Abstract
BACKGROUND
Anxiety disorders are among the most common psychiatric disorders; meditative therapies are frequently sought by patients with anxiety as a complementary therapy. Although multiple reviews exist on the general health benefits of meditation, no review has been focused on the efficacy of meditation for anxiety specifically.
METHODS
Major medical databases were searched thoroughly with keywords related to various types of meditation AND anxiety. Over 1000 abstracts were screened, and 200+ full articles were reviewed. Only RCTs were included. The Boutron (2005) checklist to evaluate a report of a non-pharmaceutical trial (CLEAR-NPT) was used to assess study quality; 90% authors were contacted for additional information. Review Manager 5 was used for meta-analysis.
RESULTS
A total of 36 RCTs were included in the meta-analysis (2,466 observations). Most RCTs were conducted among patients with anxiety as a secondary concern. The study quality ranged from 0.3 to 1.0 on the 0.0–1.0 scale (mean = 0.72). Standardized mean difference (SMD) was −0.52 in comparison with waiting-list control (p < .001; 25 RCTs), −0.59 in comparison with attention control (p < .001; 7 RCTs), and −0.27 in comparison with alternative treatments (p < 0.01; 10 RCTs). 25 studies reported statistically superior outcomes in the meditation group compared to control. No adverse effects were reported.
CONCLUSIONS
This review demonstrates some efficacy of meditative therapies in reducing anxiety symptoms, which has important clinical implications for applying meditative techniques in treating anxiety. However, most studies measured only improvement in anxiety symptoms, but not anxiety disorders as clinically diagnosed.
Keywords: meditation, meditative therapies, anxiety, systematic review, meta-analysis
BACKGROUND
Description of the condition
In a given year, approximately 40 million American adults meet criteria for an anxiety disorder [1]. Although pharmacological approaches and more traditional forms of psychotherapy have strong empirical support for reducing anxiety, many patients are turning to meditation as an alternative approach to reduce stress and anxiety for a few key reasons. Meditation offers a therapeutic and often spiritual approach that avoids side effects of medications, the stigma of psychiatric treatments, as well as barriers related to issues of cost and accessibility [2–6].
Meditation: A definition and an overview of its benefits
Meditation can be defined to include any of a family of practices in which the practitioner trains an individual’s consciousness or calms his/her mind in order to realize some benefit or achieve inner peace or harmony. Despite lack of consensus in the scientific literature on a definition of meditation, most researchers agree that meditation implies a form of mental training that requires either stilling or emptying the mind, and its goal is to achieve a state of “detached observation” or “restful alertness” [7]. The foundation of meditation practice is rooted in the principles of “self-observation of immediate psychic activity, training one’s level of awareness, and cultivating an attitude of acceptance of process rather than content.” [6]
From the perspective of traditional Chinese medicine (TCM), all forms of meditation are under the general term “qigong” for mind-body integrative exercises. Qigong is defined as “the skill of mind-body exercises that integrate body, breath and mind adjustments into one” [8], which address both psychological and physiological aspects of health. Although Qigong has both dynamic (movement) and static forms, the meditative state – body, breath and mind into one – is common among all of them. Given a lack of consensus in Western psychology about the definition of meditation and exactly what techniques it includes, in this review we use the established definition of meditative therapies in Chinese medicine. Specifically, we include all mind-body exercises, both dynamic (or moving) form and static (still) form, which are aimed to integrate breath-body-mind adjustments into one. As a result, this includes all meditations, yoga, mindfulness training, Transcendental Meditation (TM), qigong, tai chi (or Taiji), and even guided imagery, as guided imagery is an ancient technique in meditation practice [8].
Numerous reviews have been conducted evaluating the physical and psychological effects of meditation practice on health [e.g. 6, 9–12]. The majority of these reviews illustrated a positive trend and/or health benefits, although their results were often inconclusive due to research design and sample limitations, More recently, Ospina et al. [6] conducted a large and thorough systematic review on meditation practices for health (from 813 predominantly peer-reviewed studies). They identified five broad categories of meditation practice (Mantra meditation, Mindfulness meditation, Yoga, Qigong, and Tai Chi) and reviewed the clinical evidence for these practices for three important and common health-related conditions: hypertension, other cardiovascular diseases, and substance abuse. Their meta-analyses of 55 studies indicated that meditation practices suggested some clinical changes and possibly positive outcomes in healthy participants, but no conclusions were able to be drawn from these studies on the clear clinical benefits of meditation.
Despite the noted beneficial trend of meditation practices according to the Ospina’s review [6], the effect of meditation on anxiety was only relevant to those with a cardiovascular condition. Additionally, the other reviews focused on examining the effects of meditation on stress and related symptoms [13,14] suggested a positive stress management function of meditation practice. However, these studies have not examined effects on clinically relevant anxiety symptoms per se, or anxiety disorders more specifically. Examining the effect of meditative therapies on anxiety outcomes has important clinical implications, particularly in considering how we can improve anxiety outcomes using an approach that may improve access and tolerability of treatment in a range of clinical settings.
Conceptual framework of meditation effects on anxiety
In conceptualizing meditation’s impact on anxiety, it is important to consider this relationship in light of existing biological, behavioral, and cognitive frameworks of anxiety. For instance, prominent biological theories such as the false suffocation alarm [15] and hyperventilation [16] theories focus on the role of respiratory abnormalities in anxiety. From a learning perspective, anxiety and fear are a product of classical conditioning where a previously novel and innocuous stimulus has come to elicit an aversive, conditioned response due to the previous pairing of that stimulus with an anxiety/fear-relevant unconditioned stimulus. Finally, from a cognitive perspective, people with anxiety disorders may be prone to overestimate danger and its potential consequences (e.g., Clark, 1999 [17]).
Considering the combined impact of biological, behavioral, and cognitive vulnerabilities to anxiety, there are several clear ways in which the role of meditation in the management of anxiety are quite clear. Addressing biological vulnerability, meditation and related breath training can reverse abnormalities and alter the anxiogenic effects of biological challenges [18, 19]. Indeed a rich literature on abdominal breathing, commonly used in meditation, has been used as a tool for coping directly with panic attacks [20, 21]. Moreover, at a neurobiological level, meditation has consistently been shown to reduce cortisol and catecholamine level (such as epinephrine and norepinephrine) that may otherwise trigger biologically-based anxiety responses [22, 23, 24]. In line with Wolpe’s work on reciprocal inhibition (i..e., inhibiting anxiety by conditioning a feeling or response that is not compatible with the feeling of anxiety in its place; [25]), meditation may address behavioral vulnerability when conducted in the context of the conditioned stimulus. In this way, meditation is then serving to create a newly conditioned response, thereby resulting in the “extinction” of the anxious/fear-related conditioned response. Finally, meditation may address cognitive vulnerability by using meditative skills to help the practitioner remain “detached” yet not avoidant to address the cognitive misattributions accompanying anxiety as a substitute for avoidance. In other words, meditation can serve as a training to control the mind as a means to reduce anxiety, as well as to develop a helpful coping mechanism to facilitate a calm and non-destructive response to stress and strain. Interestingly, these three components of a conceptual framework of anxiety—biological, behavioral, and cognitive— correspond to the three adjustments or regulations used in defining the meditative therapies: the adjustments of breathing, body, and mind.
Limitations of previous reviews
Despite the absence of a systematic review focusing on anxiety, there are numerous reports suggesting the potential benefits of meditation in reducing anxiety [26–28]. Studies have examined the effects of meditative therapies on both stress and anxiety, primarily mindfulness meditation [29–32] and yoga [33–35], which largely have demonstrated positive outcomes on anxiety. However, to date, efforts to synthesize evidence pertaining to the efficacy of meditative therapies on anxiety have been very limited. This next step in synthesizing the literature is necessary to inform our clinical understanding of which aspects of meditative therapies are most efficacious for anxiety specifically.
Existing efforts to examine the efficacy of meditation for anxiety specifically have been scarce and limited in a few distinct ways. A Cochrane review on “meditation therapy for anxiety disorders” [10] identified only two eligible randomized controlled trials (RCT), primarily because many studies have not focused on meditation for treating clinically relevant anxiety symptoms and/or disorders specifically. Indeed, an inspection of the literature reveals that most studies on meditative therapies, especially the high quality RCTs, include anxiety as a symptom or one of the multiple outcomes, but not as a primary outcome, which may explain their omission from existing systematic reviews. Further, the small number of studies included in previous reviews (e.g., of Krisanaprakornkit [10]) did not permit any conclusions to be drawn, suggesting a systematic review with more inclusive meditation and anxiety symptoms is needed on this topic.
In addition, most reviews to date focus on one type of meditation only, such as yoga [36], Mindfulness meditation [26,37–38], or Tai chi [39]. These reviews typically included only a small number of qualified studies, often with low quality according to traditional review criteria, which also do not permit conclusions to be drawn. Finally, the majority of existing reviews have applied evaluation criteria based on pharmaceutical RCTs that tended to underestimate the actual quality of these studies, since some of these traditional criteria for quality assessment may not apply to the study of meditative therapies (e.g., blindness, typically used in pharmaceutical trials, may not be applicable to meditation trials, in which blindness of the participants or provider cannot be assured).
Importance of the current review
Conducting a more thorough systematic review of the meditative therapies for reducing anxiety symptoms is an important next step, given that many meditative approaches overlap in terms of their effects, and many similar mind-body practices that we term “meditative therapies” may also have an effect on anxiety, but their efficacy has not yet been fully reviewed. The current review aimed to investigate all therapies under the rubric of “meditative,” which will all be called Qigong or meditative therapy in China (such as yoga, mindfulness meditation, Transcendental Meditation, qigong, tai chi or Taiji, and guided imagery)† to examine their effects on anxiety using more appropriate criteria for quality assessment. The objective of this review was to systematically investigate the evidence on the overall efficacy, effect size, and safety of all meditative therapies for reducing anxiety symptoms across various types of participants and health conditions in RCTs to guide clinicians and future research in this area.
