Abstract
Objective:
To evaluate the intra- and inter-examiner reliability and reproducibility of goniometry in relation to photogrammetry of hand, comparing the angles of thumb abduction, PIP joint flexion of the II finger and MCP joint flexion of the V finger.
Methods:
The study included 30 volunteers, who were divided into three groups: one group of 10 physiotherapy students, one group of 10 physiotherapists, and a third group of 10 therapists of the hand. Each examiner performed the measurements on the same hand mold, using the goniometer followed by two photogrammetry software programs; CorelDraw® and ALCimagem®.
Results:
The results revealed that the groups and the methods proposed presented inter-examiner reliability, generally rated as excellent (ICC 0.998 I.C. 95% 0.995 - 0.999). In the intra-examiner evaluation, an excellent level of reliability was found between the three groups. In the comparison between groups for each angle and each method, no significant differences were found between the groups for most of the measurements.
Conclusion:
Goniometry and photogrammetry are reliable and reproducible methods for evaluating measurements of the hand. However, due to the lack of similar references, detailed studies are needed to define the normal parameters between the methods in the joints of the hand. Level of Evidence II, Diagnostic Study.
Keywords: Goniometry, Photogrammetry, Reproducibility of tests, Hands
INTRODUCTION
The ability to move the joints is called range of motion (ROM) and can be evaluated as active and passive ROM. The active ROM is that performed when the individual uses their own muscles to make the movement, and passive ROM is one in which the examiner applies force to evaluate the range of motion.1
Range of motion (ROM) measurements are used extensively and need to be accurate. Two commonly cited sources for evaluating ROM values include the manual of the American Academy of Orthopedic Surgeons and the guide to goniometry of Norkin and White,2 dated 1997.
Authors report that the measurement of range of motion is the determinant parameter used in the evaluation and in the physiotherapy follow-up of patients with hand disability. The range of motion evaluation is necessary for the definition both of the propedeutics and of the prognosis in the individual submitted to hand rehabilitation.3
The reliability of measurements obtained by an instrument or by an examiner under the same evaluation conditions demonstrates their consistency. Intraexaminer reliability is defined as the consistency of measurements taken under the same evaluation conditions at two different times. Interexaminer reliability, in turn, is tied to the consistency of measurements taken by two different examiners. The standardization of the methodology is the fundamental parameter to control sources of mistakes, thus providing a reliable measurement.3
It is extremely difficult or even impossible to treat any hand injury without in-depth knowledge of its anatomy. This is true not only in surgical treatments, but also in the art of functionally rehabilitating this organ, which is so important in human relations. As the hand is a structure geared essentially towards function, functional anatomy or kinesiology, or the study of movements, is a vital part of the training of professionals dedicated to the treatment of hand injuries.4
The hand is an organ that is involved in practically all our activities of daily living, thus presenting a variety of functions, and to function perfectly it needs complete harmony between and among the various constituent tissues.5
Literature defines parameters in relation to the measurements taken in this study, such as palmar abduction of the thumb (0 - 50º), flexion of the proximal interphalangeal joint (0 - 110º) and flexion of the metacarpophalangeal joint (0 - 90º)1, which are consistent with other references that defined slightly different parameters such as a variation of 0 - 70º for palmar abduction of the thumb, 0 - 90º for flexion of the metacarpophalangeal joints, and also 0 - 110º for flexion of the proximal interphalangeal joints.6
Other authors define an arc of 60º for abduction movement of the thumb, 70º for flexion of the metacarpophalangeal joints, and up to 100º of flexion of the proximal interphalangeal joints of the fingers.7,8
The manual goniometry method is widely used in physiotherapy clinics for evaluation of the range of motion. The advantages of this method include low cost of the instrument and ease of measurement, which depends almost exclusively on the examiner's prior experience. These advantages made manual goniometry highly accessible in the physiotherapy clinic.1
Some studies opted for active ROMs, as they claim that these better represent function and are more reliable than passive movements; passive measurements are less reliable than active measurements, due to the variation of force applied by the therapist.9
While other authors reported that the measurement of ROM can be evaluated both actively and passively, yet passive measurement is used more often as it isolates the structures that can limit motion such as ligaments, joint capsule and antagonistic muscles, thus making it possible to extend the joint to its maximum range of motion, and for this reason, passive measurements are always higher than active.10
Limitation of motion can arise from deficient excursion of the musculotendinous unit or be due to capsuloligamentous limitation of the joint itself. Therefore, the goniometric evaluation of active joint mobility gives the idea of tendon excursion, while the evaluation of passive joint mobility reflects the ability of the joint to move within its normal range of motion, i.e., its limitation indicates problems in the joint.7
Some reports stressed the patient's comfort and listed factors that influenced the results of the measurement of the joint range of motion. These factors were age (children have a greater ROM than elderly individuals), sex (some authors found differences between men and women) and passive or active ROM (where passive ROM is greater than active) and edema or pain.1
The advantages of this method include low cost of the instrument and ease of measurement, which depends almost exclusively on the examiner's prior experience.1 These advantages made manual goniometry highly accessible in the physiotherapy clinic. The reliability of the universal goniometer, as a measuring instrument for the joints of the upper and lower limbs, is considered good to excellent, although this device presents a low level of reliability for the measurement of trunk range of motion.11
With the advent of the technology, digital photogrammetry has been considered an option for the quantitative evaluation of postural asymmetries in postural evaluation, and can be used to take linear and angular measurements.11
Computed photogrammetry, i.e., the application of metric photography, consists of a method of angular measurement of body asymmetries, using photogrammetric principles based on photographic images of the body.12 Moreover, it is a resource accessible to most physiotherapists who already use photography and own basic equipment such as a camera and a computer.13
Photogrammetry is a more accurate form of static evaluation. In this kind of evaluation, photographs are taken of the body segment to be evaluated with demarcations in pertinent anatomical reference points.14 However, the visual estimate is not an objective measure and its reliability is questionable, since there can be considerable differences between examiners.15
The studies demonstrated that universal goniometry measurements depend not only on the examiners' experience, but also on their training.16
In a recent bibliographical review, the participants did not find in literature any study with a similar proposal, or with the same division between groups, using a mold as an evaluation instrument and with the same objectives presented.
