Abstract
Objective:
To present recommendations for athletic trainers and other allied health care professionals in the conservative management and prevention of ankle sprains in athletes.
Background:
Because ankle sprains are a common and often disabling injury in athletes, athletic trainers and other sports health care professionals must be able to implement the most current and evidence-supported treatment strategies to ensure safe and rapid return to play. Equally important is initiating preventive measures to mitigate both first-time sprains and the chance of reinjury. Therefore, considerations for appropriate preventive measures (including taping and bracing), initial assessment, both short- and long-term management strategies, return-to-play guidelines, and recommendations for syndesmotic ankle sprains and chronic ankle instability are presented.
Recommendations:
The recommendations included in this position statement are intended to provide athletic trainers and other sports health care professionals with guidelines and criteria to deliver the best health care possible for the prevention and management of ankle sprains. An endorsement as to best practice is made whenever evidence supporting the recommendation is available.
Key Words: : ankle instability, syndesmotic ankle sprains, cryotherapy, immobilization, compression, sensorimotor system, taping, bracing
Ankle sprains are common injuries that affect athletes of all ages and in all sporting activities. An estimated 28 000 ankle injuries occur in the United States each day.1 These injuries translate into an enormous burden on the health care industry and result in millions of dollars spent on treatment each year. In sport, ankle injuries are the most common injury,2 with some estimates attributing upward of 45% of all athletic injuries to ankle sprains.3 In their systematic review, Fong et al2 noted that the incidence rates of ankle injury and sprain are highest in field hockey, followed by volleyball, football, basketball, cheerleading, ice hockey, lacrosse, soccer, rugby, track and field, gymnastics, and softball.
Most ankle sprains result from damage to the lateral ligament structures (anterior talofibular, calcaneofibular, and posterior talofibular ligaments) after a stress on an inverted and plantar-flexed (supinated) foot.3 Sprains are usually graded on the basis of severity and range from mild (grade I) to severe (grade III): The grading scale is a spectrum from no significant structural injury to complete rupture of the ligamentous structures. Landing from jumps, landing or stepping on another athlete's foot, trauma at heel strike during running, and stressing the foot while in a fixed position are common mechanisms for ankle sprains.3 In a comprehensive review, Beynnon et al4 evaluated intrinsic and extrinsic risk factors for ankle sprains in athletes and concluded that the only consistent risk factor identified across original research studies was a previous history of ankle sprain.
Despite the frequency of ankle sprains in athletes, the outcomes associated with these injuries are less than optimal. Individuals who sustain initial ankle sprains demonstrate high recurrence rates, prolonged symptoms, diminished quality of life, reduced physical activity levels across the lifespan, a propensity to develop chronic ankle instability, and an increased risk for ankle osteoarthritis.4 Managing these injuries appropriately is clearly problematic for sports health care professionals. The purpose of this position statement is to present recommendations for certified athletic trainers and other allied health care professionals in the conservative management and prevention of ankle sprains in athletes. Our recommendations are reinforced by relevant scholarly evidence currently available in peer-reviewed publications and graded according to the Strength of Recommendation Taxonomy (Table).5
Table.
Strength of Recommendation Taxonomy (SORT)a
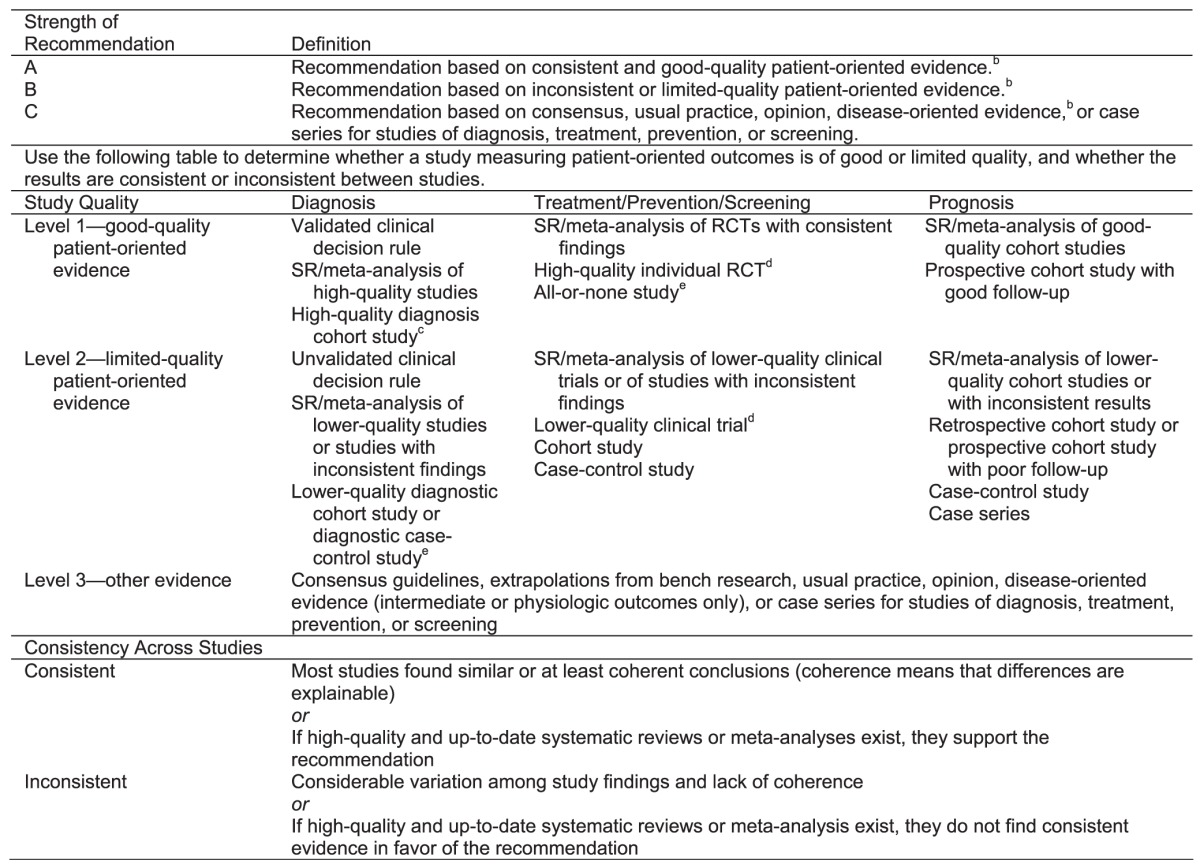
Abbreviations: RCT indicates randomized controlled trial; SR, systematic review.
In general, only key recommendations for readers require a grade of the “Strength of Recommendation.” Recommendations should be based on the highest quality evidence available. For example, vitamin E was found in some cohort studies (level 2 study quality) to have a benefit for cardiovascular protection, but good-quality randomized trials (level 1) have not confirmed this effect. Therefore, it is preferable to base clinical recommendations in a manuscript on the level 1 studies. Reprinted with permission from “Strength of Recommendation Taxonomy (SORT): A Patient-Centered Approach to Grading Evidence in the Medical Literature,” February 1, 2004, American Family Physician. Copyright © 2004 American Academy of Family Physicians. All Rights Reserved.
Patient-oriented evidence measures outcomes that matter to patients: morbidity, mortality, symptom improvement, cost reduction, and quality of life. Disease-oriented evidence measures intermediate, physiologic, or surrogate end points that may or may not reflect improvements in patient outcomes (e.g., blood pressure, blood chemistry, physiologic function, pathologic findings).
High-quality diagnostic cohort study: cohort design, adequate size, adequate spectrum of patients, blinding, and a consistent, well-defined reference standard.
High-quality RTC: allocation concealed, blinding if possible, intention-to-treat analysis, adequate statistical power, adequate follow-up (greater than 80%).
In an all-or-none study, the treatment causes a dramatic change in outcomes, such as antibiotics for meningitis or surgery for appendicitis, which precludes study in a controlled trial.
Recommendations
The National Athletic Trainers' Association (NATA) suggests the following guidelines in the management and prevention of ankle sprains in the athletic population.
Diagnosis
-
1.
The patient's history, including the mechanism of injury and past injuries and clinician observation and palpation, can provide important insights into the anatomical structures that may be injured in a patient suspected of having an ankle sprain. However, the severity of injury may be difficult to determine. Evidence Category: C
-
2.
Assessment of active, passive, and resistive range of motion (ROM) about the ankle can provide insight into injury to ligaments, muscles, tendons, and nerves. Evidence Category: C
-
3.
Special tests to assess injury to the lateral ankle ligaments, such as the anterior drawer and inversion talar tilt tests, performed soon after injury and before joint effusion has accumulated, may have better diagnostic accuracy than tests performed after effusion has occurred. Evidence Category: C
-
4.
Special tests such as the anterior drawer and inversion talar tilt tests have more diagnostic accuracy 5 days after injury than they do 2 days after injury.6,7 Evidence Category: B
-
5.
Clinicians must be vigilant in assessing associated lesions, both local and distant to the talocrural joint, that may accompany ankle sprains. Evidence Category: C
-
6.
Special tests for high ankle sprains, such as the squeeze test, Cotton test, external-rotation test, and fibular translation test, should be performed to assess injury to the anterior-inferior tibiofibular ligament. Evidence Category: C
-
7.
The Ottawa Ankle Rules (OARs) are a valid clinical tool to determine the need for radiographs of the acutely injured ankle or midfoot.8,9 Evidence Category: A
-
8.
Stress radiography is an unreliable tool to detect acute ligamentous disruption after ankle sprain.10 Evidence Category: B
-
9.
Magnetic resonance imaging (MRI) is a reliable technique to detect acute tears of the anterior talofibular ligament and calcaneofibular ligament after acute injury.11–13 Evidence Category: B
-
10.
Osteochondral lesions of the talus can be accurately detected by both MRI and computed tomography (CT).14,15 Evidence Category: B
-
11.
Compared with MRI, diagnostic ultrasound is useful but less accurate and sensitive in detecting acute lateral ankle ligamentous injury.13,16,17 Evidence Category: B
-
12.
Arthrography and tenography are less accurate than MRI and CT, especially when performed 48 hours after lateral ligamentous injury.18,19 Evidence Category: B
-
13.
After acute trauma, MRI has high sensitivity, specificity, and accuracy to determine the level of injury to the ankle syndesmotic ligaments.20,21 Evidence Category: B
Treatment and Rehabilitation
-
14.
Cryotherapy should be applied to acute ankle sprains to reduce pain, minimize swelling formation, and decrease secondary injury.22–24 Evidence Category: C
-
15.
Compression should be applied to acute ankle sprains to minimize swelling.25 Evidence Category: C
-
16.
The limb with the acute ankle sprain should be elevated to minimize swelling.26 Evidence Category: C
-
17.
Nonsteroidal anti-inflammatory drugs, administered orally or topically, reduce pain and swelling and improve short-term function after ankle sprains.27–29 Evidence Category: A
-
18.
Functional rehabilitation is more effective than immobilization in managing grade I and II ankle sprains.30,31 Evidence Category: A
-
19.
Grade III sprains should be immobilized for at least 10 days with a rigid stirrup brace or below-knee cast and then controlled therapeutic exercise instituted.30,32 Evidence Category: B
-
20.
Electrical stimulation can be used as an adjunct to minimize swelling during the acute phase of injury.33,34 Evidence Category: C
-
21.
Clinicians should refrain from thermotherapy during the acute and subacute phase of injury due to lack of evidence and the potential to exacerbate the injury.35,36 Evidence Category: C
-
22.
Cryokinetics can be used to reduce pain and thereby allow early rehabilitative exercises.26,37 Evidence Category: C
-
23.
Rehabilitation should include comprehensive ROM, flexibility, and strengthening of the surrounding musculature.30,31,38,39 Evidence Category: B
-
24.
Balance training should be performed throughout rehabilitation and follow-up management of ankle sprains to reduce reinjury rates.40–42 Evidence Category: A
-
25.
Passive joint mobilizations and mobilizations with movement should be used to increase ankle dorsiflexion and improve function.43–45 Evidence Category: B
Return-to-Play Considerations
-
26.
The patient's perception of function should be included in any return-to-play (RTP) decision making. Several instruments (eg, Lower Limb Task Questionnaire and Cumberland Ankle Instability Tool [CAIT]) may be used to help identify the patient's perception of function and aid in the RTP decision process.46–48 Evidence Category: C
-
27.
Functional performance testing should be a component of the RTP decision making. Several tests (eg, single-legged hop for distance, Star Excursion Balance Test [SEBT]) may be used to help determine the patient's ability to RTP.49–52 Before the patient returns to sport-specific tasks, the injured limb's functional performance should measure at least 80% of the uninjured limb.53,54 Evidence Category: B
-
28.
Athletes with a history of previous ankle sprains should wear prophylactic ankle supports in the form of ankle taping or bracing for all practices and games.55–57 Both lace-up and semirigid ankle braces and traditional ankle taping are effective in reducing the rate of recurrent ankle sprains in athletes.56,58,59 Evidence Category: B
Prevention
-
29.
Clinicians working with athletes should implement a multi-intervention injury-prevention program lasting at least 3 months that focuses on balance and neuromuscular control to reduce the risk of ankle injury. Athletes with a history of ankle injury may benefit more from this type of training.60–63 Evidence Category: A
-
30.
Addressing the strength of the leg muscles (evertors, invertors, dorsiflexors, and plantar flexors) and hip extensors and abductors may be an ankle injury-prevention strategy.64–69 Evidence Category: C
-
31.
Clinicians should consider assessing dorsiflexion ROM in at-risk athletes. If dorsiflexion ROM is limited, clinicians should incorporate techniques to enhance arthrokinematic and osteokinematic motion for possible prevention of ankle injury.70,71 Evidence Category: C
Special Considerations
-
32.
Syndesmotic ankle sprains (“high” ankle sprains) are characterized by symptoms proximal to the talocrural joint, including prolonged pain, functional disability, and heterotopic ossification. Evaluation should consist of palpation, clinical testing, functional evaluation, and radiography, with MRI if indicated.72 Evidence Category: C
-
33.
