52 | 0.68 | 0.46 | 0.90 | 0.38 | 0.55 | 0.41 | 0.83 | 0.48 | |
|
| |||||||||||||
| Physical Component Summary (PCS) (0–100) (SE) †† | Non-Opioid | 17 (0.7) | 14.3 (0.7) | 2.6 (0.6, 4.6) | 18.7 (0.7) | 14.9 (0.7) | 3.7 (1.7, 5.7) | 17.2 (0.7) | 15.5 (0.7) | 1.8 (−0.3, 3.8) | 17.5 (0.7) | 15.3 (0.7) | 2.2 (0.1, 4.3) |
| Opioid | 17.4 (0.6) | 13.9 (0.8) | 3.5 (1.4, 5.6) | 17.9 (0.6) | 14.7 (0.8) | 3.2 (1, 5.3) | 18.2 (0.6) | 14.5 (0.9) | 3.7 (1.5, 6) | 18 (0.7) | 13.8 (0.9) | 4.1 (1.9, 6.4) | |
|
| |||||||||||||
| pvalue | 0.61 | 0.65 | 0.49 | 0.37 | 0.84 | 0.67 | 0.25 | 0.38 | 0.15 | 0.60 | 0.18 | 0.17 | |
|
| |||||||||||||
| Oswestry Disability Index (ODI) (0–100) (SE))‡‡ | Non-Opioid | −36.3 (1.3) | −30 (1.4) | −6.2 (−10, −2.4) | −36.3 (1.3) | −31.5 (1.4) | −4.8 (−8.6, −1) | −36.1 (1.3) | −32.6 (1.4) | −3.6 (−7.4, 0.3) | −36 (1.4) | −32.9 (1.4) | −3.2 (−7.1, 0.8) |
| Opioid | −36.1 (1.1) | −28.1 (1.6) | −8 (−11.9, −4) | −35.9 (1.2) | −30.7 (1.6) | −5.1 (−9.2, −1.1) | −37.2 (1.2) | −29.6 (1.7) | −7.6 (−11.8, −3.4) | −36.5 (1.3) | −30.6 (1.7) | −5.9 (−10.2, −1.6) | |
|
| |||||||||||||
| pvalue | 0.92 | 0.32 | 0.48 | 0.82 | 0.72 | 0.89 | 0.54 | 0.14 | 0.12 | 0.79 | 0.26 | 0.30 | |
|
| |||||||||||||
| Sciatica Bothersomeness Index (0–24) (SE)§§ | Non-Opioid | −10.8 (0.4) | −9.5 (0.4) | −1.2 (−2.4, −0.1) | −10.8 (0.4) | −9.7 (0.4) | −1.1 (−2.3, 0) | −10.5 (0.4) | −10 (0.4) | −0.5 (−1.6, 0.7) | −11 (0.4) | −9.9 (0.4) | −1.1 (−2.3, 0.1) |
| Opioid | −10.9 (0.3) | −9 (0.5) | −2 (−3.2, −0.8) | −10.5 (0.3) | −8.9 (0.5) | −1.6 (−2.8, −0.4) | −11 (0.4) | −9.1 (0.5) | −1.9 (−3.2, −0.7) | −11.1 (0.4) | −9.2 (0.5) | −1.9 (−3.2, −0.6) | |
|
| |||||||||||||
| pvalue | 0.74 | 0.30 | 0.30 | 0.54 | 0.19 | 0.53 | 0.26 | 0.14 | 0.058 | 0.86 | 0.29 | 0.35 | |
|
| |||||||||||||
| Low Back Pain Bothersomeness (0–6) (SE)¶¶ | Non-Opioid | −2.1 (0.1) | −1.6 (0.1) | −0.5 (−0.8, −0.2) | −2.1 (0.1) | −1.8 (0.1) | −0.3 (−0.6, 0) | −2.1 (0.1) | −1.9 (0.1) | −0.2 (−0.5, 0.1) | −2 (0.1) | −1.9 (0.1) | −0.1 (−0.5, 0.3) |
| Opioid | −2.1 (0.1) | −1.5 (0.1) | −0.6 (−1, −0.2) | −2.1 (0.1) | −1.6 (0.1) | −0.5 (−0.9, −0.1) | −2.2 (0.1) | −1.4 (0.2) | −0.8 (−1.2, −0.4) | −2.1 (0.1) | −1.5 (0.2) | −0.5 (−0.9, −0.1) | |
