Abstract
Background: The absence or loss of elastic fibers in the skin is referred to as dermal elastolysis. Purpose: This paper describes a woman with a distinctive clinical presentation of mid-dermal elastolysis characterized morphologically by multiple horizontal raised bands on the lower back. Methods: A 20-year-old Filipino woman presented with multiple asymptomatic, flesh-colored, raised, firm, linear, cord-like bands on the lumbar area of her back. There were neither similar lesions elsewhere nor a family member with this condition. Results: Microscopic examination of the raised band showed nearly complete absence of elastic fibers in the mid dermis. In contrast, a biopsy of symmetrically located normal-appearing skin showed a uniform distribution of elastic fibers throughout the dermis. Linear lumbar localized elastolysis is a descriptive designation that accurately reflects a correlation of the clinical and pathological changes of this condition. Conclusion: The clinical differential of raised horizontal cord-like bands on the lower back (without a family history of an inherited elastic fiber disorder, a prior history of trauma, or a significant change in weight or exercise habit) includes linear focal elastosis and linear lumbar localized elastolysis. Microscopic evaluation of a Verhoeff-van Gieson stained lesion specimen (which may be accompanied by a biopsy of normal-appearing skin for comparison) will readily differentiate these conditions. The former is usually characterized by increased elastic fibers, whereas the latter, as in this patient, shows a paucity or absence of elastic fibers in the mid dermis.
Elastolysis refers to the loss of elastic fibers in the dermis. The clinical presentation of skin lesions in patients with elastolysis correlates with the location in the dermis where there is a paucity or absence of elastic fibers. The authors describe a young woman with a unique clinical presentation of mid-dermal elastolysis characterized by multiple asymptomatic, firm, raised, flesh-colored horizontal bands on her lower back: linear lumbar localized elastolysis.
CASE REPORT
