Abstract
We examined the impact of an eye health education program for older African Americans on attitudes about eye care and utilization, using a randomized trial design in a community setting. Participants were older African Americans attending activities at senior centers. Ten centers were randomized to an eye health education (InCHARGE©) or social-contact control presentation. InCHARGE© addressed the importance of annual dilated comprehensive examination and strategies reducing barriers to care. The control presentation was on the importance of physical activity. Outcomes were attitudes about eye care through questionnaire 6 months post-event, and eye care utilization during 12 months post-event through medical record abstraction. At baseline > 80% participants in both arms said transportation and finding, communicating, and trusting a doctor were not problematic and agreed that yearly care was important. One-fourth said eye examination cost was problematic; one-half said spectacle cost was problematic. There were no group differences 6 months post-event. During 12 months pre-event, dilated exam rate was similar in the groups (38.3% InCHARGE©, 40.8% control), and unchanged during 12 months post-event. Results suggest less than half of older African Americans received annual dilated eye care. Group-administered eye health education did not increase this rate. Even before the program, they had positive attitudes about care, yet many cited examination and spectacle cost as problematic, which was not mitigated by health education. Evidence-based strategies in a community setting for increasing eye care utilization rate in older African Americans have yet to be identified. Policy changes may be more appropriate avenues for addressing cost.
Keywords: eye care utilization, eye health education, barriers to care
Population-based studies indicate that older African Americans have higher rates of vision impairment and blindness as compared to whites;1–5 they are also more likely to have diabetic retinopathy and glaucoma.3,4,6,7 Previous research also suggests that older African Americans are less likely to receive annual, comprehensive eye care when newly developing eye conditions could be diagnosed and treated while in their earliest stages.8–11 This lower rate of eye care utilization may be contributing to their higher rates of vision impairment and blindness, suggesting that strategies to increase utilization rates might reduce vision impairment in this population.
Many factors contribute to African-Americans' lower eye care utilization rate.12–17 These factors include inadequate knowledge about basic symptoms, risk factors and treatments for commons eye diseases and conditions; lack of awareness about the importance of routine preventive care; cost for exams, co-pays, and spectacles; transportation challenges; and communication and trust issues with the doctor and staff. It is well-established that health education programs have the potential for increasing health care utilization rates and stimulating disease prevention behaviors in at-risk populations.18 Health education programs are typically focused on improving knowledge and attitudes about health, disease and prevention, and communicating strategies to remove the perceived barriers to care. In recent years there has been a heightened awareness of health education in the U.S. and increased implementation of eye health education programs around the country.19 However, there is very little known about the effectiveness of these programs and their messages and materials, in spite of the fact that many public and private organizations advocate for and heavily invest in making eye health education materials available to clinical and public health professionals. There have only been two previous randomized studies evaluating whether eye health education programs actually increase eye care utilization rates. Both were clinic-based studies focused on inner-city African-American and Hispanic/Latino residents with diabetes who had not received an annual eye exam; both studies reported increases in the dilated fundus exam rate after distribution of educational material and telephone counselling.20,21,22 Increasing eye care utilization rates among those already in the health care system yet with minimal or no eye care utilization, while important, is distinct from accomplishing the same task among a community-based population with a wide range of experience with and access to eye care. The educational messages delivered to this diverse population must accommodate those with a heterogeneous mix of knowledge and behavior; encouraging some to initiate eye care and others to maintain their existing levels of care; still others may need to transition from erratic pattern of eye care utilization to one that is more routine.
To our knowledge, there has been no previous randomized study evaluating the effect of an eye health educational intervention on eye care utilization rates in community-based at-risk populations. Here we describe a randomized intervention evaluation of an eye health education program delivered in senior centers in a group format to older African Americans23 in terms of its impact on knowledge and attitudes about eye care six months after the program and on eye care utilization during the year following the program.
Methods
The Institutional Review Board of the University of Alabama at Birmingham approved the study. The research was compliant with the Health Insurance Portability and Accountability Act. This study is registered at ClinicalTrials.gov as identifier NCT00591110.
The area agency on aging facilitated our establishing relationships with 10 senior centers in Birmingham, Alabama serving predominantly African American communities, whose directors agreed to host our educational presentation and participate in its evaluation. Centers were located within churches or community centers. Figure 1 shows the design of the study. Senior center was the unit of randomization. Five centers were randomized to receive an eye health education presentation with the other five receiving a “social-contact control” presentation on the importance of physical activity, both of which are described later.