|
| |||||||||||||
| pvalue | 0.95 | 0.45 | 0.54 | 0.64 | 0.15 | 0.41 | 0.41 | 0.009 | 0.011 | 0.62 | 0.077 | 0.098 | |
|
| |||||||||||||
| Very/somewhat satisfied with symptoms (%) | Non-Opioid | 71 | 55.6 | 15.4 (5.2, 25.5) | 71.9 | 62.2 | 9.7 (−0.3, 19.7) | 70.1 | 62.8 | 7.3 (−3.1, 17.7) | 73.4 | 58 | 15.3 (4.5, 26.2) |
| Opioid | 68.5 | 53.1 | 15.4 (4.5, 26.3) | 71.3 | 57.8 | 13.5 (2.6, 24.3) | 69 | 59.8 | 9.2 (−2.5, 20.8) | 69.8 | 63.1 | 6.7 (−5.1, 18.5) | |
|
| |||||||||||||
| pvalue | 0.56 | 0.64 | 0.96 | 0.88 | 0.42 | 0.62 | 0.81 | 0.60 | 0.82 | 0.43 | 0.41 | 0.25 | |
|
| |||||||||||||
| Work status: working (%) | Non-Opioid | 88.6 | 84.6 | 4.1 (−3.5, 11.7) | 82.9 | 85.8 | −3 (−11.3, 5.4) | 81.8 | 79 | 2.8 (−7, 12.5) | 85.8 | 75.7 | 10.1 (0, 20.2) |
| Opioid | 85.3 | 79.9 | 5.4 (−3.1, 13.9) | 87.7 | 81.3 | 6.5 (−1.8, 14.7) | 85.8 | 77.3 | 8.5 (−1.3, 18.4) | 85.9 | 71 | 14.9 (3.5, 26.3) | |
|
| |||||||||||||
| pvalue | 0.28 | 0.26 | 0.95 | 0.16 | 0.30 | 0.087 | 0.26 | 0.75 | 0.34 | 0.97 | 0.46 | 0.57 | |
Adjusted for age, gender, marital status, smoking status, race, compensation, herniation location, working status, stomach comorbidity, depression, other** comorbidity, self-rated health trend, duration of most recent episode, treatment preference and baseline score (for SF-36, ODI, and Sciatica Bothersomeness), and center.
Treatment effect is the difference between the surgical and non-operative mean change from baseline. Analysis is done using a mixed model with a random subject intercept term. Surgery is defined as surgery within 3 months of enrollment.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Sciatica Bothersomeness index range from 0 to 24, with lower scores indicating less severe symptoms.
The Low Back Pain Bothersomness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
Other comorbidities include: stroke, diabetes, osteoporosis, cancer, fibromyalgia, chronic fatigue syndrome (CFS), post traumatic stress disorder (PTSD), alcohol, drug dependency, heart, lung, liver, kidney, blood vessel, nervous system, hypertension, migraine, anxiety, stomach, bowel.
Table 4.
