Abstract
Context:
Two-dimensional (or medial knee displacement [MKD]) and 3-dimensional (3D) knee valgus are theorized to contribute to anterior cruciate ligament injuries. However, whether these displacements can be improved in the double-legged squat (DLS) after an exercise intervention is unclear.
Objective:
To determine if MKD and 3D knee valgus are improved in a DLS after an exercise intervention.
Design:
Randomized controlled clinical trial.
Setting:
Research laboratory.
Patients or Other Participants:
A total of 32 participants were enrolled in this study and were randomly assigned to the control (n = 16) or intervention (n = 16) group. During a DLS, all participants demonstrated knee valgus that was corrected with a heel lift.
Intervention(s):
The intervention group completed 10 sessions of directed exercise that focused on hip and ankle strength and flexibility over a 2- to 3-week period.
Main Outcome Measure(s):
We assessed MKD and 3D knee valgus during the DLS using an electromagnetic tracking system. Hip strength and ankle-dorsiflexion range of motion were measured. Change scores were calculated for MKD and 3D valgus at 0%, 10%, 20%, 30%, 40%, and 50% phases, and group (2 levels)-by phase (6 levels) repeated-measures analyses of variance were conducted. Independent t tests were used to compare change scores in other variables (α < .05).
Results:
The MKD decreased from 20% to 50% of the DLS (P = .02) and 3D knee valgus improved from 30% to 50% of the squat phase (P = .001). Ankle-dorsiflexion range of motion (knee extended) increased in the intervention group (P = .009). No other significant findings were observed (P > .05).
Conclusions:
The intervention reduced MKD and 3D knee valgus during a DLS. The intervention also increased ankle range of motion. Our inclusion criteria might have limited our ability to observe changes in hip strength.
Key Words: movement analysis, screening, anterior cruciate ligament, dynamic knee valgus, dorsiflexion
Key Points.
A systemic corrective exercise program decreased 2- and 3-dimensional knee valgus and increased ankle-dorsiflexion flexibility during a double-legged squat.
Hip-extension and -abduction strength increased after the exercise program, but the findings were not statistically significant.
Knee valgus is believed to be a major contributor to noncontact anterior cruciate ligament (ACL) injuries.1 Three-dimensional (3D) assessment of knee-valgus angle (3D knee valgus) is considered the gold standard method of measurement; it is assessed via motion analysis and describes the relative relationship between the femur and tibia. However, 2-dimensional (2D) knee-valgus assessment methods are popular because of low cost, ease of implementation, and the ability to screen large numbers of participants.2,3 Various methods of calculating 2D knee valgus have been reported in the literature and have been referred to as knee-separation distance, frontal-plane projection angle, and medial knee displacement (MKD).2,4–6 All of these measurements assess frontal-plane knee motion and use combinations of standard video cameras, basic editing software, and motion analysis, depending on the measure of interest.
Knee valgus results from a combination of femoral and tibial motions, which can be influenced by the joints proximal and distal to the knee, including the trunk, hip, and ankle.7–11 Lack of femoral control can result in excessive adduction and internal rotation, which can stress the ACL.10,12 However, the relationship between hip-muscle strength and frontal-plane knee motion is not as clear as one might expect.5,8,13 For example, Thijs et al14 calculated 2D valgus angles during a lunge and observed no relationship between frontal-plane motion and hip-muscle strength. Norcross et al13 also observed no relationship between isometric or eccentric hip strength (hip abductor and external rotation) and 3D knee valgus during a lateral step-down test. Additionally, Bell et al9 concluded that their participants had adequate hip strength and range of motion (ROM) despite excessive MKD during a double-legged squat (DLS). Yet these findings contrast with those of other authors4,15 who have observed relationships between hip strength and knee motion. Further research is needed to definitively describe the relationships between hip-muscle strength and frontal-plane knee motion.
Foot pronation and limited ankle dorsiflexion are also believed to influence knee valgus.7–9,12 Rabin and Kozol8 grouped individuals based on performance during a lateral step-down test. Females with worse movement quality (including knee position, pelvic position, and trunk movement) had restricted ankle-dorsiflexion motion as a result of gastrocnemius and soleus tightness. These results were similar to the findings of Bell et al,9 who examined hip and ankle strength and ROM based on movement during the DLS. Participants with visual knee valgus were compared with those who kept their knees over their toes during the DLS. The valgus group tended to have soleus-restricted ankle ROM. Thus, limited ankle dorsiflexion is believed to result in biomechanical compensations at the knee by increasing subtalar pronation and tibial abduction and internal rotation,12 which are components of knee valgus.10 Because excessive knee valgus (MKD and 3D) is most likely caused by a combination of hip- and ankle-muscle imbalances, comprehensive strategies that focus on the joints proximal and distal to the knee should be investigated to determine if knee alignment can be corrected during functional tasks.
Interventions have been developed to reduce the risk of lower extremity injury.16–19 In a recent review20 of intervention programs, the authors concluded that many focus on limiting valgus positioning during dynamic activity. In fact, participation in an injury prevention program may be most beneficial to individuals with poor movement quality.21,22 Identifying and classifying individuals based on performance during functional tasks is common.8,9,23–25 They are observed during squatting or jumping to identify poor movement quality, which is theorized to increase the risk of injury. For example, Myer et al21 classified female athletes into high-risk and low-risk categories based on external knee-abduction moment. After completing a training program, participants with greater levels of abduction moment, and thus theoretically higher risk, reduced abduction moment postintervention. DiStefano et al22 observed similar results when athletes were grouped using a clinical screening examination that incorporated 2D videography (Landing Error Scoring System). When compared with individuals who had better landing mechanics, those with poorer landing mechanics improved their scores in response to an exercise intervention. Identifying poor movement patterns allows clinicians to prescribe focused corrective exercise interventions to high-risk individuals.