Syndesmotic ankle sprains should be treated more conservatively than lateral ankle sprains. Acute management requires immobilization (nonweight bearing, walking boot, casting, or bracing) for a time period sufficient to allow healing and functional return.73 Evidence Category: C
-
34.
Surgical fixation should be considered for syndesmotic ankle sprains that demonstrate widening of the ankle mortise greater than 2 mm or joint incongruity on standard or stress radiographs.74 Evidence Category: C
-
35.
Clinicians should be aware of characteristics that define chronic ankle instability (CAI). Several instruments (Foot and Ankle Ability Measure [FAAM], Ankle Instability Instrument, and CAIT) may be used to help identify patients with CAI and quantify the severity of the condition.75–78 Evidence Category: C
-
36.
Mechanical and functional deficits in patients with CAI should be identified. These deficits include but are not limited to increased laxity,70 impaired dorsiflexion ROM,77 deficient leg and hip strength,70,79 diminished postural control,45,80 and impaired movement strategies.79,80 Evidence Category: C
-
37.
Intervention strategies should address specific deficits in patients with CAI. Manual therapy techniques used to restore normal arthrokinematic motion may be beneficial to help restore dorsiflexion ROM.44,81 Strategies that focus on balance, strength, and dynamic movements with changes in direction may be effective in reducing the risk of recurrent ankle sprains in patients with functional deficits.41,63,80 Evidence Category: B
BACKGROUND AND LITERATURE REVIEW
Physical Examination
History, Observation, and Palpation
The clinician begins the physical examination of a patient with an acute ankle injury by asking about any history of injury. A previous ankle sprain is the most common predisposing factor for a recurrent ankle sprain.4 The mechanism of injury should provide insight into which anatomical structures may be damaged. The most common mechanism of injury for a lateral ankle sprain is a distinct inciting event that involves supination of the rearfoot coupled with external rotation of the lower leg. This mechanism is often described as a plantar flexion-inversion mechanism, but it is important to realize that this mechanism frequently involves internal rotation (adduction) of the foot as well. The anterior talofibular ligament (ATFL) is the most commonly sprained lateral ligament, followed by the calcaneofibular ligament (CFL).82 Less often, eversion and external rotation (abduction) of the foot coupled with internal rotation of the lower leg may result in a medial ankle sprain involving the deltoid ligament. This mechanism can also produce concomitant or isolated injury to the distal tibiofibular syndesmosis. Syndesmotic injury can also occur with forced and excessive plantar flexion of the ankle, such as when a player is tackled from behind in football, or with excessive dorsiflexion, such as when an individual accidently steps in a hole.83
Thorough observation of the foot, ankle, and lower leg on the injured side should provide further insight as to which anatomic structures may be injured. The clinician should look for deformity, swelling, and discoloration. Gross deformities are typically seen with fractures and dislocations, but it is important to note that not all fractures present with deformity. Ankle sprains are often accompanied by swelling in and around the ankle joint; the location of the swelling may indicate which structures are involved, especially if the observation occurs in the minutes or hours immediately after injury. Swelling magnitude does not correlate with self-reported function after acute ankle sprain.84 Quantification of swelling with a figure-8 measure of ankle girth or water volumetrics may be useful in tracking changes over the course of injury recovery. Additionally, ascertaining if the athlete was able to bear weight or continue playing before reporting the injury is important in helping to rule out a fracture.8
Palpation of specific anatomical structures at and around the injured ankle will yield further information for formulating a differential diagnosis. Point tenderness over the injured ligaments is a good indicator of the injured structures85; however, the structural integrity of potentially injured ligaments should also be assessed with special tests. Bony tenderness over the fibular attachment sites of the ATFL should not raise suspicion of a fracture.8 Surrounding muscles and tendons should also be palpated. Ankle ROM should be assessed comprehensively and include testing of passive, active, and resistive ROM in both the sagittal (plantar-dorsiflexion) and frontal (inversion-eversion) planes. Limited total ROM may be due to an intra-articular lesion or swelling within the joint. Passive ROM is helpful in identifying injured structures under tension, whereas active and resistive ROM testing may be used to identify musculotendinous damage, muscle inhibition associated with joint injury, or both.
Ligamentous Special Tests
Surprisingly few authors have evaluated the diagnostic accuracy of special tests to assess the most commonly injured ankle ligaments. The gold standard for ligamentous injury has been observation of such injury during surgery.6,7,86,87 These results can thus be applied to the diagnostic accuracy of special tests in the assessment of severe, rather than mild, ankle sprains. The anterior drawer test is the most common test performed to assess the integrity of the ATFL. Sensitivity values have been reported to range from 32% to 80%.6,86,87 Specificity of the anterior drawer test has only been reported in 1 study6,7 and was 80%. A positive anterior drawer test 5 days after injury is more sensitive and specific than an examination performed within 48 hours of injury.7 Diagnostic accuracy of the inversion talar tilt test has been reported in a single study,86 with sensitivity of 52%. Specificity of the inversion talar tilt test has not been reported. Several special tests have been advocated for identifying high ankle sprains, including the squeeze test, Cotton test, external-rotation test, and fibular translation test; however, the diagnostic accuracy of these tests has received little attention.18 Similarly, the diagnostic accuracy of physical examination immediately after injury in athletes has not been determined. Special tests performed before swelling accumulates in and around the ankle may be of more clinical utility than tests performed later after injury.
Imaging: Osseous Injuries
Radiographs are ordered for 80% to 95% of patients who present to the hospital emergency room after foot and ankle trauma, yet only 15% of these patients actually have bone fractures.88 The OARs were developed to reduce unnecessary radiography in patients with ankle sprains.89 These clinical decision guidelines state that radiographs of the ankle are necessary only when pain is present in the malleolar zone and the patient exhibits any of the following findings: (1) bone tenderness along the distal 6 cm of the posterior edge of the medial or lateral malleolus, (2) bone tenderness directly at the tip of the medial or lateral malleolus, or (3) inability to bear weight and walk 4 steps immediately after the injury or at the emergency room. Radiographs of the feet are indicated with pain in the midfoot zone and any of the following findings: (1) tenderness of the navicular bone or the base of the fifth metatarsal or (2) inability to bear weight and walk 4 steps immediately after the injury or at the emergency room. These rules were later modified by Leddy et al90 to include tenderness at the middle third of the malleoli, with some improvement in specificity but no change in sensitivity compared with the standard OARs.
The OARs have been extensively studied for accuracy in predicting the presence of fractures in the ankle and midfoot of patients with an ankle sprain. Bachman et al8 conducted a systematic review of 27 studies involving 15 581 patients who had sustained an ankle sprain. The OARs demonstrated nearly 100% sensitivity in detecting a fracture of the ankle or midfoot, but specificity was quite variable, ranging from 10% to 79%. The missed fracture rate was 1.4%, which indicates that fewer than 2% of patients who were negative for fracture according to the OARs actually had a fracture.
A systematic review of studies of the accuracy of the OARs to exclude fracture of the ankle and midfoot in children was conducted by Dowling et al.9 Twelve studies of 3130 children (age range = 6 to 19 years) who presented to the emergency room after ankle trauma demonstrated 671 fractures (prevalence = 21.4%). The pooled sensitivity of the OARs to exclude fracture of the ankle or midfoot was 98.5%, whereas specificity was 7.9% to 50%. When the OARs were applied in this pediatric population, 1.2% of fractures were missed. The authors concluded that the OARs could reduce radiographs in children by 24.8%.
Jenkin et al91 noted several limitations of studies evaluating the OARs in athletic patients. Most investigations have been conducted in the emergency departments of hospitals, and few describe the qualifications of the clinicians who evaluated the patients. No studies of accuracy of application of the OARs by certified athletic trainers have been published.
Other fractures can accompany inversion ankle injury. Fractures of the anterior process of the calcaneus are caused by an avulsion injury from the bifurcate ligament, which occurs with forced inversion of the ankle and hindfoot. A snowboarder's injury, which may be misdiagnosed as a lateral ankle sprain, occurs when an abrupt shear force is exerted on the lateral process of the talus, resulting in fracture when the foot is in a dorsiflexed, externally rotated, and everted position. Inversion ankle injuries may also cause avulsion of the posterior-lateral process of the talus at the attachment site of the posterior talofibular ligament. Additionally, avulsion fractures at the base of the fifth metatarsal can occur from stretching of the peroneus brevis muscle during inversion trauma.92 Although all 3 types of fractures may be diagnosed with conventional radiographs, advanced techniques using CT or MRI are often required to adequately visualize the injury.93
Imaging: Ligamentous Injury
Several diagnostic imaging techniques are available to assess injury to ligaments after ankle trauma. The purpose of advanced imaging is to determine the exact location and severity of injury. However, imaging studies that evaluate ligament integrity have questionable value in assessing acute ankle injury because treatment decisions and outcomes are not usually influenced by the results of these studies.94
Stress radiography has long been used to diagnose mechanical instability of the lateral ligaments of the ankle, but the reliability of these measures has been questioned.11 Radiographic measurements of anterior drawer and talar tilt tests show low sensitivity (50% and 36%, respectively) but high specificity (100%).95 A critical review10 of 7 studies of stress radiography to diagnose ligamentous rupture after acute ankle sprain concluded that anterior drawer and talar tilt stress radiographs are not reliable enough to make the diagnosis of ligament rupture, regardless of whether mechanical devices or local anesthesia is used.
Other radiographic techniques used in the past include ankle arthrography and peroneal tenography. The accuracy of ankle arthrography ranges from 65% to 96%,18 and the accuracy of peroneal tenography to detect rupture of the CFL ranges from 83% to 95%.19 Disadvantages of arthrography include reduced accuracy 48 hours after trauma, the invasive nature of the procedure, and the lack of direct visualization of the injured ligaments.18
As the preferred imaging technique to detect ligament rupture after ankle sprain, MRI has replaced arthrography. However, the accuracy, sensitivity, and specificity of MRI to diagnose ligament injury in acute ankle sprains are inconsistent, particularly when acute injury is compared with CAI. The gold standard with which MRI is compared is intraoperative inspection. Breitenseher et al11 found 74% sensitivity and 100% specificity of MRI to detect lateral collateral ligament disruption after acute ankle injury. Conversely, Verhaven et al12 showed 100% sensitivity and 50% specificity for MRI to detect tears of the ATFL and 92% sensitivity and 100% specificity to detect tears of the CFL. In patients with CAI, MRI specificity was 100% for the diagnosis of ATFL and CFL tears, and accuracy was 91.7% for ATFL and 87.5% for CFL tears.96 In a mixed population of CAI and acute ankle instability patients, MRI showed 97% sensitivity, 100% specificity, and 97% accuracy.13 However, when evaluating only acutely injured patients, the results were 100% for all 3 categories.13 In addition, MRI can be useful in demonstrating any associated injuries that may delay complete recovery, such as osteochondral contusions in the ankle, which are prevalent after inversion sprains.97
The ankle syndesmotic ligament complex includes the anterior inferior tibiofibular ligament, posterior inferior tibiofibular ligament, interosseus ligament, and interosseous membrane. For athletes suspected of sustaining a high ankle sprain, plain radiographs are recommended and may demonstrate widening of the ankle mortise when the injury is significant.93 Less severe injuries to the syndesmosis will not show a clear change of alignment on plain radiographs, and additional evaluation with MRI imaging, CT, or arthroscopy is recommended.97 Overall, although radiographs can reveal frank diastasis of the ankle, they should not be relied upon to detect lesser degrees of syndesmotic injury.97,37 For evaluation of the ankle syndesmotic ligaments after acute injury, MRI has high sensitivity and specificity, with the former ranging from 93% to 100% and the latter ranging from 96% to 100%.20,98
Disadvantages of MRI for acute ankle injuries include cost, lack of accessibility in the average clinical setting, and time required for the test. Diagnostic ultrasound has gained increased popularity as an alternative to MRI because it is portable and less expensive and provides immediate and dynamic images for interpretation. However, it is important to note that these advantages are operator dependent. Oae et al13 prospectively studied 19 patients with acute ankle sprains and compared ultrasonography with MRI for accuracy in detecting injury to the ATFL as confirmed by arthroscopy. For ultrasound versus MRI, accuracy was 95% and 100%, and sensitivity was 50% and 100%, respectively. Other authors16,17 who compared ultrasonography for acute ankle injuries with surgical findings have shown accuracy ranging from 90% to 100% for both the ATFL and CFL.
Imaging: Osteochondral Injuries
An osteochondral lesion of the talus (OLT) is a defect in the articular cartilage and underlying cancellous bone. The cause of this injury has been debated, but there appears to be a strong link with trauma to the talus during inversion ankle injury. A comprehensive review99 of 582 patients with OLT lesions showed that 76% reported trauma99; 56% of the lesions were medial, and 44% were lateral. Patients who developed sequelae from inversion ankle injury had an incidence of OLT between 38% and 81%.100 Similarly, patients who underwent surgery for lateral ankle instability demonstrated a 17% to 63% incidence of OLT.101
Plain radiographs often do not reveal the presence or extent of OLT, particularly in cases of acute ankle trauma. When an OLT is suspected, MRI and CT both offer advantages. In 1 study,14 sensitivity and specificity for MRI, CT, and arthroscopy were 96%, 81%, and 100% and 96%, 99%, and 97%, respectively. Although CT may better show the extent of bone injury, MRI is preferred as the initial tool to evaluate OLT because a wider range of other conditions can also be detected.15
Management of Lateral Ankle Sprains
Rest, ice, compression, and elevation (RICE) is almost universally accepted as best practice by athletic trainers and other health care professionals immediately after acute ankle sprains.22,24,26,102 The acute phase of injury is defined as the period from the time of injury until the signs of inflammation (pain, heat, swelling, redness, and loss of function) peak and then begin to diminish. The subacute phase of injury occurs as the body shifts from inflammation to the proliferative stage, which is characterized by new collagen and capillary formation. The goals of acute care are to protect the injured ankle from further injury, control pain, limit swelling, and reduce the secondary hypoxic injury that results from the acute inflammatory reaction.26 In spite of this near-unanimous clinical consensus, limited evidence from high-quality randomized clinical trials supports the use of these interventions. Typically, components of RICE are applied simultaneously in both clinical practice and research studies, making it impossible to determine which components are truly effective or potentially deleterious.22,24 Sports health care professionals, athletic trainers in particular, advocate the application of RICE immediately after injury and are arguably the only health care professionals who can consistently apply these interventions within minutes because they are often on site at the time of injury. Most of the rationale for using RICE or individual components is based largely on low-quality clinical trials and laboratory studies with uninjured participants or animal models.22,24,27,33
Cryotherapy
Laboratory and animal studies indicate that cryotherapy reduces nerve conduction velocity, causing analgesia of the skin, curbing swelling formation, and decreasing metabolic activity and subsequent secondary injury.26,33 Strong clinical evidence for advocating cryotherapy is limited,22,24 and 1 author102 justified using cryotherapy on the basis that there is no evidence not to apply it.