Figure 1.
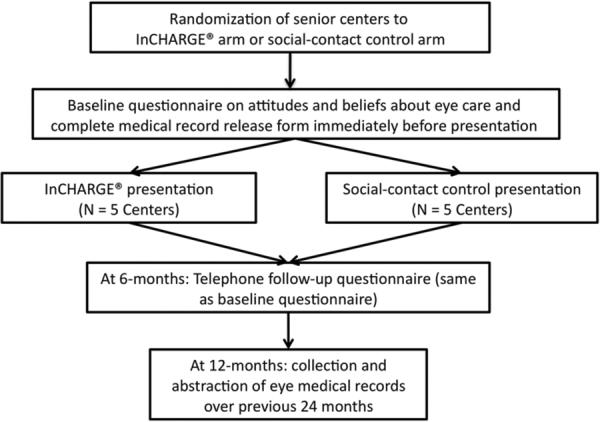
Study design.
Approximately one week before the presentation's scheduled date at a senior center, posters announcing the upcoming event were posted, and brochures were made available in areas of the center frequented by its visitors. In addition to a trained instructor who delivered the presentation, the team consisted of 2–3 assistants who helped greet attendees and assisted with distributing a short 7-item questionnaire to attendees before the presentation began.23 The questionnaire asked about attitudes, beliefs and perceived barriers with respect to issues involved in going to the ophthalmologist or optometrist, including: “If you wanted to see an eye doctor, would it be hard to find one?,” “If you had an appointment at an eye doctor, would you have a way to get there?,” “Is the cost of having an eye exam a problem for you?,” “If you need to get new eye glasses, would cost be a problem for you?,” “Are you comfortable talking to the eye doctor about your eyesight?,” “Do you think it is important to go to the eye doctor every year?” and “Do you think the eye doctor cares about your eyesight?” The response options were “yes” or “no.” The questionnaire was self-administered except in a few cases where an assistant administered the questionnaire to the attendee because of reading difficulty. Attendees were asked to provide their names, addresses, and telephone numbers as part of the questionnaire. They were informed that we would be telephoning them in six months to repeat the questionnaire and to gather their feedback on the presentation. They were also invited to complete a medical record release identifying the name of their “eye doctor” (ophthalmologist or optometrist), if they had one, and granting the project permission to obtain copies of their eye care medical records for research purposes. If they indicated that they had no eye care provider, this was noted on the form.
The presentation started after questionnaires and medical record releases were collected. The instructor stood in front of the group, and an easel was set up in front of the room displaying a sequence of posters conveying key messages and themes, synchronized in time with the instructor's remarks. The presentation lasted approximately 30 minutes and involved audience interaction in that the instructor often posed questions and solicited comments from the audience to facilitate audience participation and rapport. As attendees left the event, each received a tote bag containing an illustrated booklet summarizing the key points of either the eye health education program or the physical activity program, depending upon what study arm the center was assigned to.
Six months (± 2 weeks) after the date of the eye health education event/control event, participants received a telephone call at which time the aforementioned seven-item questionnaire was repeated. For those in the eye health education group we also asked an open-ended question “What was the most important thing you learned from the class?” Up to ten phone call attempts were made at various times of the day and early evening; after ten calls, if we were still unable to reach the participant, we sent the participant a brief letter indicating that we were trying to reach them in order to complete the follow-up questionnaire and requested they call us.
Twelve months following the date an attendee participated in an event, we obtained eye care medical records for those who completed a medical release form. Records were requested from their eye care provider for all visits over the previous 24 months. This provided information on visits 12-months before and 12-months after a participant's event date. At telephone follow-up participants were also asked if they had any eye care providers in the ensuing months in addition to the doctor they identified at baseline, and if so, medical records were also obtained from the additional provider(s). The exam at each visit was coded in terms of whether it was a dilated comprehensive examination or a non-dilated examination.