The DLS test is a common screening task used during functional movement examinations.26,27 During the DLS test, a participant squats 5 times; if visual knee valgus is observed, then 2-in (5.08-cm) heel lifts are placed under both heels, and 5 additional squats are performed.9,23 Squatting on a heel lift is theorized to differentiate between ankle and hip-muscle imbalance as the primary contributor to dynamic knee valgus.9,23 As previously mentioned, if visual knee valgus is corrected when the squats are performed on the lift, then restrictions in ankle motion (restricted dorsiflexion) are thought to be the primary contributor to knee valgus.9 The heel lift results in ankle plantar flexion and alleviates the dorsiflexion restriction caused by the gastrocnemius and soleus, thereby normalizing knee alignment during the squat. Previous researchers9,23 using this classification system have observed that participants with dynamic valgus that is corrected by a heel lift have tight and weak ankle plantar flexors compared with individuals with proper squat technique. However, to our knowledge, no investigators have determined if knee valgus can be altered in individuals who have been screened via this classification system.
The primary purpose of our study was to determine if an exercise training program could decrease knee valgus during the DLS in individuals with visually identified knee valgus that was corrected with a heel lift. A secondary purpose was to determine if the training program could alter hip strength and ankle-dorsiflexion ROM, because these factors are believed to be related to knee-valgus alignment. Our general hypothesis was that knee valgus would be improved after a comprehensive training program focused on the joints proximal and distal to the knee as a result of improved hip strength and increased ankle ROM.
METHODS
Participants
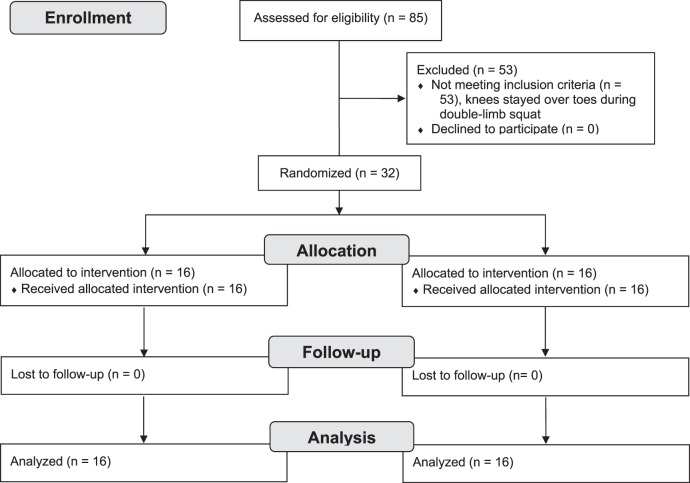
All volunteers read and signed an informed consent agreement approved by the university's institutional review board before participation. Testing took place in a sports medicine research laboratory. Sample size was calculated based on pilot data and previous literature.28 With 11 participants in each group, we had 80% power (α = .05) to detect a clinically relevant 50% improvement in MKD and 3D knee valgus across squat phases. A total of 85 volunteers were screened for enrollment in the study by performing the DLS test, which consisted of 5 squats from a standardized position: feet shoulder-width apart, toes straight ahead, hands overhead with elbows locked.9,23 All participants had visually identified knee valgus that was corrected when a second set of 5 squats was performed on heel lifts.9 Visual valgus was considered present when the midpoint of the patella passed medial to the great toe in 3 of 5 squats.9 We followed previously published classification guidelines9 to increase group homogeneity: (1) a categorical yes–no grading system, in which participants were classified as either having or not having excessive visual knee valgus, (2) participants with questionable excessive knee valgus were not included in the study, and (3) all participants were screened live in real time, similar to how they would be screened in a clinical setting by the primary investigator (D.R.B.). Other inclusion criteria were age 18 to 35 years and no current or previous musculoskeletal injuries in the past 6 months. A total of 32 volunteers met all criteria and were randomly assigned to either a control (CON: age = 20.4 ± 2.9 years, height = 168.2 ± 6.7 cm, mass = 62.5 ± 9.3 kg) or intervention (INT: age = 20.9 ± 2.6 years, height = 169.8 ± 6.4 cm, mass = 66.3 ± 12.1 kg) group via coin flip and a test-retest study design was used (Figure). We tried to equally distribute sexes between groups; however, 3 men were enrolled in the study, resulting in an uneven distribution between groups (CON = 2 men, INT = 1 man). All enrollees completed the study. Blinding the investigators was not feasible. Intrarater reliability coefficients (3,1) for all variables ranged from 0.85 to 0.99.
Figure.
Participant enrollment, allocation, follow-up, and analysis.
Instrumentation
Kinematic data were collected at 100 Hz using an electromagnetic tracking system (Ascension Technologies, Burlington, VT) interfaced with MotionMonitor software (version 8.0; Innovative Sports Training, Chicago, IL). Mean isometric force data were collected using a handheld dynamometer (model Chatillon MSC-500; AMETEK, Largo, FL) and ROM was assessed using a standard 12-in (30.48-cm) goniometer.
