Abstract
Objective
Determine, through dissection in fresh cadavers, the topographic anatomy of the tibial nerve and its branches at the ankle, in relation to the tarsal tunnel.
Methods
Bilateral dissections were performed on 26 fresh cadavers and the locations of the tibial nerve bifurcation and its branches were measured in millimeters. For the calcaneal branches, the amount and their respective nerves of origin were also analyzed.
Results
The tibial nerve bifurcation occurred under the tunnel in 88% of the cases and proximally in 12%. As for the calcaneal branches, the medial presented with one (58%), two (34%) and three (8%) branches, with the most common source occurring in the tibial nerve (90%) and the lower with a single branch per leg and lateral plantar nerve as the most common origin (70%). Level of Evidence, V Expert opinion.
Keywords: Tarsal tunnel syndrome, Tibial nerve/anatomy & histology, Peripheral nerves, Cadáver, Dissection
INTRODUCTION
As an evolutionary integral part of diabetes mellitus, neuropathies appear as diverse entities. As final consequences in its physiopathology, there is the occurrence of edema and loss of neuronal elasticity, entailing alterations in the conductivity of nerve impulses and a greater propensity to compression at specific anatomic sites. The compression syndrome known as tarsal tunnel syndrome, initially described by Kopell and Thompson,1 in 1960, and independently established in 1962, by Keck2 and Lam,3 may be triggered by a metabolic disorder such as diabetes mellitus, contributing to and preceding the development of the diabetic foot syndrome.4,5 Despite efforts to decrease the number of amputations in the United States, their number grew from 54,000, in 19906 to 92,000, in 1999.7 The annual cost of diabetic neuropathy and its complications ranges between US$ 4.6 and US$ 13.7 billion in the United States.8 In spite of the shortage of global studies on diabetes, it is estimated that there will be an increase from 171 million diabetics in 2000 to 366 million in 2030.9 In our environment, the Plastic Surgery Discipline of the School of Medicine of Universidade de São Paulo (FMUSP) has concerned itself with the assessment of sensitivity in lower limbs of diabetic patients, aiming to determine quantitative evidence of alterations in pressure thresholds and associations with compression syndromes.10-11 Treatment of the tarsal tunnel with decompression surgery in diabetes patients still generates controversy between surgeons and clinical societies of neurology and diabetology. This is associated with a difference of opinion between the classical descriptions of tibial nerve anatomy and its terminal branches found in text books and anatomy atlases,12-15 vis-à-vis the findings of scientific studies of an anatomical nature, which demonstrated varied patterns of location of the tibial nerve bifurcation, while variations both in the site of origin and in the number of branches of the medial calcaneal nerve16-30 contribute to increase uncertainties in this territory.
The observation that tarsal tunnel syndrome, considered rare in the population in general, could appear in an increasingly large population, undoubtedly augments the number of candidates to interventions in an area with anatomy subjects to variations.
OBJECTIVE
Determine, through dissection in fresh cadavers, the topographic anatomy of the tibial nerve and its branches at the ankle, in relation to the tarsal tunnel.
MATERIAL AND METHOD
The study was conducted through bilateral anatomical dissection of 26 fresh cadavers, originating from the Coroner's Service (SVO, Serviço de Verificação de Óbitos) of the capital city - USP and from the Instituto de Medicina Legal Nina Rodrigues (IML-BA - Institute of Forensic Medicine).
The selection of the sample number was based on the time required for dissection of each leg and the difficulty in accessing this anatomic site of the human body for dissections in fresh cadavers (restricted to unclaimed bodies of destitute individuals). The criterion of exclusion selected in the study was direct blunt trauma to the leg precluding the performance of dissection.
In each procedure the feet remained in neutral position and the surgical exploration was initiated 15 centimeters proximal to the center of the medial malleolus, continuing distally up to the insertion of the plantar nerves on the plantar surface of the foot. A longitudinal incision covered this entire distance and two transversal incisions, one at each end of the longitudinal incision, completed the approach, facilitating the elevation of two skin flaps, with ample exposure of the region.
After cutaneous flap elevation and in view of the difficulty in distinguishing between these structures, the superficial and deep fasciae were incised and elevated together with the flexor retinaculum and superficial fascia of the abductor hallucis muscle, exposing all the structures that form the medial distal third of the leg and ankle (posterior tibial tendons and long finger flexor tendon, posterior tibial neurovascular bundle and flexor hallucis longus tendon).