In this study we analyzed the reproducibility and reliability of three range of motion evaluation methods: the universal goniometer and photogrammetry through two types of software. We also analyzed the interexaminer and intra-instrument reliability for the angular measurements of opening of first web space (since the thumb does not favor goniometry use and there is a long list of traumatic or non-traumatic pathologies that decrease the first web space), flexion of the proximal interphalangeal joint of the forefinger and flexion of the metacarpophalangeal joint of the fifth finger, measurements that were chosen at random.
MATERIAL AND METHOD
Ethical considerations
The present survey was approved by the Institutional Research Board of Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), according to process HCRP no. 12811/2008. The participants were duly briefed on the study goals and signed the informed consent form expressing their agreement to take part in the survey, and received explanations about the procedures that would be required during the study.
Sample
The volunteers who met the criteria necessary to constitute the sample group of this study were invited to take part in the survey on an absolutely voluntary basis.
This sample group was made up of thirty volunteers divided according to level of education, with one group of ten university students from the ninth stage of the Physiotherapy course of FMRP-USP, the second group formed by ten physiotherapists with at least two years of experience in the area of Orthopedics and the third by ten hand therapists, chosen randomly, providing they were in a good state of health and agreed to take part in the survey.
The measurements were performed using a plaster-strengthened hand mold, taken by the three groups divided according to the level of education. Each group evaluated the same plaster-strengthened wax hand mold (Figure 1), and this was evaluated by all the methods and by all the examiners.
Figure 1.

Wax hand in the position in which the photographic record was taken.
The measurements were recorded by the researcher and later compared within each group, between the groups and between instruments.
Procedures
After the initial clarifications and agreement, all the participants became familiar with the instruments and began the collections according to the scheduled collection dates.
There was no demarcation of points due to their total visualization on the hand and to prevent volunteer inducement
Goniometric evaluation
Some rooms available at the Rehabilitation Center (CER) and outpatient department of Hospital das Clínicas (HC) da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP) were used for the study procedures. The rooms contained natural, as well as artificial lighting, and were reserved to ensure the privacy of the examiners.
Each examiner was positioned seated in a chair, and manipulated the hand mold to become familiar with it. They also handled the adapted goniometer to allow the best possible evaluation in the mold. The evaluation of range of motion was performed using the CARCI goniometer from Americanópolis, São Paulo. (Figure 2)
Figure 2.
Goniometer used - CARCI, Americanópolis, São Paulo, adapted at the Precision Workshop of USP.
Then each volunteer was asked to position the fulcrum of the goniometer corresponding to the axes of each joint according to their experience and practice in clinical evaluation.
Angles analyzed
The first measurement in the mold was abduction of the thumb, where the alignment of the goniometer follows steps 1) centralize the goniometer axis on the lateral surface of the radial styloid process, 2) align the proximal arm with the lateral midline of the second metacarpal, using the center of the second MCP joint as a reference and 3) align the distal arm of the goniometer with the lateral midline of the first metacarpal, using the center of the first MCP joint as a reference.16
The second measurement was flexion of the proximal interphalangeal joint of the second finger, where the steps for alignment of the goniometer are: 1) centralize the goniometer axis on the dorsal surface of the PIP joint, 2) align the proximal arm on the dorsal midline of the proximal phalanx and 3) align the distal arm of the goniometer on the dorsal midline of the middle phalanx.16 Finally, the third measurement, flexion of the metacarpophalangeal joint of the fifth finger, with the positioning of the goniometer following the steps 1) centralize the goniometer axis on the dorsal surface of the side of the MCP joint, 2) align the proximal arm on the midline of the metacarpal and 3) align the distal arm of the goniometer on the dorsal midline of the proximal phalanx.16 Each examiner from each group performed three measurements from each angle, always following the same sequence of angles analyzed.
There were limitations due to the fact that the measurements were taken in a wax hand mold that was separate from the body, which differs from a human hand.
Photographic evaluation - Photogrammetry
The photographic records were taken with a Sony digital camera with resolution of 7.2 mega pixels, positioned parallel to the ground, on a leveled Weifeng WT 3770 tripod. The digital images obtained were stored in a SAMSUNG - 500 GB external hard drive for subsequent analysis.
The researcher photographed the wax hand mold positioned on top of a 23.6cm bench on a table, from both sides.
The distance between camera and mold was standardized as 1m, with the help of a Tramontina® measuring tape. Due to the fact that the same mold was used for all the photographs, the tripod height was standardized at 1.12m (Figure 3). There were no markers used.
Figure 3.

Angle of palmar abduction of thumb, using CorelDraw X3 software.
IMAGE ANALYSIS
Software for data analysis
The digital photos were analyzed in an Acer computer with Windows XP, and the software CorelDraw X3 and ALCimagem 2.1 to quantify angles 1 (palmar abduction of the thumb), 2 (Flexion of the proximal interphalangeal joint of the second finger) and 3 (flexion of the metacarpophalangeal joint of the fifth finger of the hand), where each examiner from each group took three measurements from each angle, following the same sequence as the goniometric evaluation. The Corel Draw X3 software allows users to perform the digital definition of the straight lines that determine angular values in degrees. The ALCimagem software (Figure 4) is a mathematical algorithm that transforms image points into axes of Cartesian coordinates. The program allows users to quantify angles using the captured image.17
Figure 4.

Angle of flexion of the proximal interphalangeal joint of the second finger using ALCimagem 2.1 software.
The thirty volunteers once again took three consecutive measurements from each one of the angles with the two types of software separately, having the opportunity to repeat these measurements as many times as they considered necessary to be certain of the calculated angle. Once this procedure was completed the researchers noted down the angles of each examiner on their individual datasheet.
All the examiners evaluated at different times from the others and were only asked to perform the measurement on the dorsum of the hand for standardization of the method, improving accuracy and minimizing the possibility of errors, since many examiners expressed uncertainty regarding the positioning of the goniometer on the hand.