Procedures
Demographic information was recorded, and then participants warmed up on a cycle ergometer at a self-selected pace for 5 minutes. Testing was performed on the dominant leg, which was defined as the leg used to kick a ball for maximal distance. Electromagnetic sensors were placed over the apex of the sacrum, midpoint of the lateral thigh, and medial tibia using double-sided tape and elastic wrap. Participants stood in neutral position while the bony landmarks were digitized: the medial and lateral epicondyles of the femur, the medial and lateral malleoli of the ankle, and the left and right anterior-superior iliac spines. The epicondyle and malleolus digitization points were used to calculate the knee- and ankle-joint centers, respectively. The anterior-superior iliac spine digitization points were used to determine the hip-joint center using the Bell et al method.29
After setup, participants stood in relaxed position with hands at their sides to allow for calibration of their neutral stance. Squat depth was controlled using a tripod placed behind the participant to provide feedback at 90° of knee flexion. Foot position during the squat was recorded by marking and measuring the medial aspect of each foot with tape. This ensured that foot position would be similar between testing sessions. Participants performed 1 set of 5 squats, which were averaged and used for data analysis. Consecutive squats were chosen instead of individual squats because this procedure is used during clinical screenings.
Strength was assessed via 3- to 5-second maximal voluntary isometric contractions (MVICs) for the gluteus maximus, gluteus medius, and hamstrings. Average force was recorded over the 5-second MVIC in newtons, and the average of 3 trials was used for analysis, with a 30-second period between trials to minimize fatigue. The primary investigator completed all strength measurements in a randomized order. Strength was assessed using active resistance tests.9,30 For the gluteus maximus and hamstrings, the participant was in a prone position with the knee bent to 90°. The dynamometer was placed on the posterior thigh proximal to the knee (gluteus maximus) or posterior aspect of the lower leg in line with the malleoli (hamstrings). Participants were instructed to extend the hip or flex the knee, respectively. Finally, hip abduction was assessed in the side-lying position with the dynamometer placed proximal to the lateral knee-joint line.31
We assessed active dorsiflexion ROM of the ankle using a standard 30.5-cm (1-in) goniometer. The primary investigator made all measurements; 3 trials were taken for each motion and the average was used for analysis. Ankle-dorsiflexion ROM was assessed with the knee straight and flexed to determine if the restriction in ankle motion was caused by the gastrocnemius or soleus, respectively. Participants were positioned supine with the leg extended and a foam roller placed under the distal shank in order to ensure full knee extension.9 For the knee-flexed condition, the foam roller was placed under the knee and the ankle was allowed to hang off the end of the table.9 The stationary arm was in line with the fibula while the mobile arm was aligned with the fifth metatarsal and the axis of the goniometer was placed distal to the lateral malleolus.9
Intervention Program
This intervention program was developed on the basic procedures outlined in the National Academy of Sports Medicine corrective exercise strategies textbook.26 Each participant in the INT group completed 10 sessions of directed exercise with the principal investigator (PI) (D.R.B.) over a 3-week period. Exercises became more challenging with each session by increasing sets, repetitions, or resistance or changing to a new exercise entirely. A comprehensive approach was used that focused on joints proximal and distal to the knee, with 5 exercises focused on the hip musculature and 5 on the ankle musculature. Exercises were implemented in order to correct alignment during functional tasks. Exercises used and a typical progression during the intervention period are shown in Tables 1 and 2. Exercises were performed in a specific sequence via a corrective exercise strategy that included (1) inhibiting overactive muscles, (2) lengthening tight muscles, (3) strengthening weak muscles, and (4) performing an integrative exercise with proper form and technique, including keeping the knees over the toes during these tasks. Participants received this instruction at the beginning of the integrative exercise only. Progression decisions were made by the PI and were based on feedback given by individual participants. Once a participant indicated that an exercise was becoming easier, a progression was made during the next visit. After each visit, the PI would ask about each exercise to ensure that each participant was challenged by proper level of resistance or repetitions.
Table 1.
Exercises and Theoretical Application During the 10-Session Exercise Intervention
| Exercise Sequence |
Muscles Theorized to Contribute to MKD |
Exercise Protocol |
| 1. Inhibit overactive muscles | Gastrocnemius, lateral hamstring, adductors | Foam roll each muscle for 2 min; let foam roller sit for 30 s over tight or painful areas |
| 2. Lengthen tight muscles | Gastrocnemius, soleus, lateral hamstring, adductors | Static stretch: 2 sets × 30-s hold |
| 3. Strengthen weak musclesa | Medial gastrocnemius, medial hamstring, tibialis posterior | Each repetition should last for 7 counts at a slow, controlled tempo: concentric contraction (1 count) → isometric contraction (2 counts) → eccentric contraction (4 counts) |
| 4. Integration exercise | SLS, SEB, SLS unstable surface, SEB unstable surface, hop to balance (10–15 reps) |
Abbreviations: MKD, medial knee displacement; SEB, Star Excursion Balance; SLS, single-legged squats.
Add elastic resistance to increase difficulty.
Table 2.
