Abstract
While placement of ink into the skin is a long-standing tradition, patients are now seeking tattoo removal on a more frequent basis. Once considered acceptable removal options, tattoo ink removal via physical destruction included dermabrasion, chemical destruction, salabrasion, thermal destruction, and cryotherapy. Now these options are used extremely infrequently. These modalities provided unpredictable results and often required prolonged healing times and left patients with skin discoloration, pain, scarring, and ink retention. Even the widely adopted use of lasers, now considered the gold standard method, offers some level of unpredictability surrounding the natural progression of ink resolution. Multiple factors need to be taken into consideration when successfully removing tattoo pigment including the modalities used, number and frequency of treatments, proper device technique, and physiological barriers to tattoo removal. This paper serves to elucidate the common causes of ink retention following tattoo removal treatment with recommendations on how best to address this relatively common occurrence.
Clinicians with ample experience performing tattoo removal procedures are aware that there is some level of unpredictability surrounding the natural progression of ink resolution. While some patients may only want to fade a tattoo, the vast majority desire complete resolution of their tattoo ink. Yet, patients will occasionally experience unanticipated ink retention following the tattoo removal treatment. The authors define unanticipated ink retention as visible tattoo pigment that has remained after tattoo removal treatments have been performed. Several factors to consider include the modalities used, number and frequency of treatments, proper device technique, and physiological barriers to ink removal. This paper serves to elucidate the common causes of ink retention following tattoo removal treatment with recommendations on how best to alleviate this complication.
MODALITIES USED
Physical modalities for tattoo removal. Older methods of removing unwanted tattoo ink that were once considered acceptable options included dermabrasion,1-3 chemical destruction,4-7 salabrasion,8,9 thermal destruction,10 and cryotherapy (Table 1).11,12 These physically destructive modalities provided unpredictable results, required prolonged healing times, and frequently left patients with skin discoloration, pain, scarring, and ink retention. It is recommended that these physical modalities no longer be used given the availability of better technologies (i.e., quality-switched lasers) for tattoo removal.
TABLE 1.
Description of physical modalities
| Chemical destruction: puncture or incision of the skin with subsequent application of tannic acid and/or silver nitrate to tattoo; phenol solution or trichloracetic acid application to the tattoo |
| Cryosurgery: liquid nitrogen application to the tattoo |
| Dermabrasion: use of a rapidly spinning wheel or wire brush to abrade the skin |
| Salabrasion: abrading superficial dermis with common table salt and abrasive pad |
| Thermal destruction: use of thermal cautery, electrocautery, or infrared coagulation to destroy tattoo pigment |
Light-based (non-quality-switched laser) techniques for tattoo removal. In the late 1970s and 1980s, continuous wave lasers, in particular the argon13 and carbon dioxide laser14-18 were used to treat unwanted tattoo ink. Although these devices did target tattoo ink, due to their nonselective ablative properties, they were also frequently associated with unfavorable tissue texture changes, hypertrophic scarring, and ink retention. Although very rarely used for tattoo removal today, occasionally a physician will still attempt to remove tattoo ink with a continuous wave device.
Intense pulsed light (IPL) devices have been unsuccessful as a tattoo ink removal option. These devices are commonly used for hair reduction treatment and photo rejuvenation. Because of their nonselective destruction (i.e., range of wavelengths) and longer pulse duration, the light intensities associated with this device is not sufficient or specific to destroy tattoo ink.19 The pulse duration of an IPL device is in the milliseconds, which is in contrast to the quality-switched lasers whose duration is in the nanosecond range. In addition, when tattoo ink particles are exposed to IPL, they conduct heat to adjacent skin, further leading to scarring and discoloration. Unfortunately, all too often, novice healthcare practitioners erroneously attempt to remove tattoo ink with an IPL device causing scarring and ink retention. It is recommended that neither continuous wave nor IPL light devices be used for tattoo removal.