The eye health education program evaluated is called InCHARGE©, which stands for In Communities Helping African Americans Receive General Eye Care.17,23 It is targeted for older African Americans and promotes annual dilated eye examination by educating about the importance of routine preventive care and communicating strategies for removing perceived barriers to eye care. As described previously,17,23 InCHARGE©'s curriculum (Table 1) is both theoretically and empirically based. The curriculum guide and participant booklet are available at http://medicine.uab.edu/eyedoc/79227/. Its structure is motivated by theories of health behavior, specifically the empowerment model,24 the health belief model,25 and social learning theory.26 Its content is derived from several sources including focus groups with older African Americans in Birmingham and Montgomery, Alabama about attitudes and beliefs about eye care and perceived barriers to care,14 focus groups with ophthalmologists and optometrists providing care in these same communities, who discussed the same topics,14 the American Academy of Ophthalmology clinical practice patterns for comprehensive eye care,27 and materials made available through the National Eye Health Education Program.19
Table 1.
InCHARGE© curriculum
| Key Components |
|---|
| Being InCHARGE© of your eye health |
| Understanding prevention |
| What is prevention and why it is advantageous to health |
| How a comprehensive eye exam can be a way to prevent eye problems |
| Common eye problems for older African Americans |
| Blurry vision (near-sightedness, far-sightedness, presbyopia, cataract) |
| Glaucoma |
| Diabetic Retinopathy |
| What does a comprehensive eye exam involve |
| Parts of the eye your doctor may discuss with you |
| What does “dilated” mean; why is it important to have your eyes dilated |
| The difference between a comprehensive eye exam and a vision screening |
| Why it's important to get a comprehensive eye exam every year |
| Being InCHARGE© of solving common challenges |
| How to find an eye doctor |
| What is an ophthalmologist; optometrist; optician |
| Resource list for eye doctors in your area. |
| Making and keeping the appointment |
| How to find transportation to the eye doctor |
| Transportation services in your area if you don't drive or family/friend can't take you |
| Covering the cost of your comprehensive eye exam |
| Medicare and Medicaid: What do they cover |
| If you don't have health insurance: a resource list for eye care services |
| Communicating with your doctor |
| Your rights as a patient |
| Being a good listener |
| If you have questions, ask them. |
| Before the doctor leaves the room … |
| Building trusting relationship with your doctor |
| Being InCHARGE© of your eye care future |
| Setting a goal to have a dilated comprehensive eye exam every year |
| Be InCHARGE©; Steps 1, 2, and 3 |
| Making the commitment to your eye health |
For those senior centers randomized to the social contact control arm of the study, they received a presentation on the importance of physical activity. This presentation was delivered by the same instructor using the same format (e.g., posters displaying key points synchronized to the instructor's comments, audience interaction, same duration) as for the InCHARGE© presentations. The curriculum for the physical activity presentation was based on health education material made available through the websites of the Centers for Disease Control and Prevention, the National Institutes of Health, and the American Heart Association. Topics covered were the role of physical activity in preventing chronic diseases, common challenges to becoming physically active, and strategies for engaging in physical activity to improve wellness.
Statistical analysis
Based upon the number of enrollment study participants this study had approximately 80% power to detect a 20% difference between the InCHARGE© and control arms. A difference of this magnitude was chosen based upon similar community-based randomized trials in community or senior centers on the impact of health education on health care utilization among older African Americans.28,29 Differences in the responses to the questionnaire items between the InCHARGE© and control groups at baseline and 6-month follow-up were evaluated using Fisher's exact test. Within group changes from baseline to 6-month follow-up were evaluated using McNemar's test. P-values of ≤0.05 (two-sided) were considered statistically significant.
Results
There were 184 persons who attended either an InCHARGE© (81) or control (96) event across all senior centers, of whom 177 qualified for enrollment in the study because they were ≥ 60 years of age and African American. The number of participants at InCHARGE© events ranged from 14 to 18 attendees (mean 16) and from 13 to 23 (mean 19) at control events. Average median household income for the zip codes where our enrollees resided based on the 2000 U.S. census averaged $26,500.
A total of 117 persons completed both baseline and the 6-month follow-up telephone questionnaires, 54 in the InCHARGE© arm and 63 in the control arm. Reasons for not obtaining 6-month questionnaire data were person declined to be interviewed (5), could not be contacted because of no answer or invalid phone number (35), no phone number was provided at baseline (9), or significant frailty (e.g., in nursing home) (11). Of those who completed both the baseline and 6-month follow-up questionnaire, mean age in the InCHARGE© arm was 75 years (SD 8) and in the control arm 77 years (SD 8), p = 0.38. The distribution of men and women was identical in the two study arms with 87% women and 13% men.