Average over four years area under the curve results (per year) from adjusted as-treated outcome analysis by utilization of opioid at enrollment.
| IDH | ESI | Surgical | Non-operative | Treatment Effect† (95% CI) |
|---|---|---|---|---|
| SF-36 Bodily Pain (BP) (0–100) (SE) | Non-Opioid | 44 (1.2) | 39.9 (1.3) | 4.2 (0.5, 7.8) |
| Opioid | 44.1 (1.1) | 36.7 (1.5) | 7.4 (3.6, 11.2) | |
|
| ||||
| pvalue | 0.96 | 0.078 | 0.15 | |
|
| ||||
| SF-36 Physical Function (PF) (0–100) (SE) | Non-Opioid | 41 (1.2) | 34.8 (1.3) | 6.2 (2.6, 9.8) |
| Opioid | 40.7 (1.1) | 33.2 (1.4) | 7.5 (3.8, 11.3) | |
|
| ||||
| pvalue | 0.84 | 0.36 | 0.55 | |
|
| ||||
| Oswestry Disability Index (ODI) (0–100) (SE) | Non-Opioid | −34.8 (1) | −29.9 (1.1) | −4.9 (−7.9, −1.8) |
| Opioid | −35.1 (0.9) | −28.4 (1.2) | −6.7 (−9.9, −3.5) | |
|
| ||||
| pvalue | 0.84 | 0.30 | 0.34 | |
|
| ||||
| Sciatica Bothersomeness Index (0–24) (SE) | Non-Opioid | −9.7 (0.3) | −8.6 (0.3) | −1.1 (−1.9, −0.2) |
| Opioid | −9.8 (0.3) | −8.1 (0.3) | −1.7 (−2.6, −0.8) | |
|
| ||||
| pvalue | 0.78 | 0.17 | 0.20 | |
Figure 2.
Primary Outcomes over Time for Non-Narcotics and Had-Narcotics Use at Baseline. Surgery p-value compares Non-Narcotics to Had-Narcotics among surgery. Non-operative p-value compares Non-Narcotics to Had-Narcotics among non-operative. Interaction p-value compares treatment effect (surgery vs. non-operative) between Non-Narcotics and Had-Narcotics.* P-values are time weighted average 4 years (Area Under Curve p-values).
Crossover between surgically and nonsurgically assigned/chosen Opioid patients is reported in Table 5. There was significantly less crossover from surgical to nonsurgical treatment in the Opioid patients versus the non-Opioid patients (Had-Opioids 11% vs Non-Opioids 19%, p=0.0108). There was significantly increased crossover from nonsurgical treatment to surgery in the Opioid pain medication patients (Had-Opioids 45% vs Non-Opioids 31%, p=0.0045).
Table 5.
Crossover of Assigned/Chosen Treatment Groups up to Four Years Follow-up
| Non-Opioid (n = 520) | Opioid (n = 542) | p-value* | |
|---|---|---|---|
| Assigned/Chose Surgery Crossover to Nonoperative (%) | 54/290 (19%) | 43/375 (11%) | 0.0108 |
| Assigned/Chose Nonoperative Crossover to Surgery (%) | 71/230 (31%) | 75/167 (45%) | 0.0045 |
p-value is from the Chi-square test, which tests whether there is a statistically significant difference in crossover between Non-Opioid and Opioid groups for the surgical group and nonoperative group, respectively.
| Percent Having Surgery (among enrolled)
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Non-Opioid | Opioid | |||||||
|
| ||||||||
| Assigned/Chose Surgery | Assigned/Chose Non operative | Assigned/Chosen Surgery | Assigned/Chose Non operative | |||||
| N | 290 | 230 | 375 | 167 | ||||
|
| ||||||||
| 6W | 194 | 67% | 16 | 7% | 294 | 78% | 27 | 16% |
| 3M | 219 | 76% | 37 | 16% | 319 | 85% | 47 | 28% |
| 6M | 229 | 79% | 55 | 24% | 329 | 88% | 62 | 37% |
| 1Y | 233 | 80% | 64 | 28% | 331 | 88% | 67 | 40% |
| 2Y | 235 | 81% | 67 | 29% | 331 | 88% | 70 | 42% |
| 3Y | 235 | 81% | 68 | 30% | 331 | 88% | 72 | 43% |
| 4Y | 236 | 81% | 71 | 31% | 332 | 89% | 75 | 45% |
The incidence of opioid use at four years among patients who were using opioids at baseline(n=356) was 16% (n=56) at four years (Figure 3, Appendix I). Of the four year followup data available, 5% (n=18) of the non-opioid users at baseline (n=372) were using opioids at four years (Appendix II).