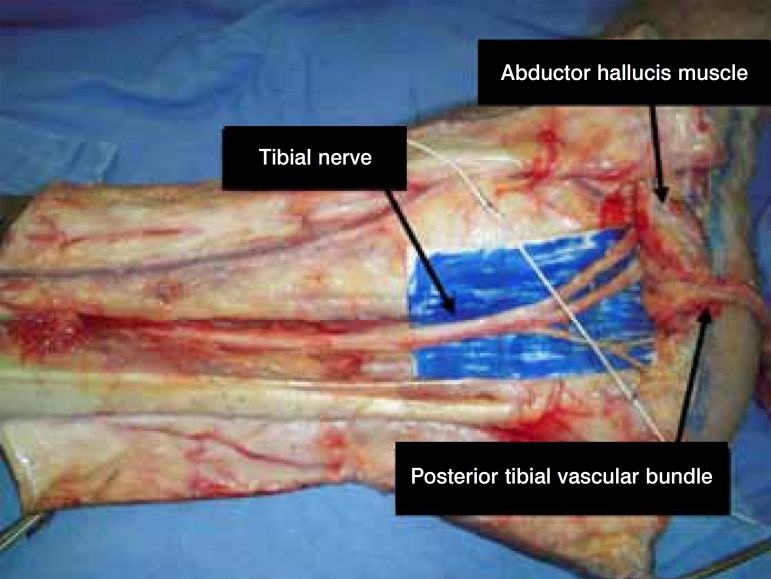
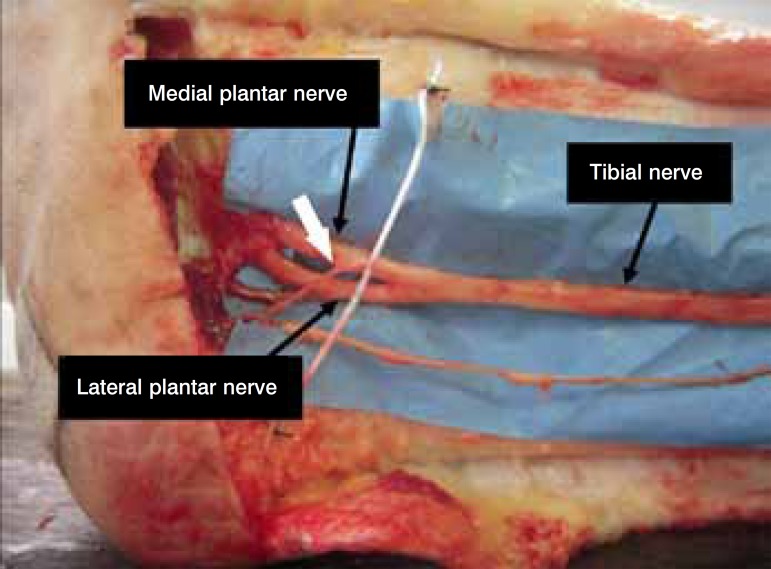
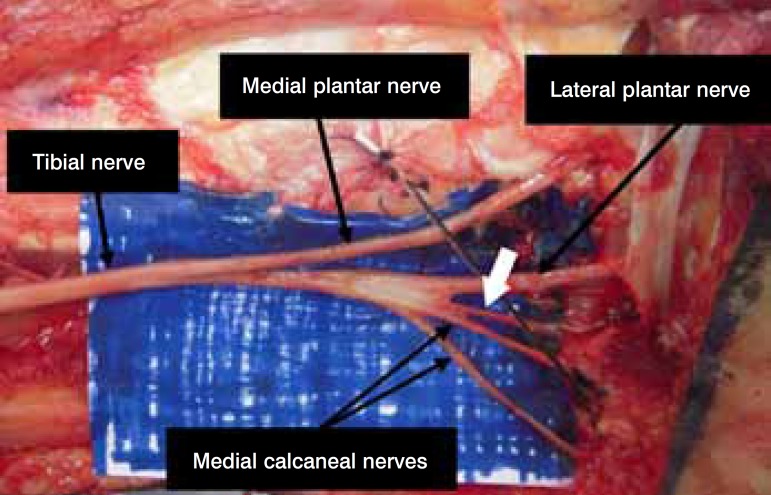
The neurovascular bundle, which is wrapped in its own sheath, was then incised and the vascular structures separated from the tibial nerve, thus exposing a significant part of the path of this nerve in front of, inside and behind the tarsal tunnel. To facilitate the visualization of the terminal branches, the abductor hallucis muscle was resected from its origin in the calcaneus, maintaining its deep fascia. (Figure 1) The procedures were executed under surgical magnification, using a 3.5x magnifying glass and appropriate dissection material.
Figure 1.
Elevated cutaneous and fascial flaps; dissection of the vascular bundle (reflected distally) and deinsertion of the abductor hallucis muscle.
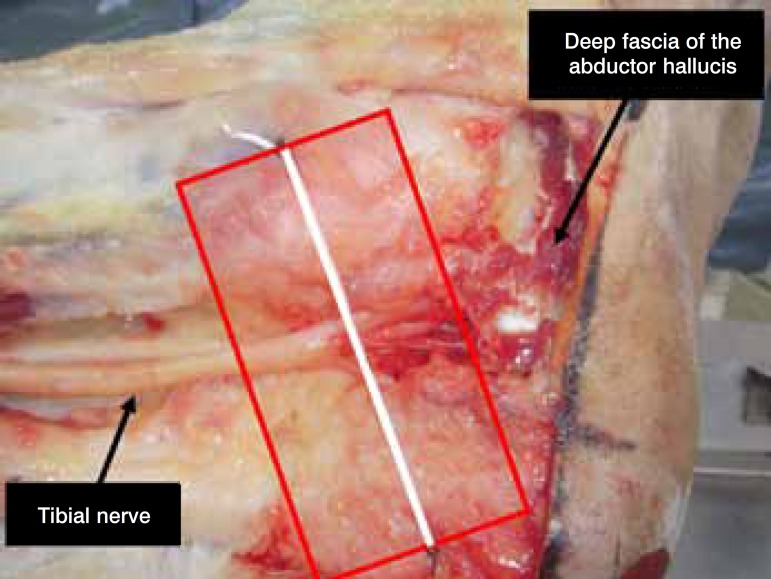
After this initial stage, a reference line (malleolar-calcaneal axis - MCA) was fixed between the center of the medial malleolus and the medial calcaneal tuberosity, according to the descriptions of Dellon and Mackinnon.17 A size zero cotton thread fastened to the periosteum of the respective anatomical parameters with a simple stitch in 3-0 mononylon was used for this purpose.
Due to the lack of anatomical clarity in distinguishing the end of the deep fascia, the start of the retinacular ligament, its end and the start of the abductor hallucis fascia, the tarsal tunnel was defined by extending two centimeters proximal and distal to this axis.18 (Figure 2)
Figure 2.
Malleolar-calcaneal axis (MCA) and limits of the retinaculum.
As regards the MCA, a digital caliper properly calibrated in millimeters was used to measure the distances of the anatomical parameters in question, where each measurement was made four times and their means were computed as the final value. The following were determined: 1 - Location of the tibial nerve bifurcation into the plantar nerves; 2 - Locations of the medial calcaneal branch(es); 3 - Origin of the medial calcaneal branch(es); 4 - Quantity of medial calcaneal branches; 5 -Location of the lower calcaneal branch(es); 6 - Origin of the lower calcaneal branch; 7 - Quantity of lower calcaneal branches.