A 20-year-old healthy Filipino woman presented with multiple asymptomatic raised linear lesions on her lower back since the age of eight years. There was no history of inherited disorders affecting elastic fibers, such as cutis laxa, Marfan syndrome, or pseudoxanthoma elasticum. Also, there was no history of pregnancy, previous trauma to the area, significant and rapid change in weight, or alteration of exercise habits. The lesions were not present at any other site and no family member had similar skin lesions.
Clinical examination showed 16 firm, smooth, 5mm wide, flesh-colored, raised, horizontal, cord-like bands extending partially or completely across the lumbar back (Figure 1). The remaining physical examination revealed no other similar-appearing lesions.
Figures 1A and 1B.

Distant (A) and closer (B) views of the lumbar back of a 20-year-old Filipino woman showing asymptomatic, linear, raised, firm, flesh-colored horizontal bands that partially to completely extend across her lower back.
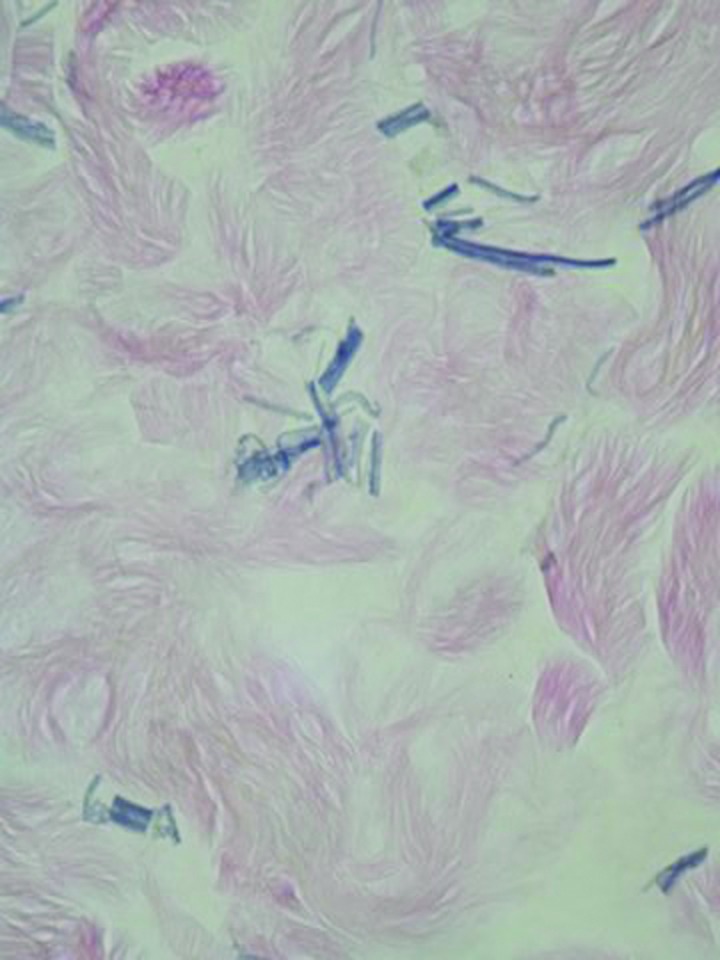
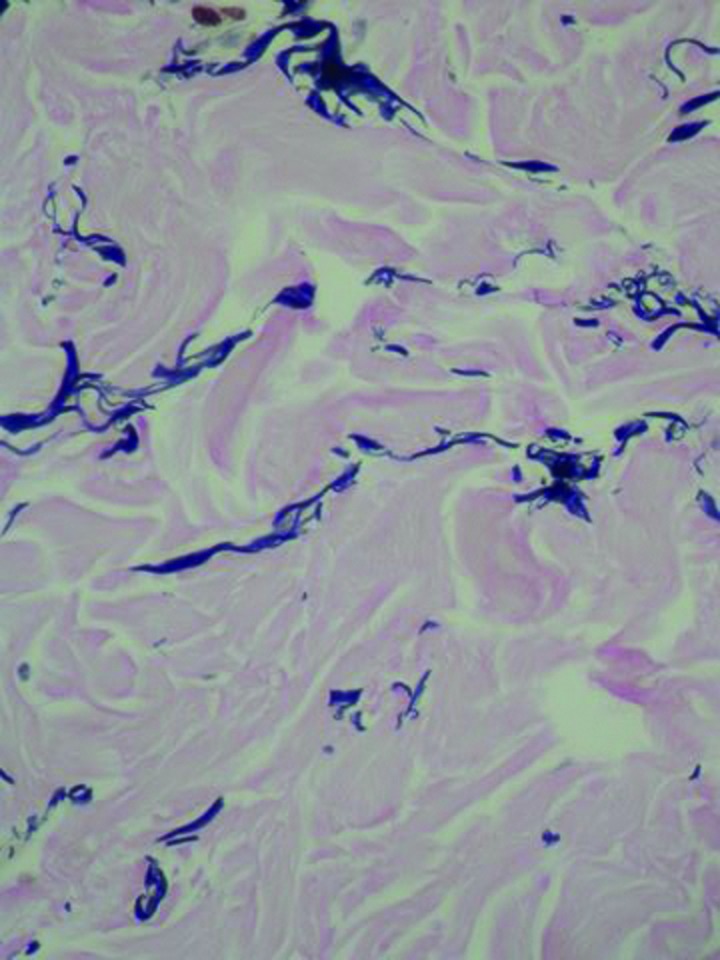
A punch biopsy was not only performed on the central aspect of a raised band, but also from a symmetric area of skin for comparison. Microscopic examination of the Verhoeff-van Gieson stained specimen from the lesion showed an epidermis without alteration and a normal density and morphology of elastic fibers in the papillary dermis and deep reticular dermis. However, there was nearly complete absence of elastic fibers in the mid dermis with a few fragmented elastic fibers remaining (Figure 2). In contrast, the specimen from her normal skin showed a uniform distribution of normal-appearing elastic fibers throughout the dermis (Figure 3).
Figures 2A and 2B.
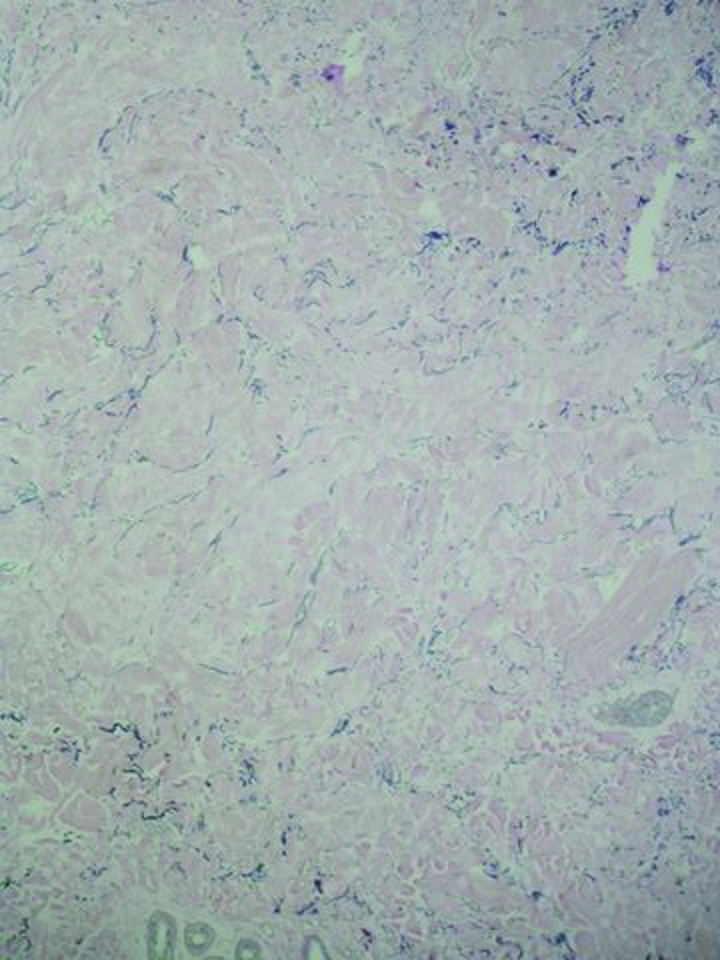
Microscopic examination—Intermediate (A) and higher (B) magnification—of the linear, raised, horizontal, lumbar bands show a localized lysis of the elastic fibers in the mid dermis: There is a paucity of fragmented elastic fibers in the upper portion of the reticular dermis. In contrast, normal-appearing elastic fibers are present in both papillary dermis and the deep reticular dermis (Verhoeff-van Gieson: A=X10; C=X20).
Figures 3A and 3B.