The CorelDraw X3 software presents the result of the angle on the computer screen on top of the studied image, and therefore, with each measurement obtained, the examiners call out the results to be recorded by the researcher. As the measurements using method 3, i.e., the ALCimagem 2.1 software, followed the sequence of the measurements performed using CorelDraw X3 software, and differed since the results appeared in a box in the right-hand corner of the screen, the researcher opted to keep the results of the angles that the examiners were evaluating hidden from them, and covered half of the computer screen with a sheet of wood paper. Hence the examiners were unaware of the angle that the researcher had recorded for all the results using this method, and this procedure also served to prevent the examiners from being influenced by the results of the method evaluated previously.
To evaluate the level of confidence among the different examiners, the same angles were analyzed by goniometry and by the two items of photogrammetry software, at different times and without their knowledge of the results obtained. Furthermore, during the evaluation with the ALCimagem software, the volunteers did not have access to the result to enable us to also conduct an evaluation comparing the two photogrammetry methods. In drawing the angles on the computer screen, a box would appear separate from the photo, whose researcher prevented visualization by the volunteer by means of a sheet of wood paper, and was the only one to have access, recording the measurements. The examiners could do and undo the measurements as many times as they wanted, and only inform them when they believed they were certain of the angle measured.
To guarantee the reliability of the angular measurements in the three methods, all the examiners had the same procedure. After the performance of the angle measurements, the results were deleted in the case of photogrammetry and the goniometer was closed and reset to zero, then the procedures were repeated twice more. In order to verify the intraexaminer reproducibility of the methods used in each specific group, the data of the three groups were compared within each group and with the others.
Statistical Analysis
The analysis of the interexaminer and intraexaminer reliability, and of the reproducibility of the method, was tested by the intraclass correlation coefficient - ICC, with a confidence interval (CI) of 95%. The ICC allows us to evaluate to which extent the multiple measurements are in agreement. The means of the values based on goniometry and photogrammetry obtained through the application of the variance analysis (ANOVA) were used for these calculations.
The Analysis of Variance (ANOVA) Method for Repeated Measurements was used both in the comparison between the groups for each angle and for each method, and in the comparison between the methods for each angle, in general and for each group. When there was a significant difference, we used the Bonferroni post hoc test. The statistical tests referred to here were carried out using the SPSS (Statistical Package for Social Sciences) program in version 17.0, considering significant differences p ≤ 0.05.
RESULTS
Results of the interexaminer reliability analysis - general data
The analysis of the general ICC values, i.e., the mean of the three angular measurements of each examiner in each situation (understanding situation as each method and each angle evaluated), forming nine measurements for each examiner, was classified as excellent (general ICC = 0.998 C.I. 95% 0.995 - 0.999).
Results of the interexaminer reliability analysis - specific data.
Table 1 illustrates the results referring to the ICC for each group (all the examiners from each group in all the situations).
Table 1.
ICC values for the interexaminer angular measurements obtained in the three groups 1 (scholars), 2 (physiotherapists), 3 (hand therapists).
| Group | ICC | C.I. | Classification |
| Group 1 | 0.995 | C.I. 95%(0.988-0.999) | Excellent |
| Group 2 | 0.995 | C.I. 95%(0.987-0.999) | Excellent |
| Group 3 | 0.992 | C.I. 95%(0.982-0.998) | Excellent |
ICC: Intraclass correlation coefficient; C.I.: Confidence interval.
Results of the interexaminer reliability analysis for each angle
The analysis of the ICC values for interexaminer reliability in all the situations for each angle revealed that the angular measurements represent excellent, acceptable and good levels. (Table 2)
Table 2.
ICC values for the interexaminer angular measurements obtained for each angle: 1 (palmar abduction of thumb), 2 (flexion of the proximal interphalangeal joint of the second finger), 3. (flexion of the metacarpophalangeal joint of the fifth finger).
| Angle | ICC | C.I. | Classification |
| Angle 1 | 0.903 | C.I. 95%(0.658-0.997) | Excellent |
| Angle 2 | 0.701 | C.I. 95%(0.0-0.992) | Acceptable |
| Angle 3 | 0.869 | C.I. 95%(0.576-0.996) | Good |
ICC: Intraclass correlation coefficient; C.I.: Confidence interval.
Results of the interexaminer reliability analysis for each method
The analysis of the ICC values for each method in all the situations is shown in Table 3, where they were classified as presenting excellent reliability. (ICC>0.900).
Table 3.
ICC values for the interexaminer angular measurements obtained in the three methods 1 (goniometer), 2 (Corel Draw photogrammetry), 3. (ALCimagem photogrammetry).
| Method | ICC | C.I. | Classification |
| Method 1 | 0. 998 | C.I. 95% (0. 988-0. 999) | Excellent |
| Method 2 | 0. 998 | C.I. 95% (0. 987-0. 999) | Excellent |
| Method 3 | 0.999 | C.I. 95% (0. 982-0. 998) | Excellent |
ICC: Intraclass correlation coefficient; C.I.: Confidence interval.
Results of the intraexaminer reliability analysis - general data.
Meaning the consistency of the measurements performed under the same conditions at two (or more, in this case, three) different times. Thirty volunteer examiners were assessed, hence each one had their ICC and the general was the mean of the ICCs of the examiners.
An excellent level of intraexaminer reliability was found, with mean ICC between the groups of 0.985, SD= 0.024.
Results of the intraexaminer reliability analysis - specific data.
Table 4 schematizes the degree of intraexaminer agreement of each group through the intraclass correlation coefficient, observing an excellent level of reliability.
Table 4.
ICC and standard deviation values for the intraexaminer angular measurements obtained for each group 1. (scholars), 2. (physiotherapists), 3. (hand therapists).
| Group | ICC | Standard Deviation |
| Group 1 | 0.986 | 0.022 |
| Group 2 | 0.974 | 0.033 |
| Group 3 | 0.993 | 0.003 |
ICC: Intraclass correlation coefficient.