NUMBER AND FREQUENCY OF TREATMENTS
Number of treatments needed. It is well established that multiple laser treatments are required to remove a tattoo. Unfortunately, not all practitioners provide patients with accurate information at the time of the initial consultation including the estimated number of total treatments to achieve complete ink resolution and all too often “guess work” takes place. Moreover, patients without a thorough understanding of the process may not be compliant with their return appointments, leading to patient dissatisfaction and improper stigmatization of the removal process. In 2009, the Kirby-Desai Scale was proposed as a tool to estimate the number of treatments needed for laser tattoo removal assuming the medical practitioner is using a quality-switched laser device (Figure 1).20 The scale calculates the estimated number of treatments based on a standardized set of parameters, such as the patient’s skin type, location of the tattoo, and number and density of tattoo inks used.20 This scale is now used by clinicians during the initial patient presentation to provide a more accurate estimation as to the number of treatments required for complete tattoo removal than was previously available. By educating patients about the likely necessary number of treatments required, patients are much more inclined to complete the entire recommended course of treatment and minimize the incidence of ink retention.
Figure 1.
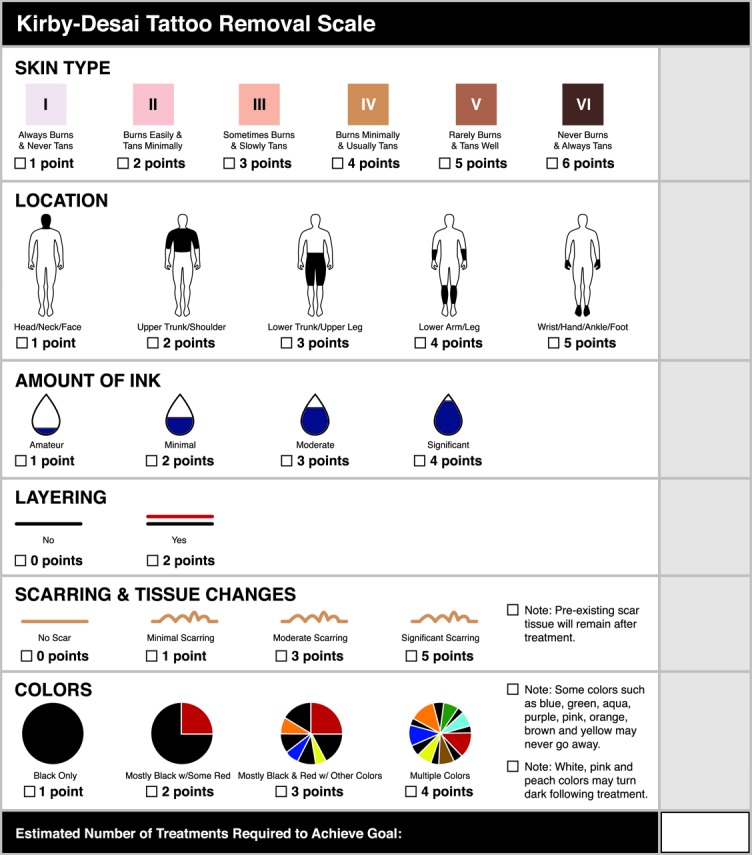
The Kirby Desai Scale
Frequency of treatments. In addition to the number of treatments needed for tattoo removal, incorrect intervals between treatments may be another factor that contributes to unanticipated ink retention. Patients seeking tattoo removal desire that the ink be removed as quickly as possible as it is a common misconception that decreasing treatment intervals will increase ink resolution. Adequate time between treatments, however, is necessary to allow for ink resolution. It has been reported that treatment intervals of one month could interfere with the activity of macrophages.21,22 Moreover, it is commonly noted that treating too frequently may increase the rate of side effects including scarring and ink retention. Many dermatologists are now recommending a minimum of eight weeks between laser treatments.23 Even longer intervals should be considered for patients who are experiencing tissue texture changes, who are likely to experience skin discoloration, or who have little ink remaining.
Thus patients with complaints of ink retention may have simply not been properly informed of the estimated number of treatments or frequency of intervals, which warrants re-education and additional treatments if ink retention occurs. It is recommended that patients be informed of the estimated number of treatments and frequency of intervals needed prior to removal to avoid the complication of ink retention.
