Abstract
Applied Relaxation (AR), which involves noticing early signs of anxiety and responding with a relaxation response, is an empirically supported treatment for Generalized Anxiety Disorder (GAD). However, research on hypothesized mechanisms of AR (e.g., reduced muscle tension) has been mixed, making it likely that additional mechanisms are contributing to the efficacy of AR. Stemming from more recent conceptualizations of GAD, it is hypothesized that mindfulness, decentering, and acceptance may be potential mechanisms of change in AR. Outcome, mechanism data, and case descriptions from three individuals diagnosed with GAD who received 16 weeks of AR as part of a larger randomized controlled trial are presented to demonstrate the ways that AR may lead to clinical improvement through mindfulness, decentering, and acceptance.
Generalized Anxiety Disorder (GAD) is characterized by anxiety, tension, and chronic and persistent worry (American Psychiatric Association, 2000). It is a chronic disorder, unlikely to remit without treatment (Yonkers, Warshaw, Massion, & Keller, 1996), which affects between 4–7% of the population (Kessler, Keller, & Wittchen, 2001). GAD is associated with a diminished quality of life (Hoffman, Dukes, & Wittchen, 2008) and is frequently comorbid with other anxiety and mood disorders (Kessler, Walters, & Wittchen, 2004). Cognitive-behavioral therapy, and in particular Applied Relaxation (AR), is considered an empirically supported treatment for GAD (Chambless & Ollendick, 2001).
As described in Borkovec and Costello (1993), AR is based on the premise that anxiety involves an interacting system of cognitive, physiological, affective, and behavioral responses. These responses are proposed to develop over time, with each channel amplifying the others, increasing the intensity of the anxious response. AR is aimed at teaching clients to notice the earliest signs of anxiety and to react with a different response, namely relaxation, before the cycle of anxiety has a chance to strengthen.
There is a large body of research showing that AR is efficacious in treating anxiety disorders. For example, AR has been shown to be more effective than a nondirective therapy (Borkovec & Costello, 1993) and roughly as effective as cognitive therapy (Arntz, 2003; Öst & Breitholtz, 2000) in treating GAD. In a meta-analysis, Siev and Chambless (2007) found that cognitive therapy and relaxation therapy were equivalent treatments for GAD. One study showed a clear benefit of CBT over relaxation therapy (Butler, Fennell, Robson, & Gelder, 1991); however, this study used only progressive muscle relaxation (PMR) and did not integrate applied relaxation (Öst, 1987). Although the efficacy of PMR and AR have yet to be compared for individuals with GAD, AR has incremental benefits over PMR in the treatment of panic disorder (Öst, 1988). It is worth noting that AR is just one of several efficacious approaches for GAD. For example, there are treatments that address other processes of GAD such as metacognitive awareness (Wells, 2007), intolerance of uncertainty (Robichaud & Dugas, 2006), emotion regulation (Mennin, 2004), interpersonal relationships (Newman, Castonguay, Borkovec, Fisher, & Nordberg, 2008), and mindfulness, acceptance, and engagement in valued actions (Roemer & Orsillo, 2009). While these processes also deserve research attention, the focus of this manuscript will be on a select group of change process that may be involved in AR.
It has been hypothesized that AR leads to changes in anxiety by decreasing muscle tension. If psychological distress stems from a generalized stress activation response that is comprised of multiple central and peripheral physiological systems (e.g., Öst, 1987), then learning to reduce activation of one system, here the muscular system, should also reduce activation in other systems (e.g., Gellhorn & Kiely, 1972). However, the research on the role of reduced muscle activation has been mixed at best (see Conrad & Roth, 2007 for a review). Therefore, while the reduction in tension likely plays some role in the efficacy of AR, there are likely other mechanisms of action that are playing important roles as well.
With the rise of acceptance-based interventions, there has been an increased focus on particular mechanisms of action that may be playing a role in cognitive behavioral therapies more generally. For example, both Arch and Craske (2008) and Orsillo, Roemer, Block Lerner, and Tull (2004) highlight the similarities and overlap between acceptance-based interventions and more “traditional” cognitive-behavioral therapies. Given this degree of similarity, coupled with our clinical observations of the kinds of changes clients receiving AR make, we were interested in looking more specifically at the ways that AR may lead to changes in three proposed mechanisms of change: mindfulness, decentering, and acceptance (described below). What follows is a description of how AR may lead to change through these mechanisms.
Mindfulness and decentering
It has been proposed that anxiety is partially maintained by a rigid, fused, judgmental relationship with internal experiences (Roemer & Orsillo, 2009). In fact, individuals diagnosed with GAD report lower levels of mindfulness than those without clinically significant anxiety (Roemer et al., 2009). Therefore, strategies that cultivate mindfulness, or a curious, non-judgmental awareness of the present moment (Kabat-Zinn, 2005) and promote decentering, that is, the process of seeing thoughts and feelings as objective events in the mind rather than personally identifying with them (Safran & Segal, 1990), are proposed to change this problematic relationship and reduce anxiety and related distress.
Many of the strategies used in AR likely cultivate mindfulness and decentering as relaxation is functionally similar to mindfulness (Borkovec & Sharpless, 2004). For example, self-monitoring of early indicators of anxiety likely changes an individual’s relationship with anxiety. The act of self-monitoring requires a different type of awareness, one that is characterized by a more objective and curious stance towards anxious responses. Furthermore, the acts of recording early cues on a monitoring sheet and observing and reporting on responses during an imaginal exercise both require the client to decenter and more objectively consider her or his responses.
PMR may also cultivate present moment awareness as clients who may typically seek to avoid or ignore anxiety-related symptoms are encouraged to focus on the sensations of tension and relaxation in the body. In addition to present-moment awareness, mindfulness also involves a compassionate, less judgmental type of awareness (Kabat-Zinn, 2005). This part of mindfulness is not explicit in PMR and we do not believe that all clients receiving PMR experience this self-compassionate mindful awareness; however, as illustrated below, some clients do appear to use PMR and early cue detection to change their relationships with their internal experiences in a mindful, decentered, or self-compassionate way.
Acceptance
Experiential avoidance, or the tendency to want to avoid or change one’s internal experience, has also been considered a fundamental process in anxiety disorders (Hayes, Strosahl, & Wilson, 1999) and has been shown to differentiate those with and without a diagnosis of generalized anxiety disorder (Lee, Orsillo, Roemer, & Allen, 2010). Although a natural response to uncomfortable experiences like anxiety is to avoid the anxiety-provoking stimuli, this response is often ineffective and may actually paradoxically increase distress (Salters-Pedneault, Tull, & Roemer, 2004). Each time an unwanted sensation arises, the inability to remove or change the unwanted experience serves as a reminder of the struggle with control. This inability to change the experience then elicits more negative reactions and urges to avoid and escape, perpetuating the cycle of anxiety. The alternative to experiential avoidance is acceptance (Hayes, Luoma, Bond, Masuda, & Lillis, 2006), or the recognition that experiences will come and go and that judging or resisting them is not useful.
