Abstract
T-cell and NK-cell lymphomas are uncommon lymphomas with an aggressive clinical course. The causes and precise cellular origin of most T-cell lymphomas are still not well defined. The WHO classification utilizes morphologic and immunophenotypic features in conjunction with clinical aspects and in some instances genetics to delineate a prognostically and therapeutically meaningful categorization. The anatomic localization of neoplastic T-cells and NK-cells parallels in part their proposed normal cellular counterparts and functions. T-cells of the adaptive immune system are mainly based in lymph nodes and peripheral blood, whereas lymphomas derived from T-cells and NK-cells of the innate immune system are mainly extranodal. This approach allows for better understanding of some of the manifestations of the T-cell and NK-cell lymphomas, including their cellular distribution, some aspects of morphology and even associated clinical findings.
Keywords: pathobiology, pathogenesis, anaplastic large cell lymphoma, peripheral T-cell lymphoma, extranodal NK/T-cell lymphoma, enteropathy associated T-cell lymphoma, hepatosplenic T-cell lymphoma, subcutaneous panniculitis-like T-cell lymphoma, primary cutaneous コλ T-cell lymphoma, cellular origin, nodal, extranodal, innate immune system, adaptive immune system, T-follicular helper cells, αβ T-cell receptor, コλ T-cell receptor
(A) INTRODUCTION
T-cell and natural killer (NK)-cell lymphomas are uncommon neoplasms comprising fewer than 10% of all non-Hodgkin lymphomas (NHL) [1]. They have complex and often overlapping morphological and immunophenotypic characteristics, with as yet relatively little understanding of their molecular pathogenesis. Thus, clinical features play a significant role in the recognition of proposed entities in the WHO classification [2]. The most common of the T-cell and NK-cell lymphomas is peripheral T-cell lymphoma, not otherwise specified (PTCL, NOS) comprising 25% overall. This is closely followed by angioimmunoblastic T-cell lymphoma (AITL) (18.5%) [1]. This review will focus on the most common entities as defined in the current WHO Classification (see Table 1) [3]. Some entities are omitted from this discussion, since they are covered in depth in other articles within this issue.
Table 1.
WHO classification of tumors of haematopoietic and lymphoid tissues (2008).
| Mature T-cell and NK-cell neoplasms |
|---|
| T-cell prolymphocytic leukemia |
| T-cell large granular lymphocytic leukemia |
| Chronic lymphoproliferative disorder of NK-cells |
| Aggressive NK leukemia |
| Systemic EBV positive T-cell lymphoproliferative disease of childhood |
| Hydroa vacciniforme-like lymphoma |
| Adult T-cell leukemia/lymphoma |
| Extranodal NK/T cell lymphoma, nasal type |
| Enteropathy-associated T-cell lymphoma |
| Hepatosplenic T-cell lymphoma |
| Subcutaneous panniculitis-like T-cell lymphoma |
| Mycosis fungoides |
| Sezary syndrome |
| Primary cutaneous CD30 positive T-cell lymphoproliferative disorders |
| Lymphomatoid papulosis |
| Primary cutaneous anaplastic large cell lymphoma |
| Primary cutaneous gamma-delta T-cell lymphoma |
| Primary cutaneous CD8 positive aggressive epidermotropic cytotoxic T-cell lymphoma |
| Primary cutaneous CD4 positive small/medium T-cell lymphoma |
| Peripheral T-cell lymphoma, NOS |
| Angioimmunoblastic T-cell lymphoma |
| Anaplastic large cell lymphoma, ALK positive |
| Anaplastic large cell lymphoma, ALK negative |
| Proviional entities are in italics. Entities discussed in this article are underlined. |
An understanding of the normal immune system is helpful in categorizing T-cell and NK-cell malignancies. The innate immune system is a primitive defense system important in barrier (mucosal or skin) immunity. It includes NK cells and γδ T-cells[4]. γδ T-cells represent fewer than 5% of normal T-cells and are particularly enriched in certain locations, such as splenic red pulp, intestinal mucosa and other epithelial sites, sites in which γδ T-cell lymphomas often present [4]. Normal γδ T-cells in the spleen, thymus, and intestinal epithelia express the Vγ1 gene. Hepatosplenic T cell lymphoma (HSTL) also shows preferential expression of Vγ1, suggesting that the normal splenic γδ T-cells are counterparts of this lymphoma. Conversely, γδ T-cells in peripheral blood, tonsil, and skin express Vγ2, similar to primary cutaneous gamma-delta T cell lymphoma (PCGD)-TCLs[5].
The adaptive immune system is a more heterogeneous and complex system. Antigen recognition is MHC restricted. Immune memory also is a hallmark feature of the adaptive immune system and results in a more efficient response upon secondary exposure to the same antigen. T cells that are a part of adaptive immune system are quite heterogeneous and functionally complex. Effector T cells include regulatory T cells (Treg), follicular helper T cells (TFH), cytotoxic T cells, and memory T cells. CD4 positive T cells act via cytokine production, while CD8 positive and double negative T-cells are primarily cytotoxic, acting via secretion of cytotoxic molecules directly affecting target cells. Functional counterparts of these T-cell subsets have been recognized among the T-cell lymphomas, as will be discussed below.
A. NODAL T-CELL LYMPHOMAS
B. Peripheral T-cell lymphomas, not otherwise specified (PTCL, NOS)
PTCL, NOS comprises over 25% of all peripheral T-cell lymphomas and NK/T- cell lymphomas and is the most common subtype[1]. It is a diagnosis of exclusion, not corresponding to any of the specific mature T-cell lymphoma entities listed in the current WHO 2008, analogous to diffuse large B-cell lymphoma, not otherwise specified (DLBCL-NOS). Most patients are adults with a median age of 60 and a male to female ratio 2:1 [6]. The majority of cases are nodal in origin. However, extranodal presentations can occur in 13% of patients and most commonly involve skin and gastrointestinal tract.
The cytologic spectrum is very broad, ranging from polymorphous to monomorphous. Three morphologically defined variants have been described, including lymphoepithelioid (Lennert) variant, T-zone variant and follicular variant . The lymphoepithelioid variant of PTCL contains abundnant background epithelioid histiocytes and is commonly positive for CD8. It has been associated with a better prognosis [6]. The follicular variant of PTCL, NOS, is emerging as potentially a distinct clinicopathologic entity and will be discussed in the context of other TFH tumors.
The majority of PTCL, NOS have a mature T-cell phenotype with most cases being CD4 positive. 75% of cases show variable loss of at least one pan T-cell marker (CD3, CD2, CD5 or CD7), with CD7 and CD5 being most often downregulated [7]. CD30 and rarely CD15 can be expressed [8],with CD15 being an adverse prognostic feature[7]. CD56 expression, although uncommon, also has negative prognostic impact. Additional adverse pathologic prognostic factors include a proliferation rate greater than 25% based on KI-67 expression, and presence of more than 70% transformed cells. It is possible that in the future, distinct entities will be delineated within this currently heterogeneous category; however, thus far immunophenotypic analysis of these lymphomas offered little insight into their biology.
(B) Angioimmunoblastic T-cell lymphoma (AITL) and other TFH related nodal lymphomas
AITL is a systemic disease characterized by a polymorphous infiltrate involving lymph nodes, prominent high endothelial venules (HEV) and peri-vascular expansion of follicular dendritic cell (FDC) meshworks (Figure 1A–C). AITL was originally termed “ lymphadenopathy with dysproteinemia” and was believed to be a condition with a high risk of progression to lymphoma [9, 10].Today AITL is considered a de-novo T-cell lymphoma derived from αβ T-cells of follicular helper type (TFH ), normally found in the germinal centers [11–14].