A new classification was prepared for the tibial nerve bifurcation, in relation to the MCA, with five subtypes based on the initial proposal of Bilge,26 adapted and expanded: type I represents that the bifurcation is proximal to the axis, but inside the tarsal tunnel; type II represents that the bifurcation occurs at the axis; type III represents that the bifurcation is distal to the axis, but inside the tarsal tunnel; type IV represents that the bifurcation is proximal to the axis, yet outside the tarsal tunnel, while type V represents that the bifurcation is distal to the axis and outside the tunnel.
The medial calcaneal branches were grouped according to the patterns found, seeking to establish the most frequent pattern. They were also analyzed with regards to the number of branches and nerve of origin, as well as the level at which the ramification was established, in relation to the MCA. The same procedure was applied to the lower calcaneal branch.
The results were transformed into rates (percentage), tabulated and compared to the data available in published studies from the literature.
All the dissections had their scientific photographic documentation produced using a digital camera, and the most pertinent findings are shown here.
RESULTS
Twenty-six cadavers were submitted to the dissections, totaling 50 legs. Two met the exclusion criterion.
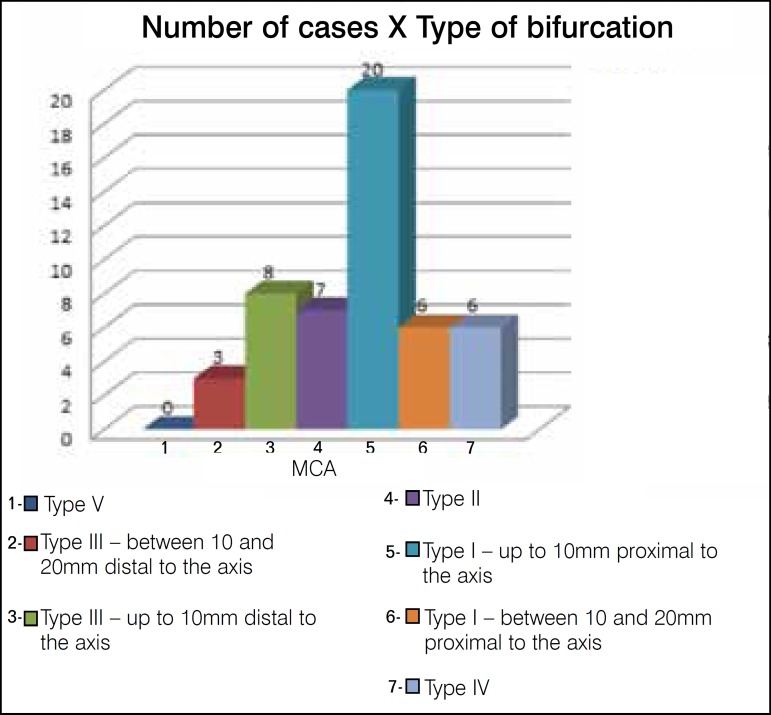
Tibial nerve bifurcation into the plantar nerves
The tibial nerve bifurcation into medial and lateral plantar nerves occurred inside the retinaculum in 44 studied limbs (88%). In six pieces the division occurred proximal to the flexor retinaculum (12%). Applying the classification by types, we obtained type I in 26 cases (52%), type II in seven (14%), type III in 11 (22%), type IV in six (12%) and type V was not visualized. (Figures 3 and 4) The tibial nerve bifurcations, inside the tarsal tunnel, occurred, on average, at 7.23mm (1.81mm to 14.86mm), when identified in topography proximal to the MCA, and at 7.72mm (2.13mm to 19.23mm), when in distal topography, with 70% of these occurring within an area corresponding to 10 mm proximal and distal to the axis. The six divisions proximal to the tarsal tunnel occurred at 22.31mm, 24.71mm, 27mm, 46mm and 53mm and 53.30mm (mean of 37.72mm).
Figure 3.
Location of the tibial nerve bifurcations in relation to the MCA.
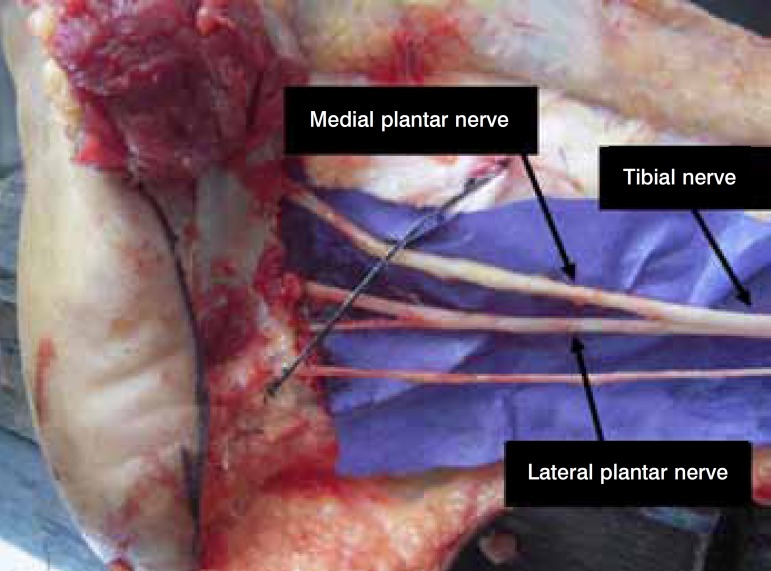
Figure 4.
Example of type IV bifurcation.
The plantar nerves always penetrated their own osteofibrous tunnels, having the deep fascia of the abductor hallucis muscle as a roof and separated by a fibrous septum connecting the roof to the bone floor.
Medial calcaneal branch
The medial calcaneal branches were visualized in presentations that ranged from one to three ramifications. The division of the medial calcaneal nerve according to the number of branches and percentages is presented in Table 1 and the division in terms of nerves of origin in Table 2 and Figures 5 and 6. In Table 3 we can visualize the distribution of the medial calcaneal branches according to the nerve of origin and quantity of branches.
Table 1.