Results from the baseline and 6-month follow-up questionnaires are presented in Table 2. At baseline there were no differences in the distribution of responses to questionnaire items in the InCHARGE© and control arms. The vast majority, over 80%, of participants in both the InCHARGE© and control arms at baseline, indicated that finding a doctor, transportation to an appointment, and communicating with the doctor were not problematic for them, and acknowledged the importance of going to the eye doctor each year and that the doctor cared about their eyesight. About three-fourths of participants in both groups (77.4% InCHARGE© group, 74.6% control group) indicated that cost of an eye exam was not a problem, and about half the participants in both groups (56.6% InCHARGE©, 55.0% control) indicated that the cost of eyeglasses was not a problem.
Table 2.
Participants in the InCHARGE© and control arms responding as indicated below on the questionnaire at baseline and 6-month follow-up
| Baseline | 6-Month Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| InCHARGE© arm | Control arm | p-valuea | InCHARGE© arm | Control arm | p-valueb | InCHARGE© arm pre vs. post p-value | Control arm pre vs. post p-value | |
| n (%) | n (%) | n (%) | n (%) | |||||
| Not hard to find doctor | 48 (88.9) | 58 (92.1) | 0.752 | 50 (92.6) | 58 (92.1) | 1.0 | .317 | 1.0 |
| Have a way to get to appointment | 47 (87.0) | 50 (80.7) | 0.453 | 42 (77.8) | 52 (83.9) | .479 | .166 | .467 |
| Comfortable talking to eye doctor | 51 (94.4) | 56 (90.3) | 0.500 | 51 (94.4) | 60 (98.4) | .340 | 1.0 | .025 |
| Important to go to eye doctor each year | 48 (88.9) | 60 (96.8) | 0.143 | 48 (92.3) | 57 (96.6) | .416 | .414 | 1.0 |
| Eye doctor cares about my eyesight | 52 (98.1) | 61 (98.4) | 1.0 | 46 (93.9) | 57 (90) | .096 | .317 | --- |
| Cost of exam not a problem | 41 (77.4) | 47 (74.6) | 0.829 | 44 (83.0) | 54 (85.7) | .799 | .405 | .052 |
| Cost of eyeglasses not a problem | 30 (56.6) | 33 (55.0) | 1.0 | 39 (72.2) | 39 (63.9) | .425 | .029 | .201 |
Comparison of study arms at baseline.
Comparison of study arms at 6-month follow-up.
At the six-month follow-up, there was no difference in the distribution of responses between the InCHARGE© and control arms for any of the questionnaire items. When change in questionnaire responses from baseline to six-months was analyzed within each group separately, for the InCHARGE© group the percentage of those acknowledging that cost was not a problem increased from 56.6% to 63.9% six-months after the InCHARGE© presentation (p =.029); responses on the other items did not change from baseline to follow-up. For the control arm, the percentage of those acknowledging that they were comfortable talking to the doctor increased from 90.3% to 98.4% (p=.025); responses on the other items did not change from baseline to follow-up. For those in the InCHARGE© arm, when asked at the 6-month follow-up “What was the most important thing you learned from the InCHARGE© class”, 53.7% (29 of 54) gave a response that was consistent with InCHARGE©'s main messages (e.g., importance of routine comprehensive eye examination, importance of having a dilated exam, information about common eye conditions in older African Americans). Thirty-three percent (18 of 54) said they could not recall anything they learned or had no response.
Of the 177 who attended InCHARGE© or control events, 136 (76.8%) completed a medical record release at baseline. When considered by group, 60 of 81 (74.1%) persons in the InCHARGE© group completed a release and 76 of 96 (79.2%) in the control group. Over the 24-month period (12 months before the event and 12 months after the event) there was a total of 109 exams in the InCHARGE© group for 60 persons, and a total of 129 exams in the control group for 76 persons. Two-thirds of exams (66%, 158 of 238) were dilated exams.