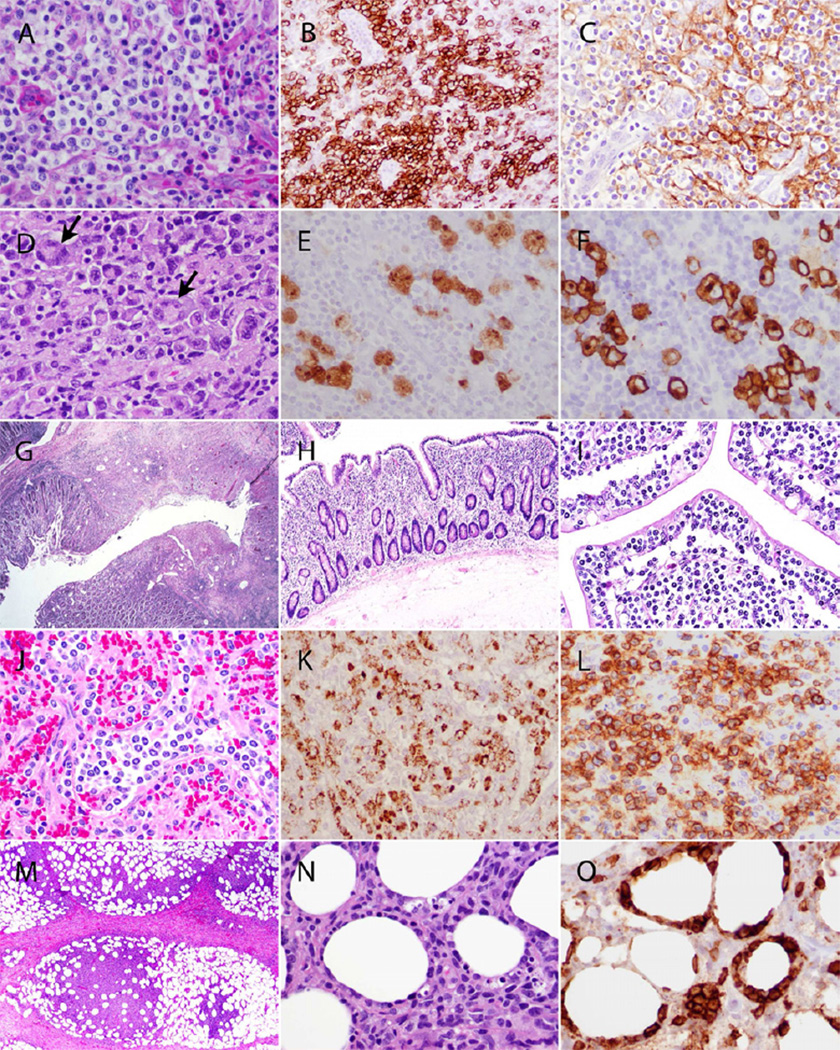
Figure 1. Pathological spectrum of T-cell lymphomas.
(A–C) Angioimmunoblastic T-cell lymphoma, lymph node. A. H&E stained section shows prominent clusters of atypical lymphocytes with clear cytoplasm surrounding the HEV. B. PD-1 positivity within the neoplastic cells clustered around the HEV. C. CD21 immunohistochemical stain demonstrating expanded perivascular FDC meshworks .
(D–F) Anaplastic large cell lymphoma, ALK positive, lymph node. D. Characteristic “hallmark” cells (examples indicated by arrows) with eccentric horseshoe-shaped nuclei and prominent perinuclear eosinophilic Golgi regions. E. Cytoplasmic and nuclear ALK expression in the neoplastic cells. F. Strong CD30 expression with a membranous and perinuclear dot-like staining pattern (highlighting Golgi region).
(G–I) Enteropathy-associated T-cell lymphoma, Types I and II, small intestine. G. EATL, type I. Low-power view of small intestinal lesion with a penetraing mucosal ulcer. Atypical lymphoid cells infiltrate the intestinal wall. H. EATL, Type I. Adjacent mucosa shows marked villous blunting. I. EATL, Type II. There is marked infiltration of the mucosa by monomorphic medium-sized cells with clear cytoplasm.
(J–L) Hepatosplenic T-cell lymphoma, spleen. J. H&E stained section of spleen demonstrating red pulp involvement by monotonous population of neoplastic cells. K. TIA-1 positivity within the neoplastic cells. L. The neoplastic cells express the T-cell receptor gamma chain, indicating a gamma-delta phenotype.
(M–O) Subcutaneous panniculitis-like T-cell lymphoma, skin. M. Subcutaneous tissue involvement predominantly affecting the fat lobules with sparing of the septa. N. High-power view demonstrating rimming of the individual fat cells by neoplastic cells. O. Neoplastic cells surrounding the fat cells are strongly CD8 positive.
AITL is the second most common entity among peripheral T-cell lymphoma and NK/T-cell lymphomas, comprising about 18.5% of cases [1]. It occurs in middle aged to elderly adults, with a median age of 65 years old. It has not been described in children. The incidence in males and females is approximately equal. Clinically, patients usually have advanced stage disease, with generalized lymphadenopathy, hepatosplenomegaly and prominent constitutional symptoms. Skin rash with associated pruritus is commonly present. There is often polyclonal hypergammaglobulinemia, associated with autoimmune phenomena.
Three different morphologic patterns are described in AITL [11, 15]. The early lesion of AITL (Pattern I) usually shows preserved architecture with characteristic hyperplastic follicles. The neoplastic proliferation is localized to the periphery of the follicles and is better visualized on immunohistochemical stains. In Pattern II the nodal architecture is partially effaced with retention of few regressed follicles, while no residual follicles are present in Pattern III. The subcapsular sinuses are preserved and even dilated. The paracortex contains arborizing HEV and there is a proliferation of FDC beyond the B-cell follicle. The neoplastic cells are small to medium in size, with minimal cytologic atypia. They often have clear to pale cytoplasm, and may show distinct cell membranes. A polymorphous inflammatory background is usually evident.
Although AITL is a T-cell malignancy, there is a characteristic expansion of B-cells and plasma cells, which likely reflects the function of the neoplastic cells as TFH cells. Both EBV-positive and EBV-negative B-cells are present. [16] Occasionally, the atypical B-cells may resemble Hodgkin/Reed-Sternberg like cells morphologically and immunophenotypically, sometimes leading to a diagnostic confusion with that entity [17, 18]. The B-cell proliferation in AITL may be extensive and some patients develop secondary EBV-positive diffuse large B-cell lymphomas (DLBCL) or – more rarely – EBV-negative B-cell tumors, often with plasmacytic differentiation [19–22].
The neoplastic CD4-positive T cells of AITL show strong expression of CD10 and CD279 (PD-1) and are positive for CXCL13 [14, 23, 24]. CXCL13 leads to increased B-cell recruitment to lymph nodes via adherence to the HEV, B-cell activation, plasmacytic differentiation and expansion of the FDC meshworks, all contributing to the morphologic and clinical features of AITL [25]. Intense PD-1-expression in the perifollicular tumor cells is particularly helpful in distinguishing AITL pattern I from reactive follicular and paracortical hyperplasia. EBV positivity within the B-cell component in AITL is seen in up to 97% of cases.
The vast majority of cases (up to 90%) have clonal rearrangements of T-cell receptor genes [26, 27]. In addition, immunoglobulin gene rearrangements may be found in up to 25–30% of patients with AITL [26–28]. The B-cell expansion in AILT is attributed to the TFH function of the tumor cells[29]. The relationship between TFH cells and AITL has been recently confirmed by gene expression profiling studies [12].
The follicular variant of PTCL, NOS is another entity with a TFH phenotype [30–32]. In contradistinction to AITL, it does not have prominent HEV or extra-follicular expansion of FDC meshworks. The neoplastic cells may form intrafollicular aggregates, mimicking B-cell follicular lymphoma, but also can have interfollicular growth pattern or involve expanded mantle zones [32–35]. Similar to AITL, this entity occasionally has EBV positive or EBV negative Hodgkin-like cells, mimicking classical Hodgkin lymphoma [18, 36]. Clinically, the follicular variant of PTCL, NOS is distinct from AITL: patients more often present with early stage disease with partial lymph node involvement and may lack the constitutional symptoms associated with AITL.
The recent finding of TET2 mutations in 47% of AITL and 58% of PTCLs expressing TFH cell markers, suggests overlap between these entities [37] . The relationship between these two neoplasms has also been corroborated by gene expression profiling studies [12]. A subset of PTCL, NOS, follicular variant cases have a t(5;9)(q33;q22) resulting in a fusion of ITK and SYK and generation of a chimeric protein [38]. This finding was not observed in AITL, but studies of this question are limited. Further studies are necessary to determine the relationship between PTCL, NOS, follicular variant and AITL.
(B) Anaplastic large cell lymphoma, ALK-positive (ALCL, ALK+)
ALCL, ALK+ is one of the best-defined entities within the peripheral T-cell lymphomas, with characteristic “hallmark cells” bearing horseshoe-shaped nuclei and expressing ALK and CD30 (Figure 1D–1F). It accounts for about 7% of all peripheral T-cell and NK-cell lymphomas [1] and is most common in the first three decades of life. There is a slight male predominance. Patients often present with lymphadenopathy, but involvement of extranodal sites (skin, bone, soft tissues, lung, liver) is common and most patients have stage III – IV disease (70% cases). B symptoms are common. Bone marrow involvement is present in 10% of cases on H&E examination, but increases to 30% when immunohistochemistry is employed [39].