Figure 3.
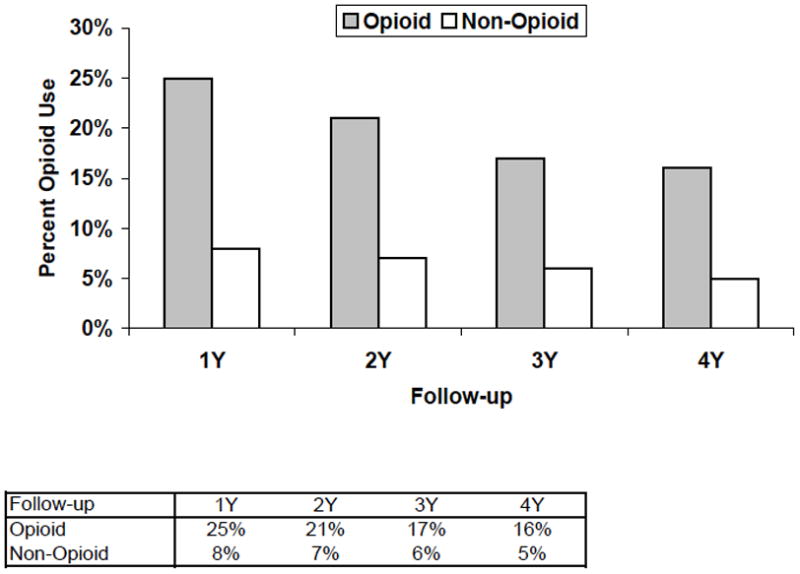
Percentage of patients with long term Narcotic use at one, two, three, and four years. Opioid patient group were patients who were treated with opioid pain medications at the time of enrollment in the study. No-Opioid patients were not treated with opioid pain medications at time of enrollment in the study.
Discussion
The results from our study indicate that there was no difference in outcome at four year followup associated with the usage of opioid pain medications despite the fact that the patients who were using opioids had a significantly worse baseline status. Opioid medications were associated with increased crossover to surgical treatment, although this may be confounded by increased preference for surgery among the Opioid patients at baseline.
Previous SPORT studies have established predictors for long term opioid use among patients. [20] Among participants who admitted opioid use at baseline, 25% reported opioid use at 12 months and 21% reported continued use at 24 months. [20] Of the opioid naïve participants at baseline, 8% reported incident use at 12 months and 7% at 24 months. [20] In this study, the long term (four year) opioid use was 16% among patients using opioids at baseline and 5% among opioid naïve patients. In addition to the incidence of long term opioid use, our aim in this study was to determine the effect of opioids upon change in outcome.
Our results indicate no significant improvement in outcome associated with opioid medications in the treatment of lumbar disk herniation. These results differ from the previous literature on opioid medication in patients with spinal disorders that demonstrates limited efficacy, erratic practice patterns, and poor results. [21] [22] [23] Opioid treatment for more than seven days after a work related back injury has been associated with increased risk of chronic disability and poor long term results. [24] Between 5–25% of patients who are prescribed opioid medications for chronic low back pain have aberrant medication taking-behaviors. [21] Chronic opioid use before cervical arthrodesis has been found to be associated with continued opioid use after surgery and worse functional outcomes following anterior cervical discectomy and fusion. [25] Similar to the results of Khoromi et al [23], there was no improvement or worsening in outcome in this study associated with opioid use. Furthermore, indirect markers of opioid tolerance, such as length of stay, or general postoperative complications, were not different between opioid and non-opioid patients. Additionally, opioid medications did not affect the treatment effect of surgery, suggesting that surgical intervention is equally as effective in patients taking opioids as in those not taking opioids.
