Abstract
BACKGROUND:
Although seasonal variation in hospitalizations due to chronic heart failure is recognized, the possible contributors to such variability are less well documented.
METHODS:
Records from all admissions to 12 hospitals in Hubei province, China, over a 10-year period with diagnostic codes for chronic systolic heart failure (CSHF) were reviewed. A total of 16,145 patients with CSHF were analyzed.
RESULTS:
There was a marked seasonal variation in the number of hospitalizations due to CSHF, with two peaks in the monthly rate of hospitalization due to CSHF occurring in December and August compared with the spring and autumn months. Monthly hospitalizations due to CSHF for patients with New York Heart Association class III and IV ranged from a peak of 40.4% and 23.3% above average in December and August, respectively, to 18.6% below average in November, while hospitalizations due to CSHF for patients with New York Heart Association class I and II exhibited no obvious seasonal variation. Blood sodium level (95% CI 2.132 to 2.144; P=0.036) was an independent risk factor for hospitalizations due to CSHF in August.
CONCLUSION:
The number of hospitalizations due to CSHF increased during the colder and warmer months in China. A low blood sodium level was associated with the peak in hospitalizations in August.
Keywords: Blood sodium, Cardiac function, Chronic systolic heart failure, Hospitalization, Seasonal variation
Chronic systolic heart failure (CSHF) remains the only cardiovascular disease with an increasing hospitalization burden, and represents an ongoing drain on health care expenditures. One study reported that CSHF is the cause of at least 20% of all hospital admissions among individuals older than 65 years of age (1). Hospitalization of patients with CSHF represents approximately three-quarters of the total treatment costs for heart failure (2,3). Despite advances in the control of cardiovascular diseases, such as myocardial infarction (MI), the incidence and prevalence of CSHF continue to increase.
Seasonal variations in the incidence of MI and blood pressure are well recognized (4–6). Recently, several investigators have documented seasonal variations in the rate of hospitalization for heart failure in temperate climates (7–10). More admissions were found to occur in the cold (winter) season. However, the potential mechanisms underlying these seasonal patterns are not well elucidated. It is possible that seasonal variations in cardiovascular function are related to factors other than temperature change. The aim of the present study was to describe the seasonal variations in hospitalizations due to CSHF and to examine possible contributors to such variability.
METHODS
Study population
A retrospective study was conducted that included patients referred to the cardiology departments of 12 hospitals in Hubei province, China, between January 2000 and December 2009. For the purpose of the current study, all hospitalizations associated with a discharge diagnosis (in any diagnostic position) of CSHF were examined.
Hospitalization data
Hospitalizations are reported from the first listed discharge diagnosis. Inclusion criteria were echocardiographic evidence of a left ventricular ejection fraction <50% and a diagnosis of CSHF. Patients were excluded if they had acute MI or acute heart failure on admission. Information obtained included admission time, age, sex, body mass index (BMI), complete blood count and biochemical investigations. The data of 16,145 patients were analyzed using Epi Info software (Centers for Disease Control and Prevention, USA). The number of hospitalizations for these diagnoses was calculated separately for each calendar month and according to New York Heart Association (NYHA) functional class.
Seasonal variation
Climatic patterns in seasonality were assessed by plotting the estimated amplitudes of temperatures in January and December in Hubei province. The mean number of hospitalizations for each month was determined to study the seasonal variation in CSHF hospitalizations.
Statistic analysis
Total seasonal variations were measured as the sum of the percentage above the mean for the month with the highest value and the percentage below the mean for the month with the lowest value. The χ2 test was used to compare discrete variables. A logarithmic conversion was performed for variables with non-normal distribution such as blood sodium levels. Independent predictors of hospitalization were examined using a logistic multivariate stepwise regression analysis that included all variables. All statistical tests were evaluated with the use of two-tailed 95% CIs; P<0.05 was considered to be statistically significant. SPSS version 15 (SPSS Inc, USA) for Windows (Microsoft Corporation, USA) was used for data analysis.