ALCL, ALK+ shows a wide morphologic spectrum, with 5 different patterns described, but all variants contain some hallmark cells. Hallmark cells have eccentric horseshoe- or kidney- shaped nuclei, and a prominent perinuclear eosinophilic Golgi region. The tumor cells grow in a cohesive pattern with predilection for sinus involvement [40]. Smaller tumor cells predominate in the small cell variant, and in the lymphohistiocytic variant abundant histiocytes mask the presence of tumor cells, many of which are small.
By definition, all cases show ALK and CD30 positivity, with expression usually weaker in the smaller tumor cells. The majority of cases are also positive for EMA. There is often loss of pan-T cell markers, with 75% of cases lacking surface expression of CD3. CD2 and CD4 are most commonly expressed [41]. In the few “null” cases, T-cell receptor gene rearrangements studies usually confirm the T-cell origin of the neoplastic cells. Most cases are positive for cytotoxic associated markers, such as TIA1, granzyme B and perforin [40].
ALK expression is a result of a characteristic recurrent genetic alteration consisting of a rearrangement of anaplastic lymphoma kinase (ALK) gene on chromosome 2p23 to one of many partner genes, resulting in expression of chimeric protein. The most common partner gene, occurring in 75% of cases, is Nucleophosmin (NPM1) on chromosome 5q35, resulting in t(2;5)(p23;q35). The cellular distribution of ALK in different translocation variants may vary depending on the partner gene [42].
ALCL, ALK+ has good prognosis with 5-year survival rate of 70–80% [43]. Relapses are common (30% cases), but the neoplasm remains chemosensitive [44]. Notably, small cell and lymphohistiocytic variants of ALCL, ALK+, often seen in children, may have a more aggressive clinical course [45].
B. Anaplastic large cell lymphoma, ALK-negative (ALCL, ALK-)
ALCL, ALK- is included as a provisional category in the 2008 WHO classification. It is defined as a CD30 positive T-cell lymphoma that is morphologically indistinguishable from ALCL, ALK+ with a cohesive growth pattern and presence of hallmark cells, but lacking ALK protein expression. Loss of T-cell markers, a cytotoxic phenotype, EMA expression and sinusoidal growth pattern, although helpful, are not essential for the diagnosis of ALK−ALCL.
Patients are usually adults between the ages of 40 and 65, in contrast to ALCL, ALK+, which is more common in children and young adults. ALCL, ALK- can involve both lymph nodes and extranodal tissues, although the latter is seen less commonly than in ALCL, ALK+ [46]. Most cases of ALCL, ALK-demonstrate effacement of lymph node architecture by sheets of cohesive neoplastic cells with typical “hallmark” features. In contrast to the ALCL, ALK+, the small cell morphologic variant is not recognized. Unlike its ALK+ counterpart, ALCL, ALK- shows a greater preservation of surface T – cell marker expression, while the expression of cytotoxic markers and EMA is less likely [43]. CD30 expression should be strong and homogeneous. Caution is advised in the differential diagnosis with CHL, since some cases of CHL can be rich in tumor cells, and negative for CD15 expression. Use of PAX5, nearly always positive in CHL, is a helpful feature.
Gene expression signatures and recurrent chromosomal imbalances are different in ALCL, ALK – and ALCL, ALK+, confirming that they are distinct entities at a molecular and genetic level [47–49]. In addition, recent studies identified a recurrent translocation t(6;9)(p25.3;q32.3) in a subset of ALCL, ALK-cases, which results in down-regulation of DUSP22 phosphatase gene expression located on chromosome 6p25.3, with some data suggesting that DUSP22 might function as a tumor suppressor gene [50].
ALCL, ALK- is clinically distinct from both ALCL, ALK+ and PTCL, NOS, with significant differences in prognosis among these three different entities. The 5 year overall survival of ALCL, ALK- is reported as 49% which is not as good as that of ALCL, ALK+ (at 70%), but at the same time it is significantly better than that of PTCL, NOS (32%)[43]. Thus, both clinical behavior and genetic studies suggest that ALCL, ALK- indeed should be considered as a separate entity. Interestingly, if patients are stratified based on age and disease stage, the prognosis of ALCL, ALK – and ALCL, ALK+ seems to be more similar, suggesting that clinical parameters are important in prognostication[43].
(B) Primary cutaneous ALCL
Primary cutaneous ALCL (C-ALCL) deserves a special mention, as it is often indistinguishable from ALCL, ALK- by morphology. It is defined as a cutaneous tumor of large cells with anaplastic, pleomorphic or immunoblastic morphology with more than 75% of cells expressing CD30. Large cell transformation of MF needs to be excluded on the basis of clinical findings and/or history. Together with lymphomatoid papulosis (LyP), C-ALCL it belongs to the spectrum of primary cutaneous CD30-positive T-cell lymphoproliferative disorders, which as a group comprise the second most common group of cutaneous T-cell lymphoproliferations after mycosis fungoides.
Clinically, C-ALCL usually presents with solitary or localized tumors or nodules. Most patients are adults. Regional lymph node involvement may be seen, which does not appear to mandate a poorer prognosis. In these cases distinction from systemic ALCL, ALK- may be complex [51, 52]. Mucosal presentations have been reported, and are likely part of the same spectrum of the disease [53].
The immunohistochemical staining profile is quite similar to ALCL, ALK- , with a greater proportion of cases staining positive for cytotoxic markers and most cases being negative for EMA. At least 75% of the tumor cells should be positive for CD30. CD15 may also be expressed, and when lymph node involvement occurs, the differential with classical Hodgkin lymphoma can be difficult [54]. Rare cases of ALCL, ALK+ may present with localized cutaneous lesions, and may resemble C-ALCL. [55]. Therefore, staining for ALK is advisable in all CD30+ T-cell neoplasms.
Similar to systemic ALCL, ALK- a subset of cases show translocations of IRF4/DUSP22 [50, 56, 57].
Despite similarities to systemic ALCL, ALK-, the prognosis in C-ALCL is excellent with 5-year overall survival at 90% [43]. In cases of C-ALCL, a period of observation is warranted since some lesions may regress, similar to LYP. Recurrences, usually confined to the skin, are common and they do not portend a poorer prognosis. Therefore, while systemic ALCL, ALK- is treated with combination chemotherapy, C-ALCL is generally sufficiently treated with local therapies [58].
(A) EXTRANODAL T-CELL AND NK-CELL LYMPHOMAS
(B) Extranodal NK/T-cell lymphoma, nasal type
Extranodal NK/T-cell lymphoma, nasal type, is an aggressive disease, often with destructive midline lesions. Necrosis is prominent. Most cases are of NK-cell derivation, but some cases are derived from cytotoxic T-cells. It is universally associated with EBV- although technical factors may impede its detection in some cases. This topic will be discussed in detail in Chapter 7 (Nakamura et al).
(B) Enteropathy-associated T-cell lymphoma (EATL)
EATL is an aggressive neoplasm thought to be derived from the intraepithelial T-cells of the intestine. Two morphologically, immunohistochemically and genetically distinct types of EATL are recognized in the 2008 WHO classification: Type I (representing the majority of EATL) and Type II (comprising 10–20% of cases) [2, 59].
C. EATL, Type I
Type I EATL is usually associated with overt or clinically silent gluten-sensitive enteropathy, and is more often seen in patients of Northern European extraction due to high prevalence of coeliac disease in this population[60]. Clinically, patients with EATL type I often have positive serologies for anti-gliadin and anti-transglutaminase antibodies, can have associated dermatitis herpetiformis and hyposplenism [61]. In addition, 90% of patients with EATL type I have coeliac disease-associated human leukocyte antigen haplotypes (HLA-DQ2/8), further strengthening the notion that EATL type I and coeliac disease are related [61]. In a proportion of cases, there is no clear-cut history of coeliac disease; however, the resection specimens reveal histologic features of celiac disease [62]. Patients usually present with abdominal pain or signs of bowel perforation and sepsis.
Most commonly, the lesions of EATL are found in the jejunum or ileum (90% of cases), with rare presentations in duodenum, colon, stomach, or areas outside of the gastrointestinal tract. The intestinal lesions are usually multifocal with mucosal ulceration (Figure 1G, H). Clinical course of EATL is aggressive with most patients dying of disease or complications of disease within 1 year.
The cytological spectrum of EATL type I is broad, and some cases may contain anaplastic cells. There is a polymorphous inflammatory background, which may obscure the neoplastic component in some cases. The intestinal mucosa in regions adjacent to the tumor often shows features of coeliac disease with blunting of the villi and increased numbers of intraepithelial lymphocytes (IEL), which may represent lesional precursor cells (Figure 1H–I) [62].