Despite using stronger pain medications, patients in this study who received opioids had significantly increased pain and worse quality of life at baseline. The baseline characteristics of these patients are consistent with previous studies that demonstrate increased baseline pain severity and symptom severity is associated with increased Opioid medication use. [26] [27] [28]. Previous studies have estimated that between 3.4%[26] and 42%[20] of spine patients are treated with opioids, although there is tremendous geographic [29] [30], racial [27], and specialty variation in opioid use. [31] There were significant demographic differences between the Opioid and Non-Opioid patient groups in our study suggesting increased disability, obesity, compensation claims, and smoking in the Opioid patients. Other studies have determined that demographic characteristics, including age, depression, personality disorder, and substance abuse, are more predictive of opioid medication use than pain intensity. [32]. From our data, nonsurgically treated patients who received opioid medications were more likely to ultimately undergo surgical treatment, suggesting that the opioid medications did not palliate the symptoms of lumbar disk herniation enough to avoid surgery. Other studies have also demonstrated an increased rate of surgery associated with opioid treatment for low back pain, although this may be confounded by the baseline increase in symptom severity. [33]
Strengths of this study include the large number of patients and followup interval. The strict inclusion criteria of the SPORT also contribute to a homogenous population of patients with lumbar disk herniation and concordant radiculopathy. Most of the previous studies focus on back pain, which is often multifactorial. [33] Therefore, the results of the present analysis may be more applicable to patients with the common clinical scenario of radiculopathy. The methodology of the SPORT study includes both surgically and nonsurgically treated patients and enables comparison of change in outcome in both groups. Previous studies have only included either surgically or nonsurgically treated patients. Weaknesses of this study include the heterogenous group of medications included in the opioids and lack of specific dosages. It is possible that there may be an effect associated with particular medications related to potency or dosage. However, the opioid medication usage is reflective of the variability in clinical practice during the enrollment period of the SPORT study. There was no prior specified subgroup analysis and the authors acknowledge that the opioid and non-opioid medication groups were not balanced at the outset. Opioid medication prescribing is a subjective decision based on numerous factors. As demonstrated in previous studies, opioid use was significantly associated with smoking and heavier body mass index. [27] Additionally, there was no psychological screening tools or opioid risk tools used in this study.
In conclusion, there was no improvement in outcome associated with the use of opioid pain medications in patients with lumbar disk herniation whether treated surgically or nonsurgically. There was also no long term worsening of outcome in patients who were treated with opioid medications and a small percentage of patients who are started on opioid medications will continue to use them four years after initiation. Patients who require opioid medications are more likely to ultimately require surgery. Further study is necessary to determine if the transient pain relief offsets the risks of opioid addition and overdose since there is no long term benefit of opioid medications to patients.
Key Points.
There were no significant differences in primary or secondary outcome measures or treatment effect of surgery between opioid and non-opioid medication patients.
Opioid medications were associated with increased crossover to surgical intervention.
The incidence of opioid use at four years was 16% among patients who were using opioids at baseline and 5% among patients who were not using opioids at baseline.
Despite treatment with stronger pain medications, patients who were treated with opioids had significantly worse baseline pain and quality of life.
Acknowledgments
The manuscript submitted does not contain information about medical device(s)/drug(s). The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention grant funds were received in support of this work. Relevant financial activities outside the submitted work: royalties, stocks, consultancy, grants, board membership.
Contributor Information
Kris Radcliff, Rothman Institute, Thomas Jefferson University, 925 Chestnut Street, Philadelphia, PA 19107.
Mitchell Freedman, Department of Physical Medicine and Rehabilitation, Thomas Jefferson University, Philadelphia, PA.
Alan Hilibrand, Rothman Institute, Thomas Jefferson University, 925 Chestnut Street, Philadelphia, PA 19107.
Roman Isaac, Thomas Jefferson University, Philadelphia, PA.
Jon D. Lurie, Dartmouth Medical, School Hanover, NH.
Wenyan Zhao, Dartmouth Medical School, Hanover, NH.
Alex Vaccaro, Rothman Institute, Thomas Jefferson University, 925 Chestnut Street, Philadelphia, PA 19107.