Figure 2 shows the percentage of participants having at least one dilated eye exam during the 12 months before the event and 12 months after, separately for the InCHARGE© group and control group. In the period 12 months before the event, the rate of dilated eye exam was similar in the two groups, with 38.3% of participants in the InCHARGE© group and 40.8% in the control group having a dilated exam (p = .860). Comparing the rate of dilated exam 12 months prior to the event to 12 months after the event within each group, there was no change in either group from the period before versus after the event (InCHARGE©, p = 0.429; control, p = .600). The percentage of those receiving a dilated eye exam 12 months following the event was not different between the two groups, with 33.3% in the InCHARGE© group and 44.7% in the control group receiving a dilated exam (p = .218). The pattern of results for any type of eye examination (regardless of whether dilated or not) was similar. This is not surprising since the majority of exams regardless of group and regardless of pre or post-event were dilated exams, as mentioned earlier.
Figure 2.
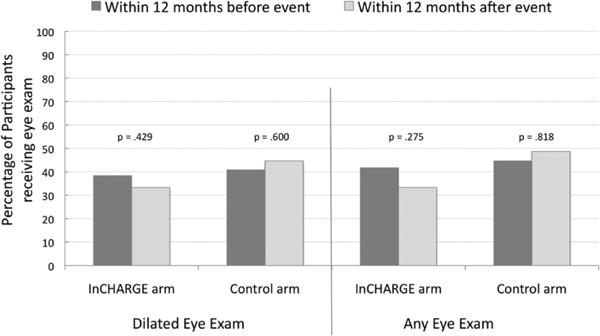
Percentage of persons receiving eye examinations during the 12-month period before and after participating in an InCHARGE© or a control event.
Discussion
An eye health education program delivered to older African Americans in the group setting of senior centers did not increase the percentage of participants getting a dilated eye exam in the year following the event, as defined by medical record abstraction. This absence of increase in the rate of dilated eye care after an eye health educational program was in spite of the fact that the InCHARGE© curriculum was theoretically motivated24–26 and empirically based14 in its focus on explaining the importance of prevention and routine dilated examination, eye health issues common among older African Americans, and strategies for removing perceived barriers to care. In addition, InCHARGE© was delivered by an instructor who used an interactive communication style, engaging participants in discussion. The facilitator was trained in InCHARGE©'s administration and was of the same race/ethnicity as the participants.
The lack of a positive impact of eye health education on the rate of eye examination in an at-risk population in the present study is in contrast to the results of two previous randomized studies20,21 where an eye health education intervention increased the rate of eye care utilization. But these disparate results may stem from important differences between our study and these prior studies20,21 which were both clinic-based, focused on a population already being seen in health system, used an individually-tailored intervention where multiple telephone counseling sessions were a key element, and focused on diabetic African American or Hispanic adults of all ages. Community outreach activities including group administration of eye health messages to at-risk populations, such as our InCHARGE© events, are a popular method for delivering eye health education messages,19 yet randomized designs have yet to establish the efficacy of this mode of delivery in terms of increasing eye care utilization. This is a critical challenge for future research.
When comparing results from the current study to prior work it is also important to consider differences in eye care utilization. Approximately 40% of the participants in the current study had received a comprehensive eye exam in the 12 months prior to the intervention whereas participants in prior studies were specifically selected on the basis of not having had a dilated retinal examination in, at a minimum, the prior 12 months. The post-intervention eye examination rate in prior studies was similar or only slightly higher than the baseline rate of eye examinations in the current study. Thus, the lack of an increase in eye examinations in the current study may be partly attributable to a ceiling effect. There may be only a limited segment of the population for whom knowledge is the primary impediment to eye care; for the remainder of the population other less surmountable factors (e.g., financial) may be of greater importance.
Our questionnaire data suggest that even before participating in an eye health education program, the vast majority of our older African American participants (> 80%) displayed positive attitudes about the importance of annual eye care and their ability to find a doctor and get to the appointment and indicated that they could communicate with the eye doctor who they also viewed as caring about them. These findings are consistent with the results of two recent studies on older African Americans in Alabama.17,23 Thus, it is unlikely that lack of awareness about the importance of eye care, how to find a doctor, communication problems and mistrust of the doctor, or transportation problems were the primary causes of the low rate of dilated eye care utilization (about 40%) in this population. About half of participants identified cost of the exam or eyeglasses as a problem, suggesting that cost is a major barrier to care in this population, consistent with previous work.4,10,13,17,23 Yet it is difficult if not impossible for an educational program, by itself, to mitigate the cost challenge. The InCHARGE© curriculum did address cost by providing information about what Medicaid and Medicare covers for those who are insured through these systems, and for those without this coverage, information was provided on how to seek services at the full-service eye clinic in the county hospital which provides services to the uninsured for a very modest fee or free of charge. However, the reality is that for those with Medicare or who seek eye care services at the county hospital, the cost of eyeglasses remains an out of pocket expense (except after cataract surgery in the case of Medicare), and the cost of refraction remains an out of pocket expense for those with Medicare. Thus, these cost barriers cannot be alleviated by an eye health education program.