Typical Exercise Progression for the Intervention Groupa
| Exercise Session |
Strengthening |
Integration |
| 1 | Heel raises with toes internally rotated: 1 × 15 | SLB with squat (1 × 15) |
| Hamstring curls with tibial internal rotation: 1 × 15 (blue) | ||
| Tibialis posterior: 1 × 15 (green) | ||
| 2 | Heel raises with toes internally rotated: 2 × 10 | SLB with squat (2 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 10 (blue) | ||
| Tibialis posterior: 2 × 10 (green) | ||
| 3 | Heel raises with toes internally rotated: 3 × 10 | SLB with squat (3 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 10 (black) | ||
| Tibialis posterior: 3 × 10 (green) | ||
| 4 | Heel raises with toes internally rotated: 3 × 10 | SEB (2 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 10 (black) | ||
| Tibialis posterior: 3 × 10 (blue) | ||
| 5 | Heel raises with toes internally rotated: 3 × 10 | SEB (3 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 10 (black) | ||
| Tibialis posterior: 3 × 10 (blue) | ||
| 6 | Heel raises with toes internally rotated: 3 × 12 | SLB with squat on unstable surface (2 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 15 (black) | ||
| Tibialis posterior: 3 × 12 (blue) | ||
| 7 | Heel raises with toes internally rotated: 3 × 12 | SLB with squat on unstable surface (3 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 15 (black) | ||
| Tibialis posterior: 3 × 15 (blue) | ||
| 8 | Heel raises with toes internally rotated: 3 × 15 | SEB on unstable surface (3 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 15 (black) | ||
| Tibialis posterior: 3 × 10 (gray) | ||
| 9 | Heel raises with toes internally rotated: 3 × 15 | SEB on unstable surface (3 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 10 (gray) | ||
| Tibialis posterior: 3 × 10 (gray) | ||
| 10 | Heel raises with toes internally rotated: 3 × 15 | Hop to balance (3 × 10) |
| Hamstring curls with tibial internal rotation: 3 × 10 (gray) | ||
| Tibialis posterior: 3 × 12 (gray) |
Abbreviations: SEB, Star Excursion Balance, SLB, single-limb balance.
Colors represent the resistance level of exercise bands used during the program.
Participants were required to attend a minimum of 2 sessions per week; however, the majority of participants completed 3 sessions per week. All participants completed 10 exercise sessions and met the 2-sessions-per-week minimum. Posttesting was scheduled 1 to 2 days after the final exercise session. Only 2 participants were unable to complete the progression outlined in Table 2 for the strengthening exercises; these participants were able to complete all progressions of the integrative exercises. Participants in the CON group returned for posttesting 3 weeks later. Both groups were instructed not to begin a new exercise regimen. At posttest, the intervention group was not given instructions or feedback about performance.
Data Reduction
Three-dimensional coordinates of the digitized bony landmarks were calculated using the Motion Monitor software. A global reference system was defined with the positive x-axis in the anterior direction, the positive y-axis to the left, and the positive z-axis in the superior direction. Lower extremity rotations were calculated as Euler angles (degrees) in the following order: Y, X, Z. The positive directions in the knee were flexion, varus, and internal rotation.31 For this study, we calculated 2D knee valgus as MKD, which was defined by tracking the displacement of knee center (meters) relative to the y-axis of the global reference system. Thus, from this point on, MKD refers to the position of the knee and is analogous to what a clinician would see during visual observation. A customized MATLAB software program (The MathWorks, Natick, MA) was used to filter and reduce all data. Kinematic data were filtered via a fourth-order Butterworth filter with a cutoff frequency of 14.5 Hz.31 Knee-flexion angle was used to define the beginning and end of the descent phase of each squat (initiation of knee flexion to peak knee flexion). The 5 trials were averaged and interpolated to 101 data points. Change scores (post-test minus pretest) were calculated every 10% over the descent phase of the squat (0%, 10%, 20%, 30%, 40%, and 50% squat phase) for MKD and 3D knee valgus. Muscle strength was measured in newtons and was normalized to body weight. The average of 5 trials was used for analysis and change scores were calculated for muscle strength and ankle ROM variables.
Analysis
For MKD and 3D knee valgus, a group (2 levels)-by squat phase (6 levels) repeated-measures analysis of variance was used to analyze these variables and the Tukey honestly significant difference was used for post hoc testing when appropriate. Independent-samples t tests were used to compare change scores in hip strength and ankle-dorsiflexion ROM. For all statistical analyses, PASW (v18; IBM Corp, Somers, NY) was used with an a priori level of significance of P < .05. Effect size (d) was calculated using the following equation: mean 1 − mean 2/pooled SD.32
RESULTS
Height, mass, and age were not different between groups (height: t1,30 = −0.68, P = .50; mass: t1,30 = −0.95, P = .35, age: t1,30 = −0.25, P = .80). The INT group reduced 3D knee-valgus angle (P = .001, F1,150 = 4.43) from 30% to 50% of the squat phase (50% squat phase d = 0.58) and MKD (F1,150 = 3.4, P = .02) from 20% to 50% of the squat phase (50% d = 1.3) (Table 3). Ankle dorsiflexion–knee extended increased in the INT group (t1,30 = 2.8, P = .009, d = 0.77), whereas ankle dorsiflexion–knee flexed (t1,30 = 0.47, P = .64) did not. No changes were observed in isometric strength (hip extension: t1,30 = −1.3, P = .20, d = 0.50); hip abduction: t1,30 = −1.5, P = .14, d = 0.27; or knee flexion: t1,30 = −1.03, P = .31, d = 0.29; Table 4).
Table 3.