Applied Relaxation may target acceptance in a number of ways. Most notably, the in-session imaginal exercises require the client to vividly recall anxiety-provoking situations. Similar to techniques used in other forms of behavior therapy, this re-experiencing exercise may serve the function of having clients notice their anxious responses while the therapist helps them to stay with the experience, encouraging clients to approach, rather than avoid. Likewise, rather than automatically responding to signs of anxiety, self-monitoring of cues also requires clients to approach the cues. PMR may also promote acceptance as clients are instructed to continue with the practice, while not responding with avoidance, regardless of what comes up during the exercise. Many clients report that they worry during PMR and so the repeated experience of practicing may be teaching clients that they can have worries without needing to respond to them; demonstrating that if they just let the worries be and focus their attention elsewhere (on relaxation), then the worries or their response to the worries eventually do change on their own. All of these aspects of AR likely increase the clients’ acceptance of the anxiety experience.
Taken together, it appears that the key elements of AR (early cue detection, self-monitoring, relaxation training, and applied practice) may at least partly impact anxiety through mindfulness, decentering, and acceptance. As a first step into the role that these mechanisms may play in AR, three cases selected from an ongoing randomized controlled trial are presented here to illustrate how the classic elements of AR can lead to changes in mindfulness, decentering, and acceptance.
Method
Participants
Three individuals who were part of a larger ongoing randomized controlled trial comparing AR to an Acceptance-based Behavioral Therapy (ABBT) were selected as participants in this study. Three therapists, who are co-authors here (SHS, AU, and JKL), each selected one client from their caseload. Clients were specifically selected because their cases demonstrated ways in which AR can lead to changes in mindfulness, decentering, and acceptance. In all three cases, potentially identifying information has been modified.
Participants were recruited into the larger treatment study from a pool of individuals who sought treatment at the Center for Anxiety and Related Disorders at Boston University. All participants were assessed using the Anxiety Disorders Interview Schedule for DSM-IV-Lifetime version (ADIS-IV-L; DiNardo, Brown, & Barlow, 1994). Trained assessors assigned clinician’s severity ratings (CSR) for each diagnosis ranging from 0 (not at all severe) to 8 (extremely severe/distressing). Assessors were blind to participants’ treatment condition for the post-treatment assessments. Participants were included in the larger study if they received a principal diagnosis of GAD (with a CSR of 4 or higher); were 18 or older; denied current suicidal intent; and did not meet criteria for bipolar disorder, substance dependence, or a psychotic disorder.
Treatment
The AR used in the present study was based on a protocol developed for the larger study (Hayes-Skelton, Roemer, & Orsillo, 2011) that was adapted from New Directions in Progressive Relaxation Training: A Guidebook for Helping Professionals (Bernstein, Borkovec, & Hazlett-Stevens, 2000) and Applied Relaxation: Manual for a Behavioral Coping Technique (Öst, unpublished). While AR has typically been conducted as a 12 session treatment, in this study, the length was extended to 16 sessions. The first four sessions were 90-minutes long and the remaining 12 were 60-minutes. Sessions were held weekly, with the exception of the last two sessions that were tapered to every other week. Each session began with a brief check-in and a diaphragmatic breathing exercise, followed by a review of the between session exercises (monitoring of anxiety and relaxation practice). Sessions ended with the assignment of skills to be practiced outside of therapy. In the first phase of therapy (sessions 1–7), sessions focused on anxiety psychoeducation, early cue detection exercises, and relaxation skills. Then, in the second phase of therapy (sessions 8–16), clients began applying brief relaxation exercises at the first sign of anxiety both in-session and throughout daily life. At the end of therapy (sessions 14–16), the focus was on maintaining skills and preventing relapse.
Relaxation training
In the first phase of therapy, sessions involved learning and practicing relaxation skills. Clients were explicitly told that the purpose of these relaxation exercises was to develop “skills that you can use to achieve a state of relaxation when you are feeling anxious and tense.” Clients were first introduced to relaxation training with diaphragmatic breathing. Several sessions were devoted to progressive muscle relaxation (PMR; Jacobson, 1934; 1938), which began with 16 different muscle groups, then was reduced to 7 and then to 4, as clients mastered the skill. To facilitate the development of relaxation strategies that could be readily applied across situations, the next step was to practice relaxing the muscles without first producing tension.
Next, cue-controlled relaxation was taught which involves pairing the word “relaxing” with the feeling of relaxation following PMR by silently repeating the words “inhale” and “relaxing” while inhaling and exhaling respectively so that eventually the word “relaxing” would induce a relaxed state. To further promote the adaptation of relaxation practice to real life situations, clients were taught differential relaxation which involves learning to relax the parts of the body that are not used during different daily activities (e.g., relaxing shoulder muscles while walking).
The final relaxation strategy taught was rapid relaxation; a practice that combines previously learned relaxation skills. Clients were instructed to take a deep breath (diaphragmatic breathing), while thinking the word “relaxing” on the exhale (cue-controlled relaxation) and scanning the body for spots of tension and releasing the tension (differential relaxation) as they engaged in daily life activities. When mastered, rapid relaxation takes 20–30 seconds and can therefore be practiced repeatedly throughout the day to address any early cues of anxiety. For a more detailed description of any of these relaxation practices, please see Bernstein and colleagues (2000).
Early cue detection
Early cue detection is based on the premise that it is easier to interrupt the cycle of anxiety early in the spiral when anxiety levels are lower. However, when anxiety is less intense, it is harder to recognize, thus practice is needed to help clients become skilled at noticing early signs of anxiety. Clients were encouraged to notice physical sensations (e.g., increased heart rate), behaviors (e.g., fidgeting), thoughts (e.g., “What if I fail the test”), or emotions (e.g. anger) as possible early signs of anxiety. Clients monitored their anxiety and detected cues outside of session. Additionally, imaginal exercises were used in session to detect early cues.
Applied Relaxation
An integral part of treatment was learning to apply relaxation to any sign of anxiety. Introduced at session eight, applied relaxation involved using early cue detection skills to monitor changes in baseline anxiety and applying a relaxation response to stop or slow its escalation. Therefore, clients were encouraged to apply relaxation in response to signs of anxiety frequently throughout the week and when they noticed an increase in anxiety during session.