In our study the percentage of African Americans ≥ 60 years old receiving annual eye care was approximately 40%, lower than the rates of 50%8 and 72%4 reported in two other studies providing estimates of utilization rates. This may stem from methodological differences among studies. In the present study utilization of eye care was defined by review of medical records provided by an ophthalmologist or optometrist, whereas in several previous studies where higher rates were reported, utilization is defined by self-report.4,8,9 Previous research has examined the relationship between self-reported healthcare utilization (not just eye care) and actual utilization, largely in older adult populations, finding that self-report data have highly variable accuracy.30 This previous research has not focused on utilization by older African Americans, and thus the literature provides little guidance about the validity of self-reported eye care utilization among older African Americans. One possible explanation for lower utilization rates for annual eye care in our study as compared to previous studies might be that the self-report methods lead to over-reporting of eye care use. This explanation seems feasible given that the questionnaire data in this and previous work17,23 suggest that many older African Americans are aware that going to the ophthalmologist or optometrist each year is useful and thus some may provide the socially-desirable, rather than veridical, response when asked whether they have seen an eye care provider recently. Recall bias may also exist, especially since they are elderly adults. Other explanations for the differences in utilization rates between our work and previous studies are also feasible. The Orr et al. study,8 part of the Salisbury Eye Evaluation,31 and the McGwin et al. study,4 an analysis of data from the Vision Impairment module of the Behavioral Risk Factor Surveillance System,32 are population-based studies, and are thus more representative of the general population. Our study sample consisted of African American older adults who attend senior center programs in their communities, and thus who are likely to be higher functioning and healthier than non-attenders since they travel outside the home on a routine basis. Additional differences in utilization rates among studies may include regional variations in cultural practices and expectations or economic status.
Strengths of this study include evaluating an eye health education intervention whose design was targeted for the population of interest, older African Americans, and whose structure and content were theoretically motivated and empirically based. The intervention evaluation study design was randomized and included a social-contact control group. Eye care utilization was defined by medical record review, rather than self-report, and over 75% of participants granted the study permission to obtain their medical records. Limitations must also be recognized. About one-third of persons who completed the baseline pre-event questionnaire were lost to telephone follow-up at 6 months mostly due to invalid phone numbers, no phone number, or no answer in spite of 10 calls. This suggests that future work in this area should consider avoiding phone contact as the primary mode of follow-up in this population. However, post-hoc analysis indicated that the baseline questionnaire data for those successfully phone-contacted at 6 months versus those lost to follow-up had similar distributions on all items, suggesting that there may not be large substantive difference in these populations with respect to the outcomes of interest. Though this study was adequately powered to detect a 20% post-intervention difference in eye care utilization rates, not all study participants completed the medical release form thus reducing the effective sample size for this comparison. However, even with a smaller sample size the study had approximately 65% power to detect the same 20% difference. Because the baseline questionnaire was administered in a field setting at an event where time was at a premium and self-administration was the primary mode of delivery, the questionnaire response options had to be simple and straightforward with a low number of items; the use of yes/no responses may not have been sensitive enough to gauge responses as compared to a Likert response scale with multiple options (e.g., extent of agreement with statement). It remains to be determined to what extent our findings generalize to older African Americans residing in other regions of the United States.
In conclusion, an eye health education program targeted for older African Americans and delivered in a group community setting did not increase the percentage of persons receiving dilated or any type of eye examination in the 12 months following the event. Even before the education event most older African Americans in our study had positive attitudes about seeking routine eye care, communicating and trusting their doctors, and setting up and getting to an eye care appointment. About one-half cited cost of eyeglasses as a problem and almost one-quarter cited the cost of the exam itself as problem, consistent with earlier work.17,23 It is unclear how group-administered eye health education could, by itself, minimize or eliminate the cost barrier; rather, policy or organizational changes and patient financial incentives may be more appropriate avenues for addressing this issue, as suggested by a recent synthesis of studies evaluating interventions to increase health care utilization rates in older adults.33
Acknowledgments
Funding support for this study was provided by the EyeSight Foundation of Alabama, Pfizer (Investigator-Initiated Research Program), Research to Prevent Blindness Inc., the Able Trust, and the National Institutes of Health (R21-EY014071).