DEVICE TECHNIQUE
Q-switched laser treatment has become widely adopted and is considered the gold standard treatment option for the removal of unwanted tattoo ink (Figure 2). Q-switched lasers are based upon the theory of selective photothermolysis, whereby a single wavelength at a particular fluence and pulsed duration can selectively target exogenous pigment in tattoos with minimal damage to the surrounding skin.24 “Q” refers to a quality factor for light traveling across the laser cavity, which can be changed suddenly to produce a short, intense burst of light. Q-switched lasers produce short pulses at very high peak power and are designed to produce pulses in the nanosecond range.25
Figure 2.
Status post-tattoo removal on showing excellent ink resolution and minimal, transient hyperpigmentation
Some clinicians are also using lasers with pulsed durations in the picoseconds range with variable results.26-28 Currently, the only picosecond device available is in a 755nm wavelength of light, and while some practitioners theorize that the picosecond speed may reduce the overall number of treatments needed to remove a tattoo, to date no large-scale studies or head-to-head unit comparisons have been performed with these devices proving improved efficacy when compared to Q-switched devices.
In addition to selecting the proper laser, routine maintenance and calibration is an imperative part of successful tattoo removal. A series of mirrors amplify photons in lasers, and the medium that the laser passes through determines the wavelength of the emitted light.29
Minor displacement of these mirrors through purposeful movement, accidental jarring, and even routine use may alter the efficacy of the treatment. If significant movement of the device has occurred, the laser device should be recalibrated. Additionally, routine maintenance should be performed at the intervals recommended by the manufacturer to ensure that the laser is operating with proper specifications. Lenses and hand pieces should also be cleansed with appropriate solvents and replaced when necessary. Regrettably, patients experiencing iatrogenic ink retention after treatment may have been treated with a poorly calibrated or poorly maintained device.
PHYSIOLOGICAL BARRIERS TO TATTOO INK REMOVAL
Undesired pigmentary alteration misdiagnosed as ink retention. Transient hyperpigmentation following Q-switched treatment is a well-established phenomenon upon complete resolution of tattoo ink following laser treatment.30,31 Patients and novice practitioners may occasionally confuse this hyperpigmentation with ink retention. Continued exposure to laser light may only prolong this transient hyperpigmentation, and thus treatments should cease once tattoo ink has resolved completely or at least improved significantly. Prolonging the intervals between treatments, topical hydroquinone, and sun avoidance measures should be considered for any patient that confuses undesired pigment alterations with ink retention.32
Paradoxical ink darkening as a cause of ink retention. Paradoxical darkening of tattoo ink can occur after Q-switched treatment and has been reported in multiple ink colors.33,34 Certain colors including yellow, white, peach, or pink35 may be susceptible to paradoxical ink darkening secondary to reduction of ferric oxide to ferrous oxide, which leads to a darkening of the ink. Another possibility to explain paradoxical ink darkening may be the Tyndall effect, since tattoo pigments are found in the dermis.33,34
Tattoos that experience paradoxical darkening often require additional treatments to obtain complete ink resolution,35 but the newly darkened ink may also be an unfortunate permanent consequence.36 Paradoxical ink darkening can be a contributing factor to ink retention and patients who will likely experience this phenomenon should be forewarned of the possibility that ink retention is a possibility following paradoxical color changes with particular tattoo colors.
Tattoo ink used does not respond to wavelength of light as anticipated. Numerous tattoo ink formulations are now available.30 Although many inks respond to laser treatment as anticipated, some tattoo ink formulations are recalcitrant to treatment.37 The most common tattoo ink color is black and the wavelength of light used most frequently to treat this color is 1064nm. Other tattoo colors appear frequently and wavelengths including 532nm, 694nm, and 755nm as well as attachable hand pieces with 585nm and 650nm wavelengths are available (Table 2). Tattoo artists will mix colors and ingredients38 and acknowledge that the formulations themselves are not uniform, frequently change, and are poorly regulated.39,40 Given the variability of these pigments, tattoo ink will occasionally present that does not respond to the treatment as predicted. In these cases, patients may experience ink retention and require more treatment sessions than originally anticipated. Clinicians may need to use more than one wavelength of light in these cases.
TABLE 2.