Cryotherapy can be applied in a variety of modes, including ice packs, water immersion, application of frozen cups of ice, chemical cold packs, cold sprays, and the commercial units that are popular among clinicians. In addition to the various modes of application and differences in the duration of treatment, rates of reapplication are highly variable. Suggested times of 20 to 30 minutes are often recommended as they allow for temporary analgesia and may reduce secondary injury.26 This time interval was challenged by Bleakley et al,23 who compared a 20-minute treatment with two 10-minute treatments separated by a 10-minute rest period; the intermittent treatment produced less pain 1 week after injury, but no differences were seen in swelling and subjective function. Currently, the optimal mode, duration, and frequency of reapplication have not been established. Caution should be used when applying chemical cold packs: The below-freezing temperature and direct exposure to the skin can cause tissue damage.26 To reduce the risk of injury, a barrier, such as a wet towel, should be applied to the skin when using a chemical cold pack. During the subacute phase of therapy, cryotherapy can be applied for approximately 10 minutes to induce analgesia and allow exercise to improve ankle function (cryokinetics).26,37 Cryotherapy can be reapplied for 3 to 5 minutes to allow additional bouts of pain-free exercise. Although the clinical evidence is sparse, cryotherapy has been a mainstay of clinical practice for rehabilitation specialists.
Compression
Compression of the injured ankle is used to control swelling during the acute and subacute phases of injury25,26 and is applied in a variety of modes, including elastic wraps, adhesive tape, commercial braces, and units that apply simultaneous cold and compression. Acute inflammation increases the permeability of capillary walls, which allows fluid to escape the vasculature and enter the tissue spaces. Applying compression against the skin over the injured tissue controls hemorrhaging and is thought to increase the hydrostatic pressure at the injury site and counteract the increased osmotic pressure resulting from the injury.25–27 As with cryotherapy, limited evidence from high-quality clinical trials supports the use of compression, and minimal research supports the advantages and disadvantages of one mode of compression over another. Wilkerson and Horn-Kingery25 compared modes of compression and found that patients who received focal compression tended to recover function sooner than those who received uniform compression, but the differences were not statistically significant. Guskiewicz et al103 examined the effects of an elastic wrap and focal compression pad versus 2 commercial braces and noted no difference in pain, swelling, or function between groups. Tsang et al104 reported that intermittent compression and elevation reduced ankle volume, but swelling returned within 5 minutes after the treatment, thereby casting doubt on the clinical usefulness of the intervention. Rucinski et al105 showed that limb volume increased with elastic wraps and intermittent compression as compared with control limbs that were elevated. In addition, some clinicians apply adhesive tape without enclosing the entire ankle, leaving a portion of the dorsal aspect open to allow for additional swelling. However, the evidence to support or refute this open-basket-weave technique is essentially nonexistent. We are unaware of any reports of detrimental effects related to the application of compression after acute ankle sprain. Although compression has near-universal clinical acceptance, limited research and conflicting results make it difficult to provide specific treatment recommendations.
Electrical Stimulation
Electrical stimulation, in particular high-voltage pulsed current (HVPC), is a common adjunct to RICE in the acute and subacute phases of ankle sprains. Clinicians apply RICE and HVPC to sprains during the acute and subacute phases of injury in part to control edema because they believe that doing so eases acute symptoms, which may in turn affect the rate of recovery of normal function. Even though HVPC reduces capillary permeability and curbs edema formation in animal models,33 data from human studies do not support this intervention or other forms of electrical stimulation in managing ankle sprains.34 Recently, Mendel et al106 reported that near-continuous HVPC applied within 24 hours of acute lateral ankle sprains did not affect RTP in intercollegiate and professional athletes. Practical constraints delayed the initiation of electrical stimulation on average by almost 8 hours, well after edema formation was underway as a result of acute inflammation; this is a plausible rationale for the different outcomes between laboratory and clinical studies.
Thermotherapy
Traditionally, thermotherapy has not been recommended for acute management of ankle sprains given the widely held empirical belief that heat increases swelling and blood flow and exacerbates the injury. In 1 of the few studies of thermotherapy, Cote et al35 examined the effect of cold, warm, and contrast therapy (alternating cold and hot) on subacute ankle edema. No effect was reported, and all interventions increased limb volume, but the most significant increases were with warm and contrast therapies. As a result, thermotherapy is not recommended due to the lack of quality research needed to make a clinical recommendation either for or against the practice. Thermal ultrasound therapy is used by clinicians for a variety of soft tissue injuries to reduce pain and increase ROM, yet the literature does not support the use of ultrasound in managing ankle sprains due to the lack of high-quality clinical trials.36
Nonsteroidal Anti-Inflammatory Drugs
Strong evidence27,29 indicates that nonsteroidal anti-inflammatory drugs (NSAIDs) used during the acute and subacute phases of injury decrease pain and improve short-term function after acute ankle sprains. Slater et al29 compared piroxicam with placebo in 364 military recruits who sustained lateral ankle sprains. The NSAID group had less pain, returned to training more quickly, and had better exercise endurance than those who received placebo treatment. However, the piroxicam group had greater instability, less ROM, and more swelling 14 days after injury. The authors speculated that the analgesic effect of piroxicam might have allowed the participants to return to activity before the healing process was complete; this issue has been raised by others,27 who advise caution in using oral NSAIDs. Some107 have suggested that NSAIDs may result in reduced strength of the healed tendons and ligaments and may, therefore, make those structures more vulnerable to future injury. In addition, gastrointestinal irritation is common with NSAIDs. Adverse effects and other medical concerns must be factored into the decision by the athletic trainer and physician to include NSAIDs in the treatment plan for a lateral ankle sprain.
In addition to oral NSAIDs, topical NSAIDs have been effective in reducing pain and improving function in patients with ankle sprains and other soft tissue injuries.28 Topical NSAIDs in the form of creams, gels, and sprays are applied or massaged (or both) over the injury site and can be reapplied several times during the day, depending on the type of medication. The major advantages to topical NSAIDs are their effectiveness in reducing pain without systemic side effects. Mazieres et al28 examined the effects of an 8.2- × 11-cm ketoprofen patch applied over the painful region once per day for 7 days after acute sprains. This intervention resulted in reduced pain and swelling and improved self-reported function as compared with control limbs.28
In addition to oral and topical NSAIDs, alternative medicine that has purported anti-inflammatory effects may be of value in managing ankle sprains and other musculoskeletal conditions. Kucera et al108 examined the effects of high and low concentrations of a topical cream containing an extract from the flowering herb of a comfrey plant. A dosage of 2 to 3 g of cream was applied and massaged over the painful area 3 times per day. The higher concentration reduced pain at rest and with movement and improved function. The authors reported that the intervention was well tolerated. Growing acceptance of alternative treatments and patient requests for these interventions warrant further investigation.
Functional Rehabilitation
The standard of care for grade I and II lateral ankle sprains is functional rehabilitation, which consists of ankle stabilization (via elastic bandage, bracing, taping, or external support or a combination of these) with progressive weight bearing and exercise.30,31,109 Eiff et al109 compared early mobilization with immobilization (nonweight-bearing cast for 10 days) and found that the former group had less pain and returned to functional activities sooner than the latter group. Beynnon et al30 expanded the concept of functional rehabilitation by randomly assigning patients with first-time grade I ankle sprains into 3 treatment groups: elastic wrap, Air-Stirrup brace (Aircast Inc, Summit, NJ), and elastic wrap plus Air-Stirrup. Grade II sprains were treated similarly except that a fourth group wore a fiberglass walking cast for 10 days, followed by an elastic wrap. Grade III sprains were treated by either brace or cast for 10 days, followed by an elastic wrap. Patients with grade I sprains treated with the elastic wrap plus Air-Stirrup returned to normal stair climbing in 5.5 days, compared with 12 days for those who received only the elastic wrap. Patients with grade II sprains treated with the elastic wrap plus Air-Stirrup returned to normal stair climbing in 11.7 days, compared with those in a cast, who took almost 28 days. Patients with grade III sprains recovered similarly, regardless of the mode of functional treatment. This study provides compelling evidence for stirrup bracing and functional rehabilitation in the management of grade I and II ankle sprains.
The optimal management of grade III ankle sprains is less clear, but the current gold standard is functional rehabilitation.30,110 Clinical consensus suggests that some form of immobilization is necessary, although the best type and duration are currently unknown. Beynnon et al30 compared an Air-Stirrup ankle brace and below-knee walking cast for 10 days followed by the use of an elastic wrap and found no difference in the number of days needed to return to normal walking and stair climbing. Like grade I and II sprains, grade III sprains are often managed by functional rehabilitation.30 However, Lamb et al32 reported that patients who wore a below-knee cast for 10 days had recovered function more rapidly by 3 months postinjury as compared with patients treated with an elastic bandage. They also reported that the Aircast brace produced similar results to the below-knee cast for ankle function at 3 months. Although these studies favor functional rehabilitation in the short term, long-term results are seldom reported, and sequelae are common. Surgical intervention is indicated when functional rehabilitation has failed and patients have chronic symptoms. Secondary reconstruction of grade III injuries is possible even years after injury, and outcomes are similar to those for primary repair.111
Therapeutic Exercise
Therapeutic exercise, or functional treatment, includes interventions to restore ROM, strength, and sensorimotor function, which may be impaired after injury. This functional treatment has been shown to speed recovery when compared with immobilization. Bleakley et al38 reported that patients who received RICE and performed exercises had improved function at 1 to 2 weeks postinjury compared with patients who received RICE but delayed initiation of exercise for 1 week. However, at 4 weeks postinjury, there was no difference between groups. Currently, best practice for management of ankle sprains includes exercises and mobilization techniques to restore ROM and strength to the periarticular musculature and balance training to restore function and reduce the risk of reinjury.40–42,64,65,112,113
Strength and Muscle Activation Deficits
Concentric and eccentric strength deficits for the ankle evertors, invertors, and plantar flexors have been reported in the literature, both after acute injury and in patients with CAI, reinforcing the need to strengthen all muscles around the ankle after injury.114–119 Muscle inhibition may also occur from joint and ligamentous trauma and effusion after a lateral ankle sprain.118,120,121 The peroneal muscles may be injured with an inversion sprain, resulting in decreased motor recruitment initially after injury and leading to secondary loss of eversion strength.122 In 1998, Konradsen et al116 reported that they were unable to test isometric eccentric eversion strength in 20% (n = 9) of their 44 participants at 3 weeks postinjury. All participants demonstrated a decreased eccentric eversion moment postinjury that normalized at 6 weeks posttrauma. Acute ankle inversion trauma has also been reported to impair peroneal nerve function.122 Kleinrensink et al122 noted decreased superficial and deep peroneal motor nerve conduction velocity in all 22 patients examined 4 to 8 days postinjury. No clinical signs of peroneal nerve palsy were present, and the sample included patients with grade I, II, or III sprains. Although the peroneal nerve latency demonstrated a trend toward recovery, deep peroneal nerve motor conduction was still delayed at 5 weeks after injury. No correlation between nerve conduction velocity and clinical evaluation of ankle instability was reported.
Eccentric muscle actions may enhance joint stability by providing an antagonistic force that resists joint translation.120,123 Contributing factors for joint stability include both muscular strength and neuromuscular control. Therefore, a stronger muscle or muscle group has a greater ability to promote joint stability.123
Concentric eversion deficits have been associated with patients who exhibit functional ankle instability (FAI).112 Although the ability of the ankle evertors to contract in sufficient time to prevent sudden inversion has been questioned,66 addressing these deficits remains a popular clinical intervention strategy. In addition, inversion strength deficits have been reported after acute injury and in patients with FAI.65 Less studied are the roles of ankle dorsiflexor and plantar-flexor strength as contributing factors to FAI. Dorsiflexion strength does not appear to contribute to FAI, but deficits in eccentric plantar-flexor strength have been reported.124 Participants with FAI who were involved in a 6-week progressive exercise program (10 minutes, 3 times per week) of 4-way resistive ankle exercises improved their ankle dorsiflexion and eversion strength and ankle-joint position sense.39 Ankle-strengthening exercises are universally performed as part of a comprehensive rehabilitation program; however, the optimal mode and intensity of exercise used during rehabilitation are unknown. Clinical consensus suggests both open and closed chain exercises in a variety of modes should be performed to enhance muscle strength.102
ROM Exercises
After a sprain, ankle-dorsiflexion ROM may be impaired, which can lead to functional limitations in gait and contribute to FAI and reinjury.43,44 Youdas et al125 examined the effects of 6 weeks of static calf stretching ranging from 30 seconds to 2 minutes but found no difference in dorsiflexion ROM between groups. Clinicians often recommend various stretching interventions (eg, wall, slant board, towel stretches) intended to elongate the posterior calf muscle-tendon unit, but the type of stretching and duration needed to produce a clinically meaningful change in ROM are unknown. Historically, ROM exercises for the ankle and foot (ie, dorsiflexion, plantar flexion, inversion, and eversion) are initiated during the acute and subacute phases of injury, but no evidence exists to suggest that 1 type of exercise is superior or even efficacious for improving patient outcomes.