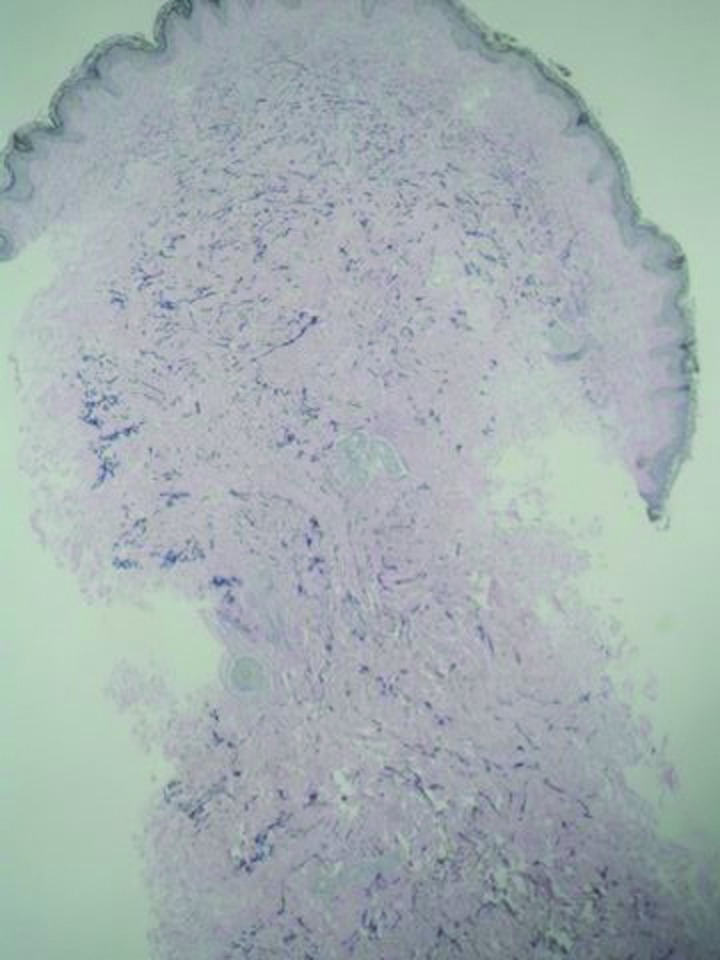
Microscopic examination—low (A) and high (B) magnifications—of a symmetric site of normal-appearing skin on the patient’s lumbar back show a uniform distribution of well-formed elastic fibers throughout the papillary and entire reticular dermis (Verhoeff-van Gieson: A=X4; B=X20).
The pathological findings established a diagnosis of mid-dermal elastolysis. Correlation of the clinical presentation (multiple, raised, horizontal, linear lumbar bands) and the microscopic features (a localized lysis of elastic fibers) prompted the authors to designate their patient’s condition as linear lumbar localized elastolysis.
DISCUSSION
Mid-dermal elastolysis is an acquired cutaneous disorder of elastic tissue that occurs predominantly in young women. Skin manifestations are asymptomatic and typically appear on the anterior and lateral trunk (of the chest and abdomen) and proximal upper extremities. Less commonly, skin lesions appear on the upper back and neck; involvement of the face and distal extremities is rare.1-5
Skin lesions attributed to mid-dermal elastolysis have been classified into three clinical types.1-5 Patients with type I lesions present with well-demarcated, often symmetric, areas of fine wrinkling.1 Individuals with type II lesions show perifollicular papillary protrusions; these often have apeau d’orange appearance.6,7 Indeed, many of the patients have not only type I lesions, but also coexisting type II lesions.1,7 Type III lesions of mid-dermal elastolysis include predominantly men who present with a persistent reticular erythema that is usually located on the chest; elastic stains demonstrate elastolysis, with or without elastophagocytosis, in the mid dermis.8-12 The patient’s lesions of mid-dermal elastolysis presented as linear, raised, horizontal bands on her lumbar back—a clinically unique morphology not previously associated with mid-dermal elastolysis.
Microscopic examination of mid-dermal elastolysis skin lesions shows a pathognomonic change: Selective loss of elastic fibers in the mid dermis. A slight lymphocytic infiltrate may be present; occasionally, elastophagocytosis of elastic fibers by macrophages and multinucleated giant cells is also observed. Why the loss of elastic fibers is restricted to the mid dermis remains to be determined. However, experimental studies suggest that pathological degradative processes (including increased elastolytic activity) are associated with elastin turnover dysbalance and subsequent loss of mid-dermis elastic fibers.1,3,5
The principle conditions in either the clinical and/or pathological differential diagnosis of mid-dermal elastolysis include anetoderma,13-16 annular elastolytic giant cell granuloma,17-21 cutis laxa,22-25 and pseudoxanthoma elasticum-like papillary dermal elastolysis26,27 (Table 1).1-38 In contrast to mid-dermal elastolysis, anetoderma and cutis laxa show loss of elastic fibers in both the papillary dermis and reticular dermis. Pseudoxanthoma elasticum-like papillary dermal elastolysis may clinically resemble the perifollicular protrusions of type II mid-dermal elastolysis; however, careful inspection will discern that the papules are nonfollicular and the microscopic examination demonstrates a band-like absence of elastic fibers restricted only to the papillary dermis.26,27 Annular elastolytic giant cell granuloma predominantly occurs in sun-exposed areas of middle aged women as an annular lesion with erythematous raised borders and an atrophic wrinkled central area17-19; at least two women have been described in whom annular elastolytic giant cell granuloma has both the clinical and pathological features of mid-dermal elastolysis, and the authors have suggested that annular elastolytic giant cell granuloma may represent a prodromal stage of mid-dermal elastolysis.1,20,21
TABLE 1.