Therapists
The therapists were two doctoral level psychologists and one advanced graduate student, two of whom had received training in AR from Dr. Tom Borkovec, an expert in treating GAD using AR (see Borkovec, 2006), while the third was trained by someone trained by him. All therapists received weekly supervision to ensure competence and adherence to the Applied Relaxation treatment manual (Hayes-Skelton, Roemer, & Orsillo, 2011). Further, selected sessions were randomly chosen to be evaluated for therapist competence and adherence by independent raters. Adherence was defined as following the treatment protocol and not engaging in methods or strategies that would overtly be considered acceptance or mindfulness based or cognitive restructuring. For these three cases, therapists were rated as adherent and competent.
Measures
Symptom Measures
The Structured Interview Guide for the Hamilton Anxiety Rating Scale (SIGH-A; Shear et al., 2001)
The SIGH-A is a structured format for administering the Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959). The SIGH-A is an interviewer-based measure of anxiety in which the interviewer assesses 14 dimensions of anxiety. Scores can range from 0 to 56 with higher scores indicating higher levels of reported anxiety.
Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990)
The PSWQ is a 16-item self-report measure of trait levels of worry. Scores on the measure range from 16 to 80 with higher scores indicating higher levels of worry. The PSWQ has demonstrated good to very good internal consistency (α from .86 to .93) and good test-retest reliability (Molina & Borkovec, 1994). Additionally, scores on the PSWQ has been found to discriminate GAD from other anxiety disorders (Brown, Antony, & Barlow, 1992).
Quality of Life Inventory (QOLI; Frisch, Cornwell, Villanueva, & Retzlaff, 1992)
The QOLI assesses the importance and satisfaction within 16 areas of life. Respondents indicate the degree of importance and the level of satisfaction in each domain and then these two values are multiplied to result in a composite score. The QOLI has demonstrated good internal consistency (α’s from .83 to .89), excellent test-retest reliability (r = .91), and adequate validity as assessed by correlations with other measures of well-being and satisfaction (Frisch et al., 1992).
Depression Anxiety Stress Scales-21-item version (DASS-21; Lovibond & Lovibond, 1995)
This self-report measure yields separate scores for depression, anxiety, and stress. For this study, we only used the Stress scale, which assesses anxiety and tension. Scores are based on a 4-point Likert-type scale and range from 0 to 21 with higher scores indicating more anxiety. The DASS-21 has demonstrated excellent internal consistency (α from .88 to .94; Antony, Bieling, Cox, Enns, & Swinson, 1998) and the longer 42-item version has demonstrated adequate test-retest reliability (Brown, Chorpita, Korotitsch, & Barlow, 1997). Additionally, the Stress scale discriminated between clients with GAD and those with other anxiety disorders (Brown, et al., 1997). To aid in comparisons with other studies and with norm data, DASS-21 scores were doubled to provide equivalent DASS-42 scores. Within a group of individuals without clinical diagnoses, the average DASS-Stress score on the 42-item version of the DASS was 10.11 (SD = 7.91; Lovibond & Lovibond, 1995). This was used as the population average to calculate standard scores on the DASS for the participants in this study.
Mechanism Measures
Acceptance and Action Questionnaire (AAQ; Hayes et al., 2004)
The AAQ is a 9-item self-report measure designed to assess acceptance of internal experiences. Lower scores on the AAQ reflect more acceptance. This measure has demonstrated adequate internal consistency (α = .70) and test-retest reliability (r = .64) over four months in an undergraduate sample (Hayes et al., 2004). Scores on the AAQ moderately correlate with measures of the related construct of cognitive avoidance (r = .50). In a sample of European-American college students, the average score on the AAQ was 33.6 (SD = 6.9; Hayes et al., 2004). This was used as the population average to calculate standard scores on the AAQ for the participants in this study.
Five Factor Mindfulness Questionnaire (FFMQ; Baer, Smith, Hopkins, Krietemeyer & Toney, 2006)
The FFMQ is a 39-item measure of various aspects of mindfulness including nonreactivity to inner experience, observing/attending to sensations, acting with awareness, describing, and nonjudging of experience. On this measure, participants respond on a 5-point Likert-type scale that ranges from never or very rarely true to very often or always true, with higher scores indicating higher levels of mindfulness. The five subscales have demonstrated good internal consistency (alphas from .75 to .91) and both incremental and discriminant validity (Baer et al., 2006). In a community based sample, the average score on the FFMQ was 116.90 (SD = 14.16; Baer et al., 2008). This was used as the population average to calculate standard scores on the FFMQ for the participants in this study.
Experiences Questionnaire – Decentering subscale (EQ-decentering; Fresco, Moore, et al., 2007)
The EQ is a 20-item self-report measure that includes two subscales designed to assess decentering and rumination. For the purposes of this study, we used the decentering subscale. On this subscale, participants respond on a 5-point Likert-type scale that ranges from never to all the time. Higher scores reflect more decentering. The decentering subscale has demonstrated convergent and discriminate validity and good internal consistency in both nonclinical and clinical samples with alpha coefficients of .83 and .84, respectively (Fresco, Moore, et al., 2007; Fresco, Segal et al., 2007). On average undergraduate students scored 37.51 (SD = 3.58) on the decentering subscale (Fresco, Moore, et al., 2007). This mean was used as the population average to calculate standard scores on the EQ-decentering subscale.
Procedures
Clients completed the diagnostic interview (ADIS-IV) and the SIGH-A prior to beginning therapy and post-treatment. The symptom and mechanism measures listed above were administered pre- and post-treatment and following sessions 4, 8, and 12. The DASS was administered at every session; however, for consistency with the other measures, only data from pre- and post-treatment and sessions 4, 8, and 12 are reported in this study.