RESULTS
General trends
The meteorological data of Hubei province shows that the annual average temperature is 18°C. Figure 1 presents the absolute difference between the annual average and each monthly average temperature from April to March. Peaks were observed in the summer (July and August) and winter (January) (Figure 1).
Figure 1).
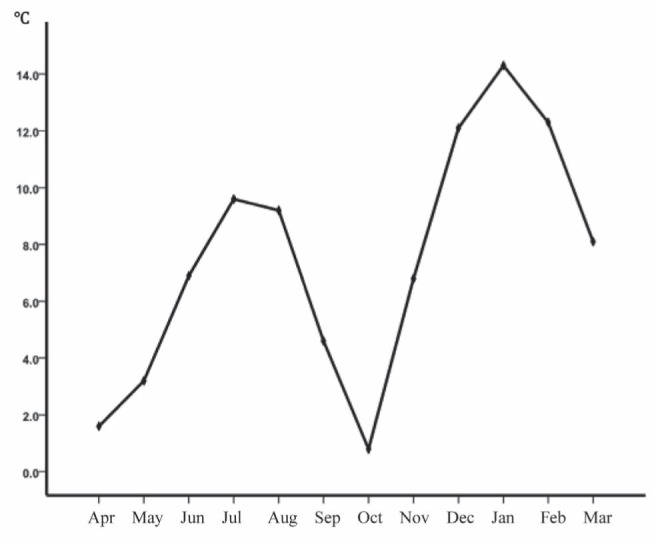
The absolute difference between annual average and monthly average temperatures from April (Apr) to March (Mar) in Hubei Province. The curve shows that there are two peaks in summer (July [Jul] and August [Aug]) and winter (January [Jan]). Jun June; Sep September; Oct October; Nov November; Dec December; Feb February
Figure 2 shows the average number of CSHF-related hospitalizations per month between 2000 and 2009. There was a marked seasonal variation, with two peaks in the monthly rate of hospitalization occurring in the winter and summer months compared with the spring and autumn months. For example, peaks occurred in December (1745 hospitalizations, 29.7% higher than average; P<0.01) and August (1589 hospitalizations, 18.1% higher than average; P<0.01), whereas the lowest rate occurred in November (1039 hospitalizations, 22.8% lower than average; P<0.01). The seasonal variation resulted in an absolute difference of 706 and 550 hospitalizations, comparing the hospital activity in November to that of December and August (1039 versus 1745; 1039 versus 1589) during the entire 10-year period.
Figure 2).
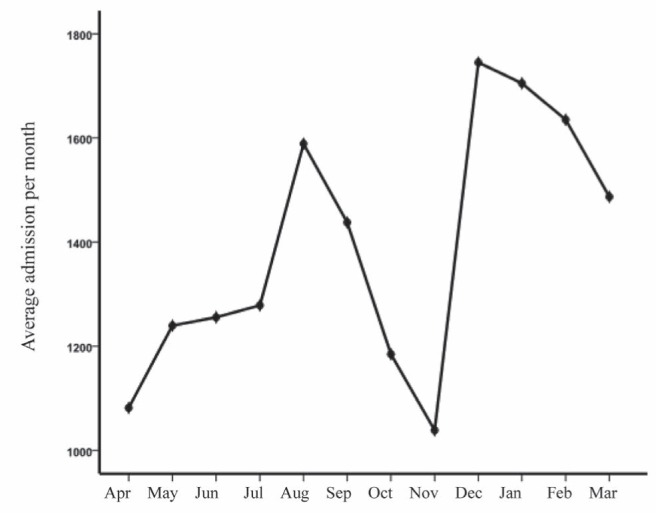
The summed average number of chronic systolic heart failure-related hospitalizations per month during the entire study period, showing a marked seasonal variation, with two peaks in the monthly rate of hospitalization occurring in the winter and summer months compared with the spring and autumn months. Apr April; Aug August; Dec December; Feb February; Jan January; Jul July; Jun June; Sep September; Oct October; Nov November; Mar March
Subgroups
In subgroups defined by NYHA functional class, the distribution of cumulative monthly hospitalizations was similar in the timing of the peaks. Peaks in hospitalizations due to CSHF were observed in January and August for individuals with NYHA functional class III and IV. Monthly CSHF hospitalizations for patients with NYHA functional class III and IV differed by as much as 59% (the largest total seasonal variation), ranging from a peak of 40.4% above average in January and 23.3% above average in August to 18.6% below average in November. However, numbers of CSHF-related hospitalizations for NYHA functional class I and II exhibited no obvious seasonal variation (Figure 3).
