Effective treatments exist for substance abuse. Yet they are not widely available (Ducharme et al, 2007; Garner et al, 2009; McLellan et al, 2003). Precise estimates cannot be discerned from existing data, but at best, 25% of community providers may offer evidence-based treatments such as addiction medications, psychosocial therapies or integrated services for persons with substance abuse and HIV or co-occurring psychiatric disorders. This problem is not unique to substance abuse treatment. In medicine, it has been suggested that it takes 17 years to translate 14% of the research to direct patient care (Balas & Boren, 2000; Green et al, 2009).
1.0 A place for implementation research in substance abuse treatment
A new science has emerged to accelerate research discovery to public health benefit. Implementation research is the scientific study of processes and factors that are associated with successful integration of evidence-based interventions within a particular setting (Colditz, 2012). However, of over $100 billion in biomedical research funding in the United States annually, less than 1% is dedicated to implementation research (Dorsey et al, 2010). This spending ratio has not resulted in a favorable “return on investment” of public health research dollars.
Implementation research is a relatively new science. It is guided by a plethora of conceptual frameworks with scientific data slowly accruing. A new National Institute for Health (NIH) committee has been recently formed to review funding applications, and the 5th NIH annual conference on implementation research was recently held. Substance abuse treatment research has thus far been marginally represented in this new field. For example, at the recent NIH conference in March 2012, less than 7% of presentations included substance abuse-related topics. It is critical for the substance abuse treatment research community to increase its commitment to this emerging field of implementation research.
Researchers and treatment developers are frustrated by the pace of community uptake of evidence-based treatments for substance abuse and related conditions. Treatment providers are equally frustrated. The barriers to implementation range from lack of knowledge to attitudes to resources to system and financial disincentives. With respect to addiction medications for alcohol, opiates and smoking cessation, physician attitudes toward pharmacotherapy, as well as skill in contending with the complex needs of patients with substance use problems have been noted. In addition, some addiction medications are heavily regulated due to diversion risk, and others are not routinely on formularies or covered by insurance plans. Evidence-based psychosocial therapies may be quite different from clinicians’ existing practices. In addition, even if clinicians are trained in these approaches, such as cognitive behavioral therapy, the necessary clinical supervision and fidelity monitoring are not typically supported and are challenging to sustain. Finally, although effective tests and antiretroviral therapies for HIV/AIDs exist, their integration into routine substance abuse treatment settings is challenged by a number of factors. Among these are the obstacles to engaging complex, at-risk patients, many with varying levels of motivation, through multiple systems of care (Volkow & Montaner, 2011).
Research on substance abuse has emphasized the discovery of efficacious treatments. This work has yielded many medications, psychosocial therapies, and integrated therapies for persons with substance use disorders. Although this body of research has been impressive, the gap in implementing these effective treatments has become increasingly obvious. The emerging science for implementation research can and should be applied to substance abuse treatment research.