Todd Albert, Rothman Institute, Thomas Jefferson University, 925 Chestnut Street, Philadelphia, PA 19107.
James Weinstein, Dartmouth Medical School, Hanover, NH, CEO, Dartmouth-Hitchcock Medical Center, Hanover, NH.
References
- 1.Olsen Y, Daumit GL, Ford DE. Opioid prescriptions by U.S. primary care physicians from 1992 to 2001. The journal of pain: official journal of the American Pain Society. 2006;7(4):225–35. doi: 10.1016/j.jpain.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Birnbaum HG, et al. Estimated costs of prescription opioid analgesic abuse in the United States in 2001: a societal perspective. The Clinical journal of pain. 2006;22(8):667–76. doi: 10.1097/01.ajp.0000210915.80417.cf. [DOI] [PubMed] [Google Scholar]
- 3.Colliver JD, KL, Dai L, Gfroerer JC. Misuse of Prescription Drugs: Data from the 2002, 2003, and 2004 National Surveys on Drug Use and Health. Vol. 2006. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2006. Prevalence and recent trends in misuse of prescription drugs. DHHS publication no. SMA 06–4192(Analytic Series A-28.) [Google Scholar]
- 4.Angst MS, Clark JD. Opioid-induced hyperalgesia: a qualitative systematic review. Anesthesiology. 2006;104(3):570–87. doi: 10.1097/00000542-200603000-00025. [DOI] [PubMed] [Google Scholar]
- 5.Mao J, Mayer DJ. Spinal cord neuroplasticity following repeated opioid exposure and its relation to pathological pain. Annals of the New York Academy of Sciences. 2001;933:175–84. doi: 10.1111/j.1749-6632.2001.tb05823.x. [DOI] [PubMed] [Google Scholar]
- 6.Ballantyne JC, Mao J. Opioid therapy for chronic pain. The New England journal of medicine. 2003;349(20):1943–53. doi: 10.1056/NEJMra025411. [DOI] [PubMed] [Google Scholar]
- 7.Daniell HW. Opioid osteoporosis. Archives of internal medicine. 2004;164(3):338. doi: 10.1001/archinte.164.3.338-a. author reply 338. [DOI] [PubMed] [Google Scholar]
- 8.Daniell HW. Opioid endocrinopathy in women consuming prescribed sustained-action opioids for control of nonmalignant pain. The journal of pain: official journal of the American Pain Society. 2008;9(1):28–36. doi: 10.1016/j.jpain.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Fleming MF, et al. Substance use disorders in a primary care sample receiving daily opioid therapy. The journal of pain: official journal of the American Pain Society. 2007;8(7):573–82. doi: 10.1016/j.jpain.2007.02.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coben JH, et al. Hospitalizations for poisoning by prescription opioids, sedatives, and tranquilizers. American journal of preventive medicine. 2010;38(5):517–24. doi: 10.1016/j.amepre.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 11.Kuehn BM. Opioid prescriptions soar: increase in legitimate use as well as abuse. JAMA: the journal of the American Medical Association. 2007;297(3):249–51. doi: 10.1001/jama.297.3.249. [DOI] [PubMed] [Google Scholar]
- 12.Kuehn BM. Alarming nonfatal overdose rates found for opioids, sedatives, and tranquilizers. JAMA: the journal of the American Medical Association. 2010;303(20):2020–1. doi: 10.1001/jama.2010.641. [DOI] [PubMed] [Google Scholar]
- 13.Noble M, et al. Long-term opioid management for chronic noncancer pain. Cochrane database of systematic reviews. 2010;(1):CD006605. doi: 10.1002/14651858.CD006605.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zerzan JT, et al. Trends and geographic variation of opiate medication use in state Medicaid fee-for-service programs, 1996 to 2002. Medical care. 2006;44(11):1005–10. doi: 10.1097/01.mlr.0000228025.04535.25. [DOI] [PubMed] [Google Scholar]