Case Descriptions and Results
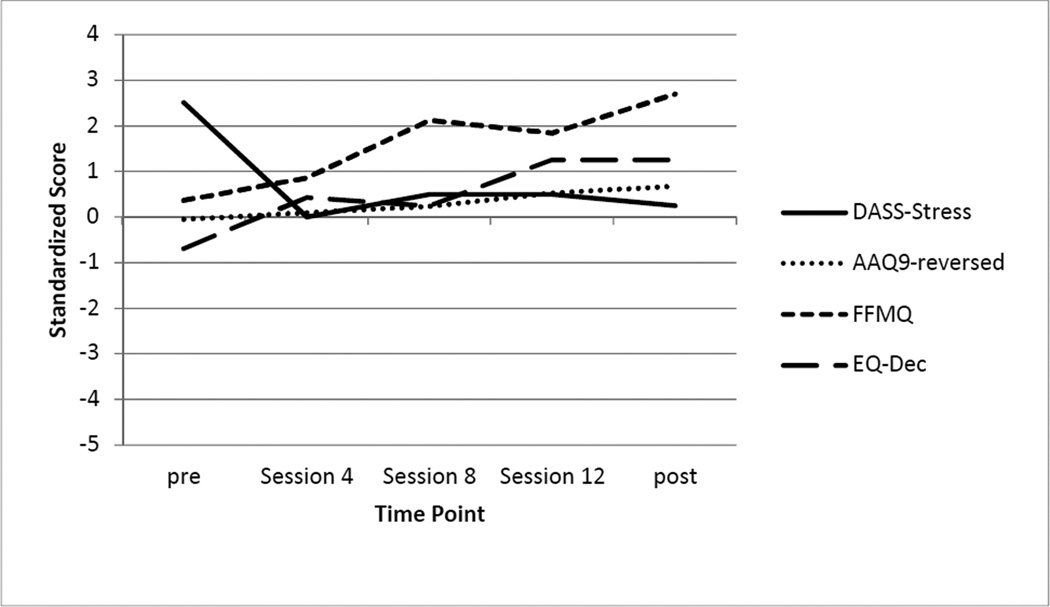
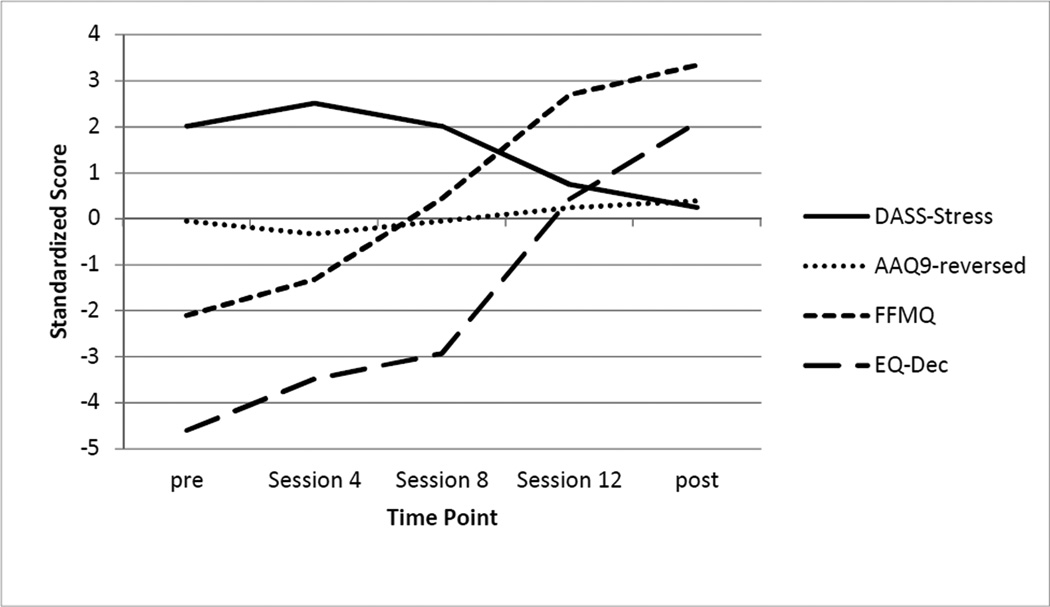
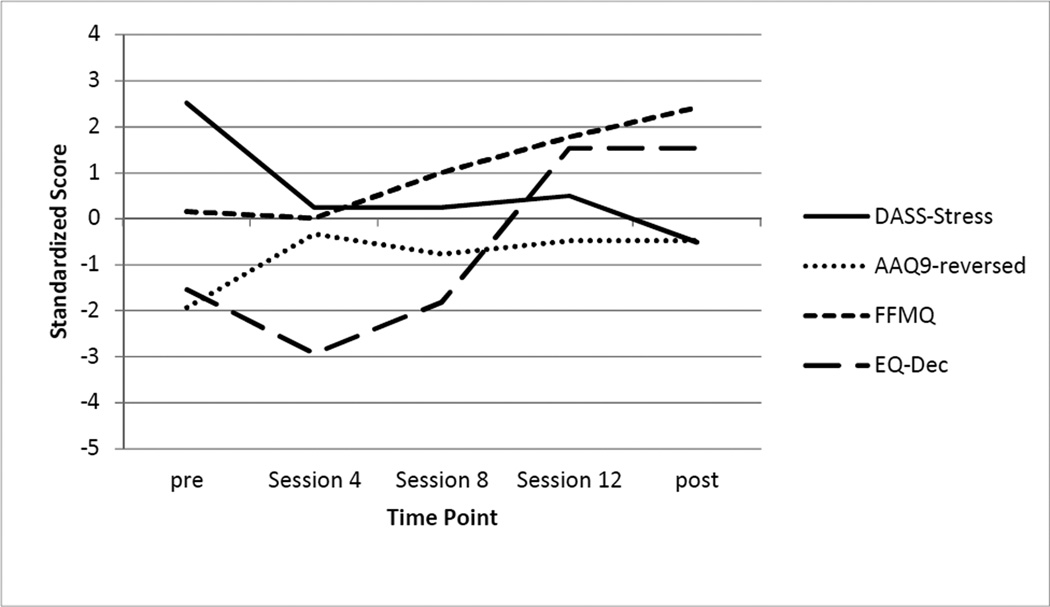
What follows are case descriptions of the three cases demonstrating the potential ways AR may influence mindfulness, decentering, and acceptance. Table 2 provides outcome data at pre- and post-treatment as well as at a 12-month follow-up assessment. Table 3 provides the scores for measures of potential treatment mechanism measured every four sessions. Figures 1–3 provide standard scores for the treatment mechanisms and DASS-stress subscale for each client.
Table 2.
Pre-treatment, Post-treatment, and Follow-up Scores on Measures of Anxiety, Worry, and Quality of Life
| Julia |
Doug |
Kendra |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | 12MFU | Pre | Post | 12MFU | Pre | Post | 12MFU | |
| ADIS Severity | |||||||||
| - GAD | 5 | 2 | 2 | 5 | 0 | 0 | 6 | 1 | 0 |
| - Other | 4 (social) | 4 (social) | -- | -- | -- | -- | 5 (panic) 5 (anxNOS) 4 (social) |
4 (anxNOS) 2 (social) |
2 (anxNOS) 2 (social) |
| SIGH-A | 26.0 | 10.5 | 4.0 | 12.0 | 2.5 | 1.5 | 22.0 | 9.5 | 5.0 |
| PSWQ | 74 | 44 | 31 | 76 | 42 | 50 | 67 | 42 | 31 |
| DASS-Stress | 30 | 12 | 6 | 30 | 6 | 6 | 26 | 12 | 8 |
| QOLI | 1.00 | 3.64 | 3.71 | 1.75 | 4.88 | 4.13 | 1.69 | 1.71 | 0.71 |
Note: 12MFU = 12-month follow-up; SIGH-A = Structured Interview Guide for the Hamilton Anxiety Rating Scale; PSWQ = Penn State Worry Questionnaire; DASS-Stress = Stress subscale from the Depression, Anxiety, and Stress Scale 21-item version; QOLI = Quality of Life Inventory.