Selected tattoo colors and commonly used lasers for removal
| COLOR | LASER |
|---|---|
| Red | QS Nd:YAG (532nm) |
| Yellow | QS Nd:YAG (532nm) |
| Green | QS Ruby (694nm), QS and Picosecond Alexandrite (755 nm), QS Nd:YAG (650nm) |
| Blue | QS Ruby (694nm), QS Nd:YAG (1064nm), QS Nd:YAG (585nm) |
| Purple | QS Nd:YAG (532nm) |
| Black | QS Nd:YAG (1064nm) is the standard but QS Ruby (694nm) and QS and Picosecond Alexandrite (755 nm) may be attempted |
| White | QS Nd:YAG (1064nm) |
| Light Brown | QS Nd:YAG (532nm) |
| Dark Brown | QS Nd:YAG (1064nm and 532nm) |
QS=Quality-switched; Nd:YAG=neodymium-doped yttrium aluminum garnet; nm=nanometers
Proper patient selection. While a patient might believe that the laser treatment is the sole reason for tattoo ink reduction, the theory behind this phenomenon also involves the patient’s own immune system. It is hypothesized that these laser-altered residual particles are phagocytosed by the body’s lymphatic system.41
Patients suffering from short- and long-term immunosuppression (i.e., via chemotherapy, drug-induced, or a medical condition) may experience poor healing, which can further lead to ink retention following laser treatments. Individuals presenting with underlying immunosuppression should be referred to the appropriate specialist for comprehensive care. Once the condition has stabilized or resolved, they should be considered appropriate candidates for laser tattoo removal treatment.
CONCLUSION
As with any medical treatment, there is some level of unpredictability with laser tattoo removal. The causes of ink retention following laser tattoo treatment can be placed into categories including the incorrect modalities used, number and frequency of laser treatments, improper device technique, and physiological barriers to ink removal. By understanding the probable reasons behind this phenomenon, the clinician’s ability to provide a patient with more realistic expectations will be enhanced and options to treat this retained ink can be appropriately considered.
ACKNOWLEDGMENTS
The authors would like to thank Ian Kirby and Emily Holmes, RN, for assistance with editing and research.
Footnotes
DISCLOSURE:Drs. Kirby, Chen, and Desai A report no relevant conflicts of interest. Dr. Tejas Desai is an investor and on the medical advisory board of Dr. Tattoff, Inc.
REFERENCES
- 1.Boo-Chai K. The decorative tattoo—its removal by dermabrasion. Plast Reconstr Surg. 1963;32:559. doi: 10.1097/00006534-196311000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Ceilley RI. Curettage after dermabrasion-techniques of removal of tattoos. J Dermatol Surg Oncol. 1979;5:905. doi: 10.1111/j.1524-4725.1979.tb00774.x. [DOI] [PubMed] [Google Scholar]
- 3.Clabaugh WA. Tattoo removal by superficial dermabrasion. Five-year experience. Plast Reconstr Surg. 1975;55(4):401–405. [PubMed] [Google Scholar]
- 4.Van der Velden EM, Van der Walle HB, Groote AD. Tattoo removal: tannic acid method of Variot. Int J Dermatol. 1993;32(5):376–380. doi: 10.1111/j.1365-4362.1993.tb01479.x. [DOI] [PubMed] [Google Scholar]
- 5.Fogh H, Wulf HC, Poulsen T, Larsen P. Tattoo removal by overtattooing with tannic acid. J Dermatol Surg Oncol. 1989;15(10):1089–1090. doi: 10.1111/j.1524-4725.1989.tb03128.x. [DOI] [PubMed] [Google Scholar]
- 6.Piggot TA, Norris RW. The treatment of tattoos with trichloroacetic acid: experience with 670 patients. Br J Plast Surg. 1988;41(2):112–117. doi: 10.1016/0007-1226(88)90036-7. [DOI] [PubMed] [Google Scholar]