Features of conditions in the clinical and/or pathological differential diagnosis of mid-dermal elastolysisa
| CONDITION | ANETODERMA | ANNULAR ELASTOLYTIC GIANT CELL GRANULOMA | CUTIS LAXA (ACQUIRED AND INHERITED) | MID-DERMAL ELASTOSIS | PSEUDOXANTHOMA ELASTICUM-LIKE PAPILLARY DERMAL ELASTOLYSIS |
|---|---|---|---|---|---|
| Clinical Features | |||||
| AGE AND/OR GENDER | Adults or children | Middle-aged women | Adults or children | Young women | Older women |
| POSSIBLY ASSOCIATED CONDITIONS | Presentb | Absent | Presentc | Presentd | Absent |
| PRECEDING INFLAMMATORY SKIN LESIONS | Presentb | Absent | Presentc | Presentd | Absent |
| MORPHOLOGY | Sac-like, circumscribed flaccid skin herniations | Red annular lesionse | Hanging skin folds and coarse wrinkles | Types I, II, and III Linear horizontal lumbar bandsf | Multiple yellow non- follicular papulesg |
| LOCATION | Trunk and proximal limbs | Sun-exposed areas (face) | Face | Trunk and proximal limbs Lumbar back | Neck, flexor forearms and axillae |
| Pathological Features | |||||
| DERMAL ELASTOLYSIS | |||||
| PAPILLARY | Present | h | Present | Absent | Presenti |
| RETICULAR | Present | h | Present | Presenti | Absent |
| DERMAL INFLAMMATION | Present/Absentj | Presentk | Present/Absentl | Present/Absentm | Absent |
| ELASTOPHAGO-CYTOSISn | Present | Present | Present | Present | Absent |
| REFERENCES | 13–16 | 17–21 | 22–25 | 1–12 | 26,27 |
Other conditions that might also be considered in either the clinical and/or pathological differential diagnosis of mid-dermal elastolysis include acrokeratoelastoidosis,24 amyloid elastolysis,28 fibroelastolytic papulosis of the neck,29 floppy eye syndrome and blepherochalasia,30 generalized elastolysis,31 granulomatous slack skin (lymphoma),32 intrinsic skin aging,33 nevus anelasticus,34 papular elastorrhexis,35 perifollicular elastolysis,36 upper dermal elastolysis,37 and white fibrous papulosis of the neck.38
Primary anetoderma has repeatedly been associated with antiphospholipid antibodies (with or without criteria of primary antiphospholipid syndrome); systemic diseases in some of these patients include autoimmune hemolysis, autoimmune thrombocytopenia, hypothyroidism, Grave’s disease, human immunodeficiency virus infection, mixed cryoglobulinemia, and systemic lupus erythematosus. Inflammatory skin lesions may precede those of anetoderma.
Cutis laxa may be inherited or acquired; the latter is often preceded by a cutaneous inflammatory condition (such as dermatitis, erythema multiforme, or urticaria) and may have associated internal organ involvement: cardiovascular, gastrointestinal, pulmonary, and/or urogenital. Marshall syndrome (postinflammatory elastolysis and cutis laxa) is a rare form of cutis laxa that has been observed in young children.
Mid-dermal elastolysis has been associated with autoimmune phenomena and autoimmune diseases (false-positive serology for Borrelia burgdorferi, elevated antinuclear antibodies and circulating immunocomplexes, Hashimoto’s thyroiditis, Grave’s disease, rheumatoid arthritis, and lupus erythematosus), dermatoses (atopic dermatitis, granuloma annulare, phototoxic dermatitis, pityriasis rosea, Sweet syndrome, and urticaria), genetic disorders (Keutel syndrome) and miscellaneous conditions (asthma, chronic hemodialysis, human immunodeficiency virus infection, mycosis fungoides, protein S deficiency, silicone mammoplasty, uterine carcinoma). In type I as well as type II, mid-dermal elastolysis preceding inflammatory skin lesions may occur.
The lesions are erythematous and annular; the borders are usually raised and red with the central portion of the lesion being atrophic and wrinkled in appearance;
In addition to our patient with linear, raised, indurated, flesh-colored horizontal bands that partially or completely extended across her lumbar back, mid-dermal elatolysis may present as plaques of fine wrinkling arranged parallel to skin cleavage lines (type I lesions), perifollicular popular protrusions with “peau d’orange” appearance (type II lesions), or persistent reticular erythema usually on the upper trunk (type III lesions).
The lesions resemble the “cobblestone” appearance of pseudoxanthoma elasticum.
There is paucity or absence of the elastic fibers in the center of the lesion.
There is a band-like loss of the elastic fibers.
In clinically inflammatory lesions, a perivascular inflammatory infiltrate may be present.
There is a granulomatous inflammatory infiltrate in the dermis consisting of histiocytes, lymphocytes, and giant cells.
Inflammatory infiltrates of neutrophils or lymphocytes may be present.
Inflammatory infiltrates of variable degree may be observed.
When present, elastophagocytosis may occur with (anetoderma, annular elastolytic giant cell granuloma and mid-dermal elastolysis) or without (cutis laxa) associated giant cells.
Mid-dermal elastolysis presenting as linear lumbar bands of localized lysis of elastic fibers is unique. The patient initially noted her lesions at eight years of age and had erroneously assumed that they were “stretch marks”; however, she had no predisposing factors associated with striae distensae. Also, in contrast to the hypopigmented-to-white, depressed, atrophic, scar-like appearance of older lesions of striae distensae, the patient’s lesions were flesh-colored, raised, firm, horizontal cord-like bands.39-42
Microscopic evaluation of a biopsy specimen from a raised cord-like horizontal band on the patient’s lumbar back readily established the diagnosis of mid-dermal elastolysis and excluded the possibility of an older lesion of striae distensae. The authors evaluated not only the lesional biopsy, but also a specimen of normal-appearing skin taken from a symmetric location on her back. Staining with the Verheoff-van Gieson stain highlighted the absence of elastic fibers in the mid dermis of the lesion and the uniform distribution of these fibers throughout the dermis of her nonlesional skin.
In contrast to mid-dermal elastolysis, the pathological changes of elastic fibers observed in striae distensae depend on the age of the lesion and the stain used for evaluation. When either the acid-orcein Giemsa stain or the Luna stain are used, numerous compact, straight, thin, elastic fibers (staining dark brown to black or purple, respectively) that are parallel to the overlying epidermis, which is flat and has lost its rete ridges, can be observed in the papillary dermis in the center of the lesion and curly and clumped elastic fibers can be noted at the periphery. However, after staining with Verheoff-van Gieson stain, early lesions of striae distensae show a reduction in elastic fibers (staining black) and older lesions show thicker elastic fibers in the affected skin. Scanning electron microscopy evaluation of these lesions supports the abundance of elastic fibers in striae distensae; they demonstrate a well-developed, dense network of fine elastic fibers. Therefore, it has been postulated that the elastic fibers present in early lesions of striae distensae are underestimated after staining with Verheoff-van Gieson stain since the elastic fibers are not able to be detected because they are immature and contain insufficient protein matrix to be demonstrated by this routine stain for elastin.42-44
The initial clinical impression of the patient’s asymptomatic, acquired, raised, firm, horizontal bands on her lower back was linear focal elastosis (Table 2).45-57 Linear focal elastosis is an uncommon condition characterized by asymptomatic linear yellow palpable indurated horizontal bands that extend across the mid and lower back of predominantly older men. Microscopic examination of the skin lesions demonstrates an increased amount of thin, wavy, elongated, fragmented, lumpy, and clumped elastic fibers separating the collagen bundles in the reticular dermis. The initial reports of linear focal elastosis described this condition predominantly in elderly Asian and Caucasian men; however, more recent studies report the dermal disorder in both younger individuals and women.48-50
TABLE 2.
