Abstract
Objective
To identify anatomical changes and skeletal maturity through radiographic analysis, allowing more accuracy for indication of surgical management of non-slipped hips in patients with epiphysiolisys.
Method
A retrospective study of the radiographs of 61 patients followed until the end of skeletal growth, assigned to two groups: 37 patients with unilateral epiphysiolysis, and 24 patients with contralateral epiphysiolysis diagnosed during follow-up. The skeletal maturity was evaluated using pelvis radiographs (Oxford method) and compared between the groups for patients of the same gender. In addition, the Southwick angle (in anteroposterior and in Lauenstein view), physeal sloping angle and physeal posterior sloping angle were compared as well.
Results
Skeletal maturity showed a statistically significant difference between the two groups for both genders. It was observed that the lateral view of the Southwick angle is mathematically equal to the physeal posterior sloping angle, and were the only ones to show relevant differences between the groups.
Conclusion
The Oxford method and the Southwick angle in Lauenstein view can be utilized as parameters to help the physician to better indicate the prophylactic surgical treatment of the contralateral hip, in patients with slipped capital femoral epiphysis (SCFE). Level of Evidence III, Diagnostic Study.
Keywords: Epiphyses, slipped; Hip joint/radiography; Femur head; Age determination by skeleton; Child; Adolescent; Humans; Male; Female
INTRODUCTION
Epiphysiolysis is a disease of the hypertrophic zone of the growth plate,1,2 which manifests between the ages of 10 and 16, during pubertal growth spurt.3 Bilaterality is observed in 20-40%, can reach 80% in some studies,4 and in approximately 88% the second epiphysiolysis event occurs within 12 to 18 months after the initial manifestation.5
The cause of epiphysiolysis is not yet clear, but there are risk factors strongly related to the disease, such as obesity associated with the anatomical sloping of the femoral neck and to accelerated growth during puberty.6
Southwick7 was the first to determine the angles between the axes of the femoral diaphysis and proximal epiphysis using the anteroposterior and Lauenstein radiographic views. Subsequent studies determined the Southwick angle found in normal children.6,8 The physeal angle (evaluated in relation to the ground), correlated with the risk of epiphysiolysis,9-11 is also helpful in the characterization of congenital coxa vara.12-14 In the lateral view, the posterior sloping angle may be related to the risk of bilaterality.15
The Oxford method uses radiographs of the pelvis and hip of healthy children to assess skeletal maturity, unlike the usual techniques for calculating bone age.16-18
The prophylactic treatment of the "normal" contralateral hip is controversial and should be compared with the risk of additional surgery.19,20
Thus the aim of this study is to identify radiographic differences of two groups of patients in relation to skeletal maturity (Oxford method) and the angular parameters (Southwick, physeal angle, physeal posterior sloping angle), allowing more accuracy for indication of both chronological age, and prophylactic stabilization for the contralateral hips.
MATERIALS AND METHODS
Reviews were carried out on 712 medical charts of patients with epiphysiolysis treated in the Department of Orthopedics and Traumatology of Santa Casa de São Paulo between 1982 and 1996, during which time there was no routine prophylactic fixation based on chronological age. Sixty-one patients (n=61) were selected for the study.
The inclusion criteria were unilateral epiphysiolysis without any radiographic signs of impairment of the opposite side and with follow-up until complete physeal closure. Cases with unsatisfactory follow-up and documentation were excluded.
Group 1 (37 patients) was of patients with unilateral epiphysiolysis and group 2 (24 patients) of patients with bilateral impairment (contralateral epiphysiolysis during outpatient follow-up). None of the patients had undergone prophylactic fixation.
As regards the sex, 33 of the patients were male (54.1%) and 28 female (45.9%). In group 1, 20 patients (54.1%) were male and 17 (45.9%) female. In group 2, 13 patients (54.2%) were male and 11 (45.8%) female.
Age at the time of epiphysiolysis ranged from 120 to 199 months (averaging 155.97), while in group 1 the average age was 158.86 and in group 2, 151.50 months.
The radiographic views analyzed were anteroposterior (AP) of the pelvis with internal rotation of the hips of 15º (lateral view of lesser trochanter) and Lauenstein (lateral view of the hips in "frog position"- flexion of 90º and abduction of 45º). Only the initial radiographs (at the time of the first epiphysiolysis event) were used, and the parameters were evaluated on the normal side, without any sign of slipping or pre-slipping.