- 7.Scutt RW. The chemical removal of tattoos. Br J Plast Surg. 1972;25(2):189–194. doi: 10.1016/s0007-1226(72)80043-2. [DOI] [PubMed] [Google Scholar]
- 8.Crittenden FM. Salabrasion-removal of tattoos by superficial abrasion with table salt. Cutis. 1971;7:295. [Google Scholar]
- 9.Koerber WA, Jr, Price NM. Salabrasion of tattoos. A correlation of the clinical and histological results. Arch Dermatol. 1978;114(6):884–888. doi: 10.1001/archderm.114.6.884. [DOI] [PubMed] [Google Scholar]
- 10.Colver GB, Cherry GW, Dawber RP. Tattoo removal using infrared coagulation. Br JDermaatol. 1985;112(4):481–485. doi: 10.1111/j.1365-2133.1985.tb02324.x. [DOI] [PubMed] [Google Scholar]
- 11.Colver GB, Dawber RP. Tattoo removal using a liquid nitrogen cryospray. Clin Exp Dermatol. 1984;9(4):364–366. doi: 10.1111/j.1365-2230.1984.tb00817.x. [DOI] [PubMed] [Google Scholar]
- 12.Colver GB, Dawber RP. The removal of digital tattoos. Int J Dermatol. 1985;24(9):567–568. doi: 10.1111/j.1365-4362.1985.tb05852.x. [DOI] [PubMed] [Google Scholar]
- 13.Apfelberg DB, Maser MR, Lash H, et al. Comparison of argon and carbon dioxide laser treatment of decorative tattoos: a preliminary report. Ann Plast Surg. 1985;14:61985. doi: 10.1097/00000637-198501000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Mcburney E. Carbon dioxide laser treatment of dermatologic lesions. South Med J. 1978;71:795–797. doi: 10.1097/00007611-197807000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Brady S, Blokmanis A, Jewett L. Tattoo removal with the carbon dioxide laser. Ann Plast Surg. 1978;2:482–490. doi: 10.1097/00000637-197906000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Beacon JP, Ellis H. Surgical removal of tattoos by carbon dioxide laser. J R Soc Med. 1980;73:298. doi: 10.1177/014107688007300418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baffin PL, Ratz JL, Levine HL. Removal of tattoos by CO2 laser. J Dermatol Surg Oncol. 1980;6:997. doi: 10.1111/j.1524-4725.1980.tb01021.x. [DOI] [PubMed] [Google Scholar]
- 18.Reid R, Muller S. Tattoo removal by CO2 laser dermabrasion. Plast Reconstr Surg. 1980;65:717. doi: 10.1097/00006534-198006000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Wenzel S, Landthaler M, Raumler W. Recurring mistakes in tattoo removal: a case series. Dermatology. 2009;218(2):164–167. doi: 10.1159/000182252. [DOI] [PubMed] [Google Scholar]
- 20.Kirby W, Desai A, Desai T. The Kirby—Desai Scale: a proposed scale to assess tattoo-removal treatments. J Clin Aesthet Dermatol. 2009;2(3):32–37. [PMC free article] [PubMed] [Google Scholar]
- 21.Bonnell JA, Russell B. Skin reactions at sites of green and red tattoo marks. Proc R Soc Med. 1956;49:823. [PubMed] [Google Scholar]
- 22.Rudlinger R. Successful removal by ruby laser of darkened ink after ruby laser treatment of mismatched tattoos for acne scars. J Cut Laser Ther. 2000;2:37–39. doi: 10.1080/14628830050516597. [DOI] [PubMed] [Google Scholar]
- 23.Kirby W, Kartono F, Small R. Tattoo removal with lasers. In: Usatine RP, Pfenninger JL, Stulberg DL, Small R, editors. Dermatologic and Cosmetic Procedures in Office Practice. 1st ed. Philadelphia, PA: Elsevier Saunders; 2011. pp. 267–376. [Google Scholar]
- 24.Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Scieence. 1983;220:524–527. doi: 10.1126/science.6836297. [DOI] [PubMed] [Google Scholar]