Figure 3).
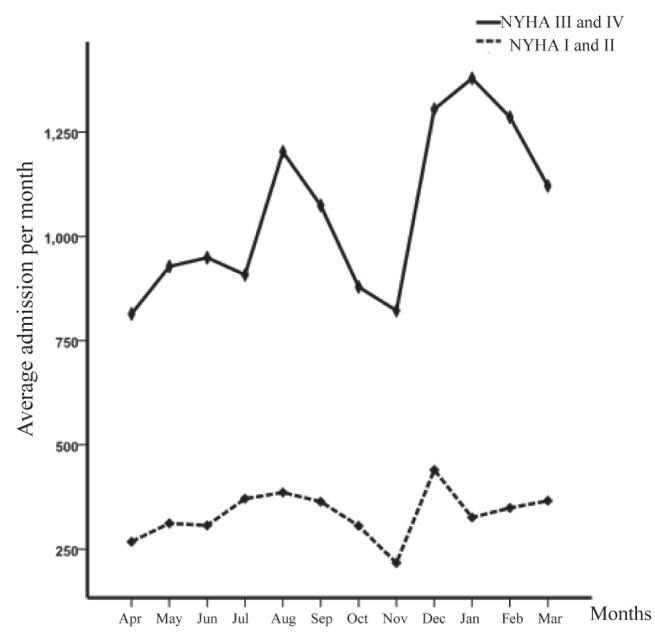
Monthly hospital admissions for chronic systolic heart failure with New York Heart Association (NYHA) functional class III or IV and I or II. Results shows that hospitalization peaks occurred in January and August for persons with NYHA functional class III and IV, while numbers of chronic systolic heart failure-related hospitalizations for NYHA functional class I and II exhibited no obvious seasonal variation. Apr April; Aug August; Dec December; Feb February; Jan January; Jul July; Jun June; Sep September; Oct October; Nov November; Mar March
Factors associated with seasonality in hospitalizations
Figure 4 shows the summed average levels of serum sodium in CSHF-related hospitalizations per month during the entire study period. Levels of serum sodium were lowest in August. To determinate the association of factors with hospitalization peaks, multivariate Cox regression analysis was used. A significant difference was observed in the blood sodium levels between patients hospitalized in August compared with other months. The results showed that blood sodium levels were the independent risk factor for hospitalizations in August (95% CI 2.132 to 2.144; P=0.036) (Table 1). However, there were no significant differences in mean BMI and heart rate in patients with CSHF-related hospitalizations per month during the entire study period.
Figure 4).
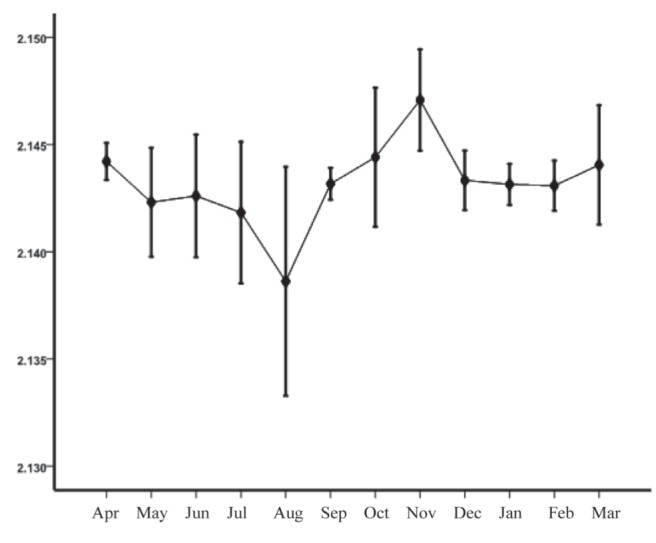
The summed monthly average serum sodium levels in patients hospitalized for chronic systolic heart failure during the entire study period. Serum sodium levels were lowest in August. Apr April; Aug August; Dec December; Feb February; Jan January; Jul July; Jun June; Sep September; Oct October; Nov November; Mar March
TABLE 1.