Table 3.
Mechanisms of Change Across Therapy: Acceptance, Mindfulness, and Decentering
| Pre- treatment |
Session 4 |
Session 8 |
Session 12 |
Post- treatment |
|
|---|---|---|---|---|---|
| AAQ | |||||
| Julia | 34 | 33 | 32 | 30 | 29 |
| Doug | 47 | 36 | 39 | 37 | 37 |
| Kendra | 34 | 36 | 34 | 32 | 31 |
| FFMQ | |||||
| Julia | 122 | 129 | 147 | 143 | 155 |
| Doug | 119 | 117 | 131 | 142 | 151 |
| Kendra | 87 | 98 | 123 | 155 | 164 |
| EQ-decentering | |||||
| Julia | 35 | 39 | 38 | 42 | 42 |
| Doug | 32 | 27 | 31 | 43 | 43 |
| Kendra | 21 | 25 | 27 | 39 | 45 |
Note: AAQ = Acceptance and Action Questionnaire; FFMQ = Five Factor Mindfulness Questionnaire; EQ = Experiences Questionnaire.
Figure 1.
Standardized Scores for Julia
Figure 3.
Standardized Scores for Kendra
Julia: A demonstration of increasing acceptance
Julia was a 45-year-old, heterosexual, married woman, with four children, who self-identified as White. She presented for treatment for chronic worry and anxiety. At her initial assessment, Julia reported significant and persistent worry in a number of areas, including completion of daily chores, finances (even when financially stable), work and interactions with her colleagues, her relationship with her husband and the health of her father and father-in-law. Julia’s father was physically disabled and she was his primary caregiver. The anxiety and worry made it difficult for Julia to relax and she often experienced physical pain and tension throughout her body, especially in her legs and back. Moreover, she noted that her worry and anxiety made it hard for her to connect with people and she felt that she pushed people away.
In addition to the worries listed above, Julia also reported severe levels of restlessness, muscle tension, irritability, and being easily fatigued more days than not on the ADIS-IV-L interview. Based on the initial ADIS-IV-L interview, Julia was assigned a principal diagnosis of GAD and an additional diagnosis of Social Phobia. Her scores on self-report measures taken at the time also indicated moderate to high levels of worry, stress, and anxiety (see Table 2). Her DASS-stress score was approximately 2.5 standard deviations above the mean. Her initial scores for mindfulness and acceptance were close to the norm, whereas her initial decentering score was approximately half a standard deviation below the mean.
During the first four sessions of therapy, Julia experienced significant improvement in her DASS-stress score as well as initial increases in mindfulness and decentering. Although she began therapy with some awareness of her early signs of anxiety, particularly physical responses such as tension in her legs or stomach, Julia’s awareness appeared to increase across these early sessions. By session four, Julia’s EQ-decentering score increased from approximately half a standard deviation below the mean to half a standard deviation above the mean.
Between sessions four and 12, Julia reported continued increases in decentering and mindfulness, as her scores were approximately one and two standard deviations above the mean at session 12. These increases were consistent with her clinical presentation. For example, Julia noted that although she occasionally experienced a “sense of anxiety,” and urgency that in the past would have cued a behavioral response, she was now able to simply notice those sensations and stay in the present moment, rather than give in to the perception that she constantly needed to be engaged in some activity. Julia also reported a steady increase in her acceptance in that her AAQ score increased from approximately the norm at session 4 to over half a standard deviation below the mean by session 12. In therapy, although Julia initially described a need to be in control of her anxiety, by session 9, she began to reflect that control over her anxiety might in fact not be necessary to live a satisfying life. At session 9, Julia also reported her lowest DASS-stress score of a 2.
Towards the end of this period in therapy, Julia reported that she no longer felt that external circumstances had to dictate her behavior and actions. She became more open to embracing life experiences, including difficult ones. This is particularly significant, because Julia’s father passed away between sessions 10 and session 11, which likely contributed to her increased DASS-stress score around this time. However, even in the midst of this painful loss, Julia continued to report increases in mindfulness and acceptance and decreases in her DASS-stress scores throughout the rest of therapy. She was particularly aware of how elements of AR had helped her during the grieving process. For example, she described accepting that losing someone was part of the human experience and expressed surprise over her continued ability to focus on other issues in the face of this loss. She also felt that the process of AR had helped her understand her father’s death and that she had taken time to “stop and feel” which was the opposite of her previous experiential avoidance habit. It is possible that early cue detection may have helped her notice her experience of grief by focusing on the emotions she felt, including any early cues of anxiety, rather than habitually avoiding them. By session 16, Julia had made significant improvement in treatment. As can be seen in Table 2, her anxiety across measures had decreased by post-treatment and at 12 month follow-up. Her independent assessor found her GAD to be at a subclinical level. During her post-treatment interview she reported a decrease to moderate feelings of fatigue, mild levels of GAD-related somatic symptoms, denied any difficulties with restlessness, muscle tension, or irritability. She also experienced decreases in worry and improvement in her quality of life. Her DASS-stress score was in the normal range by the end of therapy and it continued to decline at follow-up. Likewise, her FFMQ and EQ-decentering scores were both above the mean and her AAQ was below the mean (indicating more acceptance).
Doug: A demonstration of increasing decentering
Doug was a 25-year-old, married, White, heterosexual male with one child who sought treatment for worry and anxiety. After recently graduating from college, he had been working as an intern at a radio station. When he presented for therapy, Doug described feeling that his worry and anxiety were growing progressively worse since he had graduated from college and he described being in a perpetual state of angst. He reported experiencing very severe levels of uncontrollable worry that were primarily centered on his performance and interpersonal interactions at work. He believed that his worry and anxiety prompted feelings of anger and resentment toward work and required duties, which often led him to procrastinate. During his ADIS-IV-L interview, Doug reported moderate to severe levels of feelings of restlessness, being easily fatigued, difficulties concentrating, and difficulties sleeping more days than not. For example, at the pre-treatment assessment, his DASS-stress score was approximately 2.5 standard deviations above the mean. Based on these responses, Doug received a principal diagnosis of GAD, which was considered moderate. His initial scores on acceptance and decentering were approximately 1.5 and 2 standard deviations away from the mean indicating less acceptance and decentering, whereas his mindfulness score was similar to the population mean (see Figure 2).
Figure 2.
Standardized Scores for Doug
The first four sessions of therapy were focused on increasing Doug’s awareness of his early cues of anxiety and building relaxation skills. By session 4, Doug reported an initial drop in his DASS-stress score and a large, almost two standard deviation, change in self-reported acceptance. During these sessions, Doug described a number of new observations. For example, he remarked on how, for the first time, he was consciously and purposefully attending to his body in a relaxed state in the present moment. He also approached these new situations with curiosity.