Comparison of linear lumbar localized elastolysis and linear focal elastosis
| CONDITION | LINEAR LUMBAR LOCALIZED ELASTOLYSIS | LINEAR FOCAL ELASTOSIS |
|---|---|---|
| Clinical Features | ||
| EPIDEMIOLOGY | Young and Asian: Men:woman = 3:1 | Elderly men |
| STRIAE DISTENSAE | No | Some patientsa |
| ASSOCIATED CONDITIONS | Nob | No |
| FAMILIAL | No | Occasionalc |
| MORPHOLOGY | Linear, raised, indurated, flesh-colored horizontal bands | Linear, raised, indurated, yellow horizontal bands |
| LOCATION | Lumbar back | Mid and lower back |
| Pathological Features | ||
| ELASTIC FIBER CHANGE | Elastolysis: paucity or absence of elastic fibers; those remaining are fragmented | Elastosis: increased, thick, wavy, fragmented, lumpy, and clumpy elastic fibers |
| LOCATION | Mid dermis | Reticular dermis |
Lesions of striae distensae have been described either concurrently present (in the same or different site) or adjacent to or merging with linear focal elastosis in some of these patients.51–53
The reported patient had three annular patches on her buttocks of two years duration; biopsy revealed an atypical mononuclear infiltrate consistent with early mycosis fungoides and the skin lesions cleared after treatment with a high potency (clobetasol 0.05%) corticosteroid cream. Since the onset of her linear lumbar localized elastosis was 10 years prior to that of the onset of mycosis fungoides, the latter condition is not considered to be associated with her lesions of dermal elastolysis.
Familial linear focal elastosis have been reported in three papers54–56; we are excluding the paper in which a 15-year-old Korean boy with atrophic linear patches with decreased elastic fibers (consistent with striae distensae) was included in “a case of linear focal elastosis with a family history,” which also described his younger 13-year-old sister who had linear focal elastosis.57
After careful review of the published reports of linear focal elastosis, the authors have identified three adolescent boys (2 Korean and 1 Turkish) who had similar clinical and pathology findings as the patient described in this case (Table 3).45-47 Although the acquired skin lesions on their lumbar back were considered to represent linear focal elastosis (predominantly based upon their morphology and location), each group of investigators commented on the paucity or absence of elastic fibers in the linear raised horizontal bands. Hence, the authors respectfully suggest that the linear, raised, firm, horizontal lumbar back lesions in these individuals are more appropriately considered to represent linear lumbar localized elastolysis—an acquired disorder of elastic tissue that appears to have a predilection for Asian individuals (2 adolescent boys and 1 young woman) and an early onset age—either in adolescence (3 boys) or late childhood (1 girl).
TABLE 3.
Characteristics of patients with linear lumbar localized elastolysis
| CASE | AGE (YEARS) RACE SEX | DURATION OF LESION (MONTHS) | STRIAE DISTEN-SAE (TYPICAL MORPHOLOGY) | WEIGHT CHANGE (RECENT GAIN OR LOSS) | CORTICO-STEROID (TOPICAL OR SYSTEMIC) USE | CLINICAL PRESENTATION | PATHOLOGICAL FEATURES | REFERENCE |
|---|---|---|---|---|---|---|---|---|
| 1 | 14 Turkish Male | 3 | Not stated | Absent | Not stated | “Asymptomatic…lin ear, yellow, striae-like palpable bands surrounded by a slight erythema extending horizontally across the back. There was no scaling.” | “Coarseness in collagen bundles and homogenization. Within these homogenized areas aggregated fine elastic fibers and a decrement of elastic fibers were observed with the Verhoeff-van Gieson stain.” | 45 |
| 2 | 14 Korean Male | A few | Absent | Absent | Absent | “Asymptomatic, red, palpable and sometimes atrophic, striae-like bands extending horizontally across the middle and lower parts of the back.”a | “Near absence of mid- dermal elastic fibers (Verhoeff-van Gieson stain).”b | 46 |
| 3 | 16 Korean Male | 6 | Absent | Absent | Absent | “Asymptomatic, palpable, erythematous striae- like bands extending horizontally across the middle and lower back.”c | “The number of elastic fibers was decreased; fine fragmented elastic fibers were shown in the dermis, but there were no clumped elastic fibers (VVG stain).”d | 47 |
| 4 | 20 Filipino Female | 144 | Absent | Absent | Absent | “Asymptomatic, multiple (16), firm and smooth, 5mm wide, flesh-olored, raised and horizontal, cord-like bands extending partially or completely across the lumbar back.” | “An epidermis without alteration and a normal density and morphology of elastic fibers in the papillary dermis and deep reticular dermis. However, there was nearly complete absence of elastic fibers in the mid dermis with a few fragmented elastic fibers remaining (Verhoeff-van Gieson stain).” | Current report |
”Past and family history was not contributory, but he recalled an accidental trauma when he was struck by a cement wall on his back one month before the onset of the skin lesions.”