- 15.Weinstein J, et al. Surgical vs. nonoperative treatment for lumbar disc herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451–2459. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weinstein J, et al. Surgical versus Non-Operative Treatment for Lumbar Disc Herniation: Four-Year Results for the Spine Patient Outcomes Research Trial (SPORT) Spine. 2008;33(25):2789. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinstein J, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296(20):2441. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinstein JN, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine. 2008;33(25):2789–800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zgierska A, et al. Sleep and daytime sleepiness problems among patients with chronic noncancerous pain receiving long-term opioid therapy: a cross-sectional study. Journal of opioid management. 2007;3(6):317–27. doi: 10.5055/jom.2007.0020. [DOI] [PubMed] [Google Scholar]
- 20.Krebs EE, et al. Predictors of long-term opioid use among patients with painful lumbar spine conditions. The journal of pain: official journal of the American Pain Society. 2010;11(1):44–52. doi: 10.1016/j.jpain.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martell BA, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Annals of internal medicine. 2007;146(2):116–27. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 22.Dworkin RH, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132(3):237–51. doi: 10.1016/j.pain.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 23.Khoromi S, et al. Morphine, nortriptyline and their combination vs. placebo in patients with chronic lumbar root pain. Pain. 2007;130(1–2):66–75. doi: 10.1016/j.pain.2006.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franklin GM, et al. Early opioid prescription and subsequent disability among workers with back injuries: the Disability Risk Identification Study Cohort. Spine. 2008;33(2):199–204. doi: 10.1097/BRS.0b013e318160455c. [DOI] [PubMed] [Google Scholar]
- 25.Lawrence JT, et al. Preoperative narcotic use as a predictor of clinical outcome: results following anterior cervical arthrodesis. Spine (Phila Pa 1976) 2008;33(19):2074–8. doi: 10.1097/BRS.0b013e3181809f07. [DOI] [PubMed] [Google Scholar]
- 26.Fanciullo GJ, et al. An observational study on the prevalence and pattern of opioid use in 25,479 patients with spine and radicular pain. Spine. 2002;27(2):201–5. doi: 10.1097/00007632-200201150-00016. [DOI] [PubMed] [Google Scholar]
- 27.Stover BD, et al. Factors associated with early opioid prescription among workers with low back injuries. The journal of pain: official journal of the American Pain Society. 2006;7(10):718–25. doi: 10.1016/j.jpain.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 28.Kidner CL, Mayer TG, Gatchel RJ. Higher opioid doses predict poorer functional outcome in patients with chronic disabling occupational musculoskeletal disorders. The Journal of bone and joint surgery American volume. 2009;91(4):919–27. doi: 10.2106/JBJS.H.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luo X, Pietrobon R, Hey L. Patterns and trends in opioid use among individuals with back pain in the United States. Spine. 2004;29(8):884–90. doi: 10.1097/00007632-200404150-00012. discussion 891. [DOI] [PubMed] [Google Scholar]
- 30.Webster BS, et al. Geographic variation in opioid prescribing for acute, work-related, low back pain and associated factors: a multilevel analysis. American journal of industrial medicine. 2009;52(2):162–71. doi: 10.1002/ajim.20655. [DOI] [PubMed] [Google Scholar]
- 31.Turk DC, Brody MC, Okifuji EA. Physicians’ attitudes and practices regarding the long-term prescribing of opioids for non-cancer pain. Pain. 1994;59(2):201–8. doi: 10.1016/0304-3959(94)90072-8. [DOI] [PubMed] [Google Scholar]
- 32.Breckenridge J, Clark JD. Patient characteristics associated with opioid versus nonsteroidal anti-inflammatory drug management of chronic low back pain. The journal of pain: official journal of the American Pain Society. 2003;4(6):344–50. doi: 10.1016/s1526-5900(03)00638-2. [DOI] [PubMed] [Google Scholar]
- 33.Webster BS, Verma SK, Gatchel RJ. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use. Spine. 2007;32(19):2127–32. doi: 10.1097/BRS.0b013e318145a731. [DOI] [PubMed] [Google Scholar]