Joint Mobilization
Another clinical approach to improve dorsiflexion after ankle sprains involves joint mobilization techniques to improve arthrokinematic and osteokinematic motion. After an ankle sprain, posterior glide of the talus can be restricted and contribute to decreased dorsiflexion.43 Green et al126 reported that the addition of an anteroposterior joint mobilization to a standard RICE protocol improved dorsiflexion ROM and gait as compared with a group that received RICE alone. In addition, posterior talar mobilization with movement techniques increased ankle dorsiflexion and talar glide after ankle sprains in the short term.44
Mulligan127 proposed the concept of an anterior positional fault of the fibula after a lateral ankle sprain. He suggested that during plantar flexion and inversion, tension from the ATFL can displace the fibula anteriorly. Hubbard and Hertel128 reported that patients with subacute lateral ankle sprains had increased anterior positioning of the fibula as compared with the uninjured limb and matched controls. In addition, they showed a strong correlation between the amount of anterior positioning of the fibula and swelling. Management of positional faults with joint mobilization techniques and tape is gaining popularity, but further research is needed to clarify and substantiate the short- and long-term benefits of these interventions.
Sensorimotor Training
Freeman et al53 suggested that the high reinjury rate was, in part, caused by proprioceptive impairment after ankle sprains. Since then, balance and sensorimotor exercises have become an integral component of ankle rehabilitation and have been shown to effectively reduce ankle reinjury rates.40–42 Wester et al42 found that a 12-week wobble-board training program initiated 1 week after injury decreased the chance of developing FAI in the experimental group. Only 25% of patients who were treated with wobble-board training reinjured the ankle, compared with 54% of the control group. None of the experimental group reported subjective signs of instability, compared with 25% of those in the control group. Holme et al40 implemented 1 hour of supervised rehabilitation 2 times per week that focused on balance training; reinjury rates were 3% for treated limbs and 16% for control limbs. From these studies, McKeon and Hertel41 calculated a numbers-needed-to-treat (NNT) analysis and demonstrated an NNT of 5 for patients exposed to balance training. In other words, 5 patients exposed to balance and sensorimotor training would prevent 1 ankle reinjury. In addition, an 8-week unsupervised home-based neuromuscular training after ankle sprains reduced reinjury rates.54 Thus, balance training is a near-mandatory clinical intervention for athletes who have sustained an ankle sprain and especially for those individuals participating in high-risk activities such as basketball, soccer, volleyball, and football.
Acute and subacute management of lateral ankle sprains focuses on decreasing pain, minimizing swelling and secondary injury using RICE, and in some cases using NSAIDs. Functional rehabilitation is the treatment of choice for lateral ankle sprain and should include weight bearing as tolerated, ROM exercises, strengthening, joint mobilization techniques, and sensorimotor training as athletes transition into long-term management and return to function.
RTP Considerations
After a lateral ankle injury, it is often difficult to determine when an athlete can return to full sport participation. Although ROM, strength, and function are continually assessed during the rehabilitation process, it is also helpful to have quantifiable measures to assist in decision making. Two such measures are patient self-reports and functional performance tests. The following will provide an overview of current research related to this topic in the ankle-sprain literature.
Patient Self-Reports
When evaluating the effectiveness of any rehabilitation protocol, specific criteria are a vital component in injury management. Objective measures of function are a valuable part of this evaluation, but health-related quality-of-life assessments are equally important.129 In particular, patient self-reports can provide valuable information about an athlete's readiness to RTP. Over the years, various instruments have been developed, each designed to address either a particular condition or general lower leg and foot function. Several instruments that have been tested in patients with ankle ligament injuries will be described in greater detail. These include the Foot and Ankle Disability Index (FADI), Foot and Ankle Ability Measure (FAAM), Foot and Ankle Outcome Score, Lower Extremity Function Test (LEFS), Sports Ankle Rating System, Olerud Scoring Scale, and Karlsson Ankle Function Score. The Composite Inversion Injury Scale110 and Kaikkonen Functional Scale75,130 can also be used to evaluate patients with ankle sprains; however, they rely on clinician reports rather than patient self-reports of ankle function. Therefore, for the purpose of this paper, they were not included. Other instruments that were reviewed but have been tested using other lower extremity conditions were also not included in this review. This does not mean that these other instruments cannot be used in patients with lateral ankle sprains, only that research to date does not support their use in this population. The content validity, construct validity, reliability, and responsiveness to change of each instrument are specifically reported when available. Generally, content validity is the degree to which items on an instrument represent the attitude being tested. A group of items measures a behavior or construct. Reliability is the consistency of the instrument, and responsiveness to change is the degree to which an instrument can identify when a change occurs, such as after injury or a rehabilitation session.
The FADI was designed to identify functional limitations related to foot and ankle conditions. It has been used primarily in patients with CAI. It has 2 components: the main FADI with 26 items addresses activities of daily life, whereas the FADI-Sport has 8 items and addresses more advanced tasks that are related to physical activity.131 Each item is scored from 0 (unable to do) to 4 (no difficulty at all), and a higher score indicates a higher level of function. The FADI has been reported as reliable and sensitive in detecting injury and change.76 After extensive testing of the FADI, the FAAM was created.132 The FADI and FAAM are nearly identical, except that 5 items were removed from the latter after advanced psychometric testing was conducted. Therefore, the FAAM has 21 items related to activities of daily life and 8 items related to sport activity. The FAAM has construct validity for patients with CAI.133
The LEFS is a questionnaire that includes 20 items, and each item is scored from 0 (extreme difficulty or unable to perform activity) to 4 (no difficulty). It allows patients to report their ability to perform a variety of tasks that range from daily activities (eg, putting on shoes) to more advanced sport-specific tasks (running and hopping). The LEFS is a reliable and valid measure that is sensitive to change.134,135 Interestingly, this instrument does not ask questions that are specific to the ankle; however, it has been found to accurately report functional limitations in patients with acute inversion ankle sprains while also being sensitive to change in patients recovering from an ankle sprain.135
The Sports Ankle Rating System includes both self-assessment (Quality of Life) and clinically administered (Clinical Rating Score) components. This instrument is unique in that the components can be used individually or together to provide a more comprehensive evaluation.136 The Quality of Life outcome measure is a 5-part self-assessment questionnaire that evaluates symptoms, work and school activities, recreation and sports, activities of daily living, and lifestyle. Each item is graded using a Likert scale ranging from extreme dysfunction (0) to normal function (4). Therefore, a higher score indicates better function. The second component, the Clinical Rating Score, includes both patient-based and clinician-based parts. In the patient-based part, a visual analog scale is used to report the severity of pain, swelling, stiffness, giving way, and function. The clinician-based part evaluates gait, motion, strength, ligamentous stability, postural stability, and function. As a summary component, the Single Assessment Numeric Evaluation asks the patient to answer the following question: “On a scale of 0 to 100, how would you rate your ankle's function with 100 being normal?” The scale has excellent content validity and test-retest reliability.136 It also effectively differentiates between patients with and without ankle sprains and is responsive to change during the healing process.136
The Karlsson Ankle Function Score is an 8-item questionnaire that evaluates pain, swelling, instability, stiffness, stair climbing, running, work activities, and use of ankle supports. These items are scored; a total of 100 points indicates normal ankle function.137 Similarly, the Olerud Scoring Scale is a 9-item questionnaire that includes items related to pain, stiffness, swelling, stairs, running, jumping, squatting, use of supports, and daily life. It is also scored from zero to 100.138 Originally, the Olerud Scoring Scale was developed to evaluate the symptoms related to ankle fractures89 and other acute ankle injuries.139 Although both questionnaires have been used in research on patients with ankle injuries,139,140 no published evidence addresses their reliability or construct validity.
In summary, each of these questionnaires provides an opportunity to gather additional information related to an athlete's readiness to RTP after an ankle injury. No gold-standard questionnaire has been globally agreed upon, so clinicians should evaluate each questionnaire and determine which is best for their population and setting.
Functional Performance Testin
Restoration of sport-specific skills was 1 criterion identified in the American College of Sports Medicine's RTP consensus statement.141 Objectively, measurement of an athlete's ability to perform these skills is conducted through functional performance testing. Athletes should be able to perform a variety of functional tests from plyometric exercises to single-legged balance without pain or decreased performance before beginning sport activity.142–144 A variety of functional performance tests have been studied in participants with FAI,49–51,145,146 yet the research on functional limitation after acute lateral ankle injuries is limited, which makes it difficult to objectively measure when an athlete is ready to RTP.
Tests can progress from relatively simple tasks such as single-legged balance,130,147,148 1-legged heel or toe raises,130,148 or the Star Excursion Balance Test.149–151 All can be done without advanced laboratory or clinical equipment. The single-legged balance test measures the amount of time in balance and can be performed with the eyes open or closed.130,147,148 A more objective approach can be taken by incorporating the Balance Error Scoring System, which uses error measures that allow the clinician to quantify the athlete's postural stability. Although most of the research on the Balance Error Scoring System has been related to mild head injuries, 1 group152 identified balance deficits in participants with FAI. A more dynamic test is the single-legged heel or toe-rising test. When performed at a pace of 60 times per minute, this test can evaluate function and endurance of the lower leg muscles.130,148 Another dynamic measure of stability is the Star Excursion Balance Test (SEBT). To perform the SEBT, the athlete is instructed to stand on 1 leg and reach the contralateral leg as far as possible in 8 predetermined directions. (The 8-direction reach test was later simplified using a factor analysis.) Reach length is then standardized to the athlete's limb length.153 This functional test incorporates ROM, strength, proprioception, and neuromuscular control.150
The SEBT was determined to have a considerable amount of redundancy in the multiple reach directions. The posteromedial direction alone was the best predictor of overall performance in all directions.154 Subsequently, in an attempt to improve reliability and further simplify this dynamic task, instrumented systems that test 3 directions (anterior, posteromedial, and posterolateral) have been created. Intertester and intratester reliability of this less complex task were good to excellent.52 When dynamic balance was evaluated in patients with unilateral lateral ankle sprains using the SEBT, a significant balance deficit was identified in the sprained ankle compared with the contralateral, uninjured limb.55
A myriad of more advanced single-limbed hopping tasks have also been evaluated at the ankle based on time to completion, distance covered, or errors committed. Examples of these tests are the single-limb hopping course,49,146 1-legged hop for distance,51,146 triple-crossover hop for distance,146 6-m hop for time,146 cross 6-m hop for time,50,146 6-m shuttle run,56 single-limb hopping agility test,145 side hop,50,51 and figure-8 test.50,51 One objective criterion that has been proposed to indicate readiness to RTP is 80% or better performance on the functional hopping test compared with the uninjured limb.155,156
These functional performance tests can be used throughout the rehabilitation process but are particularly helpful when making RTP decisions. With objective measures to quantify progress during rehabilitation, the clinician has data to aid in decision making. However, none of these measures should be used independently; each provides specific information on an athlete's readiness to RTP.
Taping, Bracing, and Footwear Considerations
Taping and bracing of the ankle are common practices in the athletic setting. Generally, taping and bracing are used prophylactically in an effort to prevent a first-time ankle sprain or, more often, to prevent recurrent ankle sprains. A significant amount of research on taping and bracing has been conducted, but few authors have investigated if these measures can reduce the incidence of lateral ankle sprains. Garrick and Requa157 published 1 of the earliest studies on taping and bracing. They looked at intramural college basketball players over 2 years. One group received no tape, and the other received a standard tape application to the ankle. Interestingly, tape was more effective in those with a history of ankle sprains than in those without such a history.157 Although this initial work focused on ankle taping, most researchers have investigated the effects of ankle bracing on the prevalence of ankle sprains. Regardless of the population being tested, bracing was effective in reducing the incidence of ankle sprains.57–59,158,159–161 Sitler et al160 evaluated a group of intramural basketball players over 2 years. Approximately half of the athletes wore no ankle brace, and half wore an Aircast Sports Stirrup. Injury rates were lower in the brace group than in the no-brace group: 1.6 sprains versus 5.2 sprains, respectively, per 1000 exposures.160 Tropp et al57 assessed soccer players and found that only 3% of the athletes who used a specialized ankle brace sustained an ankle sprain, whereas 17% of the athletes in the no-brace group sustained a sprain.57 In a later study, Surve et al158 concluded that in those with a history of previous ankle sprain, the semirigid brace was effective in reducing the number of subsequent sprains. All of these studies used a semirigid brace. McGuine et al162 examined the effectiveness of lace-up ankle braces on first-time and recurrent ankle injuries in a group of high-risk high school basketball players. The lace-up ankle braces were beneficial in decreasing the rate of ankle injuries among high school basketball players, regardless of previous injuries.162 This tightly controlled randomized clinical trial is the best evidence yet to support the use of ankle bracing in preventing both first-time and subsequent ankle sprains.
When the effectiveness of taping to bracing was specifically compared, the results were mixed. Mickel et al59 found that taping and bracing were equally effective in reducing the incidence of ankle injuries. However, a limitation of their study was the relatively low number of ankle sprains that were reported. Conversely, 2 other groups58,159 reported that taping was much less effective than bracing in reducing the incidence of ankle injuries. Specifically, the use of an ankle brace reduced the risk of sustaining an ankle sprain by half compared with those who received ankle taping.58 An alternative way to evaluate this question is by determining the NNT to prevent a single ankle sprain. Olmstead et al163 demonstrated that 143 uninjured athletes and 26 previously injured athletes needed to be taped to prevent a single ankle sprain. When using a brace, the NNT was substantially lower. One limitation of this work is that only 3 published studies provided the data to conduct this calculation.157,158,160
Regardless of the type of prophylactic support, a common theme in the literature is that these methods are more effective in people with a history of ankle injuries.57,157,158,163,164 Surve et al158 found that only players who had a previous history of ankle sprains had a reduction in the incidence of ankle sprains when wearing a semirigid brace. In the athletes without a history of ankle injuries, there was no difference in the incidence of ankle sprains between the control and braced groups. This conclusion was reiterated in 2 systematic reviews163,164 that evaluated the effectiveness of ankle bracing and taping in preventing ankle sprains. The NNT to prevent a single ankle sprain was dramatically greater in athletes without a history of ankle sprain.163 For example, to prevent a sprain, 5 athletes with a history of ankle sprains needed to be braced, whereas 57 athletes without a history of ankle sprains needed to be braced.163 A separate systematic review164 concluded that athletes with previous ankle sprains who either braced or taped the ankle had approximately 70% fewer ankle injuries than the athletes without prophylactic support. These findings were not mirrored in the previously uninjured athletes, in whom no differences were identified between the braced or taped participants and those not wearing a support.164 These results prompt the question of whether it is appropriate to prophylactically brace or tape entire teams, regardless of the injury history. Recent evidence from the McGuine et al162 study suggests that bracing is effective and beneficial, even from a cost perspective, in the long run.