Raw Kinematic Values for the Control and Intervention Groups From Which Change Scores Were Calculated (Mean ± SD)a
| Squat Phase, % |
Knee Valgus, ° |
MKD, cm |
||||||
| Control |
Intervention |
Control |
Intervention |
|||||
| Pretest |
Post-test |
Pretest |
Post-test |
Pretest |
Post-test |
Pretest |
Post-test |
|
| 0 | −0.1 ± 1.1 | 0.1 ± 1.2 | −0.1 ± 1.0 | 0.2 ± 0.9 | −0.1 ± 0.3 | 0.1 ± 0.8 | 0.1 ± 0.5 | −0.1 ± 0.8 |
| 10 | −1.3 ± 2.5 | −0.7 ± 3.5 | −2.7 ± 3.4 | −2.3 ± 4.3 | −0.1 ± 0.3 | −0.2 ± 1.2 | 0.2 ± 1.3 | −0.6 ± 1.0 |
| 20b | −2.1 ± 3.5 | −1.9 ± 6.1 | −6.5 ± 6.5 | −4.3 ± 7.8 | −0.3 ± 1.4 | −0.8 ± 1.6 | 0.1 ± 2.0 | −2.1 ± 1.7 |
| 30bc | −1.9 ± 5.0 | −2.8 ± 7.8 | −8.0 ± 7.2 | −3.7 ± 8.4 | 0.6 ± 1.8 | 0.1 ± 2.6 | 0.9 ± 2.8 | −2.3 ± 2.2 |
| 40bc | −1.2 ± 6.1 | −2.5 ± 8.2 | −7.8 ± 7.2 | −2.8 ± 8.7 | 1.7 ± 2.4 | 1.1 ± 3.1 | 1.7 ± 3.0 | −2.0 ± 2.3 |
| 50bc | −0.7 ± 6.8 | −2.6 ± 7.9 | −7.7 ± 7.2 | −2.7 ± 8.9 | 2.4 ± 2.5 | 1.8 ± 3.3 | 2.2 ± 3.0 | −1.8 ± 2.4 |
Abbreviation: MKD, medial knee displacement.
A positive value for MKD indicates that the knee was displacing or collapsing medially.
MKD was different between groups from 20% to 50% of the squat phase.
3D knee valgus was different between groups from 30% to 50% of the squat phase.
Table 4.
Raw Strength and Range of Motion Variables for Each Group From Which Change Scores Were Calculated (Mean ± SD)
| Variable |
Group |
Pretest |
Posttest |
Change Score |
Mean Difference |
95% CI of Difference |
| Range of motion, ° | ||||||
| Dorsiflexion, knee straight | Control | 5.0 ± 4.6 | 3.5 ± 5.3 | −1.5 ± 4.7 | −5.0 | −8.7, −1.4 |
| Intervention | 6.9 ± 4.7 | 10.5 ± 4.6 | 3.5 ± 5.4 | |||
| Dorsiflexion, knee bent | Control | 14.3 ± 5.4 | 14.1 ± 4.9 | −0.1 ± 3.4 | 0.6 | −1.9, 3.1 |
| Intervention | 15.0 ± 5.1 | 14.3 ± 3.8 | −0.7 ± 3.6 | |||
| Strength, % BW | ||||||
| Hip extension | Control | 46.7 ± 11.9 | 50.4 ± 12.8 | 3.7 ± 13.1 | −5.5 | −14.0, 3.0 |
| Intervention | 42.4 ± 17.4 | 51.6 ± 13.7 | 9.2 ± 10.5 | |||
| Hip abduction | Control | 50.9 ± 12.2 | 50.6 ± 9.0 | −0.4 ± 7.3 | −4.7 | −10.9, 1.6 |
| Intervention | 48.2 ± 15.1 | 52.6 ± 14.3 | 4.3 ± 9.9 | |||
| Knee flexion | Control | 21.2 ± 4.8 | 21.8 ± 4.4 | 0.7 ± 2.5 | −1.2 | −3.4, 1.1 |
| Intervention | 20.1 ± 7.0 | 22.1 ± 7.8 | 1.8 ± 3.7 | |||
Abbreviations: BW, body weight; CI, confidence interval.
DISCUSSION
The most important finding of this study was that a systematic corrective exercise program successfully reduced MKD and 3D knee valgus during a DLS. This reduction in frontal-plane motion was accompanied by increased ankle-dorsiflexion ROM with the knee extended. No other significant changes in ROM or muscle strength were observed. Our hypothesis was partially supported, as the intervention improved frontal-plane motion and improvements were seen in ankle ROM. However, we were unable to detect differences in hip strength. This is not surprising, given our inclusion criteria that focused on individuals with theoretically restricted ankle motion and that our study was not powered for changes in hip strength.
Previous research28,33–36 using exercise interventions has been unsuccessful at altering 3D knee-valgus angle during landing tasks. These programs tend to focus on balance or plyometric training and are more hip dominant in terms of muscle groups being targeted. Our study is one of the first to show improvements in 3D knee valgus, which may be because of the focus on ankle strength and flexibility exercises. We recommend that interventions to improve 3D knee valgus include ankle exercises as part of a comprehensive program. Another difference is that we sought individuals with poor movement patterns. Previous researchers studied a variety of individuals who may or may not have demonstrated poor movement at baseline.
Medial knee displacement has been shown to improve postexercise.37–40 Three studies37–39 have documented improved MKD, whereas 1 group40 reported null findings. These studies used drop landings rather than a DLS, and most programs combined strength training, plyometrics, and stretching. Additionally, a key component of knee injury-prevention programs is to limit MKD during high-risk activity.41 Future investigators should determine if movement observed during the DLS is related to higher-demand activity such as a drop landing. Additionally, future researchers should determine if the positive changes observed as a result of this intervention carry over to higher-demand tasks.