The parameters of comparison between the groups were: skeletal maturity, based on the situation of the ossification centers of the pelvis and of the proximal femoral region (Oxford method);18 Southwick angle (AP and Lauenstein);6,7 and posterior sloping angle of the proximal physis of the femur (or physeal angle, in the AP view)9 and posterior sloping angle of the proximal physis of the femur (Lauenstein).15
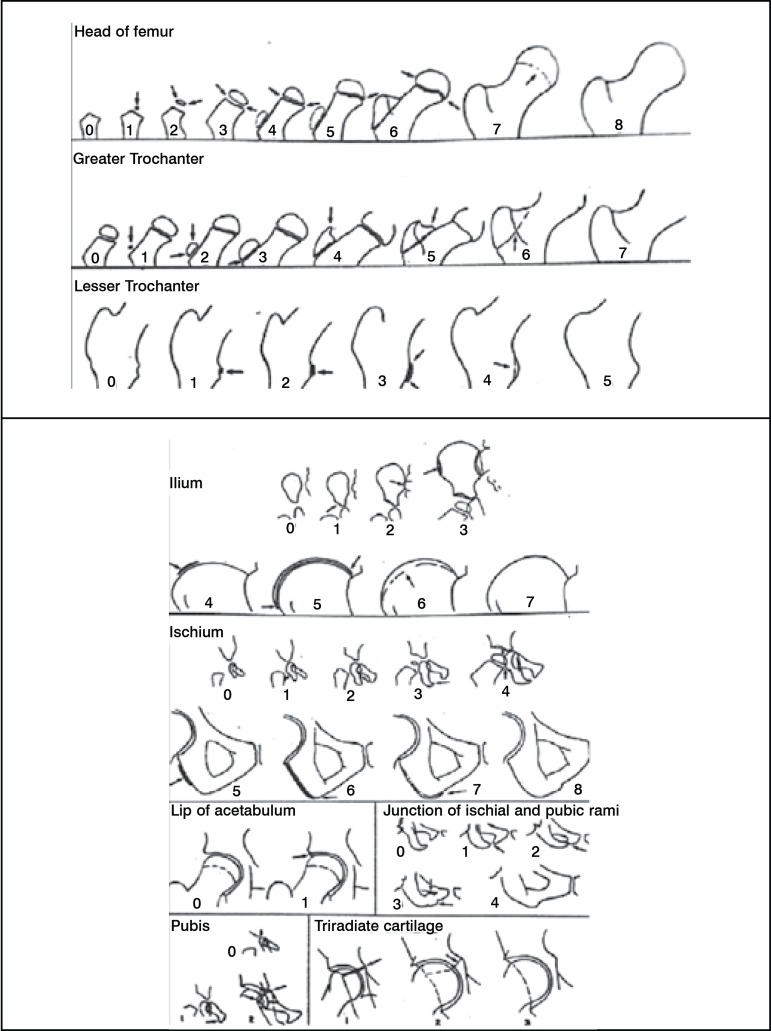
The Oxford method18 consists of a numerical score that can range from 0 (neonatal hip) to 45 (adult hip). This numerical value is found by adding up the score found in nine variables. (Figure 1) The Southwick angle is measured equally in the AP and Lauenstein views by the intersection of the straight line parallel to the long axis of the femur with the straight line that passes through the two ends of the epiphysis. In AP it is considered the greater angle and in the lateral view it is considered the lesser angle.6,7 (Figures 2A and 2B)
Figure 1.
Parameters to assess skeletal maturity (Oxford method – taken from Acheson RM. The Oxford method of assessing skeletal maturity / Clin Orthop. 1957;10:19-39)
Figure 2.