Results of the intraexaminer reliability analysis for each angle. (Table 5)
Table 5.
Mean ICC and standard deviation values for the intraexaminer angular measurements obtained for each angle 1 (palmar abduction of thumb), 2 (flexion of the proximal interphalangeal joint of the second finger), 3 (flexion of the metacarpophalangeal joint of the fifth finger) in each group 1 (scholars), 2 (physiotherapists), 3 (hand therapists).
| Angle | Group 1 | Group 2 | Group 3 | Mean ICC |
| Angle 1 | ICC 0.724 | ICC 0.558 | ICC 0.871 | ICC 0.717 |
| SD 0.290 | SD 0.435 | SD 0.203 | SD 0.338 | |
| Angle 2 | ICC 0.494 | ICC 0.610 | ICC 0.446 | ICC 0.517 |
| SD 0.414 | SD 0.317 | SD 0. 360 | SD 0. 360 | |
| Angle 3 | ICC 0.660 | ICC 0.500 | ICC 0.598 | ICC 0.586 |
| SD 0.322 | SD 0.363 | SD 0. 322 | SD 0.331 | |
ICC: Intraclass correlation coefficient; SD: Standard deviation.
Results of the intraexaminer reliability analysis for each method. (Table 6)
Table 6.
ICC and standard deviation values for the intraexaminer angular measurements obtained for each method 1 (goniometry), 2 (Corel Draw photogrammetry), 3 (ALCimagem photogrammetry) in each group 1 (scholars), 2 (physiotherapists), 3 (hand therapists) and mean ICC of each method for each group.
| Method | Group 1 | Group 2 | Group 3 | Mean ICC |
| Method 1 | ICC 0.996 | ICC 0. 925 | ICC 0.995 | ICC 0.972 |
| SD 0.003 | SD 0. 213 | SD 0.003 | SD 0.124 | |
| Method 2 | ICC 0.992 | ICC 0.993 | ICC 0.991 | ICC 0.992 |
| SD 0.009 | SD 0.006 | SD 0. 006 | SD 0. 007 | |
| Method 3 | ICC 0.987 | ICC 0.978 | ICC 0.997 | ICC 0.987 |
| SD 0.033 | SD 0.039 | SD 0. 002 | SD 0.030 | |
ICC: Intraclass correlation coefficient; SD: Standard deviation.
Results of the comparison between the methods for each angle - general data.
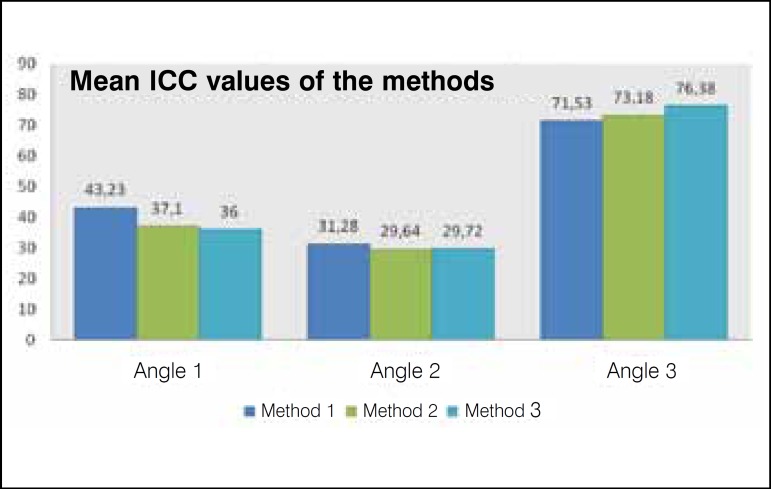
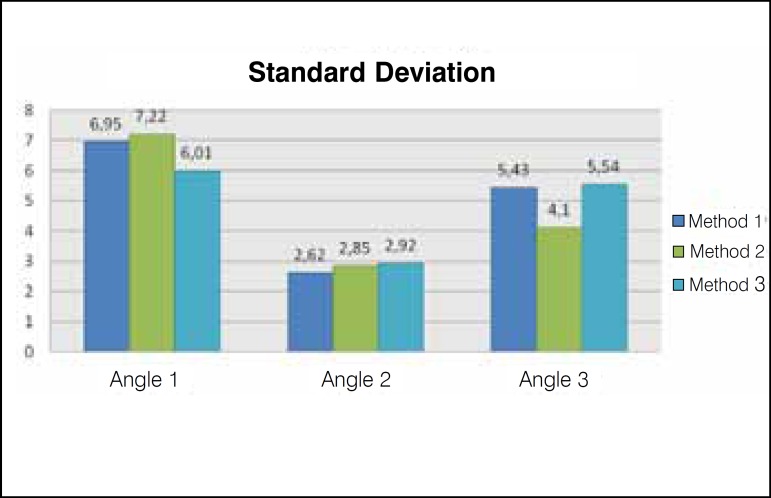
The analysis of the comparison between the three methods for each angle evaluated is shown in Figures 5 and 6. A significant difference was observed between the methods for all the angles.
Figure 5.
Mean ICC values between the methods for each angle.
Figure 6.
Mean standard deviation values between the methods for each angle.
For angle 1 (p<0.001), where method 1 has a significantly higher mean than method 2 (p = 0.002) and 3 (p= 0.001), i.e., M1 > (M2 = M3). In angle 2, we observed p = 0.03, where method 1 has a significantly higher mean than method 3 (p=0.05); therefore, M1 > M3, and in angle 3 (p < 0.001), with significant difference also existing between the methods, where method 3 has a significantly higher mean than method 1 (p<0.001) and method 2 (p<0.001), M3 > (M1 = M2).
Results of the comparison between the methods for each angle and for each group - specific data
Significance level adopted p≤0.05.