Division of the medial calcaneal nerve, according to the number of branches.
| Number of branches | No. of cases | % |
| One | 29 | 58% |
| Two | 17 | 34% |
| Three | 04 | 8% |
| Total | 50 | 100% |
Table 2.
Division of the medial calcaneal branches, according to nerve of origin.
| Origin | No. of cases | % |
| Tibial | 45 | 90% |
| Lateral plantar | 01 | 2% |
| Tibial and lateral plantar | 02 | 4% |
| Tibial and medial plantar | 02 | 4% |
| Total | 50 | 100% |
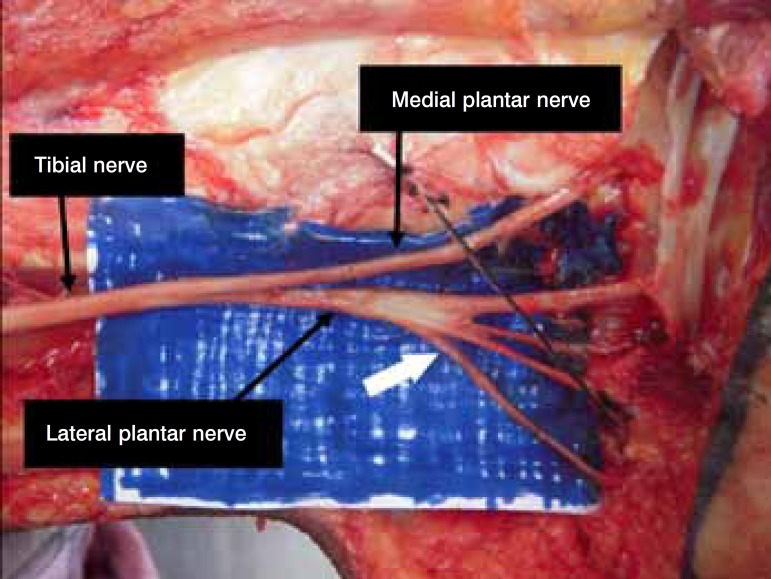
Figure 5.
Medial calcaneal branch – origin of the medial plantar nerve.
Figure 6.
Medial calcaneal branch – origin of the lateral plantar nerve.
Table 3.
Medial calcaneal branches, according to nerve of origin and quantity of branches.
| Origin of the branch | One | Two | Three | Total | ||||
| No. | % | No. | % | No. | % | No. | % | |
| Tibial | 29 | 100% | 14 | 82.3 % | 02 | 50% | 45 | 90% |
| Lateral plantar | - | - | 01 | 5.9 % | - | - | 01 | 2% |
| Tibial and lateral plantar | - | - | 01 | 5.9 % | 01 | 25% | 02 | 4% |
| Tibial and medial plantar | - | - | 01 | 5.9 % | 01 | 25% | 02 | 4% |
| Total | 29 | 100% | 17 | 10% | 04 | 100% | 50 | 100% |
These ramifications occurred under the flexor retinaculum in 27 pieces (54%). In 23 (46%) only the tibial nerve emitted such branches inside the tunnel; in two (4%), the tibial and lateral plantar nerves emitted such branches; and in two pieces (4%) the ramifications originated from the tibial and medial plantar nerves. The minimum distance of the calcaneal branches, in relation to the MCA, was 2.37mm proximal and 4.67mm distal. The maximum was 19.40mm and 10.87mm, respectively.
In 31 pieces (62%) we observed the emission of calcaneal branches proximal to the retinaculum; in 30 pieces (60%) only the tibial nerve originated such branches; and in one piece (2%) we identified calcaneal branches as originating from the lateral plantar nerve. The patterns found are set out in Table 4.
Table 4.
Patterns of presentation of the medial calcaneal branches.
| Patterns | nª | % |
| 1- Single branch of the TN proximal to the tunnel | 16 | 32% |
| 2- 02 branches of the TN proximal to the tunnel | 06 | 12% |
| 3- 02 branches of the TN 01 in the tunnel and 01 proximal | 04 | 8% |
| 4- 2 branches of the TN in the tunnel | 04 | 8% |
| 5- 01 branch of the TN proximal to the tunnel and 01 branch of the LPN in the tunnel | 01 | 2% |
| 6- 02 branches of the LPN proximal to the tunnel | 01 | 2% |
| 7- 01 branch of the TN proximal and 01 branch of the MPN inside the tunnel | 01 | 2% |
| 8- single branch of the TN in the tunnel | 13 | 26% |
| 9- 02 branches of the TN in the tunnel and 01 branch of the LPN in the tunnel | 01 | 2% |
| 10- 03 branches of the TN in the tunnel | 01 | 2% |
| 11- 02 branches of the TN proximal to the tunnel and 01 branch of the MPN in the tunnel | 01 | 2% |
| 12 - 03 branches of the TN: 02 proximal and 01 inside the tunnel | 01 | 2% |
| Total | 50 | 100% |
TN = tibial nerve; LPN = lateral plantar nerve; MPN = medial plantar nerve
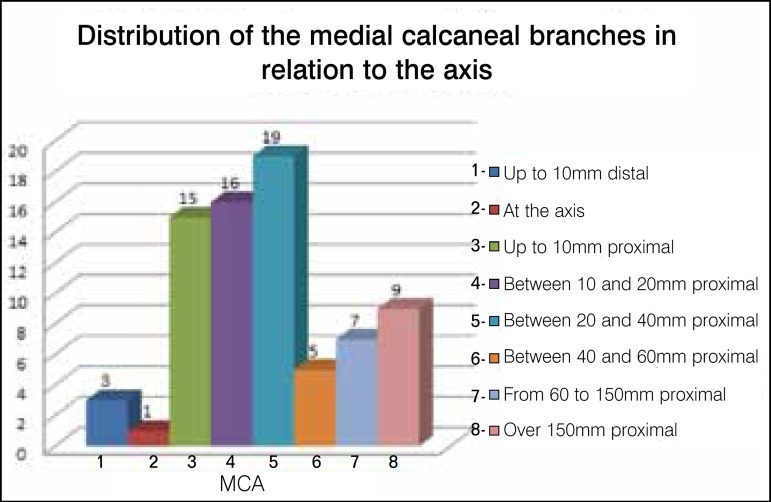
Nine proximal branches presented their origins at distances above the 15cm of exposure proposed, requiring expansion of the approach. The smallest was located 176 mm and the largest 346.60mm from the axis, averaging 241.10mm. (Figure 7) A total of 75 medial calcaneal branches were found, with their distributions in relation to the MCA presented in Figure 8.