METHODS
Literature Research
A thorough literature search was independently carried out by the reviewers through December 2010 using the following databases: Pubmed, PsychINFO, Embase, Cochrane Central Register of Controlled Trials, and Qigong database (by Qigong Institute; [40]). The keywords used in the search included a combination of diagnostic or anxiety measures (such as anxiety, anxious, phobic, panic, obsessive-compulsive disorder or OCD, social phobia, PTSD, stress disorder, neurosis or neurotic) and a meditation-related intervention (such as meditation, mindfulness, MBSR, meditative, Vipassana, Zen, yoga, yogic, pranayama, Kriya, Qigong, chi kung, Tai Chi, Taiji, Kundalini, Reiki, Prana, TM and guided imagery). Previously published reviews of meditation for stress and other health issues were also carefully screened to pick up missed clinical studies with anxiety as secondary outcomes.
Study Eligibility
Two reviewers screened the abstracts of all publications obtained by the search strategies. Studies meeting the following inclusion criteria were selected for further review: 1) prospective RCTs with meditative technique used as intervention; 2) anxiety or related diagnosis was one of the outcomes with a psychometric measure; 3) total number of randomized subjects greater than 20 (N ≥ 20) with a control group either inactive (waiting-list) or active (attention or alternative active treatment); 4) anxiety level data presented both at baseline and after intervention or training.
Exclusion criteria included the following: 1) qualitative report; 2) literature review; 3) case reports or trials with fewer than 20 subjects; 4) combined measure of anxiety and stress, or anxiety and depression (i.e. no psychometric measure for anxiety by itself); 5) children or adolescent population.
Data Coding
Of those papers that qualified for the review after the initial screening, the full articles were obtained and assessed for their relevance based on the pre-planned criteria for inclusion. Data were independently extracted by two reviewers using predesigned data collection form. Any disagreements were discussed with a third reviewer for final data coding.
Study quality was assessed using the modified Boutron et al. checklist [41]to evaluate a report of a non-pharmaceutical trial (CLEAR-NPT), which includes a checklist of 10 specific quality assessment criteria. This was developed using the Delphi technique with experienced researchers assessing report quality of NPT. We chose this checklist instead of the traditional Jadad Scale [42] because it offers more comprehensive quality details than Jadad (10 assessment criteria instead of 5) and offers an alternative when blinding is not possible for participants or clinicians in the trial. We added one criterion to the CLEAR-NPT –“were the treatment and control groups comparable at entry?” (See appendix Table for a complete list). Because some criteria may not apply to the specific study (e.g., when no providers were present for some meditation study with waiting-list control), all studies could not be evaluated equally on the 11 point scale. Therefore, we applied a quality index (range 0.0 to 1.0), dividing number of met criteria by total number of applied criteria. In the context of this metric, a score less than 0.6 was considered low quality, a score between 0.6 and 0.8 was considered acceptable, and a score greater than 0.80 was considered good quality.
Appendix Table. Meditation for Anxiety Review - Quality Assessment.
[Adapted from Boutron et al (2005)30 CLEAR-NPT]
Checklist to evaluate a report of a nonpharmacological trial (CLEAR NPT)
| Criterion | Yes | No | Unclear | |
|---|---|---|---|---|
| 1 | Was the generation of allocation sequences (group assignment procedure) adequate? | |||
| 2 | Was the treatment allocation concealed? | |||
| 3 | Were details of the intervention administered to each group stated or made available? | |||
| 4 | Were care providers experience or skill in each arm (group) appropriate? | |||
| 5 | Was participant adherence or compliance assessed quantitatively? | |||
| 6 | Were participants adequately blinded?
|
|||
| 6.1.1 | Were other treatments and care (i.e co-interventions) the same in each randomized group? | |||
| 6.1.2 | Were withdrawals and lost-to-follow-up the same in each randomized group? | |||
| 7 | Were care providers for the participants adequately blinded?
|
|||
| 7.1.1 | Were all other treatments and care (co-interventions) the same in each randomized group? | |||
| 7.1.2 | Were withdrawals and lost-to-follow up the same in each randomized group? | |||
| 8 | Were outcome assessors adequately blinded to assess the primary outcomes? | |||
| 8.1 | If outcome assessors were not adequately blinded, were specific methods used to avoid ascertainment bias (systematic differences in outcome assessment)? | |||
| 9 | Was the follow-up schedule the same in each group? (parallel design) | |||
| 10 | Were the treatment and control group comparable at entry? (Any significant differences at baseline?) | |||
| 11 | Were the main outcomes analyzed according to the intention-to-treat principle? | |||
| Total | Total Scores (number of Yes) |
Quality score = total number of Yes/total number of applied criteria
Most studies did not provide the full information needed for the quality assessment (e.g., detailed randomization procedure, allocation concealment, care-providers’ experience for each arm, or necessary quantitative data like means and standard deviations). As a result, we attempted to contact the authors to obtain additional information when necessary to provide a more objective assessment of study quality. After 3 unsuccessful contact attempts, or if the author could no longer access the pertinent data, we considered this information “unclear” and ranked it as “no” for the quality assessments of these studies.
Data Analysis
Quantitative data that could be aggregated were entered into the Cochrane Collaborative Review Manager Software (RevMan v. 5.1) [43] and analyzed by RevMan analysis, one of the most popular and most authoritative literature review softwares. Since the entire outcome measures in the reviewed studies were continuous scales, the standardized mean differences (SMD) and their 95% confidence intervals were calculated using a random effect model built in RevMan 5.1. SMD expressed the size of the intervention effect in each study relative to the variability observed in that study. Outcomes were analyzed on the changes from baseline to the endpoint of the treatment, including only the subjects with both a baseline and a final (post-intervention) assessment. The outcomes at the later follow-up were not used for meta-analysis unless they reported a larger effect than the endpoint of treatment. When multiple anxiety outcomes were present in the same study, such state and trait anxiety scales, we chose the change of SMD in the trait anxiety scale (more stable) rather than state anxiety (less stable) to be included in the meta-analysis. When standard deviation of the mean difference was not available from the paper or from the authors, the baseline standard deviation (usually larger than that of after-intervention) was used to avoid an over-estimation of the SMD.
Given the fact that the SMD was highly correlated with the type of control in the study design, we decided to conduct the meta-analysis separately by three types of control conditions (i.e., waiting list or treatment as usual, attention/education control, and alternative active therapy) so that we could provide greater details regarding the accumulated findings and level of evidence in different control conditions. We evaluated heterogeneity using the I2 statistic [43], which indicates the proportion of variability across trials not explained by chance alone. Roughly, I2 values of 50% or greater represent substantial heterogeneity, while I2 values of 40% or less is considered no problem in heterogeneity [43]. We also checked for heterogeneity by visual examination of forest plots. When substantial heterogeneity was observed, we attempted to determine potential reasons for it by removing the study with largest effect on overall SMD to examine the magnitude of the effect from that study. When possible, a sensitivity analysis was performed separately for higher quality studies. Studies in which means and standard deviations were not reported and could not be obtained from the authors were not entered into the meta-analysis and were reviewed only narratively.
RESULTS
Search Results
The original search identified more than 1000 abstracts from various databases. After careful screening of these abstracts, 201 full-text articles were obtained for further assessment for eligibility. Of these articles, 155 were excluded for reasons described in Figure 1.
Figure 1.
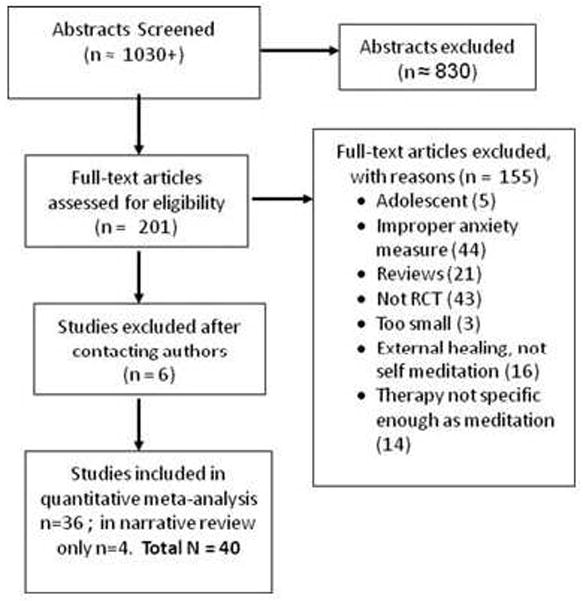
PRISMA Flow-chat of Meditation for Anxiety Review
After inclusion and exclusion criteria were applied to the remaining 46 studies with additional information from the authors as available, 6 trials were excluded -- 2 studies were based on inappropriate randomization procedures [44–45]; 1 study had an incompatible anxiety measure [46]; 2 studies were not true RCTs [31,47], and 1 study was a comparison between Qigong and Qigong plus the rehabilitation [48]. A summary flow chart with all numbers of included and excluded studies is presented in Figure 1.