Restrictions in ankle dorsiflexion appear to play a role in knee mechanics in individuals with visually identified knee valgus during a DLS. During the DLS, the participants in this study had excessive visual MKD that was corrected with a heel lift. Previous authors9 had identified weak ankle plantar-flexion strength and reduced ankle ROM in this population when compared with those without MKD during a DLS. Gastrocnemius tightness is common in populations without neurologic conditions42 and can result in excessive rearfoot pronation and flat foot.43 Tibial internal rotation is often coupled with subtalar eversion12,44; thus, tight plantar flexors could increase joint stiffness and require compensations in joints distal (increased pronation) and proximal (MKD) to the ankle to reach the required squat depth. The heel lift placed the ankle in a plantar-flexed position and likely increased the range of ankle-dorsiflexion motion during the descent phase of the squat. Placing the ankle in more plantar flexion, which resolved these restrictions, allowed the knees to stay over the toes. In this study ankle dorsiflexion was assessed in the open chain even though the DLS is a closed chain activity. Restrictions in ankle dorsiflexion have been observed using both open and closed chain assessment techniques.8 Quality of lower extremity motion was evaluated and ankle dorsiflexion was measured.8 Individuals with worse quality of movement had dorsiflexion restrictions using both open and closed chain methods.8 Thus restrictions in open chain ankle-dorsiflexion motion appear to translate to closed chain restrictions as well. Therefore, we feel that an open chain assessment of dorsiflexion is a valid representation of restrictions in the closed chain. The intervention increased ankle ROM and concomitantly improved MKD and 3D knee valgus.
Traditional 3D assessment of knee-valgus angle and moment has been shown to predict noncontact ACL injury in females with 78% sensitivity and 73% specificity.1 We used a visual screening examination to identify participants because previous research45 demonstrated a moderate relationship between MKD and 3D assessments of valgus for jumping or stepping motions. However, the relationship between MKD and 3D knee valgus may not be as strong as once thought. Ageberg et al24 used a single-legged squat, visually categorized participants into knee-over-foot or knee-medial-to-foot groups, and evaluated knee valgus using 2D and 3D methods. The 2D assessment clearly demonstrated that the knee-medial-to-foot group was in valgus, but 3D knee valgus did not differ between groups.24 This relationship was also reflected in our 3D knee-valgus results, as groups appeared unequal at baseline (Table 3). At 50% squat phase, the INT group had more than 7° of 3D knee valgus at pretest compared with the CON group. This is a slight threat to internal validity, as our randomization was not successful with this variable. However, the intervention improved 3D knee valgus by 5° (64% reduction) and was associated with a moderate effect size.32 Overall, the intervention significantly reduced 3D knee valgus.
In the current study MKD was reduced by 4 cm. Myer et al3 used an MKD assessment combined with other clinical measures (tibia length, knee-flexion motion, mass, and quadriceps-to-hamstrings strength ratio) to predict high knee-abduction moment during a drop landing with 77% sensitivity and 71% specificity. A nomogram was developed that assigned point values to these different factors associated with a high abduction moment.3 Using this nomogram and the example in the article, a female with 8.2 cm of MKD would have a 74% chance of demonstrating a high knee-abduction moment.3 A 4-cm reduction in MKD, as seen in our study, would reduce this chance to less than 40% with other variables held constant. However, our values for MKD were much lower at 2.4 cm compared with 8.2 cm. We caution the reader that we used a DLS rather than a drop landing. Although using the nomogram is both compelling and interesting, it is not clear if the magnitude of MKD change caused by our intervention would be similar during a jump landing. More research is needed to determine the relevant clinical information that can be garnered from screening examinations.
In the current study, hip-extension and -abduction strength tended to increase after the intervention; however, the findings were not statistically significant. Hip-muscle strength is believed to be important to dynamic lower extremity motion. Specifically, weakness of the hip extensors and hip abductors may result in excessive femoral adduction and internal rotation, which are components of MKD.15,46 Interestingly, the relationship between hip strength and lower extremity motion is not as clear as one might expect.13,14,47 For example, research has classified healthy adults into good or poor performers of a single-leg squat.48 Individuals with poor single-legged squat technique had 29% less hip-abduction torque compared with those with good technique. In contrast, Rabin and Kozol8 used a lateral step-down test and found no difference in hip-abduction strength between those classified as good and those classified as those classified as moderate performers. However, those classified as moderate performers had decreased ankle-dorsiflexion ROM compared with those classified as good. The difference in our results may be explained by knee-flexion angle, which is substantially less in the lateral step-down test compared with the DLS. The reduced sagittal-plane motion of the lateral step-down test may influence the relationship between hip strength and MKD. Poor movement quality in our study was partially caused by restricted ankle motion,9 which is most comparable with the findings of Rabin and Kozol.8 The current study was not powered for secondary variables of interest, but it is possible that a portion of the improvement in MKD and 3D knee valgus could be attributed to increased hip strength. Additional research is needed to clarify the relative contribution of the hip and ankle to frontal-plane knee motion.
The intervention was performed bilaterally and was completed in approximately 30 minutes per session, which may exclude its use in some settings. However, participants were able to complete the program independently. Another potential limitation is that investigators who assessed key outcomes were not blinded to group assignment, which may have led to unintentional bias, particularly during the strength and ROM measurements. Including participants with ankle-driven MKD may have reduced our ability to find significant improvements in hip-muscle strength. Additionally, the time frame of the intervention may have been adequate to increase ROM but inadequate to achieve physiologic increases in strength. Additionally, isometric strength assessments are limited to discrete joint positions. Future researchers should consider isokinetic testing to further investigate these variables. Three-dimensional knee valgus values were not equal at pretest, and the intervention was unable to improve the 3D knee-valgus angles beyond the CON group values. Finally, activity level was not controlled and may have influenced results.