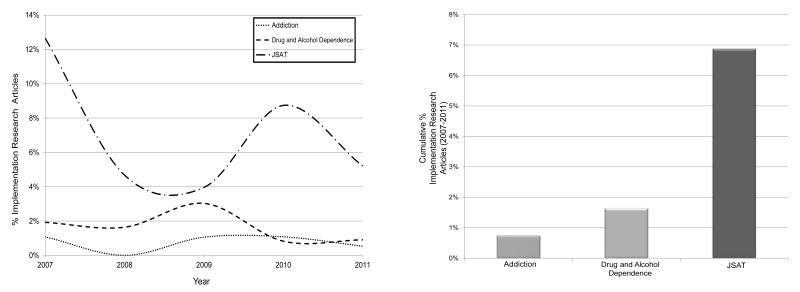
Implementation research is not simply “implementing” a treatment into a setting and then evaluating it for effectiveness. Instead, the analytic lens must expand to include not only the recipients of the treatment but the providers, organizations and systems within which the treatment is delivered. Figure 1 presents a simplified visual depiction of the path of implementation research. This path is the next leg of the journey for traditional efficacy or effectiveness research. The flow of the implementation research requires specification of the effective substance abuse “Intervention” being implemented (“Effective Treatments”), the “Routine Care Setting” within which the implementation is to take place, and “Pre-Implementation Measures” of baseline variables (for example, current use of the “intervention” and other potential mediators and moderators). The “Implementation Strategy” is the equivalent to a clinical intervention, but is the specific procedure hypothesized to increase the baseline measures of key variables. “Implementation Outcomes” pertain to the short term change in these variables as a direct result of the implementation strategies used. Comparative implementation strategy investigators may use RCT designs to articulate differential effectiveness, or in early stages, compare a promising implementation strategy to a control condition. Time series, roll-out or stepped wedge designs are alternatives. Questions arise about the sustainability or maintenance of implementation outcomes, given the continuation, removal or alteration of certain incentives. This corresponds to the maintenance of positive change (i.e. relapse prevention) and “Sustaining Outcomes.” Much like continuing care paradigms in treatment research, “Maintenance Strategies” are needed to solidify changes in routine clinical practice.
Figure 1.
Implementation Research Flow
The timeline in Figure 1 is based upon stages or phases of implementation research activity. The first phase, termed “Pre-implementation” is a preparatory stage within which the intervention is selected, measures defined and multi-level participatory groundwork completed. This may take up to 6-12 months. The Active Implementation phase may take up to 2 years (often corresponding to the timeline for an effectiveness trial period). The Maintenance phase is the relative persistence of implementation outcomes beyond the two years of active implementation.
Substance abuse treatment researchers should capitalize on foundational work by the pioneers of implementation research.
For instance, the Consolidated Framework for the Implementation Research (CFIR) is a relatively new, comprehensive synthesis of 19 preceding implementation models (Damschroder et al, 2009). This unifying framework subsumes theoretically distinct models and provides a common typology. The primary focus of the CFIR is the static and dynamic “pre-implementation” characteristics, i.e. factors or variables that may be associated with or predictive of implementation success or failure (Damschroder & Hagedorn, 2011). CFIR has been applied in post-hoc analyses of addiction treatment implementation efforts, including SBIRT, addiction medications and psychosocial therapies (Williams et al, 2011; Gordon et al, 2011; Manuel et al, 2011). Another example is the RE-AIM framework (Reach, Effectiveness, Adoption, Implementation, and Maintenance), which is increasingly utilized to plan the scope of an intervention to be implemented (Glasgow, 2006).
Finally, Proctor et al (2011) outlined three major implementation outcome dimensions: implementation, services and patient. The implementation dimension pertains to outcomes at the organizational level including cost and fidelity, the services dimension is drawn directly from the Institute of Medicine quality indicators and addresses efficiency and disparity (Institute of Medicine, 2001), and the patient dimension pertains to outcomes familiar to substance abuse treatment researchers, including alcohol and drug use, consequences and functioning.
Although Proctor et al provide a comprehensive list of potential implementation outcomes, including some familiar to treatment researchers, further specification and precision are necessary. Basic or essential implementation outcomes, describing the quantity and quality of the implementation, must be defined if not standardized.
A recent review found it impossible to conduct a systematic analysis comparing implementation strategies because of the paucity of definition and variation in terminology (Powell et al, 2012). In addition to developing operational manuals for implementation strategies, objective measures of fidelity to a given strategy are necessary. At present, there are no fidelity measures of implementation strategies, rendering comparison across studies or generalization beyond a single study impossible (McKibbon et al, 2010).
Although implementation research is itself a relatively new science, pioneering developments can serve to accelerate the relationship between addiction treatment research discoveries and routine public access. Unfortunately, many of these developments are conceptual and still need to be operationalized.