Figure 7.

Medial calcaneal branch – origin 346.60mm proximal to the MCA.
Figure 8.
Medial calcaneal branches: distances in relation to the MCA.
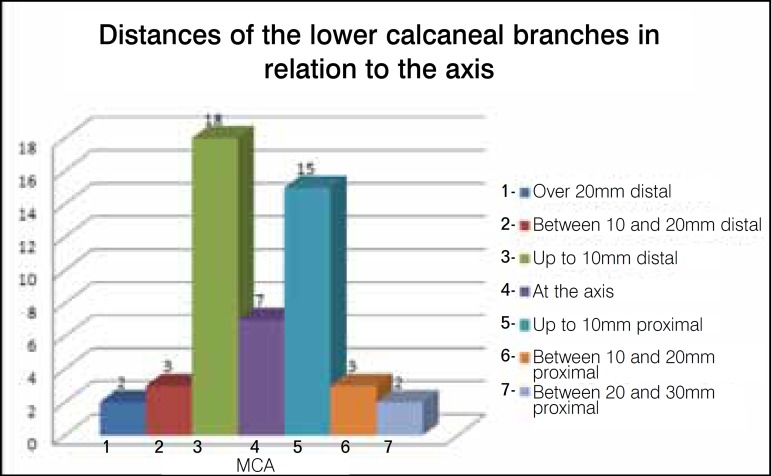
Lower calcaneal branch
In relation to the lower calcaneal branch, its constancy was 100%, with 92% of the ramifications occurring inside the flexor retinaculum, 4% proximal and 4% distal to this point. These ramifications were always positioned distal to the medial calcaneal ramifications and with only one branch per leg. The respective distances of the ramifications, in relation to the MCA, are itemized in Figure 9.
Figure 9.
Distances of the emissions of the lower calcaneal branches in relation to the MCA.
The division according to site of origin of the ramifications can be seen in Table 5 and is exemplified in Figure 10. In the 35 legs with origin of the lateral plantar nerve, the lower calcaneus appeared as the only ramification of this nerve.
Table 5.
Division of the lower calcaneal branches, according to site of origin.
| Origin | No. of cases | % |
| Total | 50 | 100% |
| Tibial | 09 | 18% |
| Lateral plantar | 35 | 70% |
| Bifurcation | 04 | 8% |
| Common trunk with the lateral plantar and medial calcaneal | 02 | 4% |
Figure 10.
Lower calcaneal branch – example of origin of the common trunk with the lateral plantar and the medial calcaneal.
DISCUSSION
Anatomical studies of the tibial nerve in the distal third of the leg and at the level of the tarsal tunnel began to take more importance with the establishment and definition of a compression pathology of this nerve, in its osteofibrous tunnel, by Lam3 and Keck,2 introducing the term tarsal tunnel syndrome. In an analogy with the upper limb, this syndrome resembles carpal tunnel syndrome, also sharing decompression surgery as one of the therapeutic approaches.
In association with this, the discovery that metabolic disorders caused by systemic diseases, including diabetes mellitus, favor the appearance of this syndrome in association with preexisting neuropathies, increased the number of patients candidates to the surgical releases of the flexor retinaculum and osteofibrous tunnels of the tarsus, giving rise to controversy among diabetologists, neurologists and surgeons.
The comparison with other anatomical studies that used the same parameters to measure the data investigated helps to increase and to enrich knowledge, expanding the horizons of those that perform or are about to perform surgical procedures at the level of the medial surface of the ankle.
In concordance with the other published articles, an important variation of the terminal branches of the tibia was observed here, both in the level of their bifurcation and in the number and origins of the medial and lower calcaneal branches, with some differences in their prevalence.
As concerns the topic of bifurcation into the plantar branches, we found 88% of these occurring under the flexor retinaculum (two centimeters proximal and distal to the MCA). The comparison with other articles can be seen in Table 6.
Table 6.
Location of the bifurcation of the tibial nerve in relation to the tarsal tunnel.
| Authors | No. of cases | Bifurcation inside the tunnel | Proximal bifurcation | Distal bifurcation |
| Horwitz (1938) | 100 | 96% | 4% | |
| Dellon (1984) | 31 | 94% | 6% | |
| Davis (1995) | 20 | 90% | 10% | |
| Louisia (1999) | 15 | 73% | 26% | |
| Heimkes (1987) | 60 | 100% | - | |
| Havel (1988) | 68 | 93% | 7% | |
| Ndiaye (2003) | 20 | 90% | 10% | |
| Bilge (2003) | 50 | 96% | - | 4% |
| Joshi (2006) | 112 | 99.9% | - | 0.89% |
| Fernandes (2006) | 30 | 86.7% | 10% | 3.3% |
| Present study (2011) | 50 | 88% | 12% | |
We also observed, in consensus with most authors, that the bifurcation occurring inside the tunnel presents a higher proportion of presentations in an area corresponding to 10mm distal and proximal to the MCA. This discovery is present in 70% of the legs dissected here.
In an attempt to standardize a comparison based on the classification by types proposed here, we applied it in the studies that presented sufficient data on the respective measurements that made it possible to achieve this purpose. The result of the comparison can be viewed in Table 7.
Table 7.