Since the significance level adopted was p≤0.05, in comparing the three methods in angle 1 for group 1, we obtained p = 0.015, with significant difference therefore existing between the methods. Method 1 has a significantly higher mean than method 3 (p = 0.04). (Table 7)
Table 7.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry) and 3 (ALCimagem photogrammetry) in angle 1 (palmar abduction of the thumb) for group 1 (scholars).
| Angle 1 | Group 1 |
| Method 1 | Mean 44.37 |
| SD 4.61 | |
| Method 2 | Mean 39.13 |
| SD 4.61 | |
| Method 3 | Mean 37.91 |
| SD 2.91 | |
SD: Standard deviation.
In the comparison between the three methods in angle 1 for group 2, we obtained p = 0.66, thus not evidencing significant difference. (Table 8)
Table 8.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry) and 3 (ALCimagem photogrammetry) in angle 1 (palmar abduction of the thumb) for group 2 (physiotherapists).
| Angle 1 | Group 2 |
| Method 1 | Mean 41.00 |
| SD 5.90 | |
| Method 2 | Mean 38.80 |
| SD 6.28 | |
| Method 3 | Mean 38.83 |
| SD 5.49 | |
SD: Standard deviation.
In the comparison between the three methods in angle 1 for group 3, we obtained p<0.001, thus evidencing significant difference. Method 1 has a significantly higher mean than method 2 (p = 0.003) and method 3 (p = 0.01). (Table 9)
Table 9.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry) and 3 (ALCimagem photogrammetry) in angle 1 (palmar abduction of the thumb) for group 3 (hand therapists).
| Angle 1 | Group 3 |
| Method 1 | Mean 44.33 |
| SD 9.54 | |
| Method 2 | Mean 33.37 |
| SD 8.34 | |
| Method 3 | Mean 31.28 |
| SD 6.33 | |
SD: Standard deviation.
In Table 10, p = 0.01, thus evidencing significant difference between the methods. Method 1 has a significantly higher mean than method 3 (p = 0.02).
Table 10.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry) and 3 (ALCimagem photogrammetry) in angle 2 (flexion of the proximal interphalangeal of the second finger) for group 1 (scholars).
| Angle 2 | Group 1 |
| Method 1 | Mean 32.33 |
| SD 2.28 | |
| Method 2 | Mean 29.87 |
| SD 1.91 | |
| Method 3 | Mean 29.51 |
| SD 1.64 | |
SD: Standard deviation.
Demonstrating in Table 11 that p= 0.74, thus not evidencing significant difference between the methods.
Table 11.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry) and 3 (ALCimagem photogrammetry) in angle 2 (flexion of the proximal interphalangeal of the second finger) for group 2 (physiotherapists).
| Angle 2 | Grupo 2 |
| Method 1 | Mean 31.37 |
| SD 3.11 | |
| Method 2 | Mean 30.03 |
| SD 3.79 | |
| Method 3 | Mean 30.67 |
| SD 3.92 | |
SD: Standard deviation.
In Table 12 we can observe p= 0.34, thus evidencing significant difference between the methods.
Table 12.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry) and 3 (ALCimagem photogrammetry) in angle 2 (flexion of the proximal interphalangeal of the second finger) for group 3 (hand therapists).
| Angle 2 | Group 3 |
| Method 1 | Mean 30.13 |
| SD 2.12 | |
| Method 2 | Mean 29.03 |
| SD 2.6 | |
| Method 3 | Mean 28.98 |
| SD 2.78 | |
SD: Standard deviation.
In Table 13, p= 0.004, thus evidencing significant difference between the methods. Method 3 has a significantly higher mean than method 1 (p = 0.02).
Table 13.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry), 3 (ALCimagem photogrammetry) in angle 3 (flexion of the metacarpophalangeal of the fifth finger) for group 1 (scholars).
| Angle 3 | Group 1 |
| Method 1 | Mean (69.37 |
| SD 6.00 | |
| Method 2 | Mean 71.73 |
| SD 2.71 | |
| Method 3 | Mean 75.14 |
| SD 6.22 | |
SD: Standard deviation.
In Table 14, p= 0.08, thus not evidencing significant difference between the methods.
Table 14.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry), 3 (ALCimagem photogrammetry) in angle 3 (flexion of the metacarpophalangeal of the fifth finger) for group 2 (physiotherapists).
| Angle 3 | Group 2 |
| Method 1 | Mean 73.40 |
| SD 4.20 | |
| Method 2 | Mean 75.13 |
| SD 4.35 | |
| Method 3 | Mean 76.83 |
| SD 4.97 | |
SD: Standard deviation.
In Table 15 it demonstrates p= 0.02, thus evidencing significant difference between the methods. Method 3 has a significantly higher mean than method 2 (p = 0.03) and method 1 (p = 0.05).
Table 15.
Comparison between the methods 1 (goniometry), 2 (Corel Draw photogrammetry), 3 (ALCimagem photogrammetry) in angle 3 (flexion of the metacarpophalangeal of the fifth finger) for group 3 (hand therapists).
| Angle 3 | Group 3 |
| Method 1 | Mean 71.83 |
| SD 5.67 | |
| Method 2 | Mean 72.67 |
| SD 4.57 | |
| Method 3 | Mean 77.18 |
| SD 5.72 | |
SD: Standard deviation.
Results of the comparison between the groups for each angle and for each method.
Significance level adopted p≤0.05.
In Table 16 we observed p= 0.48, thus not evidencing significant difference between the groups.
Table 16.
Comparison between the groups 1 (scholars), 2 (physiotherapists), 3 (hand therapists) in angle 1 (palmar abduction of the thumb) for method 1 (goniometry).
| Angle 1 | Method 1 |
| Group 1 | Mean 44.37 |
| SD 4.61 | |
| Group 2 | Mean 41.00 |
| SD 5.90 | |
| Group 3 | Mean 44.33 |
| SD 9.54 | |
SD: Standard deviation.
In Table 17 we observed p = 0.13, thus not evidencing significant difference between the groups.
Table 17.
Comparison between the groups 1 (scholars), 2 (physiotherapists) and 3 (hand therapists) in angle 1 (palmar abduction of the thumb) for method 2 (Corel Draw photogrammetry).
| Angle 1 | Method 2 |
| Group 1 | Mean 39.13 |
| SD 5.97 | |
| Group 2 | Mean 38.80 |
| SD 6.28 | |
| Group 3 | Mean 33.37 |
| SD 8.34 | |
SD: Standard deviation.