The characteristics of all patients and the multivariate Cox regression analysis for patient hospitalizations in August
| Demographic and clinical variables | All patients, n=16,145 | Patients in August, n=1589 | |||
|---|---|---|---|---|---|
|
|
|
||||
| Median or % | IQR | Median or % | IQR | HR (95% CI); P | |
| Age, years | 66 | 58–74 | 67 | 59–74 | NS |
| Female, % | 40.1 | 39.3 | NS | ||
| Heart rate, beats/min | 82 | 71–97 | 84 | 72–97 | NS |
| New York Heart Association class III or IV, % | 75.7 | 77.6 | NS | ||
| Body mass index, kg/m2 | 23.1 | 20.1–25.6 | 23.2 | 20.2–25.5 | NS |
| White blood cells, ×109/L | 6.4 | 5.1–7.8 | 6.3 | 5.1–7.7 | NS |
| Red blood cells, ×1012/L | 4.2 | 3.7–4.5 | 4.1 | 3.7–4.4 | NS |
| Sodium, mmol/L | 140.1 | 136.4–142.4 | 134.2 | 132.4–140.2 | 2.138 (2.132–2.144); 0.036 |
| Potassium, mmol/L | 4.1 | 3.64–4.4 | 3.9 | 3.64–4.2 | NS |
| Creatinine, μmol/L | 89.3 | 72.2–116 | 90.5 | 73.7–112.3 | NS |
| Total cholesterol, mmol/L | 3.9 | 3.28–4.6 | 3.92 | 3.29–4.6 | NS |
| Left atrial end-diastolic diameter, mm | 42 | 40–44 | 41 | 40–44 | NS |
| Left ventricular end-diastolic diameter, mm | 54 | 44–59 | 56 | 46–59 | NS |
| Left ventricular ejection fraction,% | 34 | 23–42 | 35 | 24–42 | NS |
Results showed that blood sodium levels were the independent risk factor for hospitalizations in August. HR Hazard ratio; IQR Interquartile range; NS Not statistically significant
DISCUSSION
The major and novel findings of the present study are that hospitalizations for CSHF in Hubei province public hospitals followed a similar seasonal pattern, with a winter-summer predominance. NYHA functional class III and IV was associated with seasonality in hospitalizations, while NYHA functional class I and II had no obvious seasonal variation. Low blood sodium level was an independent predictor of hospitalizations for CSHF in August.
Seasonal variation in hospitalization for heart failure, with a peak in the winter season, has been reported as a consequence of cardiac decompensation (7–12). Potential mechanisms underlying a seasonal pattern include the presence of other conditions with a well-known seasonal variation: respiratory tract infections, MI, high blood pressure and sudden death (13–16). Studies have documented an increase in respiratory and cardiovascular morbidity during winter (17). During winter months, hemodynamic changes are more accentuated and adverse events are triggered by low temperatures, in which the sympathetic nervous system appears to play an important role. In the present study, we not only found that there was a statistically significant increase in hospitalizations for CSHF during the colder months, but there was a statistically significant increase in the hospital admission numbers in the warmer months. What are the potential mechanisms underlying the apparent paradox of increased hospitalizations for CSHF in the hot summer in Hubei, China? There may be a number of reasons for this observed difference. During exposure to a hyperthermic environment, systemic vascular resistance normally decreases due to cutaneous vasodilation. Cardiac output must increase to maintain blood pressure. Patients with CSHF may not achieve an increase of cardiac output. During heat stress in patients with CSHF, either blood pressure will not be maintained or the skin will not be adequately vasodilated to enable thermoregulation, the latter of which will increase the risk for heat-related injuries (18). Oktay et al (20) and Koken et al (19) reported that higher temperatures appear to be an important factor in increasing the frequency of hospitalization for CSHF, and also reported a significant increase in the percentage of CSHF visits admitted to emergency departments during the warmer months. The majority of the previous reports showing that the hospitalizations for CSHF were higher in winter and lower in summer were investigated in developed countries (7–12). However, China is a developing country. Whether the different occupations, economic conditions or etiologies had influence on our results is unknown.