Comparison of findings referring to bifurcation after classification by types.
| Authors | Type I | Type II | Type III | Type IV | Type V |
| Dellon (1984) | 22.58% | 54.84% | 16.13% | 6.45% | - |
| Heimkes (1987) | 100% | - | - | - | - |
| Havel (1988) | 45.59% | 38.24% | 8.82% | 7.35% | - |
| Louisia (1999) | 37.7% | 28.6% | 7.1% | 28.6% | - |
| Ndiaye (2003) | - | 90% | 10% | - | |
| Bilge (2003) | 84% | 12% | - | 4% | |
| Joshi (2006) | 85.2% | 14.7% | 0.89% | - | - |
| Fernandes(2006) | 23.34% | 33.33% | 30% | 10% | 3.33% |
| Present study (2011) | 52% | 14% | 22% | 12% | - |
The six pieces classified as type IV occurred at distances that ranged from 22.31mm to 53.30mm in relation to the MCA. Horwitz16 described it in four pieces, with distances ranging from 75 to 100mm. Dellon et al.17 found it in two legs, of the same cadaver, with one 30mm and the other 50mm from the MCA. Havel et al.19 observed five occurrences, all 40mm from the axis. Davis et al.21 described two occurrences, one at a distance of 50mm and another of 90 mm. Louisia et al.22 reported four occurrences, one at 25mm, another at 30mm and two at 35mm. Ndiaye et al.24 described it on two occasions, in the same cadaver, both at a distance of 50mm. Fernandes et al.30 described the type in three of the pieces, with two at a distance of 30mm and the other at 57mm. Bilge et al.25 and Joshi et al.26 did not report type IV bifurcations.
The importance of this fact, also observed by other authors, appears to be related to a greater propensity to the development of tarsal tunnel syndrome in these cases, due to the presence of a larger cross-sectional area represented by the nerve already bifurcated in a narrow, rigid osteofibrous structure.17 Going by what appears to be a consensus in literature, this presentation is rare and in keeping with the rarity of this syndrome in the general population.
In relation to the topics involving the medial calcaneal branch, we found varied presentations in full consensus with the literature.
As regards the quantity of branches, we established the presence of one to three, where the most common presentation was that of a single branch in 58% of the legs. (Table 1) Horwitz16 only reported the existence of one or more branches, not specifying numbers. Dellon et al.17 found one or two branches, while the former was the most common (75%). Davis et al.21 observed from one to three branches, with two to three occurring most often (60%). Havel et al.19 and Ndiaye et al.24 reported the presence of one or two branches, with greater frequency of the former in 79% and 80% of the cases, respectively. Joshi et al.26 and Moraes Filho et al.28 found from one to four, with the same percentage for one and two branches (41.96% each), in the former, and one branch standing out, in the second study (55.26%). Fernandes et al.30 found from one to five ramifications, with the emission of two branches appearing most frequently (46.66%).
In specific research work on the anatomical variations of this branch, Louisia et al.22, Dellon et al.23, Govsa et al.27 and Moraes Filho et al.29 demonstrated the presence of one to four branches. The existence of two was observed the most often by the first, second and third (60%, 41% and 46%, respectively), with a single branch (55%) as more common in the fourth study.
As for the origin of ramifications, we verified the greater frequency of their emission from the tibial nerve, in conformity with all the authors, except for Horwitz16 (96% of origin from the lateral plantar nerve). Davis et al.21 challenged this data, believing that the author might have confused it with the lower calcaneal branch, which can effectively happen, in our opinion, if the abductor hallucis muscle is not dissected to allow a better view of the pathway of these branches. An overview of the anatomical variations of medial calcaneal branches observed in the literature can be seen in Table 8.
Table 8.
Anatomical variations of the medial calcaneal branch found in the literature.
| Authors | No. of branches | Most frequent presentation | Most frequent nerve of origin | Most frequent locations of the ramifications |
| Horwitz (1838) | 01 or more branches | NA | Plantar lateral | Inside the tunnel |
| Dellon (1984) | 01 or 02 branches | 01 branch | Tibial | Proximal to the tunnel |
| Didia (1990) | 01 to 04 branches | 02 branches | Tibial | Inside the tunnel |
| Davis (1995) | 01 to 03 branches | 02/03 branches | Tibial | Proximal to the tunnel |
| Havel (1988) | 01 or 02 branches | 01 branch | Tibial | Inside the tunnel |
| Louisia (1999) | 01 or 02 branches | 02 branches | Tibial | Inside the tunnel |
| Moraes Filho (2000) | 01 to 04 branches | 01 branch | Tibial | Proximal to the tunnel |
| Dellon (2002) | 01 to 04 branches | 02 branches | Tibial | Inside the tunnel |
| Ndiaye (2003) | 01 or 02 branches | 01 branch | Tibial | Inside the tunnel |
| Joshi (2006) | 01 to 04 branches | 01/02 branches | Tibial | Inside the tunnel |
| Fernandes (2000) | 01 to 05 branches | 02 branches | Tibial | Inside the tunnel |
| Govsa (2006) | 01 to 04 branches | 02 branches | Tibial | Inside the tunnel |
| Moraes Filho (2007) | 01 to 04 branches | 01 branch | Tibial | Proximal to the tunnel |
| Present study (2011) | 01 to 03 branches | 01 branch | Tibial | Proximal to the tunnel |
Note: Tarsal tunnel defined as 2cm proximal and distal to the MCA
What was observed in most of the studies presented here, including the present one, was the origin of these branches occurring, preferentially, from the tibial nerve trunk, followed by a mixed presentation (tibial and lateral plantar), and finally, by the lateral plantar branch. The presentation of one ramification originating from the medial plantar nerve was described only by Davis et al.21 (15%), Dellon et al.23 (46%), Havel et al.19 (5.9%), Govsa et al.27 (32%) and Moraes Filho et al.29 (1.22%). In our study this finding was present in conjunction with another ramification of different origin, in two cases (4%).
Another fact observed is related to the ramifications with locations proximal to the tarsal tunnel. We verified this finding in 31 pieces (62%); in 30 they originated only from the tibial nerve and in one, from the lateral plantar nerve. The comparison with the findings of other studies can be found in Table 9.
Table 9.