2.0 Implementation research and the Journal of Substance Abuse Treatment
The Journal of Substance Abuse Treatment (JSAT) has a longstanding tradition of connecting research findings with treatment providers. Details are provided to prospective authors in the Journal’s Aims and Scope section, placed immediately after the Table of Contents of each issue. Implementation research that focuses on the assessment and treatment of substance use and addictive disorders, including alcohol, illicit and prescription drugs, and nicotine, is highly appropriate for JSAT contributors and our readership.
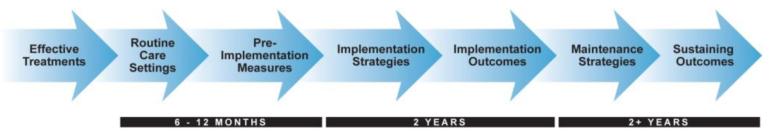
We were curious about the extent to which JSAT has published articles with an implementation research focus over the past five years. After a brief training, two research assistants independently reviewed JSAT issues, as well as the issues of two leading scientific addiction journals: Drug and Alcohol Dependence and Addiction. The audit categorized articles as implementation research related or not. Categorized articles included those involving the clinical impact of training, supervision, academic detailing, policy or protocol development, quality improvement research, dissemination, multi-faceted approaches (e.g. Network for the Improvement of Addiction Treatment [NIATx]), technology transfer or implementation. Editorials, commentary, obituaries, and other non-research articles were excluded. Over the five year period, the total number of articles (serving as the denominator) was: Addiction, 939 articles; Drug and Alcohol Dependence, 1341 articles; and JSAT, 494 articles. Generally, there was consensus on the classification of an article, and in the less than 10% of articles on which there was not, the first author determined the category. Volumes from the three journals over the past five years (2007-2011) were examined. Figure 2 depicts the findings.
Figure 2.
Implementation research publications in addiction journals, 2007-2011.
Overall, the three journals published a relatively small number of articles related to substance abuse and related condition (HIV/AIDs, co-occurring psychiatric disorders) treatment implementation research. The first graph displays the rates of implementation research articles by year. JSAT published the most articles each year, but displayed considerable variation during the five-year time frame. The second graph summarizes the data. Overall, in the past five years JSAT published twice as many papers as Addiction and Drug and Alcohol Dependence combined.
In its Aims and Scope, JSAT invites submissions that have both scientific merit and clinical relevance. The Aims and Scope of the other two journals do not share the same aims, and publish articles neither specific to treatment nor with an intention of immediate clinical relevance. In other words, we may have hypothesized a priori that JSAT would publish more articles focused on substance abuse treatment implementation research.
Nonetheless, the findings across all three journals, particularly here at JSAT, suggest that we too have not been making a sufficient commitment to implementation research.
In the following pages, you will find a Call for Papers for a Special Issue of JSAT dedicated to technology-based approaches to substance abuse treatment. Drs. Lisa Marsch, Brian Kulik and Kathleen Carroll will serve as guest editors, and welcome articles in this topic area. Technology and e-health applications hold promise to improve public access to effective treatments for substance abuse. Many behavioral health technology studies have thus far been addressing usability and efficacy, but researchers are now turning their focus to matters of implementation and sustainability in routine and ordinary clinical circumstances.
3.0 The promise and need for substance abuse implementation research
We are far from exhausting the scientific pursuit of effective treatments for substance abuse. Research is necessary to develop such treatments, to improve upon those that have already been evaluated, and of course, to explore their adaption in different settings, with different populations, and as delivered by different providers. This work must continue.
However, implementation research is necessary to take the efficacious therapies already available to scale. As a scientific discipline, implementation research has considerable room to grow. JSAT hopes to document this growth and continue to facilitate translation of evidence-based treatments into routine practice settings.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Elizabeth C. Saunders, Dartmouth Psychiatric Research Center
Eunhee Kim, Dartmouth College.