During the middle section of therapy, Doug experienced significant increases first in his mindfulness and then his decentering scores. These changes were also reflected in the language that he used during session. For example, Doug described a sensation of being “detached” from his thoughts and feelings while in the relaxed state, saying that he felt more fully aware of his experience. This allowed him to see anxiety-provoking situations differently, so that he felt like he had some flexibility and choice with regard to how he might respond. In session 7 Doug described an analogy in which his worries and anxiety were like a little kid who is having a tantrum, trying to get his attention. Rather than impulsively overreacting to these signals, Doug described what we would consider a decentered stance. Specifically, he described being able to stand back and notice anxiety simply as a natural response from his body, or as part of being human.
It was not until around session 12 that Doug began to experience a steady decline in his DASS-stress scores. In a critical moment during session 12, after a relaxation exercise, Doug described having a moment of clarity regarding his experience of worry and anxiety. He noted that worrying about minor matters may have been distracting him from a fear of pursuing his dream of composing music. Doug began to see his emotional distress as a natural result of not engaging in a meaningful career and thus he decided to leave his job, which would give him more time and flexibility to pursue more personally relevant goals. Doug’s ability to observe his anxiety from a more decentered perspective may have provided him clarity to examine the contextual factors contributing to his distress and consider a variety of behavioral options, rather than responding habitually.
By the end of therapy, Doug had quit his job and found part time employment as a barista at a café, while he made preparations to pursue a master’s degree in musical composition. He described some worry and anxiety about preparing his graduate school entrance portfolio, but, by his report, these responses caused him very little distress. He also denied any significant difficulties with restlessness, concentration, sleep, or fatigue. By the end of therapy, Doug’s decentering and mindfulness scores were approximately 1.5 and 2 standard deviations above the mean. He did not receive any diagnoses during his post-treatment independent assessment and his self-reported anxiety and worry fell below subclinical thresholds. Notably, at post assessment his DASS-stress score was half a standard deviation below the norm. These changes were maintained through his one year follow up assessment.
Kendra: A demonstration of increased mindfulness shifting experiential avoidance
Kendra was a 35-year old, White, heterosexual woman who presented to therapy with significant anxiety and worry regarding her work as a special education teacher. Although she described herself as always having been anxious, she felt her anxiety had significantly worsened in the past three years and that it was beginning to significantly interfere with her performance. Constant worries about her performance in the classroom, her ability to manage difficult students, and the appropriateness of her lesson plans were interfering with her ability to make on the spot decisions. Kendra also described frequently becoming irritable and angry with her students. Because of her discomfort in the classroom, she often woke up dreading going to school and frequently called in sick.
In addition to these concerns, Kendra reported moderate to severe muscle tension, feelings of restlessness and irritability, and a tendency to become easily fatigued more days than not on the ADIS-IV-L interview. Based on her initial ADIS-IV-L interview, she received a principal diagnosis of GAD and comorbid diagnoses of Panic Disorder with Agoraphobia, Social Phobia, and Anxiety Disorder Not Otherwise Specified. As can be seen in Table 2, Kendra reported moderate to strong levels of worry and anxiety based on the self-report questionnaires, with her pre-treatment DASS-Stress score approximately two standard deviations above the mean. Scores on mindfulness and decentering were below the mean (see Figure 3).
Kendra initially struggled to identify her early signs of anxiety. A main focus of early therapy sessions was the early cue detection exercises. Kendra imaginally recalled anxiety/anger provoking situations to try to identify the pattern of responses that led to emotional escalation. Although this strategy is used in AR to identify when relaxation can be applied, it also may increase mindful awareness of internal experiences and may have contributed to the increase in FFMQ scores Kendra experienced from pre-treatment to session 4. Although Kendra’s AAQ scores were close to the normative level through session 4, this self-reported level of acceptance was not consistent with her in session presentation. For example, at session 4, Kendra expressed anger towards her therapist for suggesting an imaginal exercise, stating that she typically tried to avoid anxiety and other emotions at all costs.
Beginning around session 8, Kendra began to express more clarity regarding her emotions. For example, Kendra noticed early anxiety cues when she arrived at school and saw her principal, who was scheduled to observe Kendra’s classroom later than afternoon. Kendra noticed a sudden increase in her heart rate and she was able to apply a breathing exercise in the moment. However, she also reported a new perspective on her anxiety that is consistent with a mindful stance. Kendra acknowledged that it was to be expected that she would be anxious about being observed and evaluated by her principal and she was able to greet him rather than responding to her anxiety with avoidance. During this phase of therapy, Kendra also began to describe her internal experiences from a decentered perspective. For example, in session 10, Kendra commented that she recognized her thoughts and emotions are not constant, that they come and go, especially when she applied relaxation in response to the early cues.
This shift in Kendra’ description of how she was responding in different situations during session appears to correspond with the large increases in self-reported scores on mindfulness and decentering measures that she reported from session 4 to 12. During the same period, her DASS-stress scores began to decrease, so that by session 12, her score was within one standard deviation of the norm. Although Kendra demonstrated changes in acceptance towards her emotions in her description of different events, her AAQ scores only showed a modest change from session 4 to 12.
By the end of therapy, Kendra stated that while she still occasionally experienced anxiety at work, it was considerably less frequent. She no longer dreaded going to work each morning and found it easier to engage with her students in the classroom. She also denied any significant difficulties with muscle tension, restlessness, irritability, or fatigue during her post-treatment interview. As can be seen in Table 2, her anxiety and worry were significantly reduced at the post-treatment and 12 month follow-up assessments and the independent assessor rated her GAD as subclinical. Interestingly, several of her comorbid diagnoses, particularly panic and social anxiety, also decreased to subclinical levels. Likewise, her mindfulness and decentering scores were approximately two and three standard deviations above average by the end of therapy. These changes were maintained at a 12-month follow-up assessment.
Discussion
The three cases presented here demonstrate how AR involving early cue detection, progressive muscle relaxation, and applied relaxation may lead to changes in mindfulness, decentering, and acceptance. These three cases were specifically selected because they most clearly demonstrated the kinds of changes that we have been routinely seeing in our AR clients. Therefore, additional empirical research, such as a study involving the administrations of measures of symptoms and potential mediators at multiple time points throughout therapy allowing for a prospective mediation analysis, is needed. However, within the context of this treatment study, where therapists are specifically instructed not to include elements of acceptance or mindfulness based therapy (i.e., no mindfulness exercises, instructions about decentering, or mention of acceptance and experiential avoidance) and adherence to this is measured, we still observed clients making these types of changes.