Proximal locations of the medial calcaneal branches in the literature.
| Authors | % cases with ramifications proximal to the tarsal tunnel |
| Dellon (1984) | 65% |
| Havel (1988) | 45,5% |
| Davis (1995) | 70% |
| Louisia (1999) | 60% |
| Dellon (2002) | 21% |
| Govsa (2006) | 26% |
| Fernandes (2006) | 60% |
| Moraes Filho (2007) | 55% |
| Present study (2011) | 62% |
Of a total of 75 medial calcaneal branches, 40 originated from outside the tunnel proximally (53.3%). The mean distance of these branches, in relation to the MCA, was 91.8mm (21.03 to 346.60mm), whereas distances of more than the 150mm of incision advocated for the approach were observed in nine pieces, a fact reported only by Fernandes et al.29 in two occurrences (170 and 367mm).
These findings can have important repercussions in the presentation of the symptomatology of patients with tarsal tunnel syndrome, since branches with proximal origins can present pathways on a plane superficial to the flexor retinaculum. Therefore, if they do not penetrate the tunnel they present lower propensity to compression, maintaining the sensitivity of their innervation territory. This presentation would justify some discrepancies between the clinic and electrical conductivity tests.
Also called first nerve of the lateral plantar branch, nerve to abductor muscle of the little finger, deep calcaneal branch, motor branch of lateral plantar nerve or Baxter's nerve, the lower calcaneal branch is described as a motor ramification for innervation of the intrinsic abductor muscle of the little finger, passing profoundly between the deep fascia of the abductor hallucis muscle, medially, and the medial plantar border, laterally.
Its importance as a cause of pain and discomfort secondary to compression were already suspected and investigated in the 40s, and in 1960, Kopell and Thompson1 put forward that most cases of pain in the heel were caused by compression of this nerve.
In 1986, Rondhuis and Huson31 demonstrated, with strong evidence, that this branch was not purely motor, but rather, mixed, with a sensory component to innervate the periosteum of the medial portion of the calcaneus. The constancy of this sensory ramification to the periosteum was proven both by Davis et al.21 and Louisia et al.22 and by Govsa et al.27
In our study, it was present in 100% of the cases, with only one branch per leg, with 92% of the ramifications occurring under the flexor retinaculum, 4% proximal to it and 4% distal. Louisia et al.22 observed 93.3% occurring under the retinaculum and 6.7% distal to the tunnel. Govsa et al.27 and Davis et al.21 did not describe the locations in relation to the MCA, precluding comparisons, but the former reports that the average distance of the origin of the branches was 17.4mm distal to the axis. Using this parameter, we obtained a mean of 9.33mm proximal and 8.7mm distal to the axis. The consensus is, effectively, of only one single branch per leg.
As regards source, we found 18% from the tibial nerve, 8% from the bifurcation, 70% from the lateral plantar nerve and 4% from the common trunk with the lateral plantar and medial calcaneal nerve. Didia et al.20 observed 81.25% from the lateral plantar nerve, 12.5% from the tibial nerve and 6,25% from the common trunk with the tibial and the medial calcaneal nerve. Davis et al.21 encountered 100% of the ramifications originating from the lateral plantar nerve. Louisia et al.22 reported 93.3% from the lateral plantar nerve and 6.7% from the common trunk with the lateral plantar and medial calcaneal nerve.
In consensus with these authors, we observe the vast majority of ramifications originating from the lateral plantar nerve, yet Govsa and cols.27 observe 82% from the tibial nerve, 10% from the bifurcation, 4% from the common trunk with the lateral plantar and medial calcaneal nerves and only 4% from the lateral plantar nerve. This once again shows the degree of variation that can be found in this anatomy in different population samples.
Although this nerve branch is not directly involved in the dermal sensitivity of the calcaneal region, the fact that its compression generates and is the cause of important pain at the point of contact of the plantar region with the ground during walking leads to alterations in the way patients position their feet when walking (antalgic positioning).
This fact brings about an increase in pressure at other plantar sites which may already be subject to a certain degree of sensitivity impairment, incrementing harmful forces for the development of precursor lesions of diabetic foot syndrome.
CONCLUSIONS
1- The bifurcation of the tibial nerve into the medial and lateral plantar branches occurred under the flexor retinaculum in 88% of the legs, located, in 70% of the cases, in an area between 10mm proximal and distal to the MCA.
2 - The medial calcaneal branch presented considerable variation both in its origin and number of branches and in its location in relation to the tarsal tunnel. The presentation of one branch with origin from the tibial nerve, in the tunnel or proximal to the tunnel, was observed the most frequently (58%).
3 - The lower calcaneal branch was always present and with a certain degree of variation in relation to its origin. The presentation of single branch originating from the lateral plantar nerve was the most constant (70%).
Footnotes
All the authors declare that there is no potential conflict of interest referring to this article.
Study conducted in the Plastic Surgery Discipline of Hospital das Clínicas of the School of Medicine of Universidade de São Paulo (FMUSP), São Paulo - SP, Brazil.