CONCLUSIONS
This study provides an effective exercise strategy to improve MKD and 3D knee valgus during a DLS and highlights the role of restricted ankle motion in lower extremity motion. Visual identification of excessive frontal-plane knee motion can be completed with little equipment and is an easy way to screen a large number of athletes. We recommend that interventions to improve knee valgus should include ankle exercises as part of a comprehensive program.
ACKNOWLEDGMENTS
This study was funded by the National Academy of Sports Medicine, which provided participant remuneration and rehabilitation supplies.
REFERENCES
- 1.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 2.Munro A, Herrington L, Carolan M. Reliability of 2-dimensional video assessment of frontal-plane dynamic knee valgus during common athletic screening tasks. J Sport Rehabil. 2012;21(1):7–11. doi: 10.1123/jsr.21.1.7. [DOI] [PubMed] [Google Scholar]
- 3.Myer GD, Ford KR, Hewett TE. New method to identify athletes at high risk of ACL injury using clinic-based measurements and freeware computer analysis. Br J Sports Med. 2011;45(4):238–244. doi: 10.1136/bjsm.2010.072843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Willson JD, Ireland ML, Davis I. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc. 2006;38(5):945–952. doi: 10.1249/01.mss.0000218140.05074.fa. [DOI] [PubMed] [Google Scholar]
- 5.National Coalition for Women and Girls in Education. Title IX at 35: Beyond the Headlines. Washington, DC: National Coalition for Women and Girls in Education; 2008. [Google Scholar]
- 6.Sigward SM, Ota S, Powers CM. Predictors of frontal plane knee excursion during a drop land in young female soccer players. J Orthop Sports Phys Ther. 2008;38(11):661–667. doi: 10.2519/jospt.2008.2695. [DOI] [PubMed] [Google Scholar]
- 7.McLean SG, Lipfert SW, van den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004;36(6):1008–1016. doi: 10.1249/01.mss.0000128180.51443.83. [DOI] [PubMed] [Google Scholar]
- 8.Rabin A, Kozol Z. Measures of range of motion and strength among healthy women with differing quality of lower extremity movement during the lateral step-down test. J Orthop Sports Phys Ther. 2010;40(12):792–800. doi: 10.2519/jospt.2010.3424. [DOI] [PubMed] [Google Scholar]
- 9.Bell DR, Padua DA, Clark MA. Muscle strength and flexibility characteristics of people displaying excessive medial knee displacement. Arch Phys Med Rehabil. 2008;89(7):1323–1328. doi: 10.1016/j.apmr.2007.11.048. [DOI] [PubMed] [Google Scholar]
- 10.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes, part 1: mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311. doi: 10.1177/0363546505284183. [DOI] [PubMed] [Google Scholar]
- 11.Dempsey AR, Lloyd DG, Elliott BC, Steele JR, Munro BJ, Russo KA. The effect of technique change on knee loads during sidestep cutting. Med Sci Sports Exerc. 2007;39(10):1765–1773. doi: 10.1249/mss.0b013e31812f56d1. [DOI] [PubMed] [Google Scholar]
- 12.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 13.Norcross MF, Halverson SD, Hawkey TJ, Blackburn JT, Padua DA. Evaluation of the lateral step-down test as a clinical assessment of hip musculature strength. Athl Train Sports Health Care. 2009;1(6):272–278. [Google Scholar]
- 14.Thijs Y, Van Tiggelen D, Willems T, De Clercq D, Witvrouw E. Relationship between hip strength and frontal plane posture of the knee during a forward lunge. Br J Sports Med. 2007;41(11):723–727. doi: 10.1136/bjsm.2007.037374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Claiborne TL, Armstrong CW, Gandhi V, Pincivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006;22(1):41–50. doi: 10.1123/jab.22.1.41. [DOI] [PubMed] [Google Scholar]
- 16.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 18.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 19.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 20.Brophy RH, Silvers HJ, Mandelbaum BR. Anterior cruciate ligament injuries: etiology and prevention. Sports Med Arthrosc. 2010;18(1):2–11. doi: 10.1097/JSA.0b013e3181cdd195. [DOI] [PubMed] [Google Scholar]
- 21.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DiStefano LJ, Padua DA, DiStefano MJ, Marshall SW. Influence of age, sex, technique, and exercise program on movement patterns after an anterior cruciate ligament injury prevention program in youth soccer players. Am J Sports Med. 2009;37(3):495–505. doi: 10.1177/0363546508327542. [DOI] [PubMed] [Google Scholar]
- 23.Hirth CJ, Padua DA. Clinical movement analysis to identify muscle imbalances and guide exercise. Athl Ther Today. 2007;12(4):10–14. [Google Scholar]
- 24.Ageberg E, Bennell KL, Hunt MA, Simic M, Roos EM, Creaby MW. Validity and inter-rater reliability of medio-lateral knee motion observed during a single-limb mini squat. BMC Musculoskelet Disord. 2010;11:265. doi: 10.1186/1471-2474-11-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ekegren CL, Miller WC, Celebrini RG, Eng JJ, MacIntyre DL. Reliability and validity of observational risk screening in evaluating dynamic knee valgus. J Orthop Sports Phys Ther. 2009;39(9):665–674. doi: 10.2519/jospt.2009.3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clark M, Lucett S, Corn R. Optimum Performance Training for the Health and Fitness Professional. 2nd ed. Chandler, AZ: National Academy of Sports Medicine;; 2004. [Google Scholar]