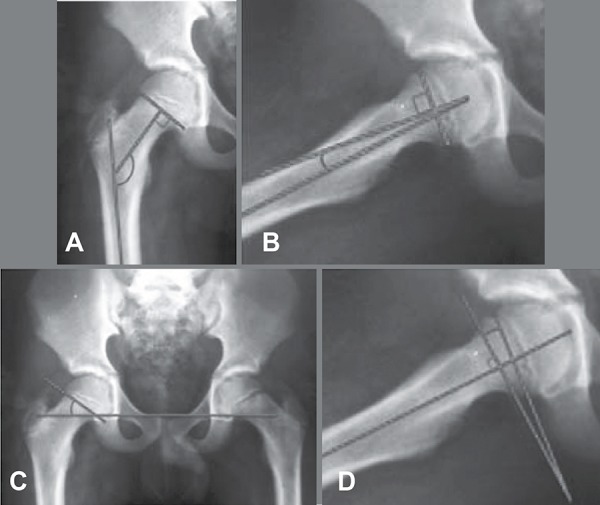
Southwick angles (A: anteroposterior; B: Lauenstein); C: sloping of the proximal femoral physis; D: posterior sloping of the physis
The sloping angle of the proximal physis is obtained in AP by the intersection of the line that crosses the "teardrop" bilaterally with another that passes through the ends of the epiphysis (as in the Southwick angle).14 (Figure 2C)
The posterior sloping angle, in the Lauenstein view, is determined by the intersection of a line perpendicular to the long axis of the diaphysis which passes through the ends of the epiphysis.20 (Figure 2D)
All the parameters described were checked by two third-year residents from the Department of Orthopedics and Traumatology, assisted by two scholars from the Faculdade de Ciências Médicas da Santa Casa de São Paulo (School of Medical Sciences), all properly trained in the application of the methods. The values obtained were sent for statistical analysis for a comparison between groups 1 and 2, applying the Student's t-test to each one of them.
RESULTS
Initially, due to the differences in the growth and maturation process between the two sexes, the Oxford method was compared among patients of the same sex. Accordingly, the groups were subdivided into male and female for the performance of the statistical analysis.
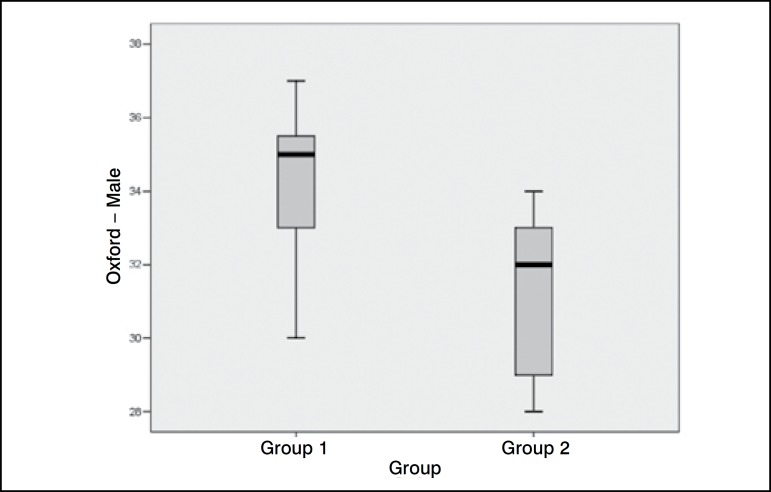
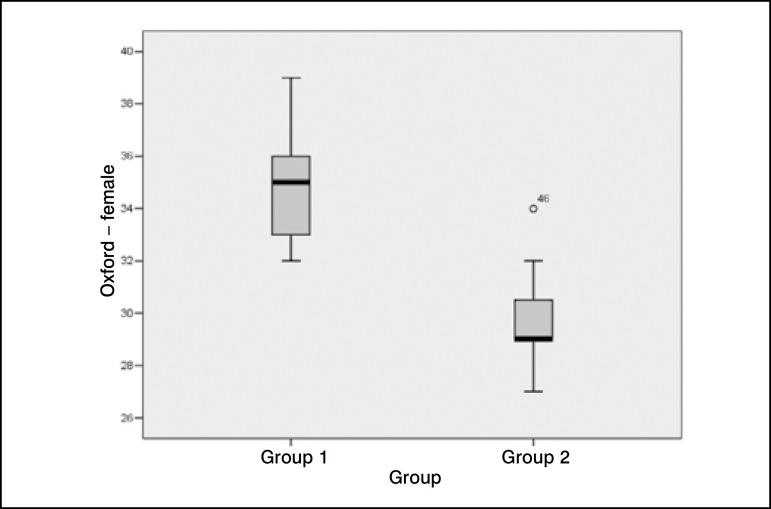
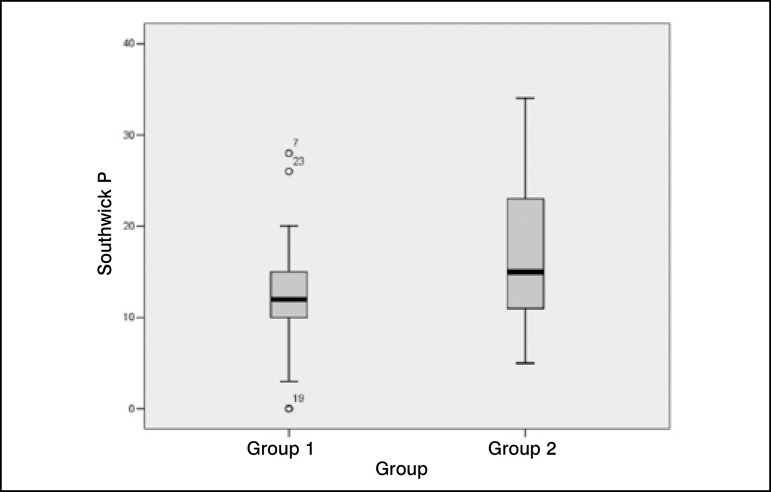
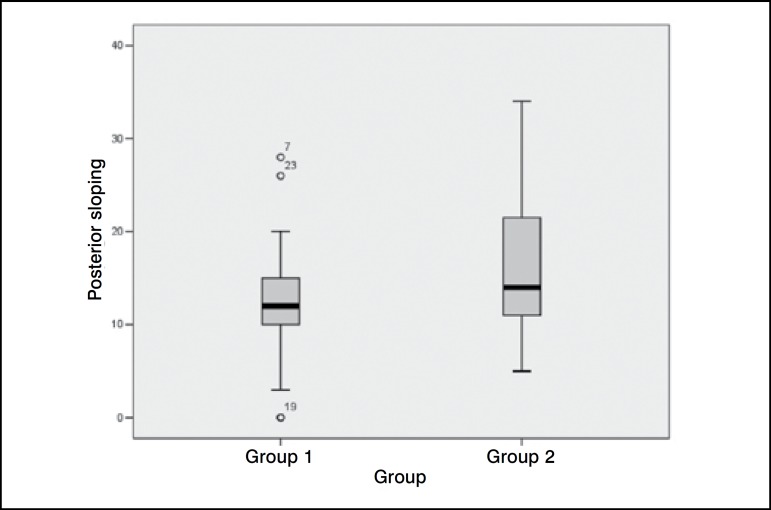
The graphs present in this study are of the boxplot type, where the gray rectangle represents 50% of the studied sample, while the other values are contained on the rest of the black line (distribution in quartiles). The small black band inside the rectangle represents the mean value. The values that fall outside standard deviation in each case are shown as isolated numbers, off the line.