Footnotes
Financial Disclosures: The authors have no financial disclosures to report related to this research.
References
- 1.Sommer A, Tielsch JM, Katz J, et al. Racial differences in the cause-specific prevalence of blindness in east Baltimore. N Engl J Med. 1991;325:1412–1417. doi: 10.1056/NEJM199111143252004. [DOI] [PubMed] [Google Scholar]
- 2.Congdon N, O′Colmain B, Klaver CC, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122:477–485. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- 3.Ryskulova A, Turczyn K, Makuc DM, Cotch MF, Klein RJ, Janiszewski R. Self-reported age-related eye diseases and visual impairment in the United States: Results of the 2002 National Health Interview Survey. Am J Public Health. 2008;98:454–461. doi: 10.2105/AJPH.2006.098202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGwin G, Khoury R, Cross JM, Owsley C. Vision impairment and eye care utilization among Americans 50 and older. Curr Eye Res. 2010;35:451–458. doi: 10.3109/02713681003664931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dillon CF, Gu Q, Hoffman HJ, Ko C-W. Vision, hearing, balance, and sensory impairment in Americans aged 70 years and over: United States, 1999–2006. NCHS Data Brief. 2010;31:1–8. [PubMed] [Google Scholar]
- 6.Friedman DS, Wolfs RC, O'Colmain BJ, et al. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol. 2004;122:532–538. doi: 10.1001/archopht.122.4.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang X, Saaddine JB, Chou C-F, et al. Prevalence of diabetic reitnopathy in the United States, 2005–2008. JAMA. 2010;304:649–656. doi: 10.1001/jama.2010.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orr P, Barron Y, Schein OD, Rubin GS, West SK. Eye care utilization by older Americans: The SEE project. Ophthalmology. 1999;106:904–909. doi: 10.1016/s0161-6420(99)00508-4. [DOI] [PubMed] [Google Scholar]
- 9.Bazargan M, Baker RS, Bazargan S. Correlates of recency of eye examination among elderly African-Americans. Ophthalmic Epidemiol. 1998;5:91–100. doi: 10.1076/opep.5.2.91.1577. [DOI] [PubMed] [Google Scholar]
- 10.Roy MS. Eye care in African Americans with Type I diabetes: the New Jersey 725. Ophthalmology. 2004;111:914–920. doi: 10.1016/j.ophtha.2003.08.033. [DOI] [PubMed] [Google Scholar]
- 11.Wang F, Javitt J, Tielsch J. Racial variations in treatment for glaucoma and cataract among medicare recipients. Ophthalmic Epidemiol. 1997;4:89–100. doi: 10.3109/09286589709057101. [DOI] [PubMed] [Google Scholar]
- 12.Walker EA, Basch CE, Howard CJ, Zybert PA, Kromholz WN, Shamoon H. Incentives and barriers to retinopathy screening among African-Americans with diabetes. J Diabetes Complications. 1997;11:298–306. doi: 10.1016/s1056-8727(96)00121-3. [DOI] [PubMed] [Google Scholar]
- 13.Hartnett ME, Key I, Loyacano N, Horswell R, DeSalvo K. Perceived barriers to diabetic eye care: qualitative study of patients and physicians. Arch Ophthalmol. 2005;123:387–391. doi: 10.1001/archopht.123.3.387. [DOI] [PubMed] [Google Scholar]
- 14.Owsley C, McGwin G, Scilley K, Girkin CA, Phillips JM, Searcey K. Perceived barriers to care and attitudes about vision and eye care: Focus groups with older African Americans and eye care providers. Invest Ophthalmol Vis Sci. 2006;47:2797–2802. doi: 10.1167/iovs.06-0107. [DOI] [PubMed] [Google Scholar]
- 15.Ellish N, Royak-Schaler R, Passmore S, Higginbotham EJ. Knowledge, attitudes, and beliefs about dilated eye examinations among African-Americans. Invest Ophthalmol Vis Sci. 2007;48:1989–1994. doi: 10.1167/iovs.06-0934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alexander RL, Miller NA, Cotch MF, Janiszewski R. Factors that influence the receipt of eye care. Am J Health Beh. 2008;32:547–556. doi: 10.5555/ajhb.2008.32.5.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Owsley C, McGwin G, Jr, Weston J, Stalvey BT, Searcey K, Girkin CA. Preliminary evaluation of the InCHARGE program among older African Americans in rural Alabama. J Health Dispar Res Pract. 2010;3:115–126. [Google Scholar]
- 18.DiClemente RJ, Crosby RA, Kegler MC. Emerging Theories in Health Promotion Practice and Research. Jossey-Bass; San Francisco CA: 2006. [Google Scholar]
- 19.National Eye Institute. National Eye Health Education Program (NEHEP) National Institutes of Health, Department of Health and Human Services [Accessed 06/15/11]; www.nei.nih.gov/nehep.