Specimens were taken from the perilesional area and atrophic and hypertrophic lesions. The specimens from the atrophic and hypertrophic lesions showed increased fragmented elastic fibers with markedly thickened collagen bundles, but the mid-dermal elastic fibers were markedly reduced. The hyperplastic plaque showed more fragmented elastic fibers and more compact collagen fibers than in atrophic plaque.”
”There was no history of debilitating infection or illness. The lesions had developed on the back about six months before presentation and migrated to his shoulder.”
”Electron microscopy showed an irregular, fragmented, electron-dense granular substance and a fragmented, electron-lucent substance between the normal collagen fibers, and no microfibrils. This indicates the degeneration of elastin, which suggests the degeneration of elastic fibers.”
It is remarkable that the location and morphology of the skin lesions in linear focal elastosis are essentially identical to those observed in the patients who had linear lumbar localized elastolysis. Yet, in contrast to the paucity or absence of elastic fibers in the mid dermis associated with linear lumbar localized elastolysis, microscopic examination of a horizontal band in a person with linear focal elastosis of the lower back shows an increase in the reticular dermal elastic fibers. Therefore, to differentiate between linear focal elastosis and linear lumbar localized 5. elastolysis, biopsies can be performed of lesional and normal skin from a symmetric site in an individual who 6. presents for evaluation of raised linear horizontal bands on the mid and lumbar back and the specimens can be evaluated not only using hematoxylin and eosin stained 7. sections, but also with Verhoeff-van Gieson stained preparations.
CONCLUSION
Linear lumbar localized elastolysis is characterized by pathognomonic pathological changes in the lesional tissue: Nearly complete absence of elastic fibers in the mid dermis with a paucity of residual fragmented elastic fibers. This condition is a unique clinical presentation of mid-dermal elastolysis morphologically presenting as multiple asymptomatic, raised, indurated, horizontal bands on the lumbar back. The clinical and pathological features of linear lumbar localized elastolysis are described in a young Filipino woman and the predominant conditions in the differential diagnosis of mid-dermal elastolysis (such as anetoderma, annular elastolytic giant cell granuloma, cutis laxa, and pseudoxanthoma elasticum-like papillary dermal elastolysis) are reviewed. The similar morphology and location of the patient’s linear lumbar localized elastolysis skin lesions and those of linear focal elastosis (of the lower back) prevented us from being able to differentiate the correct diagnosis based on the clinical presentation of her cutaneous findings. However, a lesional biopsy (especially after comparison to a specimen from a symmetric site of normal-appearing skin), evaluated after staining with Verhoeff-van Gieson stain, readily enabled the authors to definitively establish the diagnosis; linear lumbar localized elastolysis (as in the patient described in this case) showed a paucity of near absence of elastic fibers in the mid dermis, whereas linear focal elastosis demonstrates an increase in elastic fibers between the collagen tissue in the reticular dermis. Therefore, in patients who present with linear, elevated, firm, horizontal bands that partially or completely extend across the lower back, microscopic examination of the skin lesion (and perhaps also tissue of normal-appearing skin from a symmetric site for comparison) using hematoxylin and eosin stains and Verhoeff-van Gieson stain can be performed in order to differentiate between linear focal elastosis and linear lumbar localized elastolysis.
Footnotes
DISCLOSURE:The authors report no relevant conflicts of interest.
REFERENCES
- 1.Gambichler T. Mid-dermal elastolysis revisited. Arch Dermatol Res. 2010;302:85–93. doi: 10.1007/s00403-009-1004-0. [DOI] [PubMed] [Google Scholar]
- 2.Lewis KG, Dill SW, Wilkel CS, Robinson-Bostom L. Mid-dermal elastolysis preceded by acute neutrophilic dermatosis. J Cutan Pathol. 2004;31:72–76. doi: 10.1046/j.0303-6987.2004.0141.x. [DOI] [PubMed] [Google Scholar]
- 3.Patroi I, Annessi G, Girolomont G. Mid-dermal elastolysis: a clinical, histologic, and immunohistiochemical study of 11 patients. J Am Acad Dermatol. 2003;48:846–851. doi: 10.1067/mjd.2003.452. [DOI] [PubMed] [Google Scholar]
- 4.Yen A, Tschen J, Raimer SS. Mid-dermal elastolysis in an adolescent subsequent to lesions resembling granuloma annulare. J Am Acad Dermatol. 1997;37:870–872. doi: 10.1016/s0190-9622(97)80014-x. [DOI] [PubMed] [Google Scholar]
- 5.Sterling JC, Coleman N, Pye RJ. Mid-dermal elastolysis. Br J Dermatol. 1994;130:502–506. doi: 10.1111/j.1365-2133.1994.tb03386.x. [DOI] [PubMed] [Google Scholar]