By immunohistochemistry, the neoplastic cells are often CD3+CD4-CD8-CD7+CD5-CD56- βF1+, and contain cytotoxic granule-associated proteins (TIA-1, granzyme B, perforin). CD30 is partially expressed in almost all cases. Not surprisingly, CD103, which is a mucosal homing receptor, can be expressed in EATL. Interestingly, the IEL in mucosa adjacent to EATL and in refractory celiac disease (RCD) often show downregulation of CD8, similar to neoplastic cells of EATL [63].
The lymphoma cells show clonal rearrangements of TCRβ and TCRα. In addition there are frequent gains of 9q31.3, 1q32.2-q41 and 5q34-q35.2 or loss of 16q12.1. Interestingly, in patients with refractory celiac disease (RCD), who subsequently developed EATL, identical TCR gene rearrangements and gain of chromosome 1q are seen in both phenotypically aberrant IEL of RCD as well as in neoplastic cells later on [63]. This suggests that RCD with aberrant IEL is a precursor lesion of EATL. Upregulation of IL-15 in the intestinal epithelia of patients with coeliac disease has been shown to activate antiapoptotic pathways in the IEL, possibly playing a role in malignant transformation of these cells [64, 65].
C. EATL, type II
Type II EATL, also referred to as monomorphic CD56+ intestinal T-cell lymphoma, is defined as an intestinal tumor composed of small to medium-sized monomorphic T-cells that express both CD8 and CD56[59] (Figure 1I). There is often a lateral spread of tumor within the mucosa, and absence of an inflammatory background. The majority of cases express the γδ T-cell receptor [66].
EATL, II has a more world-wide distribution than EATL type I and is often seen in Asians or Hispanic populations, in whom coeliac disease is rare. [60, 67, 68]. In individuals of European descent EATL, II represents about 20% of intestinal T-cell lymphomas, with a history of coeliac disease in at least a subset of cases [60]. The clinical course is aggressive.
Gain of 9q31.3 or loss of 16q12.1 is found in majority of cases, in common with EATL type I. In contradistinction to the classic form of EATL, monomorphic variant of EATL more often shows amplification of MYC oncogene locus at 8q24, while gains in 1q and 5q are less frequent, suggesting that it is a distinct entity [62].
(B) Hepatosplenic T-cell lymphoma (HSTL)
HSTL is an aggressive systemic neoplasm derived from γδ (and rarely αβ) cytotoxic T-cells of the innate immune system [5, 69, 70]. It is one of the rarest T-cell lymphomas, and typically affects adolescents and young adults (median age, 35 years) with a strong male predominance [69, 70]. Up to 20% of cases arise in a background of chronic antigenic stimulation and concomitant immunosuppression. Patients at risk include long term solid organ transplant recipients [70–73] and patients with Crohn’s disease treated with azathioprine and infliximab [74, 75]. HSTL often presents with systemic symptom, thrombocytopenia, and marked hepatosplenomegaly in absence of lymphadenopathy [76]. Survival is usually less than 3 years, with rapid relapse and fatal outcome even in those patients who initially might have responded to chemotherapy [70, 71].
The cells are monotonous, medium sized, with narrow rim of cytoplasm. They show characteristic intrasinusoidal involvement of liver and spleen, similar to the normal distribution of γδ T-cells (Figure 1J–L) Neoplastic cells within the sinusoids of the bone marrow are best visualized with immunohistochemistry. Immunophenotypicaly, the neoplastic cells are CD3+, CD5-, CD4-, and variable expression of CD8. They are TIA-1-positive but lack granzyme B and perforin (non-activated phenotype) [69, 77]. In addition, HSTL often shows aberrant expression of multiple killer immunoglobulin-like receptors (KIR) isoforms, normally seen on NK cells, along with dim or absent CD94 [78]. The majority of cases are of γδ T-cell origin; however, there are rare cases expressing αβ T-cell receptor [79]. Most of the γδ cases express the Vδ1 epitope, which is in contrast to PCGD-TCL expressing Vδ2 epitope [70, 73]. At the genetic level, most cases have isochromosome 7q or a ring chromosome leading to 7q amplification. With disease progression, two to five copies of i(7)(q10) in addition to numerical and structural aberrations of the second chromosome 7 have been reported. Gene expression profiling showed that hepatosplenic γδ T-cell lymphoma is distinct from other non-hepatosplenic γδ T-cell lymphomas [80] and revealed similarities in HSTL expressing αβ or γδ T-cell receptor [81].
(B) Subcutaneous panniculitis-like T-cell lymphoma (SPTCL)
SPTCL is a rare T-cell lymphoma with a very wide age distribution (median age35 years) but can be seen in young children [82–84]. The infiltrate is usually confined to the subcutis, with sparing of dermis. (Figure 1M–O). Histologically, the cells surround individual fat cells (rimming) with fat necrosis and karyorrhexis [83, 85]. The infiltrating cells are positive for CD8, and negative for CD56. They express βF1 and cytotoxic markers (TIA1, perforin and granzyme B), consistent with their proposed derivation from activated cytotoxic αβ T-cells. Patients present with subcutaneous nodules on extremities and trunk. The disease has a relatively good prognosis (5 year overall survival of 80%)[82, 86].
SPTCL is associated with autoimmune disease in 20% of cases, most commonly systemic lupus erythematosus (SLE), although it is not clear what role immune dysregulation might play in the genesis of this lymphoma [86]. In some cases, distinction from benign lobular panniculitis may be difficult [82, 85, 87], but lobular pannicultis is not thought to be a predisposing factor. A hemophagocytic syndrome (HPS) is observed in 15–20% of cases and carries a poor prognosis [88]. Patients with HPS exhibit cytopenias and abnormal liver function tests. Dissemination to lymph nodes and other extracutaneous sites is rare.
(B) Primary cutaneous gamma-delta T-cell lymphoma (PCGD-TCL)
PCGD-TCL is composed of a mature activated γδ T cells. Morphologically, three patterns of involvement may be present: epidermotropic, dermal or subcutaneous mimicking SPTCL[89]. In some cases, more than one histologic pattern can be seen. Apoptosis and necrosis are frequent, often with angioinvasion [86].
Most cases occur in adults with equal prevalence in males and females. Extremities are most commonly involved, particularly thighs and buttocks. B symptoms are common. Patients may present with ulcers, plaques, or dermal / subcutaneous nodules. HPS is often present in patients with SPTCL-like involvement [86], a finding leading to a poor outcome[90]. Elevated liver enzymes and leucopenia are seen in 50% of patients, and are associated with poor prognosis [91]. Lymph nodes, spleen and bone marrow are usually spared. PCGD-TCL is resistant to multiagent chemotherapy and radiation. It is aggressive, with median survival of about 15 months.
Immunohistochemically, PCGD-TCL has an activated cytotoxic phenotype; CD8 is variably expressed and CD56 is usually positive. The cells express the γδ T-cell receptor [73].
There are rare T-cell lymphomas of γδ T-cell derivation that present in non-cutaneous extranodal sites, including nasal mucosa, intestine, lung, orbit and tongue [92]. Their relationship PCGD-TCL is uncertain.
Summary
Peripheral T-cell and NK-cell lymphomas are heterogeneous neoplasms, often with overlapping morphological features. Broadly speaking, T-cell and NK-cell lymphomas can be categorized as primarily nodal or extranodal with parallels to the adaptive and innate immune systems. The current WHO 2008 classification uses a multi-modality approach to define prognostically distinct entities. Attempts to better define the normal cellular counterparts of the T-cell/NK-cell lymphomas has resulted in better understanding of some entities such as AITL and the follicular variant of PTCL, NOS. Other categories, such as PTCL, NOS, lack clear defining characteristics and are quite heterogeneous, similar to DLBCL. Unlike B-cell lymphomas, few peripheral T-cell/NK-cell lymphomas are defined by recurrent genetic alterations, but with the implementation of new genomic sequencing strategies, the number is likely to increase. These techniques have yielded new insights into ALCL, ALK-, and the TFH malignancies in particular. In addition, effort should be expanded to identify pathologic predictors of prognosis and potential therapeutic targets within different categories of peripheral T-cell/NK-cell lymphomas. To date most treatment protocols are applied across all the T-cell lymphomas, with few exceptions. However, new drugs directed at the ALK kinase, or at CD30 expression point the way towards targeted therapies [93, 94].
Research Agenda.
The elucidation of the genomic changes associated with the specific forms of peripheral T-cell lymphoma is in its early stages.
Both exome sequencing and whole genome sequencing offer great promise to illuminate the nature of mature T-cell lymphomas, and the relationship between the histological subtypes.
Identification of relevant pathways of neoplastic transformation will have relevance for more targeted therapy of these tumors in the future.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
None.