Table 18 demonstrates p= 0.005, thus evidencing significant difference between the groups. Group 3 presented a significantly lower mean than those of groups 1 and 2. G3 < (G1 = G2).
Table 18.
Comparison between the groups 1 (scholars), 2 (physiotherapists) and 3 (hand therapists) in angle 1 (palmar abduction of the thumb) for method 3 (ALCimagem photogrammetry).
| Angle 1 | Method 3 |
| Group 1 | Mean 37.91 |
| SD 2.91 | |
| Group 2 | Mean 38.83 |
| SD 5.49 | |
| Group 3 | Mean 31.28 |
| SD 6.3 | |
SD: Standard deviation.
In Table 19, p= 0.17, thus not evidencing significant difference between the groups.
Table 19.
Comparison between the groups 1 (scholars), 2 (physiotherapists) and 3 (hand therapists) in angle 2 (flexion of the proximal interphalangeal of the second finger) for method 1 (goniometry).
| Angle 2 | Method 1 |
| Group 1 | Mean 32.33 |
| SD 2.28 | |
| Group 2 | Mean 31.37 |
| SD 3.11 | |
| Group 3 | Mean 30.13 |
| SD 2.12 | |
SD: Standard deviation.
In Table 20 we observed p= 0.72, thus not evidencing significant difference between the groups.
Table 20.
Comparison between the groups 1 (scholars), 2 (physiotherapists) and 3 (hand therapists) in angle 2 (flexion of the proximal interphalangeal of the second finger) for method 2 (Corel Draw photogrammetry®)..
| Angle 2 | Method 2 |
| Group 1 | Mean 29.87 |
| SD 1.91 | |
| Group 2 | Mean 30.03 |
| SD 3.79 | |
| Group 3 | Mean 29.03 |
| SD 2.76 | |
SD: Standard deviation.
In Table 21, p= 0.43, thus not evidencing significant difference between the groups.
Table 21.
Comparison between the groups 1 (scholars), 2 (physiotherapists) and 3 (hand therapists) in angle 2 (flexion of the proximal interphalangeal of the second finger) for method 3 (ALCimagem photogrammetry®).
| Angle 2 | Method 3 |
| Group 1 | Mean 29.51 |
| SD 1.64 | |
| Group 2 | Mean 30.67 |
| SD 3.92 | |
| Group 3 | Mean 28.98 |
| SD 2.78 | |
SD: Standard deviation.
In Table 22, p= 0.25, thus not evidencing significant difference between the groups.
Table 22.
Comparison between the groups 1 (scholars), 2 (physiotherapists) and 3 (hand therapists) in angle 3 (flexion of the metacarpophalangeal of the fifth finger) for method 1 (goniometry).
| Angle 3 | Method 1 |
| Group 1 | Mean 69.37 |
| SD 6.00 | |
| Group 2 | Mean 73.40 |
| SD 4.20 | |
| Group 3 | Mean 71.83 |
| SD 5.67 | |
SD: Standard deviation.
In Table 23 we observed p= 0.16, thus not evidencing significant difference between the groups.
Table 23.
Comparison between the groups 1 (scholars), 2 (physiotherapists) and 3 (hand therapists) in angle 3 (flexion of the metacarpophalangeal of the fifth finger) for method 2 (Corel Draw photogrammetry®).
| Angle 3 | Method 2 |
| Group 1 | Mean 71.73 |
| SD 2.71 | |
| Group 2 | Mean 75.13 |
| SD 4.35 | |
| Group 3 | Mean 72.67 |
| SD 4.57 | |
SD - Standard deviation.
In Table 24 we observed p= 0.69, thus not evidencing significant difference between the groups.
Table 24.
Comparison between the groups 1 (scholars), 2 (physiotherapists) and 3 (hand therapists) in angle 3 (flexion of the metacarpophalangeal of the fifth finger) for method 3 (ALCimagem photogrammetry®).
| Angle 3 | Method 3 |
| Group 1 | Mean 75.14 |
| SD 6.22 | |
| Group 2 | Mean 76.83 |
| SD 4.97 | |
| Group 3 | Mean 77.18 |
| SD 5.72 | |
SD: Standard deviation.
DISCUSSION
Due to the pioneer nature of the application of the instruments studied (adapted goniometer and two items of photogrammetry software) in a plaster-strengthened wax hand mold, some stages of the evaluation had to be adapted by the examiners according to the best method found in relation to the positioning of the hand for specific evaluation by each one. The fact that the study subject was made of wax, despite having been molded on a human hand, imposed some limitations in the study and may have proved a hindrance to some volunteers in the handling and positioning of the goniometer as well as in the evaluation of the photos, which on the other hand, allowed the standardization of the angular measures.