Characteristics of Included Studies
Table 1 presents the summary characteristics of the included studies on various meditative therapies used to treat anxiety symptoms. Among the 40 reviewed RCTs, 14 studies applied mindfulness meditation (MM) or mindfulness-based stress reduction (MBSR), 10 used yoga, 3 taiji, 4 qigong, 3 TM, and 6 used guided imagery. Sixteen of the studies (mostly MM) were conducted in the U.S., 6 in India, 3 in other Asian countries, 7 in European countries (Sweden, UK & Spain), 2 in Brazil, 1 in Israel, 2 in Canada and 2 in Australia. A majority of the studies (29) were conducted among patients who had health problems other than anxiety disorders but included anxiety symptoms as one of the outcome measures. Eight studies were conducted among healthy subjects, and 4 studies were conducted among patients with anxiety disorders or had anxiety as the primary outcome. The most frequently used anxiety measures were the Spielberg State-Trait Anxiety Inventory (STAI) [49], which was used in 20 studies, and the Hospital Anxiety and Depression Scale (HADS) [50], which was used in 7 studies.
Table 1.
Summary Characteristics of the Reviewed RCT Studies
| Study ID | Ns | Age | % female | Country | Type meditation | Ss | Type of control | Anxiety measure | Grp or Ind | Home- work | Duration (wks) | # Sessions | Ret rate % | CLEAR score | Main Findings on Anxiety (anx) | Notes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Banerjee et al. (2007) 77 | 68 | 44 | 85 | India | Yoga | 2 | ATT | HADS | Both | Y | 6 | 6 | 85 | 0.55 | The yoga gp had a sig decrease in anx after 6 weeks; the control gp did not. The difference in changes b/n gps was significant (p<.001). | Breast cancer |
| Branstrom et al. (2010) 13 | 71 | 52 | 99% | Sweden | MM | 2 | WL | HADS | Grp | Y | 8 | 8 | 83 | 0.89 | There was no sig difference of change in anxiety b/n MM gp and control. | Cancer |
| Carson et al. (2010) 51 | 53 | 54 | 100 | USA | Yoga | 2 | WL | FIQR | Ind | Y | 8 | 8 | 82 | 0.82 | Yoga gp had a sig greater decrease in anx as compared to WL control (p=.0407, ES=1.28) | Fibromyalgia |
| Davidson et al. 2003 52 | 41 | 36 | 71 | USA | MBSR | 1 | WL | STAI | Both | Y | 8 | 8 | 100 | 0.64 | More decrease of anx in MBSR gp as compared to control (p < 0.05) | Healthy |
| Foley et al. (2010) 53 | 115 | 55 | 77 | Australia | MBCT | 2 | WL | HAM-A | Both | Y | 10 | 8 | 93 | 1.0 | The MBCT gp had sig more improvement in anx as compared to WL (ES= .59 for pre-post) | Cancer |
| Frye et al. (2007) 54 | 84 | 69 | 64 | USA | Tai Chi | 1 | WL & AA | STAI | Grp | N | 12 | 36 | 82 | 0.64 | Both exercise and Tai Chi gps demonstrated decreased anx over 12 weeks (p<.01) but there was no sig difference b/n gps | Elderly population |
| Gonzales et al. (2010) 55 | 44 | 34 | 40 | USA | GI | 2 | WL | VAS | Ind | N | 1 day | 1 | 100 | 0.89 | Significant more decrease in anx in GI gp after one session (p=.002) as compared to WL control | Head/neck surgery |
| Gross et al. (2010) 26 | 150 | 53 | 45 | USA | MBSR | 2 | ATT | STAI | Both | Y | 26 | 9 | 92 | 0.82 | MM gp had more decrease in anx (p<.001) at 8 wks as compared to control. Tx effects were sustained at 1 year follow-up (p<.01;ES=.56). | Solid organ transplant |
| Gross et al. (2011) 84 | 30 | 50 | 73 | USA | MBSR | 2 | AA | STAI | Both | Y | 8 | 9 | 90 | 0.9 | Anxiety scores decreased in both gps but no sig difference b/n gps | Chronic insomnia |
| John et al. (2007) 78 | 72 | 34 | 68 | India | Yoga | 2 | ATT | HADS | Both | Y | 12 | 72 | 90 | 0.64 | The yoga gp demonstrated a sig drop in anx (p=.001) while an increase of anx in control gp. | Migraine without aura |
| Kabat-Zinn et al. (1998) 56 | 37 | 43 | 54 | USA (US) | MBSR | 2 | WL | STAI | Ind | N | 13 | 13 | 62 | 0.82 | There was no significant difference b/n the mindfulness and control gps on STAI. | Psoriasis |
| Kondwani et al. (2005) 79 | 34 | 50 | 56 | USA | TM | 2 | ATT | MHI | Both | Y | 52 | 19 | 81 | 0.8 | TM gp had a decrease in anx over time (p=.02) & a sig more decrease in anx as compared to the control (p=.03) | Hypertension |
| Kozasa et al (2008) 57 | 22 | 43 | 91 | Brazil | Yoga | 3 | WL | STAI | Grp | Y | 4 | 2 | unc | 0.30* | Yoga group showed more sig decrease in anxiety after treatment (sig level not available) | anxiety disorders |
| Lengacher et al. (2009) 58 | 84 | 58 | 100 | USA | MBSR | 2 | WL | STAI | Both | Y | 6 | 6 | 98 | 0.91 | Mindfulness gp had significantly more decreased anx compared to the control gp (state anx p=.03, trait anx p=.004) | Breast Cancer |
| Leon-Pizarro (2007) 59 | 66 | 24–82 | 100 | Spain | GI | 3 | WL | HADS | Ind | Y | 4 | 3 | 70 | 0.55* | GI gp showed a significant more decrease in anx (p=0.008) as compared to control. | Gyn/breast brachy-therapy |
| Li et al. (2002) 60 | 86 | 32 | 0 | China | Qigong | 2 | WL/AA | HAM-A | Grp | N | 1.5 | daily | 100 | 0.7 | Qigong (p<.001) and medicine (p<.05) gps had sig greater decrease in anx as compared to control. Qigong gp had more reduction than medicine gp (p<.001). | Heroin addicts |
| Ljotsson et al. (2010) 80 | 85 | 35 | 84 | Sweden | MBSR | 2 | ATT | VSI | Ind | Y | 10 | daily | 95 | 0.71 | Mindfulness gp had a significant more decrease in gastrointestinal-related anx (p<.001, ES 0.64) as compared to the WL | IBS |
| Malathi & Damodaran (1999) 61 | 50 | 18.5 | unc | India | Yoga | 1 | WL | STAI | Grp | N | 12 | 36 | 100 | 0.45* | On the day of the exam and after yoga session, there was a more sig reduction in anx in yoga gp as compared to control gp (p<0.001) | Med students |
| Manzaneque et al. (2009) 62 | 39 | 18–21 | 87 | Spain | Qigong | 1 | WL | STAI, BAI | Grp | Y | 4 | 20 | 85 | 0.73 | Qigong gp had a significant more decrease in anx after 1 month (p<.01) on STAI as compared to control. No change on Beck Anx Inventory | Healthy Ss |
| McMillan et al. (2002) 63 | 130 | 34 | 22 | UK | MBSR | 2 | WL & AA | HADS | Both | Y | 4 | 5 | 85 | 0.64 | No significant differences of change were found on anx scores b/n the MM gp and the physical exercise and WL control gps | TBI |
| Moffatt et al. (2010) 64 | 69 | 33 | 100 | Canada | GI | 2 | WL | STAI | Ind | N | 4 | 8 | 87 | 1.0 | No significant differences in change b/n the GI and WL control gps but pts reported positively for their GI experience | Pregnant hbp |
| Nidich et al. (2009) 65 | 298 | 26 | 61 | USA | TM | 1 | WL | POMS | Ind | Y | 12 | 13 | 69 | 0.89 | The TM gp showed significant more improvement in anx at 3 month follow up (p=.003) as compared to the WL control. | College students |
| Nunes et al. (2007) 66 | 34 | 52 | 100 | Brazil | GI | 2 | WL | BAI & STAI | Grp | Y | 4 | 24 | 100 | 0.73 | The GI group had significant more decrease in state anx(p<.05; ES 0.52) and trait anx (p<.001; ES 0.79) as compared to control | Breast cancer |
| Oken et al. (2004) 67 | 69 | 49 | 77 | USA | Yoga | 2 | WL & AA | STAI | Both | Y | 24 | 24 | 83 | 0.8 | No significant difference in change b/n yoga gp and exercise or WL control gps on anx measure. | Multiple sclerosis |
| Rao et al. (2009) 81 | 70 | 30–70 | 100 | India | Yoga | 2 | ATT | STAI | Ind | Y | 24 | 22 | 54 | 0.73 | Greater decrease in anx (p<.001) among yoga gp than control post-surgery, post-radiation (p<.01) & post-chemotherapy (p<.001). | Breast cancer |
| Schmidt et al. (2010) 68 | 177 | 53 | 100 | Germany | MBSR | 2 | WL & AA | STAI | Both | Y | 8 | 9 | 82 | 0.91 | AA gps showed more decrease in anx as compared to control (p=0.004) but no significant difference b/n MBSR and active control. | Fibromyalgia |
| Shapiro (1998) 69 | 200 | n/a | n/a | USA | MBSR | 1 | WL | STAI | Both | Y | 8 | 8 | 97 | 0.73 | The mindfulness gp showed a significant more decrease in both state anx (p<.05) and trait anx (p<.002) as compared to control | Med Student Stress |
| Sheppard et al. (1997) 86 | 44 | 50.5 | 15 | USA | TM | 1 | AA | STAI | Both | Y | 12 | 13 | 73 | 0.64 | The TM gp showed more decrease in anx at 3mos (p<0.05) as compared to control and this pattern continued at 3 yr follow up.. | Healthy |