- 20.Basch CE, Walker EA, Howard CJ, Shamoon H, Zybert P. The effect of health education on the rate of ophthalmic examinations among African Americans with diabetes mellitus. Am J Public Health. 1999;89:1878–1882. doi: 10.2105/ajph.89.12.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker EA, Schechter CB, Caban A, Basch CE. Telephone intervention to promote diabetic retinopathy screening among the urban poor. Am J Prev Med. 2008;34:185–191. doi: 10.1016/j.amepre.2007.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones HL, Walker EA, Schechter CB, Blanco E. Vision is precious: A successful behavioral intervention to increase the rate of screening for diabetic retinopathy for inner-city adults. The Diabetes Educ. 2010;36:118–126. doi: 10.1177/0145721709356116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Owsley C, McGwin G, Jr, Stalvey BT, Weston J, Searcey K, Girkin CA. Educating older African-Americans about the preventive importance of routine comprehensive eye care. J Natl Med Assoc. 2008;100:1089–1095. doi: 10.1016/s0027-9684(15)31450-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Airhihenbuwa CO, Lowe AG. Improving the health status of African Americans: Empowerment as health education intervention. In: Livingston IL, editor. Handbook of Black American Health: The Mosaic of Conditions, Issues, Policies, and Prospects. Greenwood Press; Westport CT: 1994. pp. 387–398. [Google Scholar]
- 25.Rosenstock IM. The health belief model: Explaining health behavior through expectancies. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Heath Education: Theory, Research, and Practice. Jossey-Bass Publishers; San Francisco: 1990. pp. 39–62. [Google Scholar]
- 26.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 27.American Academy of Ophthalmology [Accessed 06/15/11];Compendium of Evidence-Based Eye Care™. 2010 http://one.aao.org/CE/PracticeGuidelines/CompendiumGuidelines.aspx.
- 28.Morgan PD, Fogel J, Tyler ID, Jones JR. Culturally targeted educational intervention to increase colorectal health awareness among African Americans. J Health Care Poor Underserved. 2010;21:132–147. doi: 10.1353/hpu.0.0357. [DOI] [PubMed] [Google Scholar]
- 29.Powe BD, Ntekop E, Barron M. An intervention study to increase colorectal cancer knowledge and screening among community elders. Public Health Nurs. 2004;21:435–442. doi: 10.1111/j.0737-1209.2004.21507.x. [DOI] [PubMed] [Google Scholar]
- 30.Bhandari A, Wagner T. Self-reported utilzation of health care services: Improving measurement and accuracy. Med Care Res Rev. 2006;63:217–235. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]
- 31.West SK, Munoz B, Rubin GS, et al. Function and visual impairment in a population-based study of older adults: The SEE Project. Invest Ophthalmol Vis Sci. 1997;38:72–82. [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System. Department of Health and Human Services; [Accessed 06/15/11]. http://www.cdc.gov/brfss/index.htm. [Google Scholar]
- 33.Shekelle PG, Stone E, Maglione M, et al. Interventions that increase the utilization of Medicare-funded preventive services for persons age 65 and older. U.S. Department of Health and Human Services, Health Care Financing Administration; 2003. [Accessed 06/15/11]. http://www.rand.org/pubs/reprints/RP1229.html. [Google Scholar]