There is a considerable error of goniometry when two or more examiners are assessed; hence it is advisable for the same therapist to monitor the measurements throughout the physiotherapeutic approach.18
Some studies found greater reliability in the evaluation carried out by photogrammetry than in the evaluation carried out through postural inspection.19
Reliability is related to the consistency with which the observations can be measured and recorded. Reliability and validity evaluation methods depend on the purpose of the survey, hypotheses and methodologies, and may involve quantitative, as well as qualitative evaluations.20
In our environment and also in literature, studies on goniometry and photogrammetry of the hand are scarce, so this was one of the reasons for the development of this investigation, as we only came across studies evidencing their use in postural and mandibular dysfunctions, larger joints, studies with cadavers, head and neck posture, and evaluation of the functional hand. Reports from the literature affirm that measurements in the hand are conflicting, and are not always performed in clinical practice, hence we failed to find any parameters for the establishment of multiple comparisons.21
In a similar study, when evaluating 28 volunteers, when they wished to quantify the accuracy in the measurement of the ROM of three joints of the fingers in a team of 13 surgeons and 13 hand therapists, to investigate the effect of a standardized goniometry protocol on this accuracy and to compare the accuracy between hand therapists and surgeons in the hand of a patient diagnosed with Dupuytren's disease, their results indicated that the accuracy of the hand therapists changed very little over the course of the study, as was already widely known. Using a standardized evaluation protocol, they concluded that the introduction of the standardized protocol positively influenced the accuracy of the results of the group of surgeons, and stressed the need to use standardization of the goniometry protocol in the evaluation of the ROM to improve the clinicians' accuracy with the tool and, therefore, to maintain the reliability of its results. They are also mindful of evidence that rounding the ROM up or down to the nearest degree, affected the accuracy of the results obtained.21
In our study dorsal placement of the goniometer was used to reduce the margin of error and to maintain standardization based on literature. The dorsal placement of the goniometer was preferred by 73% of the 231 professional volunteers in their research, and they also reported that lateral placement is occasionally preferred in difficult clinical situations (20%), while 7% of the practitioners revealed that they prefer lateral placement.22
The present study adopted the ICC values classified according to literature that considered: 1) excellent reliability for ICC above 0.90; 2) good reliability for ICC between 0.80 and 0.89; 3) acceptable for ICC between 0.70 and 0.79; 4) not acceptable for ICC below 0.70. These references were also used by Iunes in 2004 in his study that analyzed inter and intraexaminer reliability in postural evaluation using computed photogrammetry.17,23
The reference recommended for evaluation of the goniometric measurements is the technique of Norkin and White,2 as it systematically standardizes the position of the individual to be tested and of the goniometer, detailing the placement of the axis and fixed and mobile arms of this device.
Our findings sustain this claim, suggesting that a certain degree of standardization is necessary to obtain reliable data.
There are accounts that the fact that the examiners are inexperienced in measurement procedures and have one week of training would justify the low reliability of results found in their study.3 Our results are in accordance when we compare the methods, since we noted that there was only statistically significant difference when the group of scholars assessed flexion of the PIP of the 2nd finger, while there was no significant difference for the groups of physiotherapists and of hand therapists.
The reliability of goniometric measurements is affected by the measurement procedure. Many studies verified an increase of interexaminer reliability, when all the examiners used consistent and well defined test positions and measurement methods, which partly corroborates the results found in this study, since they reveal excellent inter (ICC 0.998 C.I. 95% 0.995 - 0.999) and intraexaminer (ICC 0.995 SD = 0.024) reliability.
Evaluating the means of the measurements performed through the three methods, we noted that the values obtained were very close, yet the statistical analysis carried out demonstrates that the measurements compared between the methods in each angle for each group are significantly different.
The Analysis of Variance (ANOVA) Method for repeated measurements was used for the comparison between methods, while the Bonferroni post hoc test was used when there was a significant difference. The significance level p≤0.05 was adopted.
When comparing the methods, in the angle of thumb abduction (p = 0.66), and flexion of the MCP of the 5th finger (p = 0.08), we only found no significant difference between the methods in the physiotherapists' group.
Based on the results found, we were able to observe that goniometry and computed photogrammetry using the two items of software (CorelDraw® and ALCimagem®) appeared very similar for the physiotherapists' group.
Another aspect to be highlighted in relation to the results is the analysis of the comparison between the groups for each angle and for each method. We verified that there was no statistical difference between the groups for most of the measurements taken, with the exception of the measurement of the thumb abduction angle with the ALCimagem® photogrammetry method between the three groups. This means that both the group of physiotherapy scholars, and the group of physiotherapists and hand therapists, as they were in full performance of their activities and practicing the method with standardization, presented reliable evaluation means.
It is believed that the unsatisfactory results found in this study are due to the fact that we used a wax hand mold and not a human hand, which may have influenced the positioning of the goniometer arms and hampered the trustworthy visualization of the hand in the photos in view of the hand's position, since Barry et al.,24 who wrote a summary on the use of digital photography in hand surgery and rehabilitation evaluating methods and results, claim that the angle in which the photo was taken interferes in the evaluation.
The results demonstrate that the methods proposed for the evaluations of hand measurements by photogrammetry and goniometry are satisfactorily reliable for most angular measures studied, when evaluated by the same examiner on different occasions and by different examiners in the same photographic record.
Note that there is still scarce literature on the association of photogrammetry and goniometry in hand measurements. This being the case, it is suggested that new studies be developed in the area to confirm and discuss our results and to get to know these methods better in these proposed angles.
CONCLUSIONS
Based on the results of this study, it was concluded that both in photogrammetry and in goniometry, significant correlation was observed in general between the groups and the methods. This indicates that, proportionally, the measurements vary in a similar manner, are related to one another and are reliable at the same time, thus generating reproducible data.
In relation to the proposed objectives, we concluded that:
There was excellent inter and intraexaminer reliability.
In analyzing and comparing the methods in relation to each angle and to each group, it was observed that depending on the angle there are different values between the methods. After comparison between the groups in relation to each angle and to each method, the results revealed that in the angles of flexion of the PIP of the 2nd finger and flexion of the MCP of the 5th finger for all the methods, there were no significant differences between the groups. And in the thumb abduction angle, there was only significant difference between the groups for the ALCimagem® method.
The standardization of measurements is essential to reduce the margin of errors.
Goniometry and photogrammetry are able to provide valid and reproducible data in the evaluation of ROM when the application methods are strictly followed, although there is still controversy regarding the best way of evaluating some joints. Therefore there is a great deal of room for further research, for there to be easy and comprehensive communication among health professionals working in the area.
It is also worth emphasizing that future studies should investigate these findings in the same joints and in other joints of the body in order to confirm the results afforded in the present study.
Acknowledgments
Faculdade de Medicina de Ribeirão Preto - Universidade de São Paulo, for the opportunity for accomplishment in the master's degree course. Coordenação de Aperfeiçoamento Pessoal de Nível Superior (CAPES) for their encouragement during the development of this study.
Footnotes
All the authors declare that there is no potential conflict of interest referring to this article.
Study conducted at Hospital das Clínicas de Ribeirão Preto in the Department of Biomechanics, Medicine and Rehabilitation of the Musculoskeletal System of Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo - FMRPUSP, Ribeirão Preto.