- 27.Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function, part 1. N Am J Sports Phys Ther. 2006;1(2):62–72. [PMC free article] [PubMed] [Google Scholar]
- 28.DiStefano LJ, Blackburn JT, Marshall SW, Guskiewicz KM, Garrett WE, Padua DA. Effects of an age-specific anterior cruciate ligament injury prevention program on lower extremity biomechanics in children. Am J Sports Med. 2011;39(5):949–957. doi: 10.1177/0363546510392015. [DOI] [PubMed] [Google Scholar]
- 29.Bell AL, Pedersen DR, Brand RA. A comparison of the accuracy of several hip center location prediction methods. J Biomech. 1990;23(6):617–621. doi: 10.1016/0021-9290(90)90054-7. [DOI] [PubMed] [Google Scholar]
- 30.Kendall F, McCreary E, Provance P. Muscles: Testing and Function With Posture and Pain. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins;; 1993. [Google Scholar]
- 31.Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108–2116. doi: 10.1177/0363546509337934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River, NJ: Pearson/Prentice Hall;; 2009. xix, 892. [Google Scholar]
- 33.Lephart SM, Abt JP, Ferris CM, et al. Neuromuscular and biomechanical characteristic changes in high school athletes: a plyometric versus basic resistance program. Br J Sports Med. 2005;39(12):932–938. doi: 10.1136/bjsm.2005.019083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nagano Y, Ida H, Akai M, Fukubayashi T. Effects of jump and balance training on knee kinematics and electromyography of female basketball athletes during a single limb drop landing: pre-post intervention study. Sports Med Arthrosc Rehabil Ther Technol. 2011;3(1):14. doi: 10.1186/1758-2555-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pollard CD, Sigward SM, Ota S, Langford K, Powers CM. The influence of in-season injury prevention training on lower-extremity kinematics during landing in female soccer players. Clin J Sport Med. 2006;16(3):223–227. doi: 10.1097/00042752-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):445–455. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 37.Herrington L. The effects of 4 weeks of jump training on landing knee valgus and crossover hop performance in female basketball players. J Strength Cond Res. 2010;24(12):3427–3432. doi: 10.1519/JSC.0b013e3181c1fcd8. [DOI] [PubMed] [Google Scholar]
- 38.Lim BO, Lee YS, Kim JG, An KO, Yoo J, Kwon YH. Effects of sports injury prevention training on the biomechanical risk factors of anterior cruciate ligament injury in high school female basketball players. Am J Sports Med. 2009;37(9):1728–1734. doi: 10.1177/0363546509334220. [DOI] [PubMed] [Google Scholar]
- 39.Noyes FR, Barber-Westin SD, Fleckenstein C, Walsh C, West J. The drop-jump screening test: difference in lower limb control by gender and effect of neuromuscular training in female athletes. Am J Sports Med. 2005;33(2):197–207. doi: 10.1177/0363546504266484. [DOI] [PubMed] [Google Scholar]
- 40.Grandstrand SL, Pfeiffer RP, Sabick MB, DeBeliso M, Shea KG. The effects of a commercially available warm-up program on landing mechanics in female youth soccer players. J Strength Cond Res. 2006;20(2):331–335. doi: 10.1519/R-17585.1. [DOI] [PubMed] [Google Scholar]
- 41.Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players, part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17(8):859–879. doi: 10.1007/s00167-009-0823-z. [DOI] [PubMed] [Google Scholar]
- 42.DiGiovanni CW, Kuo R, Tejwani N, et al. Isolated gastrocnemius tightness. J Bone Joint Surg Am. 2002;84(6):962–970. doi: 10.2106/00004623-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 43.DiGiovanni CW, Langer P. The role of isolated gastrocnemius and combined Achilles contractures in the flatfoot. Foot Ankle Clin. 2007;12(2):363–379. doi: 10.1016/j.fcl.2007.03.005. viii. [DOI] [PubMed] [Google Scholar]
- 44.Nawoczenski DA, Saltzman CL, Cook TM. The effect of foot structure on the three-dimensional kinematic coupling behavior of the leg and rear foot. Phys Ther. 1998;78(4):404–416. doi: 10.1093/ptj/78.4.404. [DOI] [PubMed] [Google Scholar]
- 45.McLean SG, Walker K, Ford KR, Myer GD, Hewett TE, Vanden Bogert AJ. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Br J Sports Med. 2005;39(6):355–362. doi: 10.1136/bjsm.2005.018598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nguyen AD, Shultz SJ, Schmitz RJ, Luecht RM, Perrin DH. A preliminary multifactorial approach describing the relationships among lower extremity alignment, hip muscle activation, and lower extremity joint excursion. J Athl Train. 2011;46(3):246–256. doi: 10.4085/1062-6050-46.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Heiderscheit BC. Lower extremity injuries: is it just about hip strength? J Orthop Sports Phys Ther. 2010;40(2):39–41. doi: 10.2519/jospt.2010.0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crossley KM, Zhang WJ, Schache AG, Bryant A, Cowan SM. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39(4):866–873. doi: 10.1177/0363546510395456. [DOI] [PubMed] [Google Scholar]