Contributor Information
Ewa B. Bajor-Dattilo, Laboratory of Pathology, National Cancer Institute, Building 10, Room 2N113, Bethesda, MD 20892, USA, Tel: +1-301-402-2457, Fax: +1-301-402-2415, ewa.bajor-dattilo@nih.gov
Stefania Pittaluga, Laboratory of Pathology, National Cancer Institute, Building 10, Room 2N109, Bethesda, MD 20892, USA, Tel: +1-301-402-0297, Fax: +1-301-402-2415, stefpitt@mail.nih.gov.
Elaine S. Jaffe, Laboratory of Pathology, National Cancer, Institute, Building 10, Room 2B42, Bethesda, MD 20892, USA, Tel: +1-301-496-0183, Fax: +1-301-402-2415, ejaffe@mail.nih.gov.
References
- 1.Vose J, Armitage J, Weisenburger D. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2008 Sep 1;26(25):4124–4130. doi: 10.1200/JCO.2008.16.4558. [DOI] [PubMed] [Google Scholar]
- 2.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri S, Stein H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed. Lyon: IARC Press; 2008. [Google Scholar]
- 3.Jaffe ES, Nicolae A, Pittaluga S. Peripheral T-cell and NK-cell lymphomas in the WHO classification: pearls and pitfalls. Modern Pathology. 2013 Jan;26(Suppl 1):S71–S87. doi: 10.1038/modpathol.2012.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carding SR, Egan PJ. Gammadelta T cells: functional plasticity and heterogeneity. Nat Rev Immunol. 2002 May;2(5):336–345. doi: 10.1038/nri797. [DOI] [PubMed] [Google Scholar]
- 5.Przybylski GK, Wu H, Macon WR, Finan J, Leonard DG, Felgar RE, et al. Hepatosplenic and subcutaneous panniculitis-like gamma/delta T cell lymphomas are derived from different Vdelta subsets of gamma/delta T lymphocytes. The Journal of molecular diagnostics : JMD. 2000 Feb;2(1):11–19. doi: 10.1016/s1525-1578(10)60610-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weisenburger DD, Savage KJ, Harris NL, Gascoyne RD, Jaffe ES, MacLennan KA, et al. Peripheral T-cell lymphoma, not otherwise specified: a report of 340 cases from the International Peripheral T-cell Lymphoma Project. Blood. 2011 Mar 24;117(12):3402–3408. doi: 10.1182/blood-2010-09-310342. [DOI] [PubMed] [Google Scholar]
- 7.Went P, Agostinelli C, Gallamini A, Piccaluga PP, Ascani S, Sabattini E, et al. Marker expression in peripheral T-cell lymphoma: a proposed clinical-pathologic prognostic score. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2006 Jun 1;24(16):2472–2479. doi: 10.1200/JCO.2005.03.6327. [DOI] [PubMed] [Google Scholar]
- 8.Barry TS, Jaffe ES, Sorbara L, Raffeld M, Pittaluga S. Peripheral T-cell lymphomas expressing CD30 and CD15. Am J Surg Pathol. 2003 Dec;27(12):1513–1522. doi: 10.1097/00000478-200312000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Lukes RJ, Tindle BH. Immunoblastic lymphadenopathy. A hyperimmune entity resembling Hodgkin's disease. The New England journal of medicine. 1975 Jan 2;292(1):1–8. doi: 10.1056/NEJM197501022920101. [DOI] [PubMed] [Google Scholar]
- 10.Frizzera G, Moran EM, Rappaport H. Angio-immunoblastic lymphadenopathy with dysproteinaemia. Lancet. 1974 Jun 1;1(7866):1070–1073. doi: 10.1016/s0140-6736(74)90553-4. [DOI] [PubMed] [Google Scholar]
- 11.Attygalle A, Al-Jehani R, Diss TC, Munson P, Liu H, Du MQ, et al. Neoplastic T cells in angioimmunoblastic T-cell lymphoma express CD10. Blood. 2002 Jan 15;99(2):627–633. doi: 10.1182/blood.v99.2.627. [DOI] [PubMed] [Google Scholar]
- 12.de Leval L, Rickman DS, Thielen C, de Reynies A, Huang YL, Delsol G, et al. The gene expression profile of nodal peripheral T-cell lymphoma demonstrates a molecular link between angioimmunoblastic T-cell lymphoma (AITL) and follicular helper T cells (TFH) Blood. 2007 Feb 6; doi: 10.1182/blood-2006-10-055145. [DOI] [PubMed] [Google Scholar]
- 13.Dorfman DM, Brown JA, Shahsafaei A, Freeman GJ. Programmed death-1 (PD-1) is a marker of germinal center-associated T cells and angioimmunoblastic T-cell lymphoma. Am J Surg Pathol. 2006 Jul;30(7):802–810. doi: 10.1097/01.pas.0000209855.28282.ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grogg KL, Attygalle AD, Macon WR, Remstein ED, Kurtin PJ, Dogan A. Expression of CXCL13, a chemokine highly upregulated in germinal center T-helper cells, distinguishes angioimmunoblastic T-cell lymphoma from peripheral T-cell lymphoma, unspecified. Modern Pathology. 2006 Aug;19(8):1101–1107. doi: 10.1038/modpathol.3800625. [DOI] [PubMed] [Google Scholar]
- 15.Attygalle AD, Kyriakou C, Dupuis J, Grogg KL, Diss TC, Wotherspoon AC, et al. Histologic evolution of angioimmunoblastic T-cell lymphoma in consecutive biopsies: clinical correlation and insights into natural history and disease progression. Am J Surg Pathol. 2007 Jul;31(7):1077–1088. doi: 10.1097/PAS.0b013e31802d68e9. [DOI] [PubMed] [Google Scholar]
- 16.Weiss LM, Jaffe ES, Liu XF, Chen YY, Shibata D, Medeiros LJ. Detection and localization of Epstein-Barr viral genomes in angioimmunoblastic lymphadenopathy and angioimmunoblastic lymphadenopathy-like lymphoma. Blood. 1992 Apr 1;79(7):1789–1795. [PubMed] [Google Scholar]
- 17.Quintanilla-Martinez L, Fend F, Moguel LR, Spilove L, Beaty MW, Kingma DW, et al. Peripheral T-cell lymphoma with Reed-Sternberg-like cells of B-cell phenotype and genotype associated with Epstein-Barr virus infection. Am J Surg Pathol. 1999;23(10):1233–1240. doi: 10.1097/00000478-199910000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Nicolae A, Pittaluga S, Venkataraman G, Vijnovich-Baron A, Xi L, Raffeld M, et al. Peripheral T-cell Lymphoma of Follicular T-Helper Cell Derivation with Hodgkin/Reed-Sternberg Cells of B-cell lineage: Both EBV-positive and EBV-negative Variants Exist. American Journal of Surgical Pathology. doi: 10.1097/PAS.0b013e3182785610. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abruzzo LV, Schmidt K, Weiss LM, Jaffe ES, Medeiros LJ, Sander CA, et al. B-cell lymphoma after angioimmunoblastic lymphadenopathy: a case with oligoclonal gene rearrangements associated with Epstein-Barr virus. Blood. 1993 Jul 1;82(1):241–246. [PubMed] [Google Scholar]
- 20.Zettl A, Lee SS, Rudiger T, Starostik P, Marino M, Kirchner T, et al. Epstein-Barr virus-associated B-cell lymphoproliferative disorders in angloimmunoblastic T-cell lymphoma and peripheral T-cell lymphoma, unspecified. American journal of clinical pathology. 2002;117(3):368–379. doi: 10.1309/6UTX-GVC0-12ND-JJEU. [DOI] [PubMed] [Google Scholar]
- 21.Balague O, Martinez A, Colomo L, Rosello E, Garcia A, Martinez-Bernal M, et al. Epstein-Barr Virus Negative Clonal Plasma Cell Proliferations and Lymphomas in Peripheral T-cell Lymphomas: A Phenomenon With Distinctive Clinicopathologic Features. Am J Surg Pathol. 2007 Sep;31(9):1310–1322. doi: 10.1097/PAS.0b013e3180339f18. [DOI] [PubMed] [Google Scholar]
- 22.Huppmann AR, Roullet MR, Raffeld M, Jaffe ES. Angioimmunoblastic T-Cell Lymphoma Partially Obscured by an Epstein-Barr Virus-Negative Clonal Plasma Cell Proliferation. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012 Dec 3; doi: 10.1200/JCO.2012.43.3797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Attygalle AD, Diss TC, Munson P, Isaacson PG, Du MQ, Dogan A. CD10 expression in extranodal dissemination of angioimmunoblastic T-cell lymphoma. Am J Surg Pathol. 2004 Jan;28(1):54–61. doi: 10.1097/00000478-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Yu H, Shahsafaei A, Dorfman DM. Germinal-center T-helper-cell markers PD-1 and CXCL13 are both expressed by neoplastic cells in angioimmunoblastic T-cell lymphoma. American journal of clinical pathology. 2009 Jan;131(1):33–41. doi: 10.1309/AJCP62WRKERPXDRT. [DOI] [PubMed] [Google Scholar]