| Sloman et al. (2002) 70 | 56 | 27–79 | 46 | Israel | GI | 3 | WL | HADS | Ind | N | 4 | 4 | 100 | 0.8 | No significant decrease in anx for GI gp (p=0.57) as compared to control. | Cancer |
| Smith et al. (2007) 85 | 131 | 44 | 83 | Australia | Yoga | 1 | AA | STAI | Grp | N | 10 | 10 | 90 | 0.82 | Yoga gp had more improvement on mental health. But no sig differences b/n gps on the STAI | Healthy |
| Speca et al. (2000) 71 | 109 | 51 | 79 | Canada | MBSR | 2 | WL | POMS | Both | Y | 7 | 7 | 83 | 0.73 | MBSR had sig more decreased anxiety after intervention as compared to the control (p<0.001) | Cancer |
| Stein et al. (2010) 72 | 56 | 66 | 30 | USA | GI | 3 | WL & AA | HADS; POMS | Ind | Y | 24 | 1 | 100 | 0.67 | There was no sig difference b/n gps on anx measures but participants reported liking GI. | Coronary Bypass |
| Stenlund et al. (2009) 73 | 82 | 44 | 83 | Sweden | Qigong | 2 | WL | HADS | Grp | Y | 12 | 24 | 82 | 0.67 | No difference in anx levels b/n gps; both improved significantly on anx over time | Burnout |
| Tacon et al. (2003) 28 | 18 | 61 | 100 | USA | MBSR | 2 | WL | STAI | Both | Y | 8 | 8 | 90 | 0.58 | The mindfulness gp showed a significant more decrease in anx (p<.01) and there was no change in the control gp. | Heart Disease |
| Taneja et al. (2004) 74 | 22 | 35 | 0 | India | Yoga | 2 | WL | STAI | Ind | Y | 8 | 1 | 95 | 0.55 | At 1 month there was a more sig decrease in anxiety in yoga gp as compared to control (p<0.01), but not so at 2 months. Overall p < .05. | IBS |
| Tsai et al. (2003) 75 | 88 | 52 | 43 | Taiwan | Tai Chi | 2 | WL | STAI | Grp | N | 12 | 36 | 86 | 0.7 | Tai Chi gp showed a sig more decrease in anx (both state & trait p<.01) as compared to control. | Hypertension |
| Vadiraja et al. (2009) 82 | 88 | 47 | 100 | India | Yoga | 2 | ATT | HADS | Ind | Y | 6 | 18–24 | 89 | 0.6 | Both the yoga gp and the supportive therapy control gp decreased in anx scores but there was a significant difference b/n the gps (p<.001). | Breast cancer |
| Wang et al. (2010) 39 | 34 | 77 | 55 | Japan | Tai Chi | 2 | AA | GHQ-A | Grp | N | 12 | 12 | 85 | 0.58* | Tai Chi gp showed a significant more reduction in anx (p=.034) as compared to the control. | Stroke |
| Williams et al. (2008) 76 | 68 | 18–65 | 47 | UK | MBSR | 4 | WL | BAI | Both | Y | 8 | 8 | 81 | 0.8 | Mindfulness gp had lower anx than the control gp (p=.014) for bipolar pts, but no for unipolar pts. | Bipolar Disorder |
| Wu et al. (1999) 83 | 26 | 38 | 73 | USA | Qigong | 2 | ATT | CSAQ | Ind | Y | 10 | 6 | 85 | 0.6 | Qigong gp had greater anx reduction than control gp over time (p<.01) but no sig difference b/n gps. | Pain |
Note: Type of subjects (Ss): 1= healthy subjects; 2 = patients with health problems & anxiety symptoms; 3 = patients with anxiety disorders; 4 = Mixed.
Type of control: WL= Waiting list or treatment as usual; ATT=attention/education control; AA=alternate active therapy
Type of Meditation: MM = Mindfulness; MBSR=mindfulness-based stress reduction; TM=transcendental meditation; GI=guided imagery; MBCT=mindfulness-based cognitive therapy
Anxiety Measure: STAI = (Spielberg) State-Trait Anxiety Inventory; HAM-A=Hamilton Anxiety sale; HADS = Hospital anxiety and depression scale; BAI = Beck Anxiety Inventory; GHQ-A = General Health Question – Anxiety
Other abbreviations: Ss = Subjects; gp=group; Anx= Anxiety; tx = treatment; b/n = between; Pts=participants; ES=effect size; Ret = retention; unc = unclear;
Did not receive reply from authors for follow-up communications
The sample sizes ranged from 20 to 298 (effective cases in data analysis ranged from 18 to 207). Thirty six studies had sufficient data to be included in the meta-analysis for quantitative comparison. The pooled sample was composed of 2,466 effective unique subjects in the meta-analysis, where 1,151 were in the meditation groups, while 1,315 were in control/comparison groups (6 studies included more than one control group). RCTs with meditative therapies were then be divided into three categories in terms of the type of control conditions used for comparison: waiting-list or treatment as usual control, attention control (education or non-directive therapies), and alternative active treatment (such as music therapy, pharmacotherapy or other exercises).
The general quality of these RCTs were acceptable per CLEAR-NPT [41]: 16 (40%) studies had a quality score of 0.8 or better, indicating a good quality in research design; Seventeen studies (42.5%) fell into the category of moderate or acceptable quality (0.6 to 0.8), and only 7 studies (17.5%) had a quality score lower than 0.6.
Main Outcome Measures
Meta-analyses with standardized mean difference (SMD) for various meditative therapies were conducted by three types of control used for comparison. Most of the RCTs (28 in total) investigated the efficacy of meditative therapies for reducing anxiety symptoms by comparing the meditation plus treatment as usual (TAU) with the TAU only (for clinical samples of patients, or waiting-list control for healthy subjects) [13,28, 51–76]. All studies in this category reported greater reduction of anxiety symptoms in the meditative group than that in the waiting list or TAU group although not all were statistically significant (see Figure 2). Eighteen of the 25 studies in meta-analysis (72%) reported statistically significant differences in reducing anxiety between meditation group and the control; 12 studies (48%) showed significant differences in SMD in comparison with the TAU or waiting-list control (which may be related to the fact that we used the baseline standard deviation (SD) in calculation of SMD when SD of change was not available). Pooling the results, we found a statistically significant SMD of −0.52 (p < .001; 95% CI: −0.62, −0.41) based on a total of 1,608 unique observations (788 in meditative groups and 820 in control group).
Figure 2.
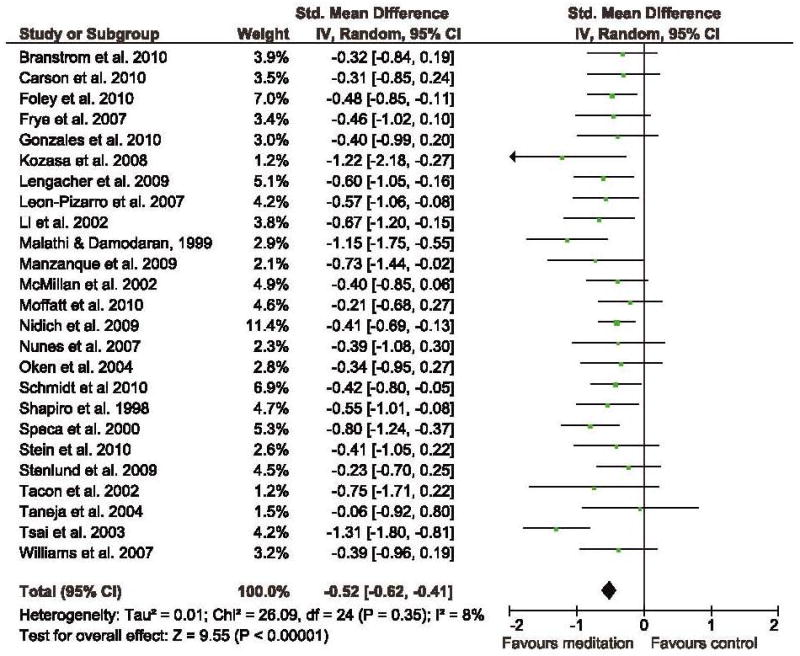
Forest plot of comparison: Meditation vs. Waiting List control Weighted Mean Differences
Eight RCTs evaluated the efficacy of meditative therapies for anxiety in comparison with similar or comparable attention [26, 77–83]. Two of the studies reported applying supportive counseling in the control group [81–82], but did not give any details on how the counseling was delivered, so we treated them as attention control. All studies in this category reported significantly greater reduction of anxiety in the meditative group than that in control, and four of them (57%) showed statistically significant SMD in comparison with the attention control. Overall, we observed a statistically significant SMD of −0.59 (p < 0.001; 95% CI: −0.79, −0.39) based on 466 unique subjects (245 in meditation, and 221 in attention control).
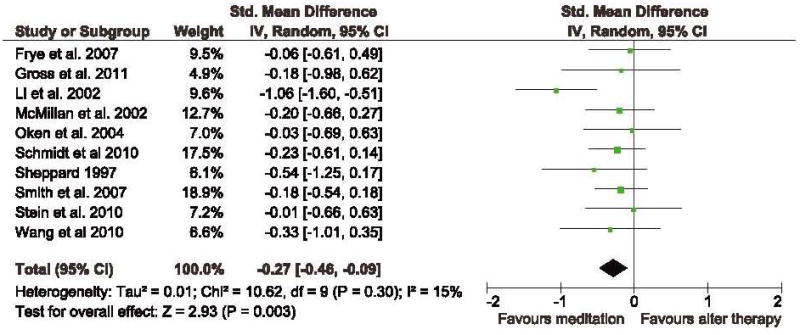
Ten RCTs compared the meditative therapies with other active therapies for a health issue or anxiety in their research design (6 had more than one control group). These other active therapies included physical exercises [54, 63, 67], pharmaceutical therapy [60,84], music therapy [72], progressive muscle relaxation [68, 85], a rehabilitation program [39], or a corporate stress management program [86]. Three studies (30%) reported significantly greater reduction of anxiety in the meditative group than that in control. Although most of these studies did not show statistically significant differences between meditative therapy and the active therapy, meditative therapy seemed to do just as well as, or better than, other active therapies in comparison. Overall we found a statistically significant SMD of −0.27 (p =0.003; 95% CI: −0.46, −0.09) based on 581 unique observations (307 in meditative group and 274 in active therapy group). If we removed the study with the largest effect [49] from the analysis (treated it as an outlier), the SMD would be reduced to −0.19 (p =0.03; 95% CI: −0.36, −0.02), which was much less robust but still significant.