We analyzed the complete blood count and blood biochemical indexes to determinate the relationship of these factors with hospitalization peaks. We also divided patients into subgroups defined by NYHA functional class and BMI. Interestingly, we found hospitalization peaks were observed in January and August for individuals with NYHA functional class III and IV, while NYHA functional class I and II exhibited no obvious seasonal variation. In addition, there was a significant reduction in blood sodium levels of patients hospitalized in August compared with other months. Studies have demonstrated that approximately one-fifth of the winter excess of hospitalizations could be accounted for by the seasonal increase in respiratory disease. Respiratory infections, especially those related to influenza, are more frequent in winter and could precipitate CSHF (21). Patients with pulmonary vascular congestion due to left ventricular failure are more susceptible to pulmonary infection compared with healthy individuals. We speculate that patients with NYHA functional class III and IV were affected by respiratory infections more frequently than patients with NYHA functional class I and II. In China, many patients lived in climate-uncontrolled buildings, and workers and farmers accounted for many of the patients. Therefore, these patients experienced longer exposures to higher temperature in summer. In addition, many patients continued to take diuretics, and seldom measured the levels of blood electrolytes. Exposure to a hyperthermic environment and sweating may aggravate the side effect of diuretics and induce electrolyte imbalance.
There are several clinical implications of these findings. Along with previous reports, these findings provide evidence for increasing the intensity of CSHF-management strategies before periods with expected higher event rates. Our results further emphasize the burden of CSHF borne by the hospital system during the summer months and warrant consideration of the potential cost-savings of alternative strategies to reduce this financial and resource burden. Such strategies must be aimed at reducing the vulnerability of these patients to the warmest weather and resultant electrolyte imbalances in China.
Study limitations
There are a number of limitations to the present study that require comment. First, to minimize the impact of varying diagnostic criteria among different doctors and services, the cases had to fulfill well-defined inclusion criteria, which were strict and clinically recognizable. However, it is conceivable that these criteria, while increasing specificity, could have reduced sensitivity. Second, it is likely that we missed some CSHF-related events in this cohort or that these had been classified as all-cause admissions. Therefore, the number of hospitalizations for individuals with a diagnosis of CSHF does not necessarily represent the prevalence of heart failure cases. Finally, we did not investigate the seasonal variations in CSHF-related mortality. Whether hospitalization peaks in summer can increase the mortality in China should be further investigated.
Footnotes
CONFLICT OF INTEREST: The authors have no conflicts of interest to declare.