References
- Balas EA, Boren SA. Managing clinical knowledge for health care improvement. In: Bemmel J, McCray AT, editors. Yearbook of medical informatics 2000: Patient-centered systems. Schattauer Verlagsgesellschaft mbH; Stuttgart, Germany: 2000. pp. 65–70. [PubMed] [Google Scholar]
- Colditz GA. The promise and challenges of dissemination and implementation research. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: Translating science to practice. First ed. Oxford University Press; New York, NY: 2012. pp. 3–22. [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science: IS. 2009;4:50. doi: 10.1186/1748-5908-4-50. PMC2736161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder LJ, Hagedorn HJ. A guiding framework and approach for implementation research in substance use disorders treatment. Psychology of Addictive Behaviors. 2011;25(2):194–205. doi: 10.1037/a0022284. [DOI] [PubMed] [Google Scholar]
- Dorsey ER, de Roulet J, Thompson JP, Reminick JI, Thai A, White-Stellato Z, et al. Funding of US biomedical research, 2003-2008. JAMA: The Journal of the American Medical Association. 2010;303(2):137–143. doi: 10.1001/jama.2009.1987. PMC3118092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducharme LJ, Mello HL, Roman PM, Knudsen HK, Johnson JA. Service delivery in substance abuse treatment: Reexamining “comprehensive” care. The Journal of Behavioral Health Services & Research. 2007;34(2):121–136. doi: 10.1007/s11414-007-9061-7. [DOI] [PubMed] [Google Scholar]
- Garner BR. Research on the diffusion of evidence-based treatments within substance abuse treatment: A systematic review. Journal of Substance Abuse Treatment. 2009;36(4):376–399. doi: 10.1016/j.jsat.2008.08.004. PMC2695403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE. RE-AIMing research for application: Ways to improve evidence for family medicine. Journal of the American Board of Family Medicine: JABFM. 2006;19(1):11–19. doi: 10.3122/jabfm.19.1.11. [DOI] [PubMed] [Google Scholar]
- Gordon AJ, Kavanagh G, Krumm M, Ramgopal R, Paidisetty S, Aghevli M, et al. Facilitators and barriers in implementing buprenorphine in the veterans’ health administration. Psychology of Addictive Behaviors. 2011;25(2):215–224. doi: 10.1037/a0022776. [DOI] [PubMed] [Google Scholar]
- Green LW, Ottoson JM, Garcia C, Hiatt RA. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annual Review of Public Health. 2009;30:151–174. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Crossing the quality chasm: A new health system for the 21st century. National Academy Press; Washington, DC: 2001. [PubMed] [Google Scholar]
- Manuel JK, Hagedorn HJ, Finney JW. Implementing evidence-based psychosocial treatment in specialty substance use disorder care. Psychology of Addictive Behaviors. 2011;25(2):225–237. doi: 10.1037/a0022398. PMC3119356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKibbon KA, Lokker C, Wilczynski NL, Ciliska D, Dobbins M, Davis DA, et al. A cross-sectional study of the number and frequency of terms used to refer to knowledge translation in a body of health literature in 2006: A tower of babel? Implementation Science: IS. 2010;5:16. doi: 10.1186/1748-5908-5-16. PMC2834600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Carise D, Kleber HD. Can the national addiction treatment infrastructure support the public’s demand for quality care? Journal of Substance Abuse Treatment. 2003;25(2):117–117. [PubMed] [Google Scholar]
- Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Medical Care Research and Review: MCRR. 2012;69(2):123–157. doi: 10.1177/1077558711430690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7. PMC3068522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Montaner J. The urgency of providing comprehensive and integrated treatment for substance abusers with HIV. Health Affairs (Project Hope) 2011;30(8):1411–1419. doi: 10.1377/hlthaff.2011.0663. PMC3190599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams EC, Johnson ML, Lapham GT, Caldeiro RM, Chew L, Fletcher GS, et al. Strategies to implement alcohol screening and brief intervention in primary care settings: A structured literature review. Psychology of Addictive Behaviors. 2011;25(2):206, 214. doi: 10.1037/a0022102. [DOI] [PubMed] [Google Scholar]