- 25.Rauln C, Schonermark MP, Greve B, Werner S. Q-switched ruby laser treatment of tattoos and benign pigmented skin lesions: a critical review. Ann Plast Surg. 1998;41:555–565. doi: 10.1097/00000637-199811000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Brauer JA, Reddy KK, Anolik R, et al. Successful and rapid treatment of blue and green tattoo pigment with a novel picosecond laser. Arch Dermatol. 2012;148(7):820–823. doi: 10.1001/archdermatol.2012.901. [DOI] [PubMed] [Google Scholar]
- 27.Ross V, Naseef G, Lin G, et al. Comparison of responses of tattoos to picosecond and nanosecond Q-switched neodymium: YAG lasers. Arch Dermatol. 1998;134(2):167–171. doi: 10.1001/archderm.134.2.167. [DOI] [PubMed] [Google Scholar]
- 28.Saedi N, Metelitsa A, Petrell K, et al. Treatment of tattoos with a picosecond alexandrite laser: a prospective trial. Arch Dermatol. 2012;148(12):1360–1363. doi: 10.1001/archdermatol.2012.2894. [DOI] [PubMed] [Google Scholar]
- 29.Herd RM, Dover JS, Arndt KA. Basic laser principles. Dermatol Clin. 1997;15(3):355–372. doi: 10.1016/s0733-8635(05)70446-0. [DOI] [PubMed] [Google Scholar]
- 30.Kuperman-Beade M, Levine V, Ashinoff R. Laser removal of tattoos. Am J Clin Dermatol. 2001;2:21–25. doi: 10.2165/00128071-200102010-00004. [DOI] [PubMed] [Google Scholar]
- 31.Karsai S, Pfirrmann G, Hammes S, Raulin C. Treatment of resistant tattoos using a new generation Q-switched Nd:YAG laser: influence of beam profile and spot size on clearance success. Lasers Surg Med. 2008;40(2):139–145. doi: 10.1002/lsm.20605. [DOI] [PubMed] [Google Scholar]
- 32.Kirby W, Koriakos A, Desai A, Desai T. Undesired pigmentary alterations associated with quality-switched laser tattoo removal treatment: a retrospective study and review of the literature. Skin & Aging. 2010;18(8):38–40. [Google Scholar]
- 33.Anderson RR, Geronemus R, Kilmer SL, et al. Cosmetic tattoo ink darkening. A complication of Q-switched and pulsed-laser treatment. Arch Dermatol. 1993;129:1010–1014. doi: 10.1001/archderm.129.8.1010. [DOI] [PubMed] [Google Scholar]
- 34.Swanson VS. Tattoo ink darkening of a yellow tattoo after Q-switched laser treatment. Clin Exp Dermatol. 2002;27(6):461–463. doi: 10.1046/j.1365-2230.2002.01070.x. [DOI] [PubMed] [Google Scholar]
- 35.Kirby W, Kaur R, Kartono F, et al. Paradoxical darkening and removal of pink ink tattoo. J Cosmet Dermatol. 2010;9(2):149–151. doi: 10.1111/j.1473-2165.2010.00493.x. [DOI] [PubMed] [Google Scholar]
- 36.Ross E, Yashar S, Michaud N, et al. Tattoo darkening and nonresponse after laser treatment: a possible role for titanium dioxide. Arch Dermatol. 2001;137:33–37. doi: 10.1001/archderm.137.1.33. [DOI] [PubMed] [Google Scholar]
- 37.Sweeney S. Tattoos: a review of tattoo practices and potential treatment options for removal. Curr Opin Pediatr. 2006;19:391–395. doi: 10.1097/01.mop.0000236388.64333.cd. [DOI] [PubMed] [Google Scholar]
- 38.Kaur R, Kirby W, Maibach H. Cutaneous allergic reactions to tattoo ink. J Cosmet Dermatol. 2009;8(4):304–309. doi: 10.1111/j.1473-2165.2009.00469.x. [DOI] [PubMed] [Google Scholar]
- 39.Tope WD. State and territorial regulation of tattooing in the United States. J Am Acad Dermatol. 1995;32(5 Pt 1):791–799. doi: 10.1016/0190-9622(95)91477-3. [DOI] [PubMed] [Google Scholar]
- 40.Armstrong ML. Tattooing, body piercing, and permanent cosmetics: a historical and current view of state regulations, with continuing concerns. J Environ Health. 2005;67(8):38–43,54,53. [PubMed] [Google Scholar]
- 41.Modi S, Stanton AWB, Mortimer PS, Levick JR. Clinical assessment of human lymph flow using removal rate constants of interstitial macromolecules: a critical review of lymphoscintigraphy. Lymphat Res Biol. 2007;5(3):183–202. doi: 10.1089/lrb.2007.5306. [DOI] [PubMed] [Google Scholar]