By examining the I2 in heterogeneity analysis, we found that heterogeneity in the reviewed studies with the waiting-list control, attention control and active therapy control were all at an acceptable level (since I2 is equal to 8%, 10% or 15% accordingly, under the 30% guideline for possible problem in heterogeneity per Cochrane Handbook [87]).
Subgroup Analysis
We conducted subgroup analyses to explore the possible differences in SMD among studies with waiting-list or attention control, given the large number of RCTs that were included in the review. There were no significant differences between the waiting-list control and attention control in the majority of the pooled outcomes (see Table 2 for the results of these exploratory subgroup comparisons in SMD of meditative therapies for reduced anxiety).
Table 2.
Exploratory Comparisons of Subgroup Differences in SMD of Reduced Anxiety among Studies with Waiting-list Control or Attention Control
| Subgroups | # Studies | # Subjects | SMD (95% CI) | p values (grp differences) |
|---|---|---|---|---|
| Total | 32 | 2,074 | −0.53 (−0.62, −0.44) | |
| By Type of Meditation1 | P = 0.48 | |||
| Mindfulness Meditation | 11 | 869 | −0.51 (−0.64, −0.37) | |
| Yoga | 9 | 424 | −0.63 (−0.88, −0.38 | |
| Qigong or Tai Chi | 5 | 288 | −0.68 (−1.07, −0.29) | |
| Guided Imagery | 5 | 252 | −0.39 (−0.64, −0.14) | |
| By Duration of Study | P = 0.81 | |||
| 4 weeks or shorter | 9 | 453 | −0.57 (−0.77, −0.36) | |
| 6 to 10 weeks | 12 | 771 | −0.56 (−0.71, −0.42) | |
| 12 weeks or longer | 11 | 850 | −0.50 (−0.66, −0.33) | |
| By Density of meditation training2 | P = 0.46 | |||
| Weekly or less | 20 | 1379 | −0.51 (−0.62, −0.40) | |
| 2+ a week to daily | 10 | 612 | −0.60 (−0.81, −0.39) | |
| By Training/Therapy Delivery method | P = 0.17 | |||
| Group or Group plus Individual | 23 | 1402 | −0.58 (−0.70, −0.46) | |
| Individual | 9 | 672 | −0.44 (−0.60, −0.29) | |
| By Homework assignment3 | P = 0.83 | |||
| With Homework | 26 | 1735 | −0.52 (−0.61, −0.42) | |
| Without Homework | 5 | 279 | −0.56 (−0.98, −0.15) | |
| By Region of studies | P = 0.04 | |||
| From Western Countries | 24 | 1631 | −0.46 (−0.56, −0.27) | |
| From Eastern Countries | 8 | 443 | −0.77 (−1.04, −0.50) | |
| By Quality of the Study | P = 0.02 | |||
| CLEAR-NPT ≥ 0.8 | 12 | 981 | −0.40 (−0.53, −0.27) | |
| CLEAR-NPT: 0.6—0.8 | 14 | 858 | −0.61 (−0.75, −0.46) | |
| CLEAR-NPT < 0.6 | 6 | 235 | −0.83 (−0.15, −0.50) | |
| By Type of Subjects4 | P = 0.91 | |||
| Patients with other health issues | 22 | 1410 | −0.53 (−0.65, −0.41) | |
| Healthy subjects (not patient) | 6 | 489 | −0.54 (−0.73, −0.35) | |
| Patients with anxiety issue | 3 | 127 | 0.61 (−0.97, −0.25) |
Note:
Two studies of TM were not included in subgroup analysis.
Two studies ran only one session of meditative training and were not included.
One residential study was not included.
One study with mixed subjects was not included.
Overall, there were no statistically significant differences in the pooled results of SMD among the majority of subgroup comparisons with two exceptions: study quality and region of the study being conducted. Therefore, we cannot draw conclusions solely based on these comparisons. The subgroup comparisons suggest that moving meditation like Qigong, tai chi or yoga practice seemed to produce the larger effect in terms of pooled SMD (−0.68 to −0.63) of reduced anxiety than those by the static meditation like guided imagery (−0.39) or mindfulness (−0.51). The longer meditation duration did not add any additional effect. No difference was found in terms of density of meditation, or type of study subjects, or homework assignment; however, we did see a trend in which studies with group delivery reported higher SMD (−0.58) than those with individual delivery (−0.44). Again, most of the subgroup differences were not statistically significant. We also noticed that all studies with healthy subjects (6 in total) reported significant differences in reduced anxiety between the meditation group and control group.
Two significant subgroup differences were found in the region where the study was conducted and in the study quality. Those studies conducted in the eastern countries (India, China and Japan) had a significantly larger effect than those conducted in the western countries (−0.77 vs. −0.46; p = 0.04), where meditation may be considered less mainstream. As to the differences in study quality, the lower quality studies tended to report a larger effect than the high-quality studies. Those studies with a CLEAR-NPT score less than 0.6 reported a mean SMD twice as much as those studies with a quality score greater than 0.8 (−0.83 vs. −0.40; p = 0.02).
A close examination of these studies for possible adverse effects found no reported side effects and most did not report the procedure for addressing adverse effects or mention safety examination. Among the studies that examined safety issues in the paper [39, 67–68], none reported any adverse effect from meditative therapies.
CONCLUSIONS
Summary of main results
The current review and meta-analysis of a number of small to medium-scale quality RCTs showed some consistent and robust evidence that meditative therapies may be an effective treatment for patients with anxiety symptoms. The pooled effects of meditative therapies for anxiety were clinically relevant when compared with the waiting list (or TAU) and the attention controls, but not as robust when compared with other active or alternative therapies. In other words, evidence from this review indicates that meditative therapies are more effective than waiting-list control or attention control, and may be considered as effective as other alternative therapies used in these studies (such as music therapy, exercises or relaxation practice) for reducing anxiety symptoms.
Differing from the findings in previous reviews of meditation, we found that quality of the reviewed RCTs was much better, mostly acceptable, and some of them (40%) were of good quality. This different finding in study quality may be related to several factors. The first factor is the quality criteria used to assess the studies. Specifically, most previous reviews used a standard Jadad scale [42], which emphasizes significance of blindness. Because blindness is hard to implement in a meditation study, we believe this is an overly strict criteria and therefore we used a more practical quality checklist (11 criteria instead of 5) that was designed for non-pharmaceutical trials. The second factor is the procedure of review. We tried to contact most authors for needed clarifications in detailed research design, treatment outcomes and other quality issues while most previous reviews, including Ospina et al [6], did not appear to apply this critical procedure. The third factor is the overall quality of meditation studies have increased continuously in the past 10 years. Our analysis of study quality over time indicates that studies published prior to 2000 had a relatively lower quality score (CLEAR = 0.66), studies published in 2000–2005 had slightly higher quality score (CLEAR = 0.69), while studies published after 2006 had a mean quality score of 0.75. Obviously our new review included more recently published high-quality studies, which likely indicate better data quality but also better control conditions and checks to limit specious findings.
Our analysis revealed that quality of the RCT directly affects the magnitude of the observed effect size. Although somewhat speculative, this implies that the results of low quality studies may reflect a greater experimenter effect or other research biases. This is particularly problematic, because study quality is extremely important when evaluating the efficacy of a specific therapy.. We also found that the studies conducted in Eastern countries (India, China and Japan) had a significantly larger effect than those conducted in the Western countries (−0.77 vs. −0.46; p = 0.04).. This finding may reflect a few factors, including the following: (1) differing degrees of acceptance of meditation as part of mainstream interventions (Eastern countries have higher acceptance than Western countries); (2) the quality of study design (researchers in Western countries may apply higher standard or quality control procedures than those in Eastern countries, or there may be more room for experimenter bias in the Eastern studies where experimenters may believe more strongly in the benefits of these approaches); and (3) differing degrees of experience with meditation (researchers in Eastern countries may be more experienced with meditation).
Limitations and challenges
Although the findings of this review suggest some promising clinical benefits of meditative therapies for anxiety, we also must acknowledge some limitations that reduce our ability to draw conclusions from these results. First and foremost, the diversity of meditation modalities and study designs make it difficult to draw a general conclusion based on the evidence, particularly because the effects of meditative therapies on anxiety differ depending on whether the meditation is compared with a waiting list (or treatment as usual), additional attention control, or alternative active therapies, and depending on the quality of studies. The clinically relevant effects of meditative therapies for anxiety when compared with a waiting list or usual care control, or with the attention control, may be partially attributable to possible placebo effects of meditative settings (for example, relaxing music in most meditation settings, or belief that meditation works before signing up for the study). It is a methodological challenge to design a compatible control when the intervention or treatment involves the patient’s active participation, making it impossible to blind the participants to which group they were assigned to, and to have a meaningful control group that will take the same amount of time and effort in treatment without substantial benefits to the studied health condition. The traditional double-blind placebo-controlled design used for pharmaceutical clinical trials is not applicable to this kind of therapy [88], as in RCTs evaluating psychotherapy [89]. However, different from research design in psychotherapy, meditation studies involved more elements of active participation and daily practice from the study subjects, and thus it may be even more difficult to apply the standardization procedure for quality control and for therapy compliance. Therefore, results in this type of RCT may be more influenced by potential placebo effects and suggest the need to identify more innovative research designs and comparable control conditions to enable true evaluation of effectiveness in reducing anxiety outcomes.