REFERENCES
- 1.Oliveira LM, Araújo PMP. Sociedade Brasileira de Terapeutas da Mão . Recomendações para avaliação do membro superior. São Paulo: Sociedade Brasileira de Terapeutas da Mão; 2003. Medida da amplitude articular; pp. 37–49. [Google Scholar]
- 2.Norkin CC, Write DJ. Medida do movimento articular: Manual de Goniometria. 2a ed. Porto Alegre: Artes Médicas; 1997. [Google Scholar]
- 3.Venturini C, Ituassú NT, Teixeira LM, Deus CVO. Confiabilidade intra e interexaminadores de dois métodos de medida da amplitude ativa de dorsiflexão do tornozelo em indivíduos saudáveis. Rev Bras Fisioter. 2006;10(4):407–11. [Google Scholar]
- 4.Pardini Junior GA. Anatomia funcional. In: Freitas PP, editor. Reabilitação da mão. São Paulo: Atheneu; 2006. [Google Scholar]
- 5.Freitas AD. Semiologia. In: Freitas PP, editor. Reabilitação da mão. São Paulo: Atheneu; 2006. [Google Scholar]
- 6.Marques AP. Manual de goniometria. São Paulo: Manole; 2002. [Google Scholar]
- 7.Araújo PMP. Avaliação funcional. In: Freitas PP, editor. Reabilitação da mão. São Paulo: Atheneu; 2006. [Google Scholar]
- 8.Hoppenffeld S. Propedêutica ortopédica: coluna e extremidades. São Paulo: Atheneu; 1998. [Google Scholar]
- 9.Andrade JA, Leite VM, Teixeira-Salmelas LF, Araújo PMP, Juliano Y. Estudo comparativo entre os métodos de estimativa visual e goniometria para avaliação das amplitudes de movimento da articulação do ombro. Acta Fisiátrica. 2003;10(1):12–6. [Google Scholar]
- 10.Barbosa MM, Filgueira VLS, Santana LA. Estudo comparative entre o goniômetro universal e o flexímetroSanny na mensuração da flexão passive da articulação do cotovelo. Fisioter Brasil. 2009;10(3):171–5. [Google Scholar]
- 11.Sacco ICN, Alibert S, Queiroz BWC, Pripas D, Kieling I, Kimura AA, et al. Confiabilidade da fotogrametria em relação a goniometria para avaliação postural de membros inferiores. Rev Bras Fisioter. 2007;11(5):411–7. [Google Scholar]
- 12.Baraúna MA. Biofotogrametria: recurso diagnóstico do fisioterapeuta. Rev O Coffito. 2002;17:7–11. [Google Scholar]
- 13.Iunes DH, Castro FA, Salgado HS, Moura IC, Oliveira ASE, Bevilaqua-Grossi D. Confiabilidade intra e interexaminadores e repetibilidade da avaliação postural pela fotogrametria. RevBrasFisioter. 2005;9(3):327–34. [Google Scholar]
- 14.Viton JM, Timsit M, Mesure S, Massion J, Franceschi JP, Delarque A. Asymmetry of gait initiation in patients with unilateral knee arthritis. Arch Phys Med Rehabil. 2000;81(2):194–200. doi: 10.1016/s0003-9993(00)90140-0. [DOI] [PubMed] [Google Scholar]
- 15.Watkins MA, Riddle DL, Lamb RL, Personius WJ. Reliability of goniometric measurements and visual estimates of knee range of motion obtained in a clinical setting. PhysTher. 1991;71(2):90–6. doi: 10.1093/ptj/71.2.90. [DOI] [PubMed] [Google Scholar]
- 16.Rome K, Cowieson F. A reliability study of the universal goniometer, fluid goniometer, and electrogoniometer for the measurement of ankle dorsiflexion. Foot Ankle Int. 1996;17(1):28–32. doi: 10.1177/107110079601700106. [DOI] [PubMed] [Google Scholar]
- 17.Iunes DH. Análise da confiabilidade inter e intra examinador na avaliação postural pela fotogrametria computadorizada [dissertação] Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo; 2004. [Google Scholar]
- 18.Youdas JW, Garrett TR, Harmsen S, Suman VJ, Carey JR. Lumbar lordosis and pelvic inclination of asymptomatic adults. PhysTher. 1996;76(10):1066–81. doi: 10.1093/ptj/76.10.1066. [DOI] [PubMed] [Google Scholar]
- 19.Iunes DH, Bevilaqua-Grossi D, Oliveira AS, Castro FA, Salgado HS. Análise comparativa entre avaliação postural visual e por fotogrametria computadorizada. RevBrasFisioter. 2009;13(4):308–15. [Google Scholar]
- 20.Ahlqvist O. Reliability and validity. In: Kitchin R, Thrifit N, editors. International encyclopedia of human geography. Oxford: Elsevier; 2009. pp. 320–3. [Google Scholar]
- 21.Pratt AL, Burr N. An investigation into the degree of precision achieved by a team of hand therapists and surgeons using hand goniometry with a standardised protocol. Br J Hand Ther. 2004;9(4):116–21. [Google Scholar]
- 22.Groth GN, Ehretsman RL. Goniometry of the proximal and distal interphalangeal joints, Part I: a survey of instrumentation and placement preferences. J Hand Ther. 2001;14(1):18–22. doi: 10.1016/s0894-1130(01)80020-x. [DOI] [PubMed] [Google Scholar]
- 23.Wahlund K, List T, Dworkin SF. Temporomandibular disorders in children and adolescents: reliability of a questionnaire, clinical examination, and diagnosis. JOrofac Pain. 1998;12(1):42–51. [PubMed] [Google Scholar]
- 24.Barry P, Meyer JC, Regnard PJ, Isselin J, Tchurukdichian A. [The use of digital photographs for surgical and rehabilitation records: Methods and results] Chir Main. 2002;21(5):329–34. doi: 10.1016/s1297-3203(02)00130-0. [DOI] [PubMed] [Google Scholar]