Table 1 and Figures 3A and 3B show the values obtained for skeletal maturity, using the Oxford method, and their distribution. The statistical analysis demonstrated that there was a statistically significant difference (p<0.001) between groups 1 and 2, divided into male and female sex, in relation to skeletal maturity. In relation to the angles assessed, Table 2 and Figures 4A and 4B show the results obtained.
Table 1.
Comparison of skeletal maturity between groups 1 and 2, according to sex
| Oxford | Sex (number) | Mean | Standard Deviation | Confidence Interval 95% | p |
| Group 1 | Male (20) | 34.45 | 1.605 | 32.845 - 36.055 | p<0.001 |
| Female (17) | 35.24 | 2.047 | 33.193 - 37.287 | ||
| Group 2 | Male (13) | 31.00 | 2.225 | 28.775 - 33.225 | |
| Female (11) | 29.73 | 2.054 | 27.676 - 31.784 | ||
Figure 3A.
Distribution in quartiles of the skeletal maturity values, obtained by the Oxford method, male sex
Figure 3B.
Distribution of the skeletal maturity values, obtained by the Oxford method, female sex
Table 2.
Values of the measured angles (minimum - maximum, mean and CI - confidence interval of 95%), showing the p-value after statistical comparison between the two groups
| Angles (in degrees) | Group 1 | Group 2 | p | ||||
| Min - Max | Mean | CI 95% | Min - Max | Mean | CI 95% | ||
| AP Southwick | 138 - 168 | 152.11 | 149.15 - 155.07 | 132 - 168 | 150.92 | 147.74 - 154.09 | p=0.589 |
| L Southwick | 0 - 28 | 12.43 | 10.45 - 14.42 | 5 - 34 | 16.58 | 13.29 - 19.88 | p=0.032 |
| Physeal angle | 10 - 41 | 26.97 | 24.26 - 29.69 | 5 - 42 | 25.96 | 22.05 - 29.87 | p=0.654 |
| Posterior sloping | 0 - 28 | 12.43 | 10.45 - 14.42 | 5 - 34 | 16.58 | 13.29 - 19.88 | p=0.032 |
Figure 4A.
Distribution of the Southwick angle values on the side that presented significant difference after statistical analysis
Figure 4B.