An additional issue that needs to be evaluated is whether bracing or taping the ankle has any negative effect on other joints in the lower extremity, specifically the knee. To date, bracing or taping the ankle does not seem to increase prevalence of knee injuries.157,158,160,165,166 However, most studies included a very small number of people who had sustained knee injuries, so definitive conclusions are difficult to make.
Work on the role of footwear in the incidence of ankle injuries has been limited and produced conflicting results. Part of this difference may be related to the type of athlete being studied. In basketball players, a high-top shoe with the ankle taped was more effective in preventing injuries than a low-top shoe with the ankle taped.157 Conversely, in football athletes, a low-top shoe with ankle stabilizer was more effective in preventing injuries than a high-top shoe with ankle stabilizer.58 Finally, 1 group60 reported no differences between high- and low-top shoes in altering the prevalence of ankle sprains in basketball players, but this may be a moot point in today's world, where most basketball footwear is either ¾ or full high top. The type of rear-foot cushioning may also contribute to the incidence of ankle sprains, but the literature on this topic conflicts as well. When elite basketball players were studied to determine which factors might predict the incidence of an ankle injury, those players who had shoes with air cells were 4 times more likely to sustain an ankle injury than those players who did not have shoes with air cells.61 More recently, springlike rear-foot cushioning was examined, and no difference was found in the prevalence of ankle sprain among different types of shoes.62 In general, more research related to this topic should be conducted before a conclusion can be drawn regarding the role of footwear in the incidence of ankle sprains.
Prevention of Lateral Ankle Sprains: Prophylactic Exercise
Prevention of orthopaedic injury is a high priority for all athletic trainers and other health care professionals who work with athletes. Information is available for external ankle supports, but data on other forms of injury prevention are limited. Most prospective studies aimed at determining the risk or incidence of ankle injury focus on balance and sensorimotor training. However, authors of some prospective investigations have looked at comprehensive programs designed to enhance strength, balance, sensorimotor function, and education about risk. Less compelling is other research that focused on strength and ROM deficits associated with a history of ankle injury. These may provide limited, indirect evidence of areas that should be considered in ankle-injury prevention.
The results of 2 recent prospective randomized controlled trials support the idea that supervised or unsupervised multi-intervention training reduces the risk of ankle injury by approximately 35% in athletes, especially court athletes.54,63 The NNT analysis performed in these controlled trials revealed that 7 to 9 players needed to be treated with an injury-prevention program to prevent 1 ankle injury. A systematic review by Hubscher et al167 suggested a similar reduction in risk (36%) of ankle sprains using comparable neuromuscular-control training regimens. The interventions in these studies included single-legged–stance balance training, balance training with additional perturbation, balance training with upper extremity movements or tasks, and dynamic jumping activities with a balance component. Other injury-prevention programs focusing on balance training have also shown a reduction in ankle-injury incidence, especially in athletes with a history of ankle injury.67–69 McKeon and Hertel41 reported a relative risk reduction of 20% to 60% based on these controlled trials.
Although this evidence appears compelling, many questions remain. The number of ankle sprains was reduced when each of these training programs was used; however, the reason for the reduction is largely unknown. Eils et al63 noted a decrease in postural sway during single-legged stance and less error in sagittal-plane angle reproduction along with a reduction in ankle sprains after a multi-intervention program. This would suggest that enhanced neuromuscular control translates into ankle-joint injury reduction, but more data are needed to solidify this conclusion. The duration, frequency, and length of the training programs reported here range from 10 minutes to 1 hour per session, repeated 1 to 7 times per week, and performed for 3 to 12 months. The optimal training protocol is still in question.
No direct evidence suggests that addressing ROM or strength should be considered strategies to prevent ankle injury. Yet indirectly, ROM and strength deficits have been identified in those with a history of ankle injury, and intuitively, each could play a role in providing mechanical and dynamic stability to the ankle during athletic activities. Strength deficits of leg muscles, specifically the plantar flexors,70,124 evertors,71,114 and invertors,65,71 have been reported in patients with ankle instability. Further, hip-extensor and -abductor strength deficits have been shown.70,168 Strength deficits and imbalances may play a role in vulnerable positioning of the foot relative to the center of mass during movement, adding to the risk of ankle injury. Dorsiflexion deficits during movement have also been demonstrated in those with ankle instability169,170; removing the foot from its most stable, closed-packed position during the stance phase of gait170 moves the toes closer to the ground during the swing phase.169 No evidence indicates that these deficits are present in athletes without ankle instability, but dysfunction of these muscles and dorsiflexion deficits may result in susceptible positions during movement, causing injury. Therefore, it may be prudent to assess strength and dorsiflexion ROM in athletes as preventive measures for ankle injury, especially in those with a history of ankle injury.
Special Considerations: Syndesmotic Ankle Sprains
Ankle sprains that produce tenderness proximal to the ankle joint and do not show signs of fracture or diastasis are commonly referred to as syndesmotic or high ankle sprains.83,171,172 They are frequently seen in athletes and may be associated with chronic pain, prolonged disability, recurrent ankle sprains, and heterotopic ossification.83,172,173 Syndesmotic ankle sprains are generally caused by hyperpronation (external rotation, eversion, and abduction), hyperdorsiflexion or hyperplantar flexion, or another athlete falling onto the fixed ankle.172,174 Syndesmotic injury can also occur in athletes enduring chronic inversion and axial loading.127,173,175 From an epidemiologic perspective, syndesmotic ankle sprains account for 1% to 11% of all ankle sprains171,172,176,177; however, in athletes, the prevalence rate may range from 40% to 74% of all ankle sprains.72,173,178
The primary role of the syndesmosis is to maintain congruency of the tibiotalar joint interface under physiologic axial loading.73 Clinicians need a thorough understanding of syndesmotic anatomy and biomechanics because recognizing proximal ankle injury can be difficult, given the variability in severity and disability of high ankle sprains.73,83,127 Disability can range from days to months. Definitive clinical tests with which to grade severity and predict disability are lacking.73,74 Several clinical tests have been reported in the literature, including the squeeze test, Kleiger test (with modifications using dorsiflexion with rotation), fibular translation test, and Cotton test, but none have been able to qualify the extent of injury. A positive squeeze test is less common but associated with a prolonged recovery. The modified Kleiger test has the greatest intertester agreement and the lowest rate of false-positive results162,164,169; however, it cannot identify the specific laxity or instability.73,74 When performing these tests, the clinician should be attentive to the provocation or reduction of symptoms that may indicate a syndesmotic injury. These clinical tests should be compared with the results of functional and radiographic studies to better determine the injury.
Classically, the patient will complain of difficulty “pushing off” or of “lacking power” when trying to regain normal function. The optimal imaging studies that should be used to identify this injury continue to be debated. Similarly, consensus is lacking as to how to appropriately manage syndesmotic injury, but most73,83,127,172,173 agree that early recognition and immobilization are important for appropriate care and recovery.
Management focuses on protecting the injured structures, treating symptoms, and increasing ROM, strength, and proprioceptive ability. For those injuries that demonstrate frank diastasis, joint incongruency on plain radiographs, or increased widening with stress radiographs, the diastasis may be best treated with surgical fixation.
The supportive role of the syndesmosis in normal ankle function cannot be overlooked. Therefore, a more conservative approach is needed to protect the syndesmosis, which is stressed throughout the ROM but particularly in the extremes of dorsiflexion and plantar flexion during weight bearing. No rehabilitation protocol is universally accepted, but recovery should focus on joint protection. Ankle braces that limit external rotation and extreme dorsiflexion and plantar flexion may be beneficial for those with syndesmotic ankle sprains. Rehabilitation emphasizes improving ROM, strength, proprioception, and functional ability. The RTP criteria should be based on ability to push off, run, cut, and function without gait limitations. Supportive taping and bracing limit hyperdorsiflexion, external rotation, and hyperpronation. An orthotic may be beneficial for functional return to activity.
Special Considerations: CAI
Chronic ankle instability is characterized by residual symptoms that include feelings of giving way and instability as well as repeated ankle sprains, persistent weakness, pain during activity, and self-reported disability.179 Two primary components of CAI are mechanical instability (ie, pathologic laxity, impaired arthrokinematics, and joint degenerative changes) and functional instability (ie, altered neuromuscular control, strength deficits, and deficient postural control).169
Chronic ankle instability is believed to occur secondary to an ankle sprain. Although most athletes return to full activity within 6 weeks of an ankle sprain, a large percentage (4% to 74%) report residual symptoms, including loss of function, repeated injury, and disability.180,181 Further, many athletes (74%) reported at least 1 residual symptom up to 4 years after injury.181 Often, an ankle injury is treated as a minor orthopaedic condition; however, in light of these data, clinicians should understand the potential link between ankle injury and CAI. Additionally, repetitive injury and other symptoms associated with CAI may lead to premature osteoarthritis.182
Several instruments have been developed to detect self-reported deficits associated with CAI.76–78,133 The FADI and its revised version, the FAAM; Ankle Instability Instrument; and CAIT are tools with published values for validity or reliability (or both).76–78,133 The FADI and FAAM provide a scale for activities of daily living and sports, offering added sensitivity for the athletic population.76,133 These tools are often used to identify a patient population to be studied in the research setting. However, they may also be used to detect the presence and severity of CAI in the clinical setting. The specific deficits that characterize mechanical ankle instability and FAI have been reviewed previously.70,183,184 Hubbard et al70 performed a relatively comprehensive assessment of CAI patients and reported that increased laxity (ie, greater inversion motion and anterior glide or the talus), balance deficits, and decreased dorsiflexion and plantar-flexion peak torque predicted CAI. Others noted limited dorsiflexion ROM,169,170 inhibition of the evertors and plantar flexors,185 diminished hip-abductor70,168 and -extensor70 strength, postural-control deficits,45,80 and altered movement strategies.79,169 These deficits and alterations are believed to contribute to the functional limitations and disability experienced by patients with CAI. Patients with CAI likely incorporate altered movement and protective strategies that predispose them to unprotected loads during functional movements.183 More data are needed to determine how each of these measured deficiencies contributes to the chronic nature of instability.
Given the many deficits that have been linked to CAI, clinicians should focus their management efforts on restoring identified deficiencies while maintaining normal movement strategies. Mobilization with movement techniques has been reported to enhance dorsiflexion ROM in participants with a history of ankle sprains.44,81,186 Hoch and McKeon187 warned that these data should be considered with caution because the effect sizes were small to moderate and the confidence intervals consistently crossed zero. Several groups63,188,18 have also shown positive outcomes in terms of reduced ankle sprains and measures of balance and postural control after exercise programs focused on progressive balance training, closed chain strengthening, and hopping exercises.9 These exercise programs varied, but all consisted of single-legged–stance activities that demanded balance in challenging environments (unstable surfaces, movement, additional upper extremity tasks, etc). Mohammadi189 used a single-legged–stance activity performed for 30 minutes every day during a soccer season. The activity progressed from a stable surface to an ankle disk and from eyes open to eyes closed. Eils et al63 used a series of stance, perturbed-stance, and jumping exercises performed once per week for 20 minutes over a single basketball season. Finally, McKeon et al188 used a series of stance, stance and reach, and jumping exercises performed 3 times per week for 4 weeks. More well-designed prospective studies are needed to determine if these intervention strategies have positive long-term outcomes for patients with CAI. For now, these strategies hold promise for reducing symptoms and risk; we must realize, however, that failed conservative management of CAI is still prevalent and other interventions (eg, surgery) may be necessary to help restore stability.
CONCLUSIONS
The clinical management of ankle sprains in athletes should include comprehensive assessment and treatment plans. Not all ankle sprains are alike, and it is important for each patient to have an individualized treatment plan. Because of the high frequency of recurrent ankle sprains, emphasis must be placed on preventing reinjury in addition to a safe return to athletic activities.
ACKNOWLEDGMENTS
We gratefully acknowledge the efforts of Richard Bouche, DPM; Douglas Comeau, DO; Phillip A. Gribble, PhD, ATC, FNATA; Arthur Horne, MEd, ATC, CSCS; Tricia Hubbard-Turner, PhD, ATC; and the Pronouncements Committee in the review of this document.
DISCLAIMER
The NATA and NATA Foundation publish position statements as a service to promote the awareness of certain issues to their members. The information contained in the position statement is neither exhaustive nor exclusive to all circumstances or individuals. Variables such as institutional human resource guidelines, state or federal statutes, rules, or regulations, as well as regional environmental conditions, may impact the relevance and implementation of these recommendations. The NATA and NATA Foundation advise members and others to carefully and independently consider each of the recommendations (including the applicability of same to any particular circumstance or individual). The position statement should not be relied upon as an independent basis for care but rather as a resource available to NATA members or others. Moreover, no opinion is expressed herein regarding the quality of care that adheres to or differs from the NATA and NATA Foundation position statements. The NATA and NATA Foundation reserve the right to rescind or modify its position statements at any time.