Participants’ preferences and expectations may also partially explain the findings. For example, we found more patients discontinued study participation in both waiting-list and attention-control groups than those in active meditation groups in many of the reviewed studies (although this difference was not statistically significant). It also was evident that the pooled effect size or SMD in comparison with attention control (−0.59) was actually slightly higher than those in comparison with waiting-list or TAU control (−0.52), suggesting that participants did worse in an attention control compared to a usual care or waiting-list control (2 of 7 studies using an attention-control group actually reported increased anxiety following the control condition). This may reflect participants in an attention control group being more aware of their assignment to a control. It is difficult to ascertain how observed benefits are attributable to specific effects of meditation.
Another potential limitation of the studies reviewed is the relatively small sample size in most studies, especially those studies using other active therapies as the comparison conditions. Most reviewed studies included fewer than 100 participants (average n = 80). Additionally, there was a wide range of study duration, with meditation training ranging from 1 day to 1 year. Although a funnel plot of all studies in waiting-list control indicates a relatively symmetric pattern, suggesting no obvious publication bias in the literature itself (see Figure 5), most studies with non-significant SMD were with smaller samples (larger standard error in Y-axis). This limitation makes it hard to draw any firm conclusions regarding effectiveness. Future larger scale studies are needed to continue to assess the efficacy and effectiveness of meditative therapies.
Figure 5.
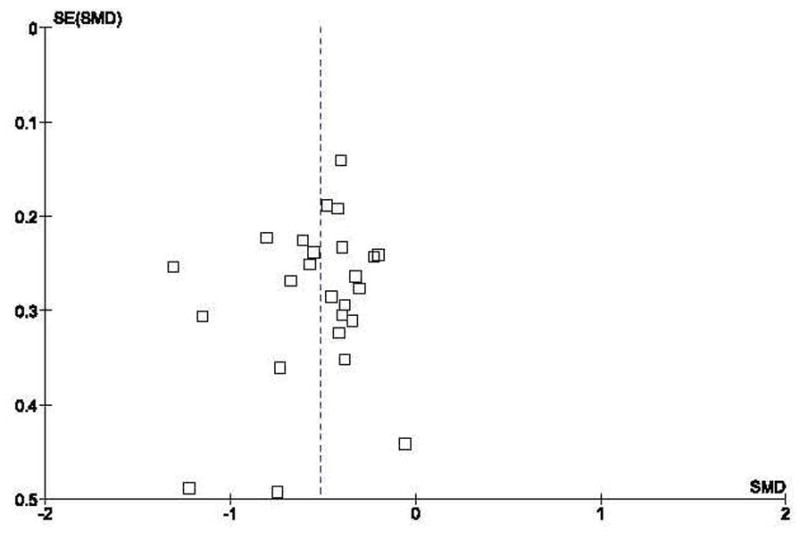
Funnel Plot of Studies Comparing Meditation Group with Waiting-list Control
Finally, several issues must be considered in terms of the clinical implications of the observed effects. First, the large majority of the reviewed studies measured the reductions in non-clinical levels of anxiety symptoms, and few studies have assessed the clinical efficacy of meditative interventions for diagnosed anxiety disorders, which is what most clinicians are confronted with in clinical setting. Therefore, conclusions about the impact of meditational approaches must be tempered as they relate to clinically relevant manifestations of anxiety. Additionally, existing literature has not reported on the effect of meditation quality or compliance on the treatment outcome, although it is assumed that quality of meditation will affect the effect size or overall conclusion. Similar to the need for monitoring drug-intake during pharmaceutical trials, studies of meditative therapies should take into account the quality of meditation and proportion of participants who are able to comply with protocol to truly assess the therapy’s feasibility and effectiveness. Among the reviewed studies, 20 of 40 studies (50%) examined the quality or compliance of meditation practice as part of research design; however, few actually compared the differences in outcomes between the low-compliance group and the high-compliance group. Future studies of meditation should more carefully address this issue. (Figure 5 here)
Implications and future directions
This review indicates the potential effectiveness of of meditative therapies in reducing anxiety. However, a few key considerations must guide future work. Meditative therapy is not a stand-alone therapy in the traditional clinical setting, and may not be able to be adequately studied using traditional double-blind placebo-controlled trial methodology. Therefore, it may not be appropriate to apply all traditional clinical criteria to assess the safety and efficacy issues in meditative therapies. Meditation is a whole package of mind-body exercise with possibility of change in life-style or attitude, which includes both specific and non-specific effects. These reviewed studies suggest that people with anxiety may find meaningful benefits through meditation or related exercise, although it cannot be determined whether these benefits may be mediated through placebo, expectation, or self-suggestion.
Second, application of the modified quality assessment tool in our review suggests that most studies of meditative therapies for anxiety are actually of good or acceptable quality, and the results of these studies can be taken into consideration in future work. As quality of the studies may directly affect the reliability of the results, it is relevant that many high quality studies in this review reported significant differences in reducing anxiety between the meditation and control groups. This is a distinct difference between this review and what previous reviews have concluded.
In conclusion, our systematic review and meta-analysis suggests that meditative therapy may be an effective option for reducing anxiety symptoms. Our findings suggest that meditation works significantly better than TAU or attention control and works as well as other active therapies used in these studies for reducing anxiety. However, to date, clinical efficacy of meditative intervention for anxiety disorders has not been well documented. Although more large-scale studies with improved quality are needed to develop more specific clinical guidelines for its applications and firm conclusions regarding its efficacy, the current review does suggest meditation to be a potential intervention for anxiety. Highlighting the effects of meditation on anxiety is important in that it may provide a useful alternative to existing pharmacotherapy and psychotherapy approaches to treat anxiety. Given the fact that meditative therapies are so easy to carry out without any known adverse effect, and the fact that no existing treatment is effective for all patients or for all anxiety disorders, clinicians may consider recommending meditation for patients of anxiety and promoting meditative therapies for anxiety and related disorders.
Figure 3.
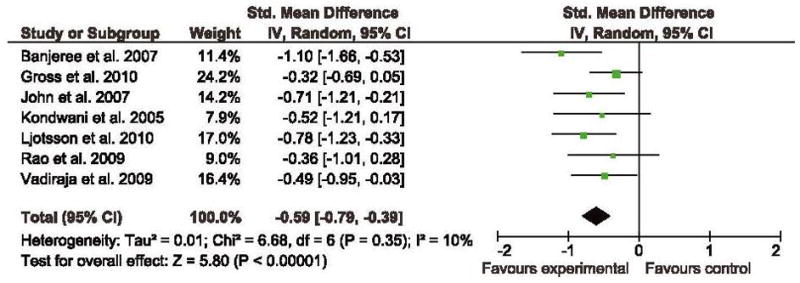
Forest plot of comparison: Meditation vs. Attention control Weighted Mean Differences
Figure 4.
Forest plot of comparison: Meditation vs. Alternative Active Therapy Group Weighted Mean Differences
Acknowledgments
This study was partially supported by an independent investigator award from Brain & Behavior Research Foundation (a.k.a. NARSAD) to Dr. Kevin Chen, and a research grant (R24 AT001293) from the National Center for Complementary and Alternative Medicine (NCCAM) at the U.S. National Institutes of Health, to the Center for Integrative Medicine at University of Maryland Baltimore (PI: Dr. Brian Berman). This paper’s contents are solely the responsibility of the authors and do not necessarily represent the official views of NARSAD or NCCAM.
Footnotes
There is no single universally agreed upon categorization or definition of meditative therapies. We have decided to use the academic definition of meditative therapy in Chinese college textbook to provide a more general focus on integrating breathing, mind, and body adjustments into one, which allows us to consider a broad range of meditation literature from which to draw a more comprehensive picture in the field. Moreover, the approach including various meditations is consistent with the existing review in this area (see Ospina et al., 2007).
Contributor Information
Kevin W Chen, Email: kchen@compmed.umm.edu.
Christine C. Berger, Email: cberger@compmed.umm.edu.
Eric Manheimer, Email: emanheimer@compmed.umm.edu.
Darlene Forde, Email: Darlene.forde@googlemail.com.
Jessica Magidson, Email: jmagidso@umd.edu.
Laya Dachman, Email: ldachma@gmail.com.