Distribution of the posterior sloping values obtained, identical to that of Southwick in the lateral view
DISCUSSION
The performance of this study was based on two hypotheses: the first, that patients with epiphysiolysis, who have the disease in both hips or have a greater risk of developing it bilaterally, are skeletally immature when compared with the children in the same age bracket with the unilateral disease, and even more so when compared to the normal children.21-23 As the physis of these predisposed patients is still very immature, it would have less resistance to mechanical loads and would have to bear these loads for a longer period of time, which would invariably predispose to physeal slipping.5,21,22 The second hypothesis is that the patients have hips with slight anatomical alterations, which can increase the risk of epiphysiolysis, and these alterations can be detected by measuring angles in simple radiographs.6,9,10,15
Prophylactic surgical treatment in the contralateral femur, when the patient presents unilateral epiphysiolysis, remains a controversial subject.24 Although the procedure is relatively simple, it implies possible complications, inherent to any surgery, which may produce more harm than good.8,19 The current indication of such a procedure is based on the chronological age, yet the idea of making a decision using other parameters in conjunction appears reasonable to us given that the chronological age is not always consistent with the degree of skeletal maturity of the individual.21,23
Evaluating the results obtained in this study, we observed that there is a clear and considerable difference between the skeletal maturity of the patients from group 1 and those from group 2. The results corroborate the hypothesis that patients with bilateral epiphysiolysis have a more immature skeleton. The radiographs required for the evaluation according to the Oxford method are the same already used in the diagnosis and follow-up of patients with epiphysiolysis, which facilitates their use in the clinical practice, allowing the performance of retrospective studies like this one.
Among the angles assessed, we were surprised by the fact that the Southwick angle in the lateral view and the posterior physeal sloping are mathematically alike, even though they are assessed differently. However, this coincidence is not reported in any other study in literature. Nonetheless, these were the only angles that presented statistically significant correlation, in our study, showing that physeal sloping in the lateral view appears to be an important factor for the prediction of the occurrence of physeal epiphysiolysis of the proximal femoral region. This finding is consistent with the study conducted by Park et al.,25 who demonstrated the usefulness of the posterior sloping angle in the prediction of bilateral involvement.
We believe that the results present in this study encourage the performance of further studies, to evaluate the reliability of the methods, both intra and interobserver, and in the attempt to define cutoff values (for skeletal maturity and for the posterior sloping angle), in which prophylactic fixation of the contralateral hip is indicated or not indicated in patients with the unilateral disease.
CONCLUSION
The data and the statistical analysis present in this study allow us to conclude that the Southwick angles in the lateral view and the posterior sloping angles (mathematically equal) showed important correlation with the risk of appearance of bilateral epiphysiolysis (p<0.05).
Skeletal maturity between the groups of patients with unilateral and bilateral epiphysiolysis, estimated by the Oxford method, presented important differences, with considerable statistical reliability (p<0.001).
These radiographic parameters can be used as complementary tools in the clinical practice, as predictors of bilateral involvement, to the effect of assisting in the choice of the prophylactic, conservative or surgical treatment, for the contralateral hip of a patient with epiphysiolysis.
Footnotes
All the authors declare that there is no potential conflict of interest referring to this article.
Study conducted in the Department of Orthopedics and Traumatology of Santa Casa de São Paulo.