REFERENCES
- 1.Kopell HP, Thompson WA. [Peripheral entrapment neuropathies of the lower extremity.] N Engl J Med. 1960;262:56–60. doi: 10.1056/NEJM196001142620202. [DOI] [PubMed] [Google Scholar]
- 2.Keck C. The Tarsal-Tunnel syndrome. Bone Joint Surgery. 1962;44:180–2. [Google Scholar]
- 3.Lam SJ. A tarsal-tunnel syndrome. Lancet. 1962;2(7270):1354–5. doi: 10.1016/s0140-6736(62)91024-3. [DOI] [PubMed] [Google Scholar]
- 4.Upton AR, McComas AJ. The double crush in nerve entrapment syndromes. Lancet. 1973;2(7825):359–62. doi: 10.1016/s0140-6736(73)93196-6. [DOI] [PubMed] [Google Scholar]
- 5.Dellon AL, Mackinnon SE. Chronic nerve compression model for the double crush hypothesis. Ann Plast Surg. 1991;26(3):259–64. doi: 10.1097/00000637-199103000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Geiss LS, Herman WH, Goldschmid MG, DeStefano F, Eberhardt MS, Ford ES, et al. Surveillance for diabetes mellitus--United States, 1980-1989. MMWR CDC Surveill Summ. 1993;42(2):1–20. [PubMed] [Google Scholar]
- 7.Bloomgarden ZT. American Diabetes Association 60th Scientific Sessions, 2000: the diabetic foot. Diabetes Care. 2001;24(5):946–51. doi: 10.2337/diacare.24.5.946. [DOI] [PubMed] [Google Scholar]
- 8.Gordois A, Scuffham P, Shearer A, Oglesby A, Tobian JA. The health care costs of diabetic peripheral neuropathy in the US. Diabetes Care. 2003;26(6):1790–5. doi: 10.2337/diacare.26.6.1790. [DOI] [PubMed] [Google Scholar]
- 9.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 10.Carvalho VF, Ferreira MC, Vieira SAT, Ueda T. Limiar de sensibilidade cutânea dos pés em pacientes diabéticos através do pressure specified sensory device: uma avaliação da neuropatia. Rev Assoc Med Bras. 2009;55(1):29–34. doi: 10.1590/s0104-42302009000100011. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira MC, Vieira SAT, Carvalho VF. Estudo comparativo da sensibilidade nos pés de diabéticos com e sem úlceras utilizando o PSSD. Acta Ortop. Bras. 2010;18(2):71–4. [Google Scholar]
- 12.Gray's anatomy: The anatomical basis of clinical practice. 40th ed. Elsevier Inc; 2008. [Google Scholar]
- 13.Moore KL, Dalley AF. Anatomia orientada para a clínica. 4a ed. Editora Guanabara Koogan; 2001. [Google Scholar]
- 14.Sobotta: Atlas de anatomia humana. 21a ed. Vol. 2. Editora Guanabara Koogan; 2000. [Google Scholar]
- 15.Netter: Concise atlas of orthopaedic anatomy. Philadelphia: Elsevier Inc; 2002. [Google Scholar]
- 16.Horwitz MT. Normal anatomy and variations of the peripheral nerve of the leg and foot: Application in operations for vascular deseases: Study of one hundred specimens. Arch Surg. 1938;36(4):626–36. [Google Scholar]
- 17.Dellon AL, Mackinnon SE. Tibial nerve branching in the tarsal tunnel. Arch Neurol. 1984;41(6):645–6. doi: 10.1001/archneur.1984.04210080053013. [DOI] [PubMed] [Google Scholar]
- 18.Heimkes B, Posel P, Stotz S, Wolf K. The proximal and distal tarsal tunnel syndromes. An anatomical study. Int Orthop. 1987;11(3):193–6. doi: 10.1007/BF00271447. [DOI] [PubMed] [Google Scholar]
- 19.Havel PE, Ebraheim NA, Clark SE, Jackson WT, DiDio L. Tibial nerve branching in the tarsal tunnel. Foot Ankle. 1988;9(3):117–9. doi: 10.1177/107110078800900304. [DOI] [PubMed] [Google Scholar]
- 20.Didia BC, Horsefall AU. Medial calcaneal nerve. An anatomical study. J Am Podiatr Med Assoc. 1990;80(3):115–9. doi: 10.7547/87507315-80-3-115. [DOI] [PubMed] [Google Scholar]
- 21.Davis TJ, Schon LC. Branches of the tibial nerve: anatomic variations. Foot Ankle Int. 1995;16(1):21–9. doi: 10.1177/107110079501600105. [DOI] [PubMed] [Google Scholar]
- 22.Louisia S, Masquelet AC. The medial and inferior calcaneal nerves: an anatomic study. Surg Radiol Anat. 1999;21(3):169–73. doi: 10.1007/BF01630895. [DOI] [PubMed] [Google Scholar]
- 23.Dellon AL, Kim J, Spaulding CM. Variations in the origin of the medial calcaneal nerve. J Am Podiatr Med Assoc. 2002;92(2):97–101. doi: 10.7547/87507315-92-2-97. [DOI] [PubMed] [Google Scholar]
- 24.Ndiaye A, Dia A, Konate I, Diop M, Sow ML. [Topographic anatomy of the tibial nerve in the medial malleolus: application to the effect of nerve block anesthesia.] Morphologie. 2003;87(277):25–7. [PubMed] [Google Scholar]
- 25.Bilge O, Ozer MA, Govsa F. Neurovascular branching in the tarsal tunnel. Neuroanatomy. 2003;2:39–41. [Google Scholar]
- 26.Joshi SS, Joshi SD, Athavale AS. Anatomy of tarsal tunnel and its applied Significeance. Journal of the Anat Soc india. 2006;55(1):52–6. [Google Scholar]
- 27.Govsa F, Bilge O, Ozer MA. Variations in the origin of the medial and inferior calcaneal nerves. Arch Orthop Trauma Surg. 2006;126(1):6–14. doi: 10.1007/s00402-005-0088-z. [DOI] [PubMed] [Google Scholar]
- 28.Moraes Filho DC, Galbiatti JA, Fialho HSA. Avaliação anatômica do túnel do tarso. Rev Bras de Ortop. 2000;35(8):282–9. [Google Scholar]
- 29.Moraes Filho DC, Carvalho Junior AE, Fialho HSA, Galbiatti JA, Carvalho DE. Nervo tibial: variações anatômicas do ramo calcâneo medial. Rev ABTPé. 2007;1(2):31–40. [Google Scholar]
- 30.Fernandes RMP, Mozella A, Dias M, Carvalho R, Andrade F, Babinski M, et al. Estudo anatômico do nervo tibial no túnel do tarso. Rev Bras de Ortop. 2006;41(7):272–7. [Google Scholar]
- 31.Rondhuis JJ, Huson A. The first branch of the lateral plantar nerve and heel pain. Acta Morphol Neerl Scand. 1986;24(4):269–79. [PubMed] [Google Scholar]