C. W. Lejuez, Email: clejuez@umd.edu.
References
- 1.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson VL, Levinson EM, Barker W, Kiewra KR. The effects of meditation on teacher perceived occupational stress, state and trait anxiety, and burnout. School Psychology Quarterly. 1999;14:3. [Google Scholar]
- 3.Deng G, Cassileth BR. Integrative oncology: Complementary therapies for pain, anxiety, and mood disturbance. CA: a cancer journal for clinicians. 2005;55:109–116. doi: 10.3322/canjclin.55.2.109. [DOI] [PubMed] [Google Scholar]
- 4.Issakidis C, Sanderson K, Corry J, Andrews G, Lapsley H. Modelling the population cost-effectiveness of current and evidence-based optimal treatment for anxiety disorders. Psychol Med. 2004;34:19–35. doi: 10.1017/s003329170300881x. [DOI] [PubMed] [Google Scholar]
- 5.Manocha R. Why meditation? Aust Fam Physician. 2000;29:1135–1138. [PubMed] [Google Scholar]
- 6.Ospina MB, Bond K, Karkhane M, et al. Evidence Reports/Technology Assessments, NO 155. Rockville, MD: Agency for Healthcare Research and Quality; Jun, 2007. Meditation practices for health: State of the research. Agency for Healthcare Research and Quality.US Department of Health and Human Services. [Google Scholar]
- 7.Travis F, Pearson C. Pure consciousness: distinct phenomenological and physiological correlates of “consciousness self”. International Journal of Neuroscience. 2000;100(1–4):77–89. [PubMed] [Google Scholar]
- 8.Liu T, Chen KW, editors. Chinese Medical Qigong. London: Jessica Kingsley; 2010. [Google Scholar]
- 9.Arias AJ, Steinberg K, Banga A, Trestman RL. Systematic review of the efficacy of meditation techniques as treatments for medical illness. The Journal of Alternative and Complementary Medicine. 2006 doi: 10.1089/acm.2006.12.817. [DOI] [PubMed]
- 10.Krisanaprakornkit T, Krisanaprakornkit W, Piyavhatkul N, Laopaiboon M. Meditation therapy for anxiety disorders. Cochrane database of systematic reviews (Online) 2006:CD004998. doi: 10.1002/14651858.CD004998.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Manzoni G, Pagnini F, Castelnuovo G, Molinari E. Relaxation training for anxiety: A ten-years systematic review with meta-analysis. BMC Psychiatry. 2008;8:41. doi: 10.1186/1471-244X-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy M, Donovan S, Taylor E. The Physical and Psychological Effects of Meditation: A Review of Contemporary Research. Published by the Institute of Noetic Sciences. [Google Scholar]
- 13.Bränström R, Kvillemo P, Brandberg Y, Moskowitz JT. Self-report mindfulness as a mediator of psychological well-being in a stress reduction intervention for cancer Patients—A randomized study. Annals of Behavioral Medicine. 2010;39:151–161. doi: 10.1007/s12160-010-9168-6. [DOI] [PubMed] [Google Scholar]
- 14.Elkins G, Fisher W, Johnson A. Mind–Body therapies in integrative oncology. Current treatment options in oncology. 2010:1–13. doi: 10.1007/s11864-010-0129-x. [DOI] [PubMed] [Google Scholar]
- 15.Klein DF. False suffocation alarms, spontaneous panics, and related conditions: An integrative hypothesis. Archive of General Psychiatry. 1993 Apr;50(4):306–17. doi: 10.1001/archpsyc.1993.01820160076009. [DOI] [PubMed] [Google Scholar]
- 16.Ley R. Blood, breath and fears: A hyperventilation theory of panic attacks and agoraphobia. Clinical Psychology Review. 1986;5:271–285. [Google Scholar]
- 17.Clark DM. Anxiety disorders: Why they persist and how to treat them. Behavior Research and Therapy. 1999;37:S5–S27. doi: 10.1016/s0005-7967(99)00048-0. [DOI] [PubMed] [Google Scholar]
- 18.Chiang LC, Ma WF, Huang JL, Tseng LF, Hsueh KC. Effect of relaxation-breathing training on anxiety and asthma signs/symptoms of children with moderate-to-severe asthma: A randomized controlled trial. International Journal of Nursing Studies. 2009;46(8):1061–1070. doi: 10.1016/j.ijnurstu.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 19.Gilbert C. Clinical applications of breathing regulation. Behavior Modification. 2003;27(5):692. doi: 10.1177/0145445503256322. [DOI] [PubMed] [Google Scholar]
- 20.Roth WT. Diversity of effective treatments of panic attacks: What do they have in common? Depression and Anxiety. 2010;27(1):5–11. doi: 10.1002/da.20601. [DOI] [PubMed] [Google Scholar]
- 21.Sánchez-Meca J, Rosa-Alcázar AI, Marín-Martínez F, Gómez-Conesa A. Psychological treatment of panic disorder with or without agoraphobia: A meta-analysis. Clinical Psychology Review. 2010;30(1):37–50. doi: 10.1016/j.cpr.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Brand S, Holsboer-Tracgsker E, Naranjo JR, Schmidt S. Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology. 2012;65(3):109–118. doi: 10.1159/000330362. [DOI] [PubMed] [Google Scholar]
- 23.Ng BH, Tsang HW. Psychophysiological outcomes of health qigong for chronic conditions: A systematic review. Psychophysiology. 2009;46(2):257–269. doi: 10.1111/j.1469-8986.2008.00763.x. [DOI] [PubMed] [Google Scholar]
- 24.Jung YH, Kang DH, Jang JH, Park HY, Byun MS, Kwon SJ, Jang GE, Lee US, An SC, Kwon JS. The effects of mind-body training on stress reduction, positive affect, and plasma catecholamines. Neuroscience Letters. 2010;479(2):138–142. doi: 10.1016/j.neulet.2010.05.048. [DOI] [PubMed] [Google Scholar]
- 25.Wolpe J. Psychotherapy by Reciprocal Inhibition. California: Stanford University Press; 1958. [Google Scholar]
- 26.Gross CR, Kreitzer MJ, Thomas W, et al. Mindfulness-based stress reduction for solid organ transplant recipients: A randomized controlled trial. Altern Ther Health Med. 2010;16:30–38. [PMC free article] [PubMed] [Google Scholar]
- 27.Miller JJ, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders* 1. Gen Hosp Psychiatry. 1995;17:192–200. doi: 10.1016/0163-8343(95)00025-m. [DOI] [PubMed] [Google Scholar]
- 28.Tacón AM, McComb J, Caldera Y, Randolph P. Mindfulness meditation, anxiety reduction, and heart disease: A pilot study. Fam Community Health. 2003;26:25. doi: 10.1097/00003727-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: A systematic review and meta-analysis. Psychiatry Res. 2011;187:441–453. doi: 10.1016/j.psychres.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 30.Chiesa A, Malinowski P. Mindfulness-based approaches: Are they all the same? J Clin Psychol. 2011 doi: 10.1002/jclp.20776. [DOI] [PubMed]
- 31.Kim YW, Lee SH, Choi TK, et al. Effectiveness of mindfulness - based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depress Anxiety. 2009;26:601–606. doi: 10.1002/da.20552. [DOI] [PubMed] [Google Scholar]
- 32.Zeidan F, Johnson SK, Diamond BJ, David Z, Goolkasian P. Mindfulness meditation improves cognition: Evidence of brief mental training. Conscious Cogn. 2010;19:597–605. doi: 10.1016/j.concog.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 33.Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10:83. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saeed S, Antonacci D, Bloch R. Exercise, yoga, and meditation for depressive and anxiety disorders. Am Fam Physician. 2010;81:981. [PubMed] [Google Scholar]
- 35.Ülger Ö, YaglI NV. Effects of yoga on the quality of life in cancer patients. Complementary Therapies in Clinical Practice. 2010;16:60–63. doi: 10.1016/j.ctcp.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 36.Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: A systematic review of the research evidence. Br J Sports Med. 2005;39:884. doi: 10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yook K, Lee SH, Ryu M, et al. Usefulness of mindfulness-based cognitive therapy for treating insomnia in patients with anxiety disorders: A pilot study. J Nerv Ment Dis. 2008;196:501. doi: 10.1097/NMD.0b013e31817762ac. [DOI] [PubMed] [Google Scholar]
- 38.Chiesa A. Vipassana meditation: Systematic review of current evidence. The Journal of Alternative and Complementary Medicine. 2010;16:37–46. doi: 10.1089/acm.2009.0362. [DOI] [PubMed] [Google Scholar]
- 39.Wang W, Sawada M, Noriyama Y, et al. Tai chi exercise versus rehabilitation for the elderly with cerebral vascular disorder: A single - blinded randomized controlled trial. Psychogeriatrics. 2010;10:160–166. doi: 10.1111/j.1479-8301.2010.00334.x. [DOI] [PubMed] [Google Scholar]
- 40.Sancier KM. Search for medical applications of qigong with the qigong database™. The Journal of Alternative & Complementary Medicine. 2001;7:93–95. doi: 10.1089/107555301300004574. [DOI] [PubMed] [Google Scholar]
- 41.Boutron I, Moher D, Tugwell P, et al. A checklist to evaluate a report of a nonpharmacological trial (CLEAR NPT) was developed using consensus. J Clin Epidemiol. 2005;58:1233–1240. doi: 10.1016/j.jclinepi.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 42.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 43.Review Manager 5.0 website. http://ims.cochrane.org/revman.