REFERENCES
- 1.Adams J, Barton E, Collings J, DeBlieux P, Gisondi M, Nadel E. Emergency Medicine. Philadelphia, PA: Saunders, Elsevier, Inc;; 2008. pp. 897–898. [Google Scholar]
- 2.Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11(3):659–662. doi: 10.1016/j.fcl.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37(4):376–380. [PMC free article] [PubMed] [Google Scholar]
- 5.Ebell M, Siwek J, Weiss B, et al. Strength of Recommendation Taxonomy (SORT): a patient-centered approach to grading evidence in medical literature. Am Fam Physician. 2004;69(3):548–556. [PubMed] [Google Scholar]
- 6.van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg Br. 1996;78(6):958–962. doi: 10.1302/0301-620x78b6.1283. [DOI] [PubMed] [Google Scholar]
- 7.van Dijk CN, Mol BW, Lim LS, Marti RK, Bossuyt PM. Diagnosis of ligament rupture of the ankle joint: physical examination, arthrography, stress radiography and sonography compared in 160 patients after inversion trauma. Acta Orthop Scand. 1996;67(6):566–570. doi: 10.3109/17453679608997757. [DOI] [PubMed] [Google Scholar]
- 8.Bachmann LM, Kolb E, Koller MT, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ. 2003;326(7386):417. doi: 10.1136/bmj.326.7386.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dowling S, Spooner CH, Liang Y, et al. Accuracy of Ottawa Ankle Rules to exclude fractures of the ankle and midfoot in children: a meta-analysis. Acad Emerg Med. 2009;16(4):277–287. doi: 10.1111/j.1553-2712.2008.00333.x. [DOI] [PubMed] [Google Scholar]
- 10.Frost SC, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999;9(1):40–45. doi: 10.1097/00042752-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Breitenseher MJ, Trattnig S, Kukla C, et al. MRI versus lateral stress radiography in acute lateral ankle ligament injuries. J Comput Assist Tomogr. 1997;21(2):280–285. doi: 10.1097/00004728-199703000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Verhaven EF, Shahabpour M, Handelberg FW, Vaes PH, Opdecam PJ. The accuracy of three-dimensional magnetic resonance imaging in the diagnosis of ruptures of the lateral ligaments of the ankle. Am J Sports Med. 1991;19(6):583–587. doi: 10.1177/036354659101900605. [DOI] [PubMed] [Google Scholar]
- 13.Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skelet Radiol. 2010;39(1):41–47. doi: 10.1007/s00256-009-0767-x. [DOI] [PubMed] [Google Scholar]
- 14.Verhagen RA, Maas M, Dijkgraaf MG, Tol JL, Krips R, van Dijk CN. Prospective study on diagnostic strategies in osteochondral lesions of the talus. Is MRI superior to helical CT? J Bone Joint Surg Br. 2005;87(1):41–46. [PubMed] [Google Scholar]
- 15.DeSmet AA, Dalinka MK, Alazraki N, et al. Chronic ankle pain. American College of Radiology. ACR appropriateness criteria. Radiology. 2000;215((suppl)):321–332. [PubMed] [Google Scholar]
- 16.Friedrich JM, Schnarkowski P, Rubenacker S, Wallner B. Ultrasonography of capsular morphology in normal and traumatic ankle joints. J Clin Ultrasound. 1993;21(3):179–187. doi: 10.1002/jcu.1870210306. [DOI] [PubMed] [Google Scholar]
- 17.Peetrons P, Creteur V, Bacq C. Sonography of ankle ligaments. J Clin Ultrasound. 2004;32(9):491–499. doi: 10.1002/jcu.20068. [DOI] [PubMed] [Google Scholar]
- 18.Beumer A, Swierstra BA, Mulder PG. Clinical diagnosis of syndesmotic ankle instability: evaluation of stress tests behind the curtains. Acta Orthop Scand. 2002;73(6):667–669. doi: 10.1080/000164702321039642. [DOI] [PubMed] [Google Scholar]
- 19.Evans GA, Frenyo SD. The stress tenogram in the diagnosis of ruptures of the lateral ligaments of the ankle. J Bone Joint Surg Br. 1979;61(3):347–351. doi: 10.1302/0301-620X.61B3.113414. [DOI] [PubMed] [Google Scholar]
- 20.Vogl TJ, Hochmuth K, Diebold T, et al. Magnetic resonance imaging in the diagnosis of acute injured distal tibiofibular syndesmosis. Invest Radiol. 1997;32(7):401–409. doi: 10.1097/00004424-199707000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Muhle C, Frank LR, Rand T, et al. Tibiofibular syndesmosis: high resolution MRI using a local gradient coil. J Comput Assist Tomogr. 1998;22(6):938–944. doi: 10.1097/00004728-199811000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med. 2004;32(1):251–261. doi: 10.1177/0363546503260757. [DOI] [PubMed] [Google Scholar]
- 23.Bleakley CM, McDonough SM, MacAuley DC, Bjordal J. Cryotherapy for acute ankle sprains: a randomised controlled study of two different icing protocols. Br J Sports Med. 2006;40(8):700–705. doi: 10.1136/bjsm.2006.025932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hubbard TJ, Aronson SL, Denegar CR. Does cryotherapy hasten return to participation? A systematic review. J Athl Train. 2004;39(1):88–94. [PMC free article] [PubMed] [Google Scholar]
- 25.Wilkerson GB, Horn-Kingery HM. Treatment of the inversion ankle sprain: comparison of different modes of compression and cryotherapy. J Orthop Sports Phys Ther. 1993;17(5):240–246. doi: 10.2519/jospt.1993.17.5.240. [DOI] [PubMed] [Google Scholar]
- 26.Knight KL. Cryotherapy in Sport Injury Management. Champaign, IL: Human Kinetics;; 1995. p. 92. [Google Scholar]
- 27.Bleakley CM, McDonough SM, MacAuley DC. Some conservative strategies are effective when added to controlled mobilisation with external support after acute ankle sprain: a systematic review. Aust J Physiother. 2008;54(1):7–20. doi: 10.1016/s0004-9514(08)70061-8. [DOI] [PubMed] [Google Scholar]
- 28.Mazieres B, Rouanet S, Velicy J, Scarsi C, Reiner V. Topical ketoprofen patch (100 mg) for the treatment of ankle sprain a randomized, double-blind, placebo-controlled study. Am J Sports Med. 2005;33(4):515–523. doi: 10.1177/0363546504268135. [DOI] [PubMed] [Google Scholar]
- 29.Slatyer MA, Hensley MJ, Lopert R. A randomized controlled trial of piroxicam in the management of acute ankle sprain in Australian Regular Army recruits: the Kapooka Ankle Sprain Study. Am J Sports Med. 1997;25(4):544–553. doi: 10.1177/036354659702500419. [DOI] [PubMed] [Google Scholar]
- 30.Beynnon BD, Renstrom PA, Haugh L, Uh BS, Barker H. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. Am J Sports Med. 2006;34(9):1401–1412. doi: 10.1177/0363546506288676. [DOI] [PubMed] [Google Scholar]
- 31.Kerkhoffs GM, Rowe BH, Assendelft WJ, Kelly K, Struijs PA, van Dijk C. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;(3) doi: 10.1002/14651858.CD003762. CD003762. [DOI] [PubMed] [Google Scholar]
- 32.Lamb SE, Marsh JL, Hutton JL, et al. Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet. 2009;373(9663):575–581. doi: 10.1016/S0140-6736(09)60206-3. [DOI] [PubMed] [Google Scholar]
- 33.Dolan MG, Mychaskiw AM, Mendel FC. Cool-water immersion and high-voltage electric stimulation curb edema formation in rats. J Athl Train. 2003;38(3):225–230. [PMC free article] [PubMed] [Google Scholar]
- 34.Snyder AR, Perotti AL, Lam KC, Bay RC. The influence of high-voltage electrical stimulation on edema formation after acute injury: a systematic review. J Sport Rehabil. 2010;19(4):436–451. doi: 10.1123/jsr.19.4.436. [DOI] [PubMed] [Google Scholar]
- 35.Cote DJ, Prentice WE, Jr, Hooker DN, Shields EW. Comparison of three treatment procedures for minimizing ankle sprain swelling. Phys Ther. 1988;68(7):1072–1076. doi: 10.1093/ptj/68.7.1072. [DOI] [PubMed] [Google Scholar]
- 36.Van Der Windt DA, Van Der Heijden GJ, Van Den Berg SG, Ter Riet G, De Winter AF, Bouter LM. Ultrasound therapy for acute ankle sprains. Cochrane Database Syst Rev. 2002;(1) doi: 10.1002/14651858.CD001250. CD001250. [DOI] [PubMed] [Google Scholar]
- 37.Pincivero DM, Gieck JH, Saliba EN. Rehabilitation of a lateral ankle sprain with cryokinetics and functional progressive exercise. J Sport Rehabil. 1993;2(3):200–207. [Google Scholar]
- 38.Bleakley CM, O'Connor SR, Tulty MA, et al. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. BMJ. 2010 doi: 10.1136/bmj.c1964. 340:c1964. [DOI] [PubMed] [Google Scholar]
- 39.Docherty CL, Moore JH, Arnold BL. Effects of strength training on strength development and joint position sense in functionally unstable ankles. J Athl Train. 1998;33(4):310–314. [PMC free article] [PubMed] [Google Scholar]
- 40.Holme E, Magnusson SP, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9(2):104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 41.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athl Train. 2008;43(3):305–315. doi: 10.4085/1062-6050-43.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23(5):332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 43.Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32(4):166–173. doi: 10.2519/jospt.2002.32.4.166. [DOI] [PubMed] [Google Scholar]
- 44.Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36(7):464–471. doi: 10.2519/jospt.2006.2265. [DOI] [PubMed] [Google Scholar]
- 45.McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. doi: 10.1186/1471-2474-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cronkey J, Laporto G. Rating systems for evaluation of functional ankle instability: prospective evaluation in a cohort of patients treated with monopolar capacitive-coupled radiofrequency. Foot Ankle Spec. 2012;5(5):293–299. doi: 10.1177/1938640012457941. [DOI] [PubMed] [Google Scholar]
- 47.McNair PJ, Prapavessis H, Collier J, Bassett S, Bryant A, Larmer P. The lower-limb task questionnaire: an assessment of validity, reliability, responsiveness, and minimal important differences. Arch Phys Med Rehabil. 2007;88(8):993–1001. doi: 10.1016/j.apmr.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 48.Larmer P, McNair PJ, Smythe L, Williams M. Ankle sprains: patients perceptions of function and performance of physical tasks: a mixed methods approach. Disabil Rehabil. 2011;33((23–24)):2299–2304. doi: 10.3109/09638288.2011.568668. [DOI] [PubMed] [Google Scholar]
- 49.Buchanan AS, Docherty CL, Schrader J. Functional performance testing in participants with functional ankle instability and in a healthy control group. J Athl Train. 2008;43(4):342–346. doi: 10.4085/1062-6050-43.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Caffrey E, Docherty CL, Schrader J, Klossner J. The ability of 4 single-limb hopping tests to detect functional performance deficits in individuals with functional ankle instability. J Orthop Sports Phys Ther. 2009;39(11):799–806. doi: 10.2519/jospt.2009.3042. [DOI] [PubMed] [Google Scholar]
- 51.Docherty CL, Arnold BL, Gansneder BM, Hurwitz S, Gieck J. Functional-performance deficits in volunteers with functional ankle instability. J Athl Train. 2005;40(1):30–34. [PMC free article] [PubMed] [Google Scholar]
- 52.Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the Star Excursion Balance Test. N Am J Sports Phys Ther. 2009;4(2):92–99. [PMC free article] [PubMed] [Google Scholar]
- 53.Freeman MA, Dean MR, Hanham IW. Etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47(4):678–685. [PubMed] [Google Scholar]
- 54.Hupperets MD, Verhagen EA, van Mechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomised controlled trial. BMJ. 2009 doi: 10.1136/bmj.b2684. 339:b2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Akbari M, Karimi H, Farahini H, Faghihzadeh S. Balance problems after unilateral lateral ankle sprains. J Rehabil Res Dev. 2006;43(7):819–824. doi: 10.1682/jrrd.2006.01.0001. [DOI] [PubMed] [Google Scholar]
- 56.Demeritt KM, Shultz SJ, Docherty CL, Gansneder BM, Perrin DH. Chronic ankle instability does not affect lower extremity functional performance. J Athl Train. 2002;37(4):507–511. [PMC free article] [PubMed] [Google Scholar]
- 57.Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13(4):259–262. doi: 10.1177/036354658501300408. [DOI] [PubMed] [Google Scholar]
- 58.Rovere G, Clarke T, Yates C, Burley K. Retrospective comparison of taping and ankle stabilizers in preventing ankle injuries. Am J Sports Med. 1988;16(3):228–233. doi: 10.1177/036354658801600305. [DOI] [PubMed] [Google Scholar]
- 59.Mickel TJ, Bottoni CR, Tsuji G, Change K, Baum L, Tokushige KA. Prophylactic bracing versus taping for the prevention of ankle sprains in high school athletes: a prospective, randomized trial. Foot Ankle Surg. 2006;45(6):360–365. doi: 10.1053/j.jfas.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 60.Barrett JR, Tanji JL, Drake C, Fuller D, Kawasaki RI, Fenton RM. High versus low top shoes for the prevention of ankle sprains in basketball players: a prospective randomized study. Am J Sports Med. 1993;21(4):582–585. doi: 10.1177/036354659302100416. [DOI] [PubMed] [Google Scholar]
- 61.McKay G, Goldie P, Payne W, Oakes B. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Curtis CK, Laudner KG, McLoda TA, McCaw ST. The role of shoe design in ankle sprain rates among collegiate basketball players. J Athl Train. 2008;43(3):230–233. doi: 10.4085/1062-6050-43.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eils E, Schroter R, Schroder M, Gerss J, Rosenbaum D. Multistation proprioceptive exercise program prevents ankle injuries in basketball. Med Sci Sports Exerc. 2010;42(11):2098–2105. doi: 10.1249/MSS.0b013e3181e03667. [DOI] [PubMed] [Google Scholar]