REFERENCES
- 1.Lacroix P, Verbrugge J. Slipping of the upper femoral epiphysis; a pathological study. J Bone Joint Surg Am. 1951;33(2):371–81. [PubMed] [Google Scholar]
- 2.Bowen JR. Development disorders of the hip. In: Scoles PV, editor. Pediatric orthopedics in clinical practice. St. Louis: Mosby; 1988. pp. 171–8. [Google Scholar]
- 3.Wilson PD. Conclusions regarding the treatment of slipping of the upper femoral epiphysis. Surg Clin North Am. 1936;16:733–52. [Google Scholar]
- 4.Gholve PA, Cameron DB, Millis MB. Slipped capital femoral epiphysis update. Curr Opin Pediatr. 2009;21(1):39–45. doi: 10.1097/MOP.0b013e328320acea. [DOI] [PubMed] [Google Scholar]
- 5.Loder RT, Aronson DD, Greenfield ML. The epidemiology of bilateral slipped capital femoral epiphysis. A study of children in Michigan. J Bone Joint Surg Am. 1993;75(8):1141–7. doi: 10.2106/00004623-199308000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Santili C., de Assis MC, Kusabara FI, Romero IL, Sartini CM, Longui CA. Southwick's head-shaft angles: normal standards and abnormal values observed in obesity and in patients with epiphysiolysis. J Pediatr Orthop B. 2004;13(4):244–7. doi: 10.1097/01.bpb.0000111042.46580.68. [DOI] [PubMed] [Google Scholar]
- 7.Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1967;49(5):807–35. [PubMed] [Google Scholar]
- 8.Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am. 1993;75(8):1134–40. doi: 10.2106/00004623-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Hughes LO, Aronson J, Smith HS. Normal radiographic values for cartilage thickness and physeal angle in the pediatric hip. J Pediatr Orthop. 1999;19(4):443–8. doi: 10.1097/00004694-199907000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Speer DP. The hip: proceedings of the Hip Society. St. Louis: Mosby; 1982. Experimental epiphysilolysis: etiologic models of slipped capital femoral epiphysis; pp. 68–88. [PubMed] [Google Scholar]
- 11.Speer DP, Abbott J. Physeal inclination angle of the proximal femur during normal development; poster exhibit at the 31st Annual Orthopaedic Research Society Meeting; Las Vegas, Nevada. January 21, 1985. [Google Scholar]
- 12.Amstutz HC, Freiberger RH. Coxa vara in children. Clin Orthop. 1962;22:73–92. [PubMed] [Google Scholar]
- 13.Babb FS, Ghormley RK, Chatterton CC. Congenital coxa vara. J Bone Joint Surg Am. 1949;31(1):115–31. [PubMed] [Google Scholar]
- 14.Weinstein JN, Kuo KN, Millar EA. Congenital coxa vara. A retrospective review. J Pediatr Orthop. 1984;4(1):70–7. doi: 10.1097/01241398-198401000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Barrios C, Blasco MA, Blasco MC, Gascó J. Posterior sloping angle of the capital femoral physis: a predictor of bilaterality in slipped capital femoral epiphysis. J Pediatr Orthop. 2005;25(4):445–9. doi: 10.1097/01.bpo.0000158811.29602.a5. [DOI] [PubMed] [Google Scholar]
- 16.Greulich WW, Pyle SI. Radigraphic atlas of skeletal development of the hand and wrist. 2nd ed. Stanford: Stanford Univ. Press; 1950. [Google Scholar]
- 17.Todd TW. Atlas of Skeletal Maturation. Part 1. The hand and wrist. St. Louis: Mosby; 1937. [Google Scholar]
- 18.Acheson RM. The Oxford method of assessing skeletal maturity. Clin Orthop. 1957;10:19–39. [PubMed] [Google Scholar]
- 19.Segal LS, Davidson RS, Robertson WW Jr, Drummond DS. Growth disturbances of the proximal femur after pinning of juvenile slipped capital femoral epiphysis. J Pediatr Orthop. 1991;11(5):631–7. [PubMed] [Google Scholar]
- 20.Fahey JJ., O'Brien ET Acute slipped capital femoral epiphysis: review of the Literature and report of ten cases. J Bone Joint Surg Am. 1965;47:1105–27. [PubMed] [Google Scholar]
- 21.Kelsey JL, Acheson RM, Keggi KJ. The body build of patients with slipped capital femoral epiphysis. Am J Dis Child. 1972;124(2):276–81. doi: 10.1001/archpedi.1972.02110140126018. [DOI] [PubMed] [Google Scholar]
- 22.Morscher E. Strength and morphology of growth cartilage under hormonal influence of puberty. Animal experiments and clinical study on the etiology of local growth disorders during puberty. Reconstr Surg Traumatol. 1968;10:3–104. [PubMed] [Google Scholar]
- 23.Sorensen KH. Slipped upper femoral epiphysis. Clinical study on aetiology. Acta Orthop Scand. 1968;39(4):499–517. doi: 10.3109/17453676808989667. [DOI] [PubMed] [Google Scholar]
- 24.Kocher MS, Bishop JA, Hresko MT, Millis MB, Kim YJ, Kasser JR. Prophylactic pinning of the contralateral hip after unilateral slipped capital femoral epiphysis. J Bone Joint Surg Am. 2004;86(12):2658–65. doi: 10.2106/00004623-200412000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Park S, Hsu JE, Rendon N, Wolfgruber H, Wells L. The utility of posterior sloping angle in predicting contralateral slipped capital femoral epiphysis. J Pediatr Orthop. 2010;30(7):683–9. doi: 10.1097/BPO.0b013e3181efb888. [DOI] [PubMed] [Google Scholar]