- 44.Cheung B, Lo J, Fong D, et al. Randomised controlled trial of qigong in the treatment of mild essential hypertension. J Hum Hypertens. 2005;19:697–704. doi: 10.1038/sj.jhh.1001884. [DOI] [PubMed] [Google Scholar]
- 45.Hui PN, Wan M, Chan WK, Yung PMB. An evaluation of two behavioral rehabilitation programs, qigong versus progressive relaxation, in improving the quality of life in cardiac patients. Journal of Alternative & Complementary Medicine. 2006;12:373–378. doi: 10.1089/acm.2006.12.373. [DOI] [PubMed] [Google Scholar]
- 46.Nyklcek I, Kuijpers KF. Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: Is increased mindfulness indeed the mechanism? Annals of Behavioral Medicine. 2008;35:331–340. doi: 10.1007/s12160-008-9030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448–474. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- 48.Stenlund T, Ahlgren C, Lindahl B, et al. Cognitively oriented behavioral rehabilitation in combination with qigong for patients on long-term sick leave because of burnout: REST—a randomized clinical trial. Int J Behav Med. 2009;16:294–303. doi: 10.1007/s12529-008-9011-7. [DOI] [PubMed] [Google Scholar]
- 49.Spielberger CD. State - Trait anxiety inventory. Corsini Encyclopedia of Psychology. 1996 [Google Scholar]
- 50.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale:: An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 51.Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD. A pilot randomized controlled trial of the yoga of awareness program in the management of fibromyalgia. Pain. 2010;151:530–539. doi: 10.1016/j.pain.2010.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davidson RJ, Kabat-Zinn J, Schumacher J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65:56. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- 53.Foley E, Baillie A, Huxter M, Price M, Sinclair E. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: A randomized controlled trial. J Consult Clin Psychol. 2010;78:72. doi: 10.1037/a0017566. [DOI] [PubMed] [Google Scholar]
- 54.Frye B, Scheinthal S, Kemarskaya T, Pruchno R. Tai chi and low impact exercise: Effects on the physical functioning and psychological well-being of older people. Journal of Applied Gerontology. 2007;26:433. [Google Scholar]
- 55.Gonzales EA, Ledesma RJA, McAllister DJ, Perry SM, Dyer CA, Maye JP. Effects of guided imagery on postoperative outcomes in patients undergoing same-day surgical procedures: A randomized, single-blind study. AANA Journal. 2010:78. [PubMed] [Google Scholar]
- 56.Kabat-Zinn J, Wheeler E, Light T, et al. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA) Psychosom Med. 1998;60:625. doi: 10.1097/00006842-199809000-00020. [DOI] [PubMed] [Google Scholar]
- 57.Kozasa EH, Santos RF, Rueda AD, Benedito-Silva AA, De Ornellas FL, Leite JR. Evaluation of Siddha Samadhi yoga for anxiety and depression symptoms: a preliminary study 1, 2. Psychol Rep. 2008;103:271–274. doi: 10.2466/pr0.103.1.271-274. [DOI] [PubMed] [Google Scholar]
- 58.Lengacher CA, Johnson-Mallard V, Post-White J, et al. Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology. 2009;18:1261–1272. doi: 10.1002/pon.1529. [DOI] [PubMed] [Google Scholar]
- 59.León-Pizarro C, Gich I, Barthe E, et al. A randomized trial of the effect of training in relaxation and guided imagery techniques in improving psychological and quality-of-life indices for gynecologic and breast brachytherapy patients. Psycho-Oncology. 2007;16:971–979. doi: 10.1002/pon.1171. [DOI] [PubMed] [Google Scholar]
- 60.Li M, Chen K, Mo Z. Use of qigong therapy in the detoxification of heroin addicts. Altern Ther Health Med. 2002;8:50–59. [PubMed] [Google Scholar]
- 61.Malathi A, Damodaran A. Stress due to exams in medical students--role of yoga. Indian J Physiol Pharmacol. 1999;43:218–224. [PubMed] [Google Scholar]
- 62.Manzaneque JM, Vera FM, Rodriguez FM, Garcia GJ, Leyva L, Blanca MJ. Serum cytokines, mood and sleep after a qigong program. Journal of Health Psychology. 2009;14:60. doi: 10.1177/1359105308097946. [DOI] [PubMed] [Google Scholar]
- 63.McMillan T, Robertson IH, Brock D, Chorlton L. Brief mindfulness training for attentional problems after traumatic brain injury: A randomised control treatment trial. Neuropsychological rehabilitation. 2002;12:117–125. [Google Scholar]
- 64.Moffatt FW, Hodnett E, Esplen MJ, Watt-Watson J. Effects of guided imagery on blood pressure in pregnant women with hypertension: A pilot randomized controlled trial. Birth. 2010;37:296–306. doi: 10.1111/j.1523-536X.2010.00424.x. [DOI] [PubMed] [Google Scholar]
- 65.Nidich SI, Rainforth MV, Haaga DAF, et al. A randomized controlled trial on effects of the transcendental meditation program on blood pressure, psychological distress, and coping in young adults. American journal of hypertension. 2009;22:1326–1331. doi: 10.1038/ajh.2009.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nunes DFT, Rodriguez AL, da Silva Hoffmann F, Luz C. Relaxation and guided imagery program in patients with breast cancer undergoing radiotherapy is not associated with neuroimmunomodulatory effects. J Psychosom Res. 2007;63:647–655. doi: 10.1016/j.jpsychores.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 67.Oken B, Kishiyama S, Zajdel D, et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004;62:2058. doi: 10.1212/01.wnl.0000129534.88602.5c. [DOI] [PubMed] [Google Scholar]
- 68.Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Treating fibromyalgia with mindfulness-based stress reduction: Results from a 3-armed randomized controlled trial. Pain. 2010;2:361–369. doi: 10.1016/j.pain.2010.10.043. [DOI] [PubMed] [Google Scholar]
- 69.Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med. 1998;21:581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- 70.Sloman R. Relaxation and imagery for anxiety and depression control in community patients with advanced cancer. Cancer Nurs. 2002;25:432. doi: 10.1097/00002820-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 71.Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: The effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62:613. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 72.Stein TR, Olivo EL, Grand SH, Namerow PB, Costa J, Oz MC. A pilot study to assess the effects of a guided imagery audiotape intervention on psychological outcomes in patients undergoing coronary artery bypass graft surgery. Holist Nurs Pract. 2010;24:213. doi: 10.1097/HNP.0b013e3181e90303. [DOI] [PubMed] [Google Scholar]
- 73.Stenlund T, Birgander LS, Lindahl B, Nilsson L, Ahlgren C. Effects of qigong in patients with burnout: A randomized controlled trial. J Rehabil Med. 2009;41:761–767. doi: 10.2340/16501977-0417. [DOI] [PubMed] [Google Scholar]
- 74.Taneja I, Deepak K, Poojary G, Acharya I, Pandey R, Sharma M. Yogic versus conventional treatment in diarrhea-predominant irritable bowel syndrome: A randomized control study. Appl Psychophysiol Biofeedback. 2004;29:19–33. doi: 10.1023/b:apbi.0000017861.60439.95. [DOI] [PubMed] [Google Scholar]
- 75.Tsai JC, Wang WH, Chan P, et al. The beneficial effects of tai chi chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. The Journal of Alternative & Complementary Medicine. 2003;9:747–754. doi: 10.1089/107555303322524599. [DOI] [PubMed] [Google Scholar]
- 76.Williams JMG, Alatiq Y, Crane C, et al. Mindfulness-based cognitive therapy (MBCT) in bipolar disorder: Preliminary evaluation of immediate effects on between-episode functioning. J Affect Disord. 2008;107:275–279. doi: 10.1016/j.jad.2007.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Banerjee B, Vadiraj HS, Ram A, et al. Effects of an integrated yoga program in modulating psychological stress and radiation-induced genotoxic stress in breast cancer patients undergoing radiotherapy. Integrative Cancer Therapies. 2007;6:242. doi: 10.1177/1534735407306214. [DOI] [PubMed] [Google Scholar]
- 78.John PJ, Sharma N, Sharma CM, Kankane A. Effectiveness of yoga therapy in the treatment of migraine without aura: A randomized controlled trial. Headache: The Journal of Head and Face Pain. 2007;47:654–661. doi: 10.1111/j.1526-4610.2007.00789.x. [DOI] [PubMed] [Google Scholar]
- 79.Kondwani K, Schneider R, Alexander C, et al. Left ventricular mass regression with the transcendental meditation technique and a health education program in hypertensive African Americans. Journal of Social Behavior and Personality. 2005;17:181. [Google Scholar]
- 80.Ljótsson B, Andréewitch S, Hedman E, Rück C, Andersson G, Lindefors N. Exposure and mindfulness based therapy for irritable bowel syndrome-an open pilot study. J Behav Ther Exp Psychiatry. 2010;41:185–190. doi: 10.1016/j.jbtep.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 81.Rao MR, Raghuram N, Nagendra HR, et al. Anxiolytic effects of a yoga program in early breast cancer patients undergoing conventional treatment: A randomized controlled trial. Complement Ther Med. 2009;17:1–8. doi: 10.1016/j.ctim.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 82.Vadiraja HS, Raghavendra RM, Nagarathna R, et al. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: A randomized controlled trial. Integrative Cancer Therapies. 2009;8:37. doi: 10.1177/1534735409331456. [DOI] [PubMed] [Google Scholar]
- 83.Wu WH, Bandilla E, Ciccone DS, et al. Effects of qigong on late-stage complex regional pain syndrome. Altern Ther Health Med. 1999;5:45–54. [PubMed] [Google Scholar]
- 84.Gross CR, Kreitzer MJ, Reilly-Spong M, et al. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: A randomized controlled clinical trial. Explore: The Journal of Science and Healing. 2011;7:76–87. doi: 10.1016/j.explore.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Smith C, Hancock H, Blake-Mortimer J, Eckert K. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complement Ther Med. 2007;15:77–83. doi: 10.1016/j.ctim.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 86.Sheppard WD, II, Frank J, Jr, John L. The effects of a stress management program in a high security government agency. Anxiety, Stress, Coping. 1997;10:341–350. [Google Scholar]
- 87.Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011] The Cochrane Collaboration. 2011 [Google Scholar]
- 88.Dakwar E, Levin FR. The emerging role of meditation in addressing psychiatric illness, with a focus on substance use disorders. Harv Rev Psychiatry. 2009;17:254–267. doi: 10.1080/10673220903149135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Straus JL, von Ammon Cavanaugh S. Placebo effects. Issues for clinical practice in psychiatry and medicine. Psychosomatics. 1996;37:315. doi: 10.1016/S0033-3182(96)71544-X. [DOI] [PubMed] [Google Scholar]