- 64.Kaminski TW, Hartsell HD. Factors contributing to chronic ankle instability: a strength perspective. J Athl Train. 2002;37(4):394–405. [PMC free article] [PubMed] [Google Scholar]
- 65.Wilkerson GB, Pinerola JJ, Caturano RW. Invertor vs. evertor peak torque and power deficiencies associated with lateral ankle ligament injury. J Orthop Sports Phys Ther. 1997;26(2):78–86. doi: 10.2519/jospt.1997.26.2.78. [DOI] [PubMed] [Google Scholar]
- 66.Konradsen L, Voigt M, Hojsgaard C. Ankle inversion injuries: the role of the dynamic defense mechanism. Am J Sports Med. 1997;25(1):54–58. doi: 10.1177/036354659702500110. [DOI] [PubMed] [Google Scholar]
- 67.Verhagen E, van der Beek A, Twisk J, Bouter L, Bahr R, van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32(6):1385–1393. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
- 68.McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34(7):1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- 69.Bahr R, Lian O, Bahr IA. A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: a prospective cohort study. Scand J Med Sci Sports. 1997;7(3):172–177. doi: 10.1111/j.1600-0838.1997.tb00135.x. [DOI] [PubMed] [Google Scholar]
- 70.Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Contributing factors to chronic ankle instability. Foot Ankle Int. 2007;28(3):343–354. doi: 10.3113/FAI.2007.0343. [DOI] [PubMed] [Google Scholar]
- 71.Hartsell HD, Spaulding SJ. Eccentric/concentric ratios at selected velocities for the invertor and evertor muscles of the chronically unstable ankle. Br J Sports Med. 1999;33(4):255–258. doi: 10.1136/bjsm.33.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kim S, Huh Y, Song H, et al. Chronic tibiofibular syndesmosis injury of ankle: evaluation with contrast-enhanced fat-suppressed 3D fast spoiled gradient-recalled acquisition in the steady state MR imaging. Radiology. 2007;2(1):225–235. doi: 10.1148/radiol.2421051369. 24. [DOI] [PubMed] [Google Scholar]
- 73.Lin CF, Gross ML, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006;36(6):372–384. doi: 10.2519/jospt.2006.2195. [DOI] [PubMed] [Google Scholar]
- 74.Beumer A, Valstar ER, Garling EH, et al. Effects of ligament sectioning on the kinematics of the distal tibiofibular syndesmosis: a radiostereometric study of 10 cadaveric specimens based on presumed trauma mechanisms with suggestions for treatment. Acta Orthop. 2006;77(3):531–540. doi: 10.1080/17453670610012557. [DOI] [PubMed] [Google Scholar]
- 75.Kaikkonen A, Kannus P, Jurvinen M. Surgery versus functional treatment in ankle ligament tears. Clin Orthop Rel Res. 1996;326:194–202. doi: 10.1097/00003086-199605000-00023. [DOI] [PubMed] [Google Scholar]
- 76.Hale SA, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 77.Docherty CL, Gansneder BM, Arnold BL, Hurwitz SR. Development and reliability of the ankle instability instrument. J Athl Train. 2006;41(2):154–158. [PMC free article] [PubMed] [Google Scholar]
- 78.Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland Ankle Instability Tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 79.Delahunt E, Monaghan K, Caulfield B. Ankle function during hopping in subjects with functional instability of the ankle joint. Scand J Med Sci Sports. 2007;17(6):641–648. doi: 10.1111/j.1600-0838.2006.00612.x. [DOI] [PubMed] [Google Scholar]
- 80.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part I: can deficits be detected with instrumented testing? J Athl Train. 2008;43(3):293–304. doi: 10.4085/1062-6050-43.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Collins N, Teys P, Vicenzino B. The initial effects of a Mulligan's mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man Ther. 2004;9(2):77–82. doi: 10.1016/S1356-689X(03)00101-2. [DOI] [PubMed] [Google Scholar]
- 82.Holmer P, Sondergaard L, Konradsen L, Nielsen PT, Jorgensen LN. Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int. 1994;15(2):72–74. doi: 10.1177/107110079401500204. [DOI] [PubMed] [Google Scholar]
- 83.Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29(1):31–35. doi: 10.1177/03635465010290011001. [DOI] [PubMed] [Google Scholar]
- 84.Man IO, Morrissey MC. Relationship between ankle-foot swelling and self-assessed function after ankle sprain. Med Sci Sports Exerc. 2005;37(3):360–363. doi: 10.1249/01.mss.0000155435.10686.04. [DOI] [PubMed] [Google Scholar]
- 85.Fallat L, Grimm DJ, Saracco JA. Sprained ankle syndrome: prevalence and analysis of 639 acute injuries. J Foot Ankle Surg. 1998;37(4):280–285. doi: 10.1016/s1067-2516(98)80063-x. [DOI] [PubMed] [Google Scholar]
- 86.Blanshard KS, Finaly DB, Scott DJ, Ley CC, Siggins D, Allen MJ. A radiological analysis of lateral ligament injuries of the ankle. Clin Radiol. 1986;37(3):247–251. doi: 10.1016/s0009-9260(86)80328-2. [DOI] [PubMed] [Google Scholar]
- 87.Raatikainen T, Putkonen M, Puranen J. Arthrography, clinical examination, and stress radiograph in the diagnosis of acute injury to the lateral ligaments of the ankle. Am J Sports Med. 1992;20(1):2–6. doi: 10.1177/036354659202000102. [DOI] [PubMed] [Google Scholar]
- 88.Sujitkumar P, Hadfield JM, Yates DW. Sprain or fracture? An analysis of 2000 ankle injuries. Arch Emerg Med. 1986;3(2):101–106. doi: 10.1136/emj.3.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Worthington JR. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann Emerg Med. 1992;21(4):384–399. doi: 10.1016/s0196-0644(05)82656-3. [DOI] [PubMed] [Google Scholar]
- 90.Leddy JJ, Smolinski RJ, Lawrence J, Snyder JL, Priore RL. Prospective evaluation of the Ottawa ankle rules in a university sports medicine center: with a modification to increase specificity for identifying malleolar fractures. Am J Sports Med. 1998;26(2):158–165. doi: 10.1177/03635465980260020201. [DOI] [PubMed] [Google Scholar]
- 91.Jenkin M, Sitler MR, Kelly JD. Clinical usefulness of the Ottawa Ankle Rules for detecting fractures of the ankle and midfoot. J Athl Train. 2010;45(5):480–482. doi: 10.4085/1062-6050-45.5.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Egol K, Walsh M, Rosenblatt K, Capla E, Koval KJ. Avulsion fractures of the fifth metatarsal base: a prospective outcome study. Foot Ankle Int. 2007;28(5):581–583. doi: 10.3113/FAI.2007.0581. [DOI] [PubMed] [Google Scholar]
- 93.Collins MS. Imaging evaluation of chronic ankle and hindfoot pain in athletes. Magn Reson Imaging Clin N Am. 2008;16(1):39–58. doi: 10.1016/j.mric.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 94.Griffith JF, Brockwell J. Diagnosis and imaging of ankle instability. Foot Ankle Clin. 2006;11(3):475–496. doi: 10.1016/j.fcl.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 95.Harper MC. Stress radiographs in the diagnosis of lateral instability of the ankle and hindfoot. Foot Ankle. 1992;13(8):435–438. doi: 10.1177/107110079201300801. [DOI] [PubMed] [Google Scholar]
- 96.Joshy S, Abdulkadir U, Chaganti S, Sullivan B, Hariharan K. Accuracy of MRI scan in the diagnosis of ligamentous and chondral pathology in the ankle. Foot Ankle Surg. 2010;16(2):78–80. doi: 10.1016/j.fas.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 97.Beumer A, van Hemert WL, Niesing R, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004;423:227–234. doi: 10.1097/01.blo.0000129152.81015.ad. [DOI] [PubMed] [Google Scholar]
- 98.Nielson JH, Gardner MJ, Peterson MG, et al. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res. 2005;432:216–221. doi: 10.1097/01.blo.0000161090.86162.19. [DOI] [PubMed] [Google Scholar]
- 99.Tol JL, Struijs PA, Bossuyt PM, Verhagen RA, van Dijk CN. Treatment strategies in osteochondral defects of the talar dome: a systematic review. Foot Ankle Int. 2000;21(2):119–126. doi: 10.1177/107110070002100205. [DOI] [PubMed] [Google Scholar]
- 100.Takao M, Uchio Y, Naito K, Fukazawa I, Ochi M. Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med. 2005;33(5):686–692. doi: 10.1177/0363546504270566. [DOI] [PubMed] [Google Scholar]
- 101.Ferkel RD, Zanotti RM, Komenda GA, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: long-term results. Am J Sports Med. 2008;36(9):1750–1762. doi: 10.1177/0363546508316773. [DOI] [PubMed] [Google Scholar]
- 102.Ivins D. Acute ankle sprain: an update. Am Fam Physician. 2006;74(10):1714–1720. [PubMed] [Google Scholar]
- 103.Guskiewicz KM, Riemann BL, Onate JA. Comparison of 3 methods of external support for management of acute lateral ankle sprains. J Athl Train. 1999;34(1):5–10. [PMC free article] [PubMed] [Google Scholar]
- 104.Tsang KKW, Hertel J, Denegar CR. Volume decreases after elevation and intermittent compression of postacute ankle sprains are negated by gravity-dependent positioning. J Athl Train. 2003;38(4):320–324. [PMC free article] [PubMed] [Google Scholar]
- 105.Rucinski TJ, Hooker DN, Prentice WE, Shields EW, Cote-Murray DJ. The effects of intermittent compression on edema in postacute ankle sprains. J Orthop Sports Phys Ther. 1991;14(2):65–69. doi: 10.2519/jospt.1991.14.2.65. [DOI] [PubMed] [Google Scholar]
- 106.Mendel FC, Dolan MG, Fish DR, Marzo J, Wilding GE. Effect of high-voltage pulsed current on recovery after Grades I and II lateral ankle sprains. J Sport Rehabil. 2010;19(4):399–410. doi: 10.1123/jsr.19.4.399. [DOI] [PubMed] [Google Scholar]
- 107.Mishra DK, Fridén J, Schmitz MC, Lieber RL. Anti-inflammatory medication after muscle injury: a treatment resulting in short-term improvement but subsequent loss of muscle function. J Bone Joint Surg Am. 1995;77(10):1510–1519. doi: 10.2106/00004623-199510000-00005. [DOI] [PubMed] [Google Scholar]
- 108.Kucera M, Barna M, Horacek O, Kovarikova J, Kucera A. Efficacy and safety of topically applied Symphytum herb extract cream in the treatment of ankle distortion: results of a randomized controlled clinical double blind study. Wien Med Wochenschr. 2004;154((21–22)):498–507. doi: 10.1007/s10354-004-0114-8. [DOI] [PubMed] [Google Scholar]
- 109.Eiff MP, Smith AT, Smith GE. Early mobilization versus immobilization in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22(1):83–88. doi: 10.1177/036354659402200115. [DOI] [PubMed] [Google Scholar]
- 110.Linde F, Hvass I, Jurgensen U, Madsen F. Compression bandage in the treatment of ankle sprains: a comparative prospective study. Scand J Rehabil Med. 1984;16(4):177–179. [PubMed] [Google Scholar]
- 111.Lynch SA, Renström PA. Treatment of acute lateral ankle ligament rupture in the athlete. Conservative versus surgical treatment. Sports Med. 1999;27(1):61–71. doi: 10.2165/00007256-199927010-00005. [DOI] [PubMed] [Google Scholar]
- 112.Arnold BL, Linens SW, de la Motte SJ, Ross SE. Concentric evertor strength differences and functional ankle instability: a meta-analysis. J Athl Train. 2009;44(6):653–662. doi: 10.4085/1062-6050-44.6.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29(5):361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- 114.Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7(5):291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- 115.Baumhauer JF, Alosa DM, Renstrom AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23(5):564–570. doi: 10.1177/036354659502300508. [DOI] [PubMed] [Google Scholar]
- 116.Konradsen L, Olesen S, Hansen HM. Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. Am J Sports Med. 1998;26(1):72–77. doi: 10.1177/03635465980260013001. [DOI] [PubMed] [Google Scholar]
- 117.Yildiz Y, Aydin T, Sekir U, Hazneci B, Komurcu M, Kalyon TA. Peak and end range eccentric evertor/concentric invertor muscle strength ratios in chronically unstable ankles: comparison with healthy individuals. J Sports Sci Med. 2003;2(3):70–76. [PMC free article] [PubMed] [Google Scholar]
- 118.Hopkins JT, Palmieri R. Effects of ankle joint effusion on lower leg function. Clin J Sport Med. 2004;14(1):1–7. doi: 10.1097/00042752-200401000-00001. [DOI] [PubMed] [Google Scholar]
- 119.Palmieri-Smith RM, Hopkins JT, Brown TN. Peroneal activation deficits in persons with functional ankle instability. Am J Sports Med. 2009;37(5):982–988. doi: 10.1177/0363546508330147. [DOI] [PubMed] [Google Scholar]
- 120.Wilkerson GB, Nitz AJ. Dynamic ankle stability: mechanical and neuromuscular interrelationships. J Sport Rehabil. 1994;3(1):43–57. [Google Scholar]
- 121.Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29(5):361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- 122.Kleinrensink GJ, Stoeckart R, Meulstee J, et al. Lowered motor conduction velocity of the peroneal nerve after inversion trauma. Med Sci Sports Exerc. 1994;26(7):877–883. [PubMed] [Google Scholar]
- 123.Blackburn JT, Prentice WE, Guskiewicz KM, Busby MA. Balance and joint stability: the relative contributions of proprioception and muscular strength. J Sport Rehabil. 2000;9(4):315–328. [Google Scholar]