REFERENCES
- 1.Lloyd-Jones D, Adams R, Carnethon M, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics – 2009 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 2.Stewart S. Financial aspects of heart failure programs of care. Eur J Heart Fail. 2005;7:423–8. doi: 10.1016/j.ejheart.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? Europace. 2011;13(Suppl 2):ii13–7. doi: 10.1093/europace/eur081. [DOI] [PubMed] [Google Scholar]
- 4.Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second national registry of myocardial infarction. J Am Coll Cardiol. 1998;31:1226–33. doi: 10.1016/s0735-1097(98)00098-9. [DOI] [PubMed] [Google Scholar]
- 5.Marchant B, Ranjadayalan K, Stevenson R, Wilkinson P, Timmis AD. Circadian and seasonal factors in the pathogenesis of acute myocardial infarction: The influence of environmental temperature. Br Heart J. 1993;69:385–7. doi: 10.1136/hrt.69.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J. 1982;285:919–23. doi: 10.1136/bmj.285.6346.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boulay F, Berthier F, Sisteron O, Gendreike Y, Gibelin P. Seasonal variation in chronic heart failure hospitalizations and mortality in France. Circulation. 1999;100:280–6. doi: 10.1161/01.cir.100.3.280. [DOI] [PubMed] [Google Scholar]
- 8.Stewart S, McIntyre K, Capewell S, McMurray JJ. Heart failure in a cold climate. Seasonal variation in heart failure-related morbidity and mortality. J Am Coll Cardiol. 2002;39:760–6. doi: 10.1016/s0735-1097(02)01685-6. [DOI] [PubMed] [Google Scholar]
- 9.Martínez-Sellés M, García Robles JA, Prieto L, et al. Annual rates of admission and seasonal variations in hospitalizations for heart failure. Eur J Heart Fail. 2002;4:779–86. doi: 10.1016/s1388-9842(02)00116-2. [DOI] [PubMed] [Google Scholar]
- 10.Gotsman I, Zwas D, Admon D, Lotan C, Keren A. Seasonal variation in hospital admission in patients with heart failure and its effect on prognosis. Cardiology. 2010;117:268–74. doi: 10.1159/000323511. [DOI] [PubMed] [Google Scholar]
- 11.Gallerani M, Boari B, Manfredini F, Manfredini R. Seasonal variation in heart failure hospitalization. Clin Cardiol. 2011;34:389–94. doi: 10.1002/clc.20895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Inglis SC, Clark RA, Shakib S, et al. Hot summers and heart failure: Seasonal variations in morbidity and mortality in Australian heart failure patients (1994–2005) Eur J Heart Fail. 2008;10:540–59. doi: 10.1016/j.ejheart.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Ornato JP, Peberdy MA, Chandra NC, Bush DE. Seasonal pattern of acute myocardial infarction in the National Registry of Myocardial Infarction. J Am Coll Cardiol. 1996;7:1684–8. doi: 10.1016/s0735-1097(96)00411-1. [DOI] [PubMed] [Google Scholar]
- 14.Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J Am Coll Cardiol. 1998;31:1226–33. doi: 10.1016/s0735-1097(98)00098-9. [DOI] [PubMed] [Google Scholar]
- 15.Arnt HR, Willich SN, Schreiber C, Brüggemann T, Stern R, Schultheiss HP. Diurnal, weekly and seasonal variation of sudden death. Population-based analysis of 24,061 consecutive cases. Eur Heart J. 2000;21:315–20. doi: 10.1053/euhj.1999.1739. [DOI] [PubMed] [Google Scholar]
- 16.Barnett AG, de Looper M, Fraser JF. The seasonality in heart failure deaths and total cardiovascular deaths. Aust N Z J Public Health. 2008;32:408–13. doi: 10.1111/j.1753-6405.2008.00270.x. [DOI] [PubMed] [Google Scholar]
- 17.The Eurowinter Group Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet. 1997;349:1341–6. [PubMed] [Google Scholar]
- 18.Arbab-Zadeh A, Crandall CG, Levine BD. Thermoregulation in patients with cardiac disease. J Cardiopulm Rehab. 2002;22:38–9. doi: 10.1097/00008483-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Koken PJ, Piver WT, Ye F, Elixhauser A, Olsen LM, Portier CJ. Temperature, air pollution, and hospitalization for cardio-vascular diseases among elderly people in Denver. Environ Health Perspect. 2003;111:1312–7. doi: 10.1289/ehp.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oktay C, Luk JH, Allegra JR, Kusoglu L. The effect of temperature on illness severity in emergency department congestive heart failure patients. Ann Acad Med Singapore. 2009;38:1081–4. [PubMed] [Google Scholar]
- 21.Fleming DM. The contribution of influenza to combined acute respiratory infections, hospital admissions, and deaths in winter. Commun Dis Public Health. 2000;3:32–8. [PubMed] [Google Scholar]