- 25.de Leval L, Gisselbrecht C, Gaulard P. Advances in the understanding and management of angioimmunoblastic T-cell lymphoma. British journal of haematology. 2010 Mar;148(5):673–689. doi: 10.1111/j.1365-2141.2009.08003.x. [DOI] [PubMed] [Google Scholar]
- 26.Attygalle AD, Chuang SS, Diss TC, Du MQ, Isaacson PG, Dogan A. Distinguishing angioimmunoblastic T-cell lymphoma from peripheral T-cell lymphoma, unspecified, using morphology, immunophenotype and molecular genetics. Histopathology. 2007 Mar;50(4):498–508. doi: 10.1111/j.1365-2559.2007.02632.x. [DOI] [PubMed] [Google Scholar]
- 27.Tan BT, Warnke RA, Arber DA. The frequency of B- and T-cell gene rearrangements and epstein-barr virus in T-cell lymphomas: a comparison between angioimmunoblastic T-cell lymphoma and peripheral T-cell lymphoma, unspecified with and without associated B-cell proliferations. The Journal of molecular diagnostics : JMD. 2006 Sep;8(4):466–75. doi: 10.2353/jmoldx.2006.060016. quiz 527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Federico M, Rudiger T, Bellei M, Nathwani BN, Luminari S, Coiffier B, et al. Clinicopathologic Characteristics of Angioimmunoblastic T-Cell Lymphoma: Analysis of the International Peripheral T-Cell Lymphoma Project. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012 Aug 6; doi: 10.1200/JCO.2011.37.3647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dunleavy K, Wilson WH, Jaffe ES. Angioimmunoblastic T cell lymphoma: pathobiological insights and clinical implications. Current opinion in hematology. 2007 Jul;14(4):348–353. doi: 10.1097/MOH.0b013e328186ffbf. [DOI] [PubMed] [Google Scholar]
- 30.de Leval L, Savilo E, Longtine J, Ferry JA, Harris NL. Peripheral T-cell lymphoma with follicular involvement and a CD4+/bcl-6+ phenotype. Am J Surg Pathol. 2001 Mar;25(3):395–400. doi: 10.1097/00000478-200103000-00015. [DOI] [PubMed] [Google Scholar]
- 31.Agostinelli C, Hartmann S, Klapper W, Korkolopoulou P, Righi S, Marafioti T, et al. Peripheral T cell lymphomas with follicular T helper phenotype: a new basket or a distinct entity? Revising Karl Lennert's personal archive. Histopathology. 2011 Oct;59(4):679–691. doi: 10.1111/j.1365-2559.2011.03981.x. [DOI] [PubMed] [Google Scholar]
- 32.Huang Y, Moreau A, Dupuis J, Streubel B, Petit B, Le Gouill S, et al. Peripheral T-cell lymphomas with a follicular growth pattern are derived from follicular helper T cells (TFH) and may show overlapping features with angioimmunoblastic T-cell lymphomas. Am J Surg Pathol. 2009 May;33(5):682–690. doi: 10.1097/PAS.0b013e3181971591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Leval L, Ferry JA, Falini B, Shipp M, Harris NL. Expression of bcl-6 and CD10 in primary mediastinal large B-cell lymphoma: evidence for derivation from germinal center B cells? Am J Surg Pathol. 2001;25(10):1277–1282. doi: 10.1097/00000478-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Bacon CM, Paterson JC, Liu H, Payne K, Munson P, Du MQ, et al. Peripheral T-cell lymphoma with a follicular growth pattern: derivation from follicular helper T cells and relationship to angioimmunoblastic T-cell lymphoma. British journal of haematology. 2008 Nov;143(3):439–441. doi: 10.1111/j.1365-2141.2008.07352.x. [DOI] [PubMed] [Google Scholar]
- 35.Ikonomou IM, Tierens A, Troen G, Aamot HV, Heim S, Lauritzsen GF, et al. Peripheral T-cell lymphoma with involvement of the expanded mantle zone. Virchows Archiv : an international journal of pathology. 2006 Jul;449(1):78–87. doi: 10.1007/s00428-005-0123-z. [DOI] [PubMed] [Google Scholar]
- 36.Moroch J, Copie-Bergman C, de Leval L, Plonquet A, Martin-Garcia N, Delfau-Larue MH, et al. Follicular peripheral T-cell lymphoma expands the spectrum of classical Hodgkin lymphoma mimics. Am J Surg Pathol. 2012 Nov;36(11):1636–1646. doi: 10.1097/PAS.0b013e318268d9ff. [DOI] [PubMed] [Google Scholar]
- 37.Lemonnier F, Couronne L, Parrens M, Jais JP, Travert M, Lamant L, et al. Recurrent TET2 mutations in peripheral T-cell lymphomas correlate with TFH-like features and adverse clinical parameters. Blood. 2012 Aug 16;120(7):1466–1469. doi: 10.1182/blood-2012-02-408542. [DOI] [PubMed] [Google Scholar]
- 38.Streubel B, Vinatzer U, Willheim M, Raderer M, Chott A. Novel t(5;9)(q33;q22) fuses ITK to SYK in unspecified peripheral T-cell lymphoma. Leukemia : official journal of the Leukemia Society of America, Leukemia Research Fund, UK. 2006 Feb;20(2):313–318. doi: 10.1038/sj.leu.2404045. [DOI] [PubMed] [Google Scholar]
- 39.Fraga M, Brousset P, Schlaifer D, Payen C, Robert A, Rubie H, et al. Bone marrow involvement in anaplastic large cell lymphoma. Immunohistochemical detection of minimal disease and its prognostic significance. American journal of clinical pathology. 1995 Jan;103(1):82–89. doi: 10.1093/ajcp/103.1.82. [DOI] [PubMed] [Google Scholar]
- 40.Jaffe ES. Anaplastic large cell lymphoma: the shifting sands of diagnostic hematopathology. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2001 Mar;14(3):219–228. doi: 10.1038/modpathol.3880289. [DOI] [PubMed] [Google Scholar]
- 41.Bonzheim I, Geissinger E, Roth S, Zettl A, Marx A, Rosenwald A, et al. Anaplastic large cell lymphomas lack the expression of T-cell receptor molecules or molecules of proximal T-cell receptor signaling. Blood. 2004 Nov 15;104(10):3358–3360. doi: 10.1182/blood-2004-03-1037. [DOI] [PubMed] [Google Scholar]
- 42.Falini B, Pileri S, Zinzani PL, Carbone A, Zagonel V, Wolf-Peeters C, et al. ALK+ lymphoma: clinico-pathological findings and outcome. Blood. 1999;93(8):2697–2706. [PubMed] [Google Scholar]
- 43.Savage KJ, Harris NL, Vose JM, Ullrich F, Jaffe ES, Connors JM, et al. ALK- anaplastic large-cell lymphoma is clinically and immunophenotypically different from both ALK+ ALCL and peripheral T-cell lymphoma, not otherwise specified: report from the International Peripheral T-Cell Lymphoma Project. Blood. 2008 Jun 15;111(12):5496–5504. doi: 10.1182/blood-2008-01-134270. [DOI] [PubMed] [Google Scholar]
- 44.Brugieres L, Quartier P, Le Deley MC, Pacquement H, Perel Y, Bergeron C, et al. Relapses of childhood anaplastic large-cell lymphoma: treatment results in a series of 41 children--a report from the French Society of Pediatric Oncology. Annals of oncology : official journal of the European Society for Medical Oncology / ESMO. 2000 Jan;11(1):53–58. doi: 10.1023/a:1008352726155. [DOI] [PubMed] [Google Scholar]
- 45.Lamant L, McCarthy K, d'Amore E, Klapper W, Nakagawa A, Fraga M, et al. Prognostic impact of morphologic and phenotypic features of childhood ALK-positive anaplastic large-cell lymphoma: results of the ALCL99 study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011 Dec 10;29(35):4669–4676. doi: 10.1200/JCO.2011.36.5411. [DOI] [PubMed] [Google Scholar]