- 124.Fox J, Docherty CL, Schrader J, Applegate T. Eccentric plantar-flexor torque deficits in participants with functional ankle instability. J Athl Train. 2008;43(1):51–54. doi: 10.4085/1062-6050-43.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Youdas JW, McLean TJ, Krause DA, Hollman JH. Changes in active ankle dorsiflexion range of motion after acute inversion ankle sprain. J Sport Rehabil. 2009;18(3):358–374. doi: 10.1123/jsr.18.3.358. [DOI] [PubMed] [Google Scholar]
- 126.Green T, Refshauge K, Crosbie J, Adams R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys Ther. 2001;81(4):984–994. [PubMed] [Google Scholar]
- 127.Mulligan EP. Evaluation and management of ankle syndesmosis injuries. Phys Ther Sport. 2011;12(2):57–69. doi: 10.1016/j.ptsp.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 128.Hubbard TJ, Hertel J. Anterior positional fault of the fibula after sub-acute lateral ankle sprains. Man Ther. 2008;13(1):63–67. doi: 10.1016/j.math.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 129.Landorf KB, Keenan AM. An evaluation of two foot-specific, health-related quality of life measuring instruments. Foot Ankle Int. 2002;23(6):538–546. doi: 10.1177/107110070202300611. [DOI] [PubMed] [Google Scholar]
- 130.Kaikkonen A, Kannus P, Jarvinen M. A performance test protocol and scoring scale for the evaluation of ankle injuries. Am J Sports Med. 1994;22(4):462–469. doi: 10.1177/036354659402200405. [DOI] [PubMed] [Google Scholar]
- 131.Martin R, Burdett R, Irrgang JJ. Development of the Foot and Ankle Disability Index (FADI) [abstract] J Orthop Sport Phys Ther. 1999;29:A32–33. [Google Scholar]
- 132.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 133.Carcia CR, Martin RL, Drouin JM. Validity of the Foot and Ankle Ability Measure in athletes with chronic ankle instability. J Athl Train. 2008;43(2):179–183. doi: 10.4085/1062-6050-43.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Brinkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther. 1999;79(4):371–383. [PubMed] [Google Scholar]
- 135.Alcock GK, Stratford PW. Validation of the Lower Extremity Functional scale on athletic subjects with ankle sprains. Physiother Can. 2002;54(4):233–240. [Google Scholar]
- 136.Williams GN, Molloy JM, DeBerardino TM, Arciero RA, Taylor DC. Evaluation of the Sports Ankle Rating System in young, athletic individuals with acute lateral ankle sprains. Foot Ankle Int. 2003;24(3):274–282. doi: 10.1177/107110070302400314. [DOI] [PubMed] [Google Scholar]
- 137.Karlsson J, Peterson L. Evaluation of ankle joint function: the use of a scoring scale. Foot. 1991;1(1):15–19. [Google Scholar]
- 138.Oleurd C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103(3):190–194. doi: 10.1007/BF00435553. [DOI] [PubMed] [Google Scholar]
- 139.Rose A, Lee RJ, Williams RM, Thomson LC, Forsyth A. Functional instability in non-contact ankle ligament injuries. Br J Sports Med. 2000;34:352–358. doi: 10.1136/bjsm.34.5.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Karlsson J, Eriksson BI, Sward L. Early functional treatment for acute ligament injuries of the ankle joint. Scand J Med Sci Sports. 1996;6(6):341–345. doi: 10.1111/j.1600-0838.1996.tb00104.x. [DOI] [PubMed] [Google Scholar]
- 141.Herring S, Bergfeld J, Boyd J, et al. The team physician and return-to-play issues: a consensus statement. Med Sci Sport Exerc. 2002;34(7):1212–1214. doi: 10.1097/00005768-200207000-00025. [DOI] [PubMed] [Google Scholar]
- 142.Mascaro TB, Swanson LE. Rehabilitation of the foot and ankle. Orthop Clin N Am. 1994;25(1):147–160. [PubMed] [Google Scholar]
- 143.Mattacola CG, Dwyer MK. Rehabilitation of the ankle after acute sprain or chronic instability. J Athl Train. 2002;37(4):413–429. [PMC free article] [PubMed] [Google Scholar]
- 144.Barr KP, Harrast MA. Evidence-based treatment of foot and ankle injuries in runners. Phys Med Rehabil Clin N Med. 2005;16(3):779–799. doi: 10.1016/j.pmr.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 145.Eechaute C, Vaes P, Duquet W. Functional performance deficits in patients with CAI: validity of the multiple hop tests. Clin J Sport Med. 2008;18(2):124–129. doi: 10.1097/JSM.0b013e31816148d2. [DOI] [PubMed] [Google Scholar]
- 146.Sekir U, Yildiz Y, Hazneci B, Ors F, Aydin T. Effect of isokinetic training on strength, functionality and proprioception in athletes with functional ankle instability. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):654–664. doi: 10.1007/s00167-006-0108-8. [DOI] [PubMed] [Google Scholar]
- 147.Chrintz H, Falster O, Roed J. Single-leg postural equilibrium test. Scand J Med Sci Sports. 1991;1(4):244–246. [Google Scholar]
- 148.Kaikkonen A, Hyppanen E, Kannus P, Jarvinen M. Long term functional outcome after primary repair of the lateral ligaments of the ankle. Am J Sports Med. 1997;25(2):150–155. doi: 10.1177/036354659702500202. [DOI] [PubMed] [Google Scholar]
- 149.Kinzey SJ, Armstrong CW. The reliability of the Star-Excursion Test in assessing dynamic balance. J Orthop Sports Phys Ther. 1998;27(5):356–360. doi: 10.2519/jospt.1998.27.5.356. [DOI] [PubMed] [Google Scholar]
- 150.Olmsted LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the Star Excursion Balance Test in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37(4):501–506. [PMC free article] [PubMed] [Google Scholar]
- 151.Miller SJ, Denegar CR. Intratester and intertester reliability during the Star Excursion Balance Test. J Sport Rehabil. 2000;9(2):104–116. [Google Scholar]
- 152.Docherty CL. Valovich McLeod TC, Shultz SJ. Postural control deficits in participants with functional ankle instability as measured by the Balance Error Scoring System. Clin J Sport Med. 2006;16(3):203–208. doi: 10.1097/00042752-200605000-00003. [DOI] [PubMed] [Google Scholar]
- 153.Gribble PA, Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Meas Phys Ed Exer Sci. 2003;7(2):89–100. [Google Scholar]
- 154.Hertel J, Braham RA, Hale SA, Olmsted LC. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131–137. doi: 10.2519/jospt.2006.36.3.131. [DOI] [PubMed] [Google Scholar]
- 155.Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1989;19(10):653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 156.Ryan J, Hopkinson WJ, Wheeler JH, Arciero RA, Swain JH. Office management of the acute ankle sprain. Clin Sports Med. 1989;8(3):477–495. [PubMed] [Google Scholar]
- 157.Garrick JG, Requa RK. Role of external support in the prevention of ankle sprains. Med Sci Sports. 1973;5(3):200–203. [PubMed] [Google Scholar]
- 158.Surve I, Schwellnus MP, Noakes T, Lombard C. A fivefold reduction in the incidence of recurrent ankle sprains in soccer players using Sport-Stirrup orthosis. Am J Sports Med. 1994;22(5):601–606. doi: 10.1177/036354659402200506. [DOI] [PubMed] [Google Scholar]
- 159.Sharpe SR, Knapik J, Jones B. Ankle braces effectively reduce recurrence of ankle sprains in female soccer players. J Athl Train. 1997;32(1):21–24. [PMC free article] [PubMed] [Google Scholar]
- 160.Sitler M, Ryan J, Wheeler B, et al. The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball: a randomized clinical study at West Point. Am J Sports Med. 1994;22(4):454–461. doi: 10.1177/036354659402200404. [DOI] [PubMed] [Google Scholar]
- 161.Stasinopoulos D. Comparison of three preventive methods in order to reduce the incidence of ankle inversion sprains among female volleyball players. Br J Sports Med. 2004;38(2):182–185. doi: 10.1136/bjsm.2002.003947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.McGuine TA, Brooks A, Hetzel S. The effect of lace-up ankle braces on injury rates in high school basketball players. Am J Sports Med. 2011;39(9):1840–1848. doi: 10.1177/0363546511406242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Olmsted LC, Vela LI, Denegar CR, Hertel J. Prophylactic ankle taping and bracing: a numbers-needed-to-treat and cost-benefit analysis. J Athl Train. 2004;39(1):95–100. [PMC free article] [PubMed] [Google Scholar]
- 164.Dizon JM, Reyes JJ. A systematic review on the effectiveness of external ankle supports in the prevention of inversion ankle sprains among elite and recreational players. J Sci Med Sport. 2010;13(3):309–317. doi: 10.1016/j.jsams.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 165.Glick JM, Gordon RB, Nishimoto D. The prevention and treatment of ankle injuries. Am J Sports Med. 1976;4(4):136–141. doi: 10.1177/036354657600400402. [DOI] [PubMed] [Google Scholar]
- 166.Amoroso PJ, Ryan JB, Bickley B, Leitschuh P, Taylor DC, Jones BH. Braced for impact: reducing military paratroopers' ankle sprains using outside-the-boot braces. J Trauma. 1998;45(3):575–580. doi: 10.1097/00005373-199809000-00028. [DOI] [PubMed] [Google Scholar]
- 167.Hubscher M, Zech A, Pfeifer K, Hansel F, Vogt L, Banzer W. Neuromuscular training for sports injury prevention: a systematic review. Med Sci Sports Exerc. 2010;42(3):413–421. doi: 10.1249/MSS.0b013e3181b88d37. [DOI] [PubMed] [Google Scholar]
- 168.Friel K, McLean N, Myers C, Caceres M. Ipsilateral hip abductor weakness after inversion ankle sprain. J Athl Train. 2006;41(1):74–78. [PMC free article] [PubMed] [Google Scholar]
- 169.Delahunt E, Monaghan K, Caulfield B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am J Sports Med. 2006;34(12):1970–1976. doi: 10.1177/0363546506290989. [DOI] [PubMed] [Google Scholar]
- 170.Drewes LK, McKeon PO, Kerrigan DC, Hertel J. Dorsiflexion deficit during jogging with chronic ankle instability. J Sci Med Sport. 2009;12(6):685–687. doi: 10.1016/j.jsams.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 171.Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294–298. doi: 10.1177/036354659101900315. [DOI] [PubMed] [Google Scholar]
- 172.Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14(4):232–236. doi: 10.1097/01.jsa.0000212329.32969.b8. [DOI] [PubMed] [Google Scholar]
- 173.Alonso A, Khoury L, Adams R. Clinical tests for ankle syndesmosis injury: reliability and prediction of return to function. J Orthop Sports Phys Ther. 1998;27(4):276–284. doi: 10.2519/jospt.1998.27.4.276. [DOI] [PubMed] [Google Scholar]
- 174.Norkus SA, Floyd RT. The anatomy and mechanisms of syndesmotic ankle sprains. J Athl Train. 2001;36(1):68–73. [PMC free article] [PubMed] [Google Scholar]
- 175.Uys HD, Rijke AM. Clinical association of acute lateral ankle sprain with syndesmotic involvement: a stress radiography and magnetic resonance imaging study. Am J Sports Med. 2002;30(6):816–822. doi: 10.1177/03635465020300061101. [DOI] [PubMed] [Google Scholar]
- 176.Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10(6):325–330. doi: 10.1177/107110079001000607. [DOI] [PubMed] [Google Scholar]
- 177.Taylor DC, Englehardt DL, Bassett F., 3rd Syndesmosis sprains of the ankle: the influence of heterotopic ossification. Am J Sports Med. 1992;20(2):146–150. doi: 10.1177/036354659202000209. [DOI] [PubMed] [Google Scholar]
- 178.Brown KW, Morrison WB, Schweitzer ME, Parellada JA, Nothnagel H. MRI findings associated with distal tibiofibular syndesmosis injury. AJR Am J Roentgenol. 2004;182(1):131–136. doi: 10.2214/ajr.182.1.1820131. [DOI] [PubMed] [Google Scholar]
- 179.Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin CW, Hiller CE. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc. 2010;42(11):2106–2121. doi: 10.1249/MSS.0b013e3181de7a8a. [DOI] [PubMed] [Google Scholar]
- 180.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3) doi: 10.1136/bjsm.2004.011676. e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Braun BL. Effects of ankle sprain in a general clinic population 6 to 18 months after medical evaluation. Arch Fam Med. 1999;8(2):143–148. doi: 10.1001/archfami.8.2.143. [DOI] [PubMed] [Google Scholar]
- 182.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–620. doi: 10.1177/0363546505281813. [DOI] [PubMed] [Google Scholar]
- 183.Gutierrez GM, Kaminski TW, Douex AT. Neuromuscular control and ankle instability. PM R. 2009;1(4):359–365. doi: 10.1016/j.pmrj.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 184.Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353–370. doi: 10.1016/j.csm.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 185.Hubbard TJ, Hertel J. Mechanical contributions to chronic lateral ankle instability. Sports Med. 2006;36(3):263–277. doi: 10.2165/00007256-200636030-00006. [DOI] [PubMed] [Google Scholar]
- 186.Reid A, Birmingham TB, Alcock G. Efficacy of mobilization with movement for patients with limited dorsiflexion after ankle sprain: a crossover trial. Physiother Can. 2007;59(3):166–172. [Google Scholar]
- 187.Hoch MC, McKeon PO. The effectiveness of mobilization with movement at improving dorsiflexion after ankle sprain. J Sport Rehabil. 2010;19(2):226–232. doi: 10.1123/jsr.19.2.226. [DOI] [PubMed] [Google Scholar]
- 188.McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008;40(10):1810–1819. doi: 10.1249/MSS.0b013e31817e0f92. [DOI] [PubMed] [Google Scholar]
- 189.Mohammadi F. Comparison of 3 preventive methods to reduce the recurrence of ankle inversion sprains in male soccer players. Am J Sports Med. 2007;35(6):922–926. doi: 10.1177/0363546507299259. [DOI] [PubMed] [Google Scholar]