All three of these clients explicitly described how AR led them to be more accepting, and less experientially avoidant of their anxiety and other internal experiences. Perhaps the most obvious was Kendra who noted that before treatment began she attempted to do everything possible to avoid and discount feelings of anxiety before therapy began. For her, the imaginal exercises aimed at helping her to notice signs of anxiety were difficult because she did not want to experience discomfort. However, over therapy her willingness to engage in the exercises increased and by the end of therapy she was more willing to encounter uncomfortable situations. Similarly, Julia explicitly talked with her therapist about how much more accepting of her emotional experiences she became over the course of therapy. Specifically, she described how in the midst of grieving for the loss of her father she could accept that losing someone was part of the human experience. While experiential avoidance is not typically discussed as one of the targets of AR, it appears that clients in this treatment may become more accepting and less avoidant of their internal experiences. It is possible that the early cue detection and relaxation exercises contributed to these changes; however, larger scale, prospective studies are needed before any conclusions about how AR may contribute to these changes can be made.
While previous research has shown that individuals diagnosed with GAD have lower mindfulness and higher experiential avoidance scores than individuals without a diagnosis of GAD, in this study Julia and Doug began therapy with mindfulness scores close to the normative level and Julia and Kendra began therapy with experiential avoidance scores near the norm. This may indicate that these clients were more prone to be mindful or accepting of their internal experiences, highlighting the need to further examine these variables in a broader sample of individuals diagnosed with GAD, with specific attention to both mediators and moderators of change.
Although AR appears to have increased mindfulness and decentering and decreased experiential avoidance in these three individual cases, it is not possible in this design to determine whether any of these constructs are the central mechanism of change. Additionally, there are other potential mechanisms of change (e.g., new learning through exposure, reduction in physical tension) not assessed here that could also be responsible. It is possible that therapists in this study were subtly encouraging changes in the constructs of interest, since all therapists were also simultaneously treating other clients with an acceptance-based behavioral approach. However, several precautions were put in place to reduce the likelihood that this would occur. For example, the therapy manual and client handouts were written with a more goal-oriented approach of AR (“the purpose of these relaxation skills is to learn to relax your body”) as opposed to the more process-oriented, mindfulness-consistent approaches to relaxation that focus solely on awareness of sensations rather than also on outcome. Likewise, adherence raters and supervisors monitored sessions for any mention of acceptance, mindfulness, or experiential avoidance on the part of the therapists. Research is needed to examine whether the same changes occur when cases are treated by therapists with no experience with acceptance and mindfulness-based approaches. It is also possible that the repeated administration of mindfulness and acceptance-based measures may have subtly encouraged the clients to notice and talk about these changes. However, regardless of these influences, it appears as though changes in acceptance, mindfulness, and decentering may be common mechanisms of change that may be influential even when they are not directly targeted in treatment.
If this finding is replicated in large scale, systematic studies, then it may be worth training AR therapists to directly encourage mindfulness, decentering, and acceptance in their clients. While AR may already lead to these changes, drawing more attention to these changes and encouraging them may further enhance the efficacy of AR. For example, responding to Kendra’s resistance to engage in the imaginal early cue exercises by explaining the role of experiential avoidance in maintaining anxiety may have enhanced her willingness to engage in these exercises. While this would need to be empirically investigated, it is possible that helping clients to change their relationship with internal experiences and increase acceptance, mindfulness, and decentering may help to alleviate symptoms of anxiety regardless of the treatment techniques used.
Table 1.
Applied Relaxation Session Content
| Content | Session | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
| Anxiety Psychoeducation | * | * | * | |||||||||||||
| Treatment Rationale | * | |||||||||||||||
| Anxiety Monitoring | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * |
| Early Signs of Anxiety | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * |
| Diaphragmatic Breathing | * | * | * | |||||||||||||
| 16-group PMR- First Half | * | |||||||||||||||
| 16-group PMR | * | * | ||||||||||||||
| 7-group PMR | * | * | ||||||||||||||
| 4-group PMR | * | |||||||||||||||
| Release only PMR | * | |||||||||||||||
| Cue-Controlled PMR | * | |||||||||||||||
| Differential Relaxation- I | * | |||||||||||||||
| Differential Relaxation- II | * | |||||||||||||||
| Rapid Relaxation | * | * | * | * | * | |||||||||||
| Relapse Prevention | * | * | ||||||||||||||
Note: All sessions involve homework review from the previous session and the assignment of homework. PMR = Progressive Muscle Relaxation.
Acknowledgments
Disclosure Statements
This work was supported by National Institute of Mental Health Grant No. MH074589 awarded to the fourth and fifth authors and MH085060 awarded to the first author. The authors thank the clients we have worked with for sharing their experience and wisdom with us.
Contributor Information
Sarah A. Hayes-Skelton, University of Massachusetts Boston
Aisha Usmani, Massachusetts General Hospital/Harvard Medical School.
Jonathan K. Lee, Suffolk University
Lizabeth Roemer, University of Massachusetts Boston.