- 46.Ferreri AJ, Govi S, Pileri SA, Savage KJ. Anaplastic large cell lymphoma, ALK-negative. Critical reviews in oncology/hematology. 2012 Jul 10; doi: 10.1016/j.critrevonc.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 47.Salaverria I, Bea S, Lopez-Guillermo A, Lespinet V, Pinyol M, Burkhardt B, et al. Genomic profiling reveals different genetic aberrations in systemic ALK-positive and ALK-negative anaplastic large cell lymphomas. British journal of haematology. 2008 Mar;140(5):516–526. doi: 10.1111/j.1365-2141.2007.06924.x. [DOI] [PubMed] [Google Scholar]
- 48.Thompson MA, Stumph J, Henrickson SE, Rosenwald A, Wang Q, Olson S, et al. Differential gene expression in anaplastic lymphoma kinase-positive and anaplastic lymphoma kinase-negative anaplastic large cell lymphomas. Human pathology. 2005 May;36(5):494–504. doi: 10.1016/j.humpath.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 49.Lamant L, de Reynies A, Duplantier MM, Rickman DS, Sabourdy F, Giuriato S, et al. Gene-expression profiling of systemic anaplastic large-cell lymphoma reveals differences based on ALK status and two distinct morphologic ALK+ subtypes. Blood. 2007 Mar 1;109(5):2156–2164. doi: 10.1182/blood-2006-06-028969. [DOI] [PubMed] [Google Scholar]
- 50.Feldman AL, Dogan A, Smith DI, Law ME, Ansell SM, Johnson SH, et al. Discovery of recurrent t(6;7)(p25.3;q32.3) translocations in ALK-negative anaplastic large cell lymphomas by massively parallel genomic sequencing. Blood. 2011 Jan 20;117(3):915–919. doi: 10.1182/blood-2010-08-303305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bekkenk MW, Geelen FA, van Voorst Vader PC, Heule F, Geerts ML, van Vloten WA, et al. Primary and secondary cutaneous CD30(+) lymphoproliferative disorders: a report from the Dutch Cutaneous Lymphoma Group on the long-term follow-up data of 219 patients and guidelines for diagnosis and treatment. Blood. 2000 Jun 15;95(12):3653–3661. [PubMed] [Google Scholar]
- 52.Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005 May 15;105(10):3768–3785. doi: 10.1182/blood-2004-09-3502. [DOI] [PubMed] [Google Scholar]
- 53.Sciallis AP, Law ME, Inwards DJ, McClure RF, Macon WR, Kurtin PJ, et al. Mucosal CD30-positive T-cell lymphoproliferations of the head and neck show a clinicopathologic spectrum similar to cutaneous CD30-positive T-cell lymphoproliferative disorders. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2012 Jul;25(7):983–992. doi: 10.1038/modpathol.2012.38. [DOI] [PubMed] [Google Scholar]
- 54.Eberle FC, Song JY, Xi L, Raffeld M, Harris NL, Wilson WH, et al. Nodal involvement by cutaneous CD30-positive T-cell lymphoma mimicking classical Hodgkin lymphoma. Am J Surg Pathol. 2012 May;36(5):716–725. doi: 10.1097/PAS.0b013e3182487158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oschlies I, Lisfeld J, Lamant L, Nakazawa A, E DA, Hansson U, et al. ALK-positive anaplastic large cell lymphoma limited to the skin: clinical, histopathological and molecular analysis of 6 pediatric cases-a report from the ALCL99 study. Haematologica. 2012 Jul 6; doi: 10.3324/haematol.2012.065664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Feldman AL, Law M, Remstein ED, Macon WR, Erickson LA, Grogg KL, et al. Recurrent translocations involving the IRF4 oncogene locus in peripheral T-cell lymphomas. Leukemia : official journal of the Leukemia Society of America, Leukemia Research Fund, UK. 2009 Mar;23(3):574–580. doi: 10.1038/leu.2008.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wada DA, Law ME, Hsi ED, Dicaudo DJ, Ma L, Lim MS, et al. Specificity of IRF4 translocations for primary cutaneous anaplastic large cell lymphoma: a multicenter study of 204 skin biopsies. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2011 Apr;24(4):596–605. doi: 10.1038/modpathol.2010.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kempf W, Pfaltz K, Vermeer MH, Cozzio A, Ortiz-Romero PL, Bagot M, et al. EORTC, ISCL, and USCLC consensus recommendations for the treatment of primary cutaneous CD30-positive lymphoproliferative disorders: lymphomatoid papulosis and primary cutaneous anaplastic large-cell lymphoma. Blood. 2011 Oct 13;118(15):4024–4035. doi: 10.1182/blood-2011-05-351346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO Classification of Tumours of the Digestive System. Lyon: IARC; 2010. [Google Scholar]
- 60.Delabie J, Holte H, Vose JM, Ullrich F, Jaffe ES, Savage KJ, et al. Enteropathy-associated T-cell lymphoma: clinical and histological findings from the international peripheral T-cell lymphoma project. Blood. 2011 Jul 7;118(1):148–155. doi: 10.1182/blood-2011-02-335216. [DOI] [PubMed] [Google Scholar]
- 61.Fasano A, Catassi C. Celiac Disease. New England Journal of Medicine. 2012;367(25):2419–2426. doi: 10.1056/NEJMcp1113994. [DOI] [PubMed] [Google Scholar]
- 62.Zettl A, deLeeuw R, Haralambieva E, Mueller-Hermelink HK. Enteropathy-type T-cell lymphoma. American journal of clinical pathology. 2007 May;127(5):701–706. doi: 10.1309/nw2bk1dxb0eqg55h. [DOI] [PubMed] [Google Scholar]
- 63.de Mascarel A, Belleannee G, Stanislas S, Merlio C, Parrens M, Laharie D, et al. Mucosal intraepithelial T-lymphocytes in refractory celiac disease: a neoplastic population with a variable CD8 phenotype. Am J Surg Pathol. 2008 May;32(5):744–751. doi: 10.1097/PAS.0b013e318159b478. [DOI] [PubMed] [Google Scholar]
- 64.Malamut G, El Machhour R, Montcuquet N, Martin-Lanneree S, Dusanter-Fourt I, Verkarre V, et al. IL-15 triggers an antiapoptotic pathway in human intraepithelial lymphocytes that is a potential new target in celiac disease-associated inflammation and lymphomagenesis. The Journal of clinical investigation. 2010 Jun;120(6):2131–2143. doi: 10.1172/JCI41344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mention JJ, Ben Ahmed M, Begue B, Barbe U, Verkarre V, Asnafi V, et al. Interleukin 15: a key to disrupted intraepithelial lymphocyte homeostasis and lymphomagenesis in celiac disease. Gastroenterology. 2003 Sep;125(3):730–745. doi: 10.1016/s0016-5085(03)01047-3. [DOI] [PubMed] [Google Scholar]
- 66.Chan JK, Chan AC, Cheuk W, Wan SK, Lee WK, Lui YH, et al. Type II enteropathy-associated T-cell lymphoma: a distinct aggressive lymphoma with frequent gammadelta T-cell receptor expression. Am J Surg Pathol. 2011 Oct;35(10):1557–1569. doi: 10.1097/PAS.0b013e318222dfcd. [DOI] [PubMed] [Google Scholar]
- 67.Akiyama T, Okino T, Konishi H, Wani Y, Notohara K, Tsukayama C, et al. CD8+, CD56+ (natural killer-like) T-cell lymphoma involving the small intestine with no evidence of enteropathy: clinicopathology and molecular study of five Japanese patients. Pathol Int. 2008 Oct;58(10):626–634. doi: 10.1111/j.1440-1827.2008.02281.x. [DOI] [PubMed] [Google Scholar]
- 68.Tung CL, Hsieh PP, Chang JH, Chen RS, Chen YJ, Wang JS. Intestinal T-cell and natural killer-cell lymphomas in Taiwan with special emphasis on 2 distinct cellular types: natural killer-like cytotoxic T cell and true natural killer cell. Human pathology. 2008 Jul;39(7):1018–1025. doi: 10.1016/j.humpath.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 69.Cooke CB, Krenacs L, Stetler-Stevenson M, Greiner TC, Raffeld M, Kingma DW, et al. Hepatosplenic T-cell lymphoma: a distinct clinicopathologic entity of cytotoxic gamma delta T-cell origin. Blood. 1996 Dec 1;88(11):4265–4274. [PubMed] [Google Scholar]