- 6.Volz A, Pfister-Wartha A, Bruckner-Tuderman L. Braun-Falco. Perifollicular protrusions—mid-dermal elastolysis. J Dtsch Dermatol Ges. 2009;7:68–69. doi: 10.1111/j.1610-0387.2008.06959.x. [DOI] [PubMed] [Google Scholar]
- 7.Maghraoui S, Grossin M, Crickx B, et al. Mid dermal elastolysis: report of a case with a predominant perifollicular pattern. J Am Acad Dermatol. 1992;26:490–492. [PubMed] [Google Scholar]
- 8.Cutillas E, Ferrando FJ, Marti ME, et al. Reticular variant of mid-dermal elastolysis after insertion of a pacemaker. Clin Exp Dermatol. 2010;35:498–500. doi: 10.1111/j.1365-2230.2009.03736.x. [DOI] [PubMed] [Google Scholar]
- 9.Martin LK, Kossard S, Murrell DF. Reticular variant of mid-dermal elastolysis. Am J Dermatopathol. 2008;30:287–290. doi: 10.1097/DAD.0b013e31816906bc. [DOI] [PubMed] [Google Scholar]
- 10.Hillen U. Reticular erythema with focal mid-dermal elastophagocytosis. J Dtsch Dermatol Ges. 2008;6:857–859. doi: 10.1111/j.1610-0387.2008.06663.x. [DOI] [PubMed] [Google Scholar]
- 11.Bannister MJ, Rubel DM, Kossard S. Mid-dermal elastophagocytosis presenting as a persistent reticular erythema. Australas J Dermatol. 2001;42:50–54. doi: 10.1046/j.1440-0960.2001.00474.x. [DOI] [PubMed] [Google Scholar]
- 12.Brod BA, Rabkin M, Rhodes AR, Jegasothy BV. Mid-dermal elastolysis with inflammation. J Am Acad Dermatol. 1992;26:882–884. doi: 10.1016/0190-9622(92)70129-4. [DOI] [PubMed] [Google Scholar]
- 13.Romani J, Perez F, Llobet M, et al. Anetoderma associated with antiphospholipid antibodies: case report and review of the literature. J Eur Acad Dermatol Venereol. 2001;15:175–178. doi: 10.1046/j.1468-3083.2001.00255.x. [DOI] [PubMed] [Google Scholar]
- 14.Venencie PY, Winkelmann RK. Histopathologic findings in anetoderma. Arch Dermatol. 1984;120:1040–1044. [PubMed] [Google Scholar]
- 15.Ricci RM, Meffert JJ, McCollough ML. Primary anetoderma. Cutis. 1998;62:101–103. [PubMed] [Google Scholar]
- 16.Lindstrom J, Smith KJ, Skelton HG, et al. Increased anticardiolipin antibodies associated with the development of anetoderma in HIV-1 disease. Int J Dermatol. 1995;34:408–416. doi: 10.1111/j.1365-4362.1995.tb04442.x. [DOI] [PubMed] [Google Scholar]
- 17.Hanke CW, Bailin PL, Roenigk Jr HH. Annular elastolytic giant cell granuloma: a clinicopathologic study of five cases and a review of similar entities. J Am Acad Dermatol. 1979;1:413–419. [PubMed] [Google Scholar]
- 18.Schwarz T, Lindlbauer R, Gschnait F. Annular elastolytic giant cell granuloma. J Cutan Pathol. 1983;10:321–326. doi: 10.1111/j.1600-0560.1983.tb00334.x. [DOI] [PubMed] [Google Scholar]
- 19.Tock CL, Cohen PR. Annular elastolytic giant cell grauloma. Cutis. 1998;62:181–187. [PubMed] [Google Scholar]
- 20.Muller FB, Groth W. Annular elastolytic giant cell granuloma: a prodromal stage of mid-dermal elastolysis? [letter] Br J Dermatol. 2007;156:1377–1379. doi: 10.1111/j.1365-2133.2007.07902.x. [DOI] [PubMed] [Google Scholar]
- 21.Hohenleutner S, Wlotzke U, Landthaler M, Stolz W. Elastolysis of the mid dermis and annular elastolytic giant cell granuloma: different stages in the clinical spectrum of dermal elastolysis? Case report and review of the literature. Hautarzt. 1997;48:45–50. doi: 10.1007/s001050050546. [DOI] [PubMed] [Google Scholar]
- 22.Lewis PG, Hood AF, Barnett NK, Holbrook KA. Postinflammatory elastolysis and cutis laxa: a case report. J Am Acad Dermatol. 1990;22:40–48. doi: 10.1016/0190-9622(90)70005-3. [DOI] [PubMed] [Google Scholar]
- 23.Kielty CM. Elastic fibres in health and disease. Expert Rev Mol Med. 2006;8:1–23. doi: 10.1017/S146239940600007X. [DOI] [PubMed] [Google Scholar]
- 24.Lewis KG, Bercovitch L, Dill SW, Robinson-Bostom L. Acquired disorders of elastic tissue. Part II Decreased elastic tissue. J Am Acad Dermatol. 2004;51:165–185. doi: 10.1016/j.jaad.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 25.Morava E, Guillard M, Lefeber DJ, Wevers RA. Autosomal recessive cutis laxa syndrome revisited. Eur J Hum Genet. 2009;17:1099–1110. doi: 10.1038/ejhg.2009.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bagher Zadeh V, Najem N, el-Sayed Hanafy M. Pseudoxanthoma elasticum-like papillary dermal elastolysis. Acta Dermatovenerol Alp Panonica Adriat. 2011;20:35–38. [PubMed] [Google Scholar]
- 27.Alves R, Ferreira L, Vale E, Bordalo O. Pseudoxanthoma elasticum papillary dermal elastolysis: a case report. Dermatol Res Pract. doi: 10.1155/2010/352724. Epub 2010 Aug 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seep N, Pichler E, Breathnach SM, et al. Amyloid elastosis: analysis of the role of amyloid P component. J Am Acad Dermatol. 1990;22:27–34. doi: 10.1016/0190-9622(90)70003-z. [DOI] [PubMed] [Google Scholar]