Susan M. Orsillo, Suffolk University
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. text rev. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Arch JJ, Craske MG. Acceptance and commitment therapy and cognitive behavioral therapy for anxiety disorders: Different treatments, similar mechanisms? Clinical Psychology: Science and Practice. 2008;15:263–279. [Google Scholar]
- Arntz A. Cognitive therapy versus applied relaxation as treatment of generalized anxiety disorder. Behaviour Research and Therapy. 2003;41:633–646. doi: 10.1016/s0005-7967(02)00045-1. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Walsh E, Duggan D, Williams JMG. Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment. 2008;15:329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Bernstein DA, Borkovec TD, Hazlett-Stevens H. New directions in progressive relaxation training: A guidebook for helping professionals. Westport, CT: Praeger Publishers; 2000. [Google Scholar]
- Borkovec TD. Applied relaxation and cognitive therapy for pathological worry and generalized anxiety disorder. In: Davey GCL, Wells A, editors. Worry and its psychological disorders: Theory, assessment, and treatment. Hoboken, NJ: Wiley Publishing; 2006. [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1993;61:611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Sharpless B. Generalized anxiety disorder: Bringing cognitive-behavioral therapy into the valued present. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. New York: Guilford; 2004. pp. 209–242. [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour Research and Therapy. 1992;30:33–37. doi: 10.1016/0005-7967(92)90093-v. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy. 1997;35:79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- Butler G, Fennell M, Robson P, Gelder M. Comparison of behavior therapy and cognitive behavior therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1991;59(1):167–175. doi: 10.1037//0022-006x.59.1.167. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Ollendick TH. Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- Conrad A, Roth WT. Muscle relaxation therapy for anxiety disorders: It works but how? Journal of Anxiety Disorders. 2007;21:243–264. doi: 10.1016/j.janxdis.2006.08.001. [DOI] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. Albany NY: Graywind Publications; 1994. [Google Scholar]
- Fresco D, Moore M, Van Dulman M, Segal Z, Ma S, Teasdale J, Williams J. Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behavior Therapy. 2007;38:234–246. doi: 10.1016/j.beth.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Fresco D, Segal Z, Buis T, Kennedy S. Relationship of post treatment decentering and cognitive reactivity to relapse in major depression. Journal of Consulting and Clinical Psychology. 2007;75:447–455. doi: 10.1037/0022-006X.75.3.447. [DOI] [PubMed] [Google Scholar]
- Frisch MB, Cornwell J, Villanueva M, Retzlaff PJ. Clinical validation of the Quality of Life Inventory: A measure of life satisfaction of use in treatment planning and outcome assessment. Psychological Assessment. 1992;4:92–101. [Google Scholar]
- Gellhorn E, Kiely WF. Mystical states of consciousness: Neurophysiological and clinical aspects. Journal of Nervous and Mental Disease. 1972;154:399–405. doi: 10.1097/00005053-197206000-00002. [DOI] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG, Bissett RT, Pistorello J, Toarmino D, Polusny MA, Dykstra TA, Batten SV, Bergan J, Stewart SH, Zvolensky MJ, Eifert GH, Bond FW, Forsyth JP, Karekla M, McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54:553–578. [Google Scholar]
- Hayes-Skelton SA, Roemer L, Orsillo SM. AR therapist manual for GAD treatment study. 2011 Unpublished manuscript. [Google Scholar]
- Hoffman DL, Dukes EM, Wittchen H-U. Human and economic burden of generalized anxiety disorder. Depression and Anxiety. 2008;25(1):72–90. doi: 10.1002/da.20257. [DOI] [PubMed] [Google Scholar]
- Jacobson E. You must relax. New York: McGraw-Hill; 1934. [Google Scholar]
- Jacobson E. Progressive relaxation. Oxford, England: University of Chicago Press; 1938. [Google Scholar]
- Kabat-Zinn J. Coming to our senses: Healing ourselves and the world through mindfulness. New York: Hyperion; 2005. [Google Scholar]
- Kessler RC, Keller MB, Wittchen H-U. The epidemiology of generalized anxiety disorder. Psychiatric Clinics of North America. 2001;24(1):19–39. doi: 10.1016/s0193-953x(05)70204-5. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Walters EE, Wittchen H-U. Epidemiology. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorder: Advances in research and practice. New York: Guildford Press; 2004. [Google Scholar]
- Lee J, Orsillo SM, Roemer L, Allen L. Distress and avoidance in generalized anxiety disorder: Exploring the relationships with intolerance of uncertainty and worry. Cognitive Behaviour Therapy. 2010;39:126–136. doi: 10.1080/16506070902966918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney: The Psychology Foundation of Australia; 1995. [Google Scholar]
- Mennin DS. Emotion regulation therapy for generalized anxiety disorder. Clinical Psychology and Psychotherapy. 2004;11:17–29. [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Molina S, Borkovec TD. The Penn State Worry Questionnaire: Psychometric properties and associated characteristics. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment and treatment. Oxford, England: John Wiley & Sons; 1994. [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Nordberg SS. An open trail of integrative therapy for generalized anxiety disorder. Psychotherapy: Theory, Research, Practice, Training. Special Issue: New treatments in psychotherapy. 2008;45:135–147. doi: 10.1037/0033-3204.45.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsillo SM, Roemer L, Block Lerner J, Tull MT. Acceptance, mindfulness, and cognitive behavioral therapy: Comparisons, contrasts and application to anxiety. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and acceptance: Expanding the cognitive-behavior tradition. New York: Guilford Press; 2004. [Google Scholar]
- Öst L-G. Applied relaxation: Description of a coping technique and review of controlled studies. Behaviour Research and Therapy. 1987;25(5):397–409. doi: 10.1016/0005-7967(87)90017-9. [DOI] [PubMed] [Google Scholar]
- Öst L-G. Applied relaxation vs progressive relaxation in the treatment of panic disorder. Behaviour Research and Therapy. 1988;26(1):13–22. doi: 10.1016/0005-7967(88)90029-0. [DOI] [PubMed] [Google Scholar]
- Öst L-G. Applied relaxation: Manual for a behavioral coping technique. Unpublished manuscript. [Google Scholar]
- Öst L-G, Breitholtz E. Applied relaxation vs. cognitive therapy in the treatment of generalized anxiety disorder. Behaviour Research and Therapy. 2000;38:777–790. doi: 10.1016/s0005-7967(99)00095-9. [DOI] [PubMed] [Google Scholar]
- Robichaud M, Dugas MJ. A cognitive-behavioral treatment targeting intolerance of uncertainty. In: Davey G, Wells A, editors. Worry and its psychological disorders: Theory, assessment and treatment. West Sussex: Wiley; 2006. pp. 289–304. [Google Scholar]
- Roemer L, Lee JK, Salters-Pedneault K, Erisman SM, Orsillo SM, Mennin D. Mindfulness and emotion regulation difficulties in generalized anxiety disorder: Preliminary evidence for independent and overlapping contributions. Behavior Therapy. 2009;40:142–154. doi: 10.1016/j.beth.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM. Mindfulness- and acceptance-based behavioral therapies in practice. New York, NY: Guildford Press; 2009. [Google Scholar]
- Safran JD, Segal ZV. Interpersonal process in cognitive therapy. New York: Basic Books; 1990. [Google Scholar]
- Salters-Pedneault K, Tull MT, Roemer L. The role of avoidance of emotional material in the anxiety disorders. Applied and Preventive Psychology. 2004;11:95–114. [Google Scholar]
- Shear MK, Vander Bilt J, Rucci P, Endicott J, Lydiard B, Otto MW, Pollack MH, Chandler L, Williams J, Ali A, Frank DM. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depression and Anxiety. 2001;13:166–178. [PubMed] [Google Scholar]
- Siev J, Chambless DL. Specificity of treatment effects: Cognitive therapy and relaxation for generalized anxiety and panic disorders. Journal of Consulting and Clinical Psychology. 2007;75:513–522. doi: 10.1037/0022-006X.75.4.513. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Warshaw MG, Massion AO, Keller MB. Phenomenology and course of generalised anxiety disorder. British Journal of Psychiatry. 1996;168:308–313. doi: 10.1192/bjp.168.3.308. [DOI] [PubMed] [Google Scholar]
- Wells A. Cognition about cognition: Metacognitive therapy and change in generalized anxiety disorder and social phobia. Cognitive and Behavioral Practice. 2007;14:18–25. [Google Scholar]