- 70.Belhadj K, Reyes F, Farcet JP, Tilly H, Bastard C, Angonin R, et al. Hepatosplenic gammadelta T-cell lymphoma is a rare clinicopathologic entity with poor outcome: report on a series of 21 patients. Blood. 2003 Dec 15;102(13):4261–4269. doi: 10.1182/blood-2003-05-1675. [DOI] [PubMed] [Google Scholar]
- 71.Gaulard P, Belhadj K, Reyes F. Gammadelta T-cell lymphomas. Seminars in hematology. 2003 Jul;40(3):233–243. doi: 10.1016/s0037-1963(03)00137-9. [DOI] [PubMed] [Google Scholar]
- 72.Vega F, Medeiros LJ, Gaulard P. Hepatosplenic and other gammadelta T-cell lymphomas. American journal of clinical pathology. 2007 Jun;127(6):869–880. doi: 10.1309/LRKX8CE7GVPCR1FT. [DOI] [PubMed] [Google Scholar]
- 73.Wu H, Wasik MA, Przybylski G, Finan J, Haynes B, Moore H, et al. Hepatosplenic gamma-delta T-cell lymphoma as a late-onset posttransplant lymphoproliferative disorder in renal transplant recipients. American journal of clinical pathology. 2000;113(4):487–496. doi: 10.1309/YTTC-F55W-K9CP-EPX5. [DOI] [PubMed] [Google Scholar]
- 74.Mackey AC, Green L, Liang LC, Dinndorf P, Avigan M. Hepatosplenic T cell lymphoma associated with infliximab use in young patients treated for inflammatory bowel disease. Journal of pediatric gastroenterology and nutrition. 2007 Feb;44(2):265–267. doi: 10.1097/MPG.0b013e31802f6424. [DOI] [PubMed] [Google Scholar]
- 75.Rosh JR, Gross T, Mamula P, Griffiths A, Hyams J. Hepatosplenic T-cell lymphoma in adolescents and young adults with Crohn's disease: a cautionary tale? Inflammatory bowel diseases. 2007 Aug 13;(8):1024–1030. doi: 10.1002/ibd.20169. [DOI] [PubMed] [Google Scholar]
- 76.Farcet JP, Gaulard P, Marolleau JP, Le Couedic JP, Henni T, Gourdin MF, et al. Hepatosplenic T-cell lymphoma: sinusal/sinusoidal localization of malignant cells expressing the T-cell receptor gamma delta. Blood. 1990 Jun 1;75(11):2213–2219. [PubMed] [Google Scholar]
- 77.Krenacs L, Smyth MJ, Bagdi E, Krenacs T, Kopper L, Rudiger T, et al. The serine protease granzyme M is preferentially expressed in NK-cell, gamma delta T-cell, and intestinal T-cell lymphomas: evidence of origin from lymphocytes involved in innate immunity. Blood. 2003 May 1;101(9):3590–3593. doi: 10.1182/blood-2002-09-2908. [DOI] [PubMed] [Google Scholar]
- 78.Morice WG, Macon WR, Dogan A, Hanson CA, Kurtin PJ. NK-cell-associated receptor expression in hepatosplenic T-cell lymphoma, insights into pathogenesis. Leukemia : official journal of the Leukemia Society of America, Leukemia Research Fund, UK. 2006 May;20(5):883–886. doi: 10.1038/sj.leu.2404168. [DOI] [PubMed] [Google Scholar]
- 79.Macon WR, Levy NB, Kurtin PJ, Salhany KE, Elkhalifa MY, Casey TT, et al. Hepatosplenic alphabeta T-cell lymphomas: a report of 14 cases and comparison with hepatosplenic gammadelta T-cell lymphomas. Am J Surg Pathol. 2001 Mar;25(3):285–296. doi: 10.1097/00000478-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 80.Miyazaki K, Yamaguchi M, Imai H, Kobayashi T, Tamaru S, Nishii K, et al. Gene expression profiling of peripheral T-cell lymphoma including gammadelta T-cell lymphoma. Blood. 2009 Jan 29;113(5):1071–1074. doi: 10.1182/blood-2008-07-166363. [DOI] [PubMed] [Google Scholar]
- 81.Travert M, Huang Y, de Leval L, Martin-Garcia N, Delfau-Larue MH, Berger F, et al. Molecular features of hepatosplenic T-cell lymphoma unravels potential novel therapeutic targets. Blood. 2012 Jun 14;119(24):5795–5806. doi: 10.1182/blood-2011-12-396150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huppmann AR, Xi L, Pittaluga S, Raffeld M, Jaffe ES. Subcutaneous panniculitis-likeT-cell lymphoma in the pedatric age group: A lymphoma of low malignant potential. Pediatric Blood and Cancer. doi: 10.1002/pbc.24462. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kumar S, Krenacs L, Medeiros J, Elenitoba-Johnson KS, Greiner TC, Sorbara L, et al. Subcutaneous panniculitic T-cell lymphoma is a tumor of cytotoxic T lymphocytes. Human pathology. 1998 Apr;29(4):397–403. doi: 10.1016/s0046-8177(98)90122-8. [DOI] [PubMed] [Google Scholar]
- 84.Salhany KE, Macon WR, Choi JK, Elenitsas R, Lessin SR, Felgar RE, et al. Subcutaneous panniculitis-like T-cell lymphoma: clinicopathologic, immunophenotypic, and genotypic analysis of alpha/beta and gamma/delta subtypes. Am J Surg Pathol. 1998 Jul;22(7):881–893. doi: 10.1097/00000478-199807000-00010. [DOI] [PubMed] [Google Scholar]
- 85.Massone C, Lozzi GP, Egberts F, Fink-Puches R, Cota C, Kerl H, et al. The protean spectrum of non-Hodgkin lymphomas with prominent involvement of subcutaneous fat. Journal of cutaneous pathology. 2006 Jun;33(6):418–425. doi: 10.1111/j.0303-6987.2006.00493.x. [DOI] [PubMed] [Google Scholar]
- 86.Willemze R, Jansen PM, Cerroni L, Berti E, Santucci M, Assaf C, et al. Subcutaneous panniculitis-like T-cell lymphoma: definition, classification, and prognostic factors: an EORTC Cutaneous Lymphoma Group Study of 83 cases. Blood. 2008 Jan 15;111(2):838–845. doi: 10.1182/blood-2007-04-087288. [DOI] [PubMed] [Google Scholar]
- 87.Pincus LB, LeBoit PE, McCalmont TH, Ricci R, Buzio C, Fox LP, et al. Subcutaneous panniculitis-like T-cell lymphoma with overlapping clinicopathologic features of lupus erythematosus: coexistence of 2 entities? The American Journal of dermatopathology. 2009 Aug 31;(6):520–526. doi: 10.1097/DAD.0b013e3181a84f32. [DOI] [PubMed] [Google Scholar]
- 88.Gonzalez CL, Medeiros LJ, Braziel RM, Jaffe ES. T-cell lymphoma involving subcutaneous tissue. A clinicopathologic entity commonly associated with hemophagocytic syndrome. Am J Surg Pathol. 1991 Jan;15(1):17–27. doi: 10.1097/00000478-199101000-00002. [DOI] [PubMed] [Google Scholar]
- 89.Toro JR, Beaty M, Sorbara L, Turner ML, White J, Kingma DW, et al. Gamma delta T-cell lymphoma of the skin: a clinical, microscopic, and molecular study. Archives of Dermatology. 2000;136(8):1024–1032. doi: 10.1001/archderm.136.8.1024. [DOI] [PubMed] [Google Scholar]
- 90.Toro JR, Liewehr DJ, Pabby N, Sorbara L, Raffeld M, Steinberg SM, et al. Gamma-delta T-cell phenotype is associated with significantly decreased survival in cutaneous T-cell lymphoma. Blood. 2003;101(9):3407–3412. doi: 10.1182/blood-2002-05-1597. [DOI] [PubMed] [Google Scholar]
- 91.Ghobrial IM, McCormick DJ, Kaufmann SH, Leontovich AA, Loegering DA, Dai NT, et al. Proteomic analysis of mantle-cell lyrnphoma by protein microarray. Blood. 2005 May 1;105(9):3722–3730. doi: 10.1182/blood-2004-10-3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Garcia-Herrera A, Song JY, Chuang SS, Villamor N, Colomo L, Pittaluga S, et al. Nonhepatosplenic gammadelta T-cell lymphomas represent a spectrum of aggressive cytotoxic T-cell lymphomas with a mainly extranodal presentation. Am J Surg Pathol. 2011 Aug;35(8):1214–1225. doi: 10.1097/PAS.0b013e31822067d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rothe A, Sasse S, Goergen H, Eichenauer DA, Lohri A, Jager U, et al. Brentuximab vedotin for relapsed or refractory CD30+ hematologic malignancies: the German Hodgkin Study Group experience. Blood. 2012 Aug 16;120(7):1470–1472. doi: 10.1182/blood-2012-05-430918. [DOI] [PubMed] [Google Scholar]
- 94.Mologni L. Inhibitors of the anaplastic lymphoma kinase. Expert Opin Investig Drugs. 2012 Jul;21(7):985–994. doi: 10.1517/13543784.2012.690031. [DOI] [PubMed] [Google Scholar]