- 29.Song YC, Oh BH, Ko JH, et al. A case of fibroelastolytic papulosis on the neck of a young man. Ann Dermatol. 2011;23:193–197. doi: 10.5021/ad.2011.23.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koursh DM, Modjtahedi SP, Selva D, Leibovitch I. The blepharochalasis syndrome. Surv Ophthalmol. 2009;54:235–244. doi: 10.1016/j.survophthal.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 31.Randle HW, Muller S. Generalized elastolysis associated with systemic lupus erythematosus. J Am Acad Dermatol. 1983;8:869–873. doi: 10.1016/s0190-9622(83)80019-x. [DOI] [PubMed] [Google Scholar]
- 32.LeBoit PE. Granulomatous slack skin. Dermatol Clin. 1994;12:375–389. [PubMed] [Google Scholar]
- 33.Tsuji T, Hamada T. Age-related changes in human dermal elastic fibres. Br J Dermatol. 1981;105:57–63. doi: 10.1111/j.1365-2133.1981.tb00882.x. [DOI] [PubMed] [Google Scholar]
- 34.Frances C, Robert J. Elastin and elastic fibers in normal and pathologic skin. Int J Dermatol. 1984;23:166–179. doi: 10.1111/j.1365-4362.1984.tb04506.x. [DOI] [PubMed] [Google Scholar]
- 35.Pajot C, Le Clec’h C, Hoareau F, et al. Two cases of papular elastorrhexis. Ann Dermatol Venereol. 2008;135:757–761. doi: 10.1016/j.annder.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 36.Varadi D, Saqueton AC. Perifollicular elastolysis. Br J Dermatol. 1970;83:143–150. doi: 10.1111/j.1365-2133.1970.tb12875.x. [DOI] [PubMed] [Google Scholar]
- 37.Hashimoto K, Tye MJ. Upper dermal elastolysis: a comparative study with mid-dermal elastolysis. J Cutan Pathol. 1994;21:533–540. doi: 10.1111/j.1600-0560.1994.tb00724.x. [DOI] [PubMed] [Google Scholar]
- 38.Gencoglan G, Ceylan C, Kazandi AC. White fibrous papulosis of the neck. Cutan Ocul Toxicol. 2011;30:69–71. doi: 10.3109/15569527.2010.521223. [DOI] [PubMed] [Google Scholar]
- 39.Cho S, Park ES, Lee DH, et al. Clinical features and risk factors for striae distensae in Korean adolescents. J Eur Acad Dermatol Venereol. 2006;20:1108–1113. doi: 10.1111/j.1468-3083.2006.01747.x. [DOI] [PubMed] [Google Scholar]
- 40.Nigam PK. Striae cutis distensae. Int J Dermatol. 1989;28:426–428. doi: 10.1111/j.1365-4362.1989.tb02497.x. [DOI] [PubMed] [Google Scholar]
- 41.Singh G, Kumar LP. Striae distensae. Indian J Dermatol Venereol Leprol. 2005;71:370–372. doi: 10.4103/0378-6323.16800. [DOI] [PubMed] [Google Scholar]
- 42.Tsuji T, Sawabe M. Elastic fibers in striae distensae. J Cutan Pathol. 1988;15:215–222. doi: 10.1111/j.1600-0560.1988.tb00547.x. [DOI] [PubMed] [Google Scholar]
- 43.Zheng P, Lavker RM, Kligman AM. Anatomy of striae. Br J Dermatol. 1985;112:185–193. doi: 10.1111/j.1365-2133.1985.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 44.Pinkus H, Keech MK, Mehregan AH. Histopathology of striae distensae, with special reference to striae and wound healing in the Marfan syndrome. J Invest Dermatol. 1966;46:283–292. doi: 10.1038/jid.1966.43. [DOI] [PubMed] [Google Scholar]
- 45.Adisen E, Ilter N, Erdem O, Gurer MA. Early onset linear focal elastosis in a Turkish boy. Turk JPediatr. 2007;49:441–443. [PubMed] [Google Scholar]
- 46.Chang SE, Park IJ, Moon KC, Koh JK. Two cases of linear focal elastosis (elastotic striae) J Dermatol. 1998;25:395–399. [PubMed] [Google Scholar]
- 47.Choi SW, Lee JH, Woo HJ, et al. Two cases of linear focal elastosis: different histopathologic findings. Int J Dermatol. 2000;39:205–217. doi: 10.1046/j.1365-4362.2000.00848.x. [DOI] [PubMed] [Google Scholar]
- 48.Pec J, Chromej I. Linear focal elastosis: what’s new? J Eur Acad Dermatol Venereol. 2004;18:247–249. doi: 10.1111/j.1468-3083.2004.00914.x. [DOI] [PubMed] [Google Scholar]
- 49.Pui JC, Arroyo M, Heintz P. Linear focal elastosis: histopathologic diagnosis of an uncommon dermal elastosis. J Drugs Dermatol. 2003;2:79–83. [PubMed] [Google Scholar]
- 50.Tamada Y, Yokochi K, Ikeya T, et al. Linear focal elastosis: a review of three cases in young Japanese men. J Am Acad Dermatol. 1997;36:301–303. doi: 10.1016/s0190-9622(97)80403-3. [DOI] [PubMed] [Google Scholar]
- 51.Hashimoto K. Linear focal elastosis: keloidal repair of striae distensae. J Am Acad Dermatol. 1998;39:309–313. doi: 10.1016/s0190-9622(98)70378-0. [DOI] [PubMed] [Google Scholar]
- 52.White GM. Linear focal elastosis: a degenerative or regenerative process of striae distensae? J Am Acad Dermatol. 1992;27:468. doi: 10.1016/s0190-9622(08)80889-4. [DOI] [PubMed] [Google Scholar]
- 53.Hagari Y, Norimoto M, Mihara M. Linear focal elastosis associated with striae distensae in an elderly woman. Cutis. 1997;60:246–248. [PubMed] [Google Scholar]
- 54.Molin A, Hashimoto K. Linear focal elastosis in a young black man: a new presentation. J Am Acad Dermatol. 1994;30:874–877. doi: 10.1016/s0190-9622(94)70103-2. [DOI] [PubMed] [Google Scholar]
- 55.Kim SE, Kim H-S, Kim J-K. Linear focal elastosis. Korean J Dermatol. 2002;40:178–180. [Google Scholar]
- 56.Whalen JG, English JC III. Case study on linear focal elastosis. Dermatol Nurs. 2006;18:469–471. [PubMed] [Google Scholar]
- 57.Seo JK, Chun JS, Jung SY, et al. A case of linear focal elastosis with a family history. Ann Dermatol. 2010;22:209–211. doi: 10.5021/ad.2010.22.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]


