Abstract
The objective of this study was to report a collision tumor of papillary and follicular carcinoma of the thyroid. Case report and review of the literature was studied. A 62 year old female presented with a thyroid mass diagnosed the year prior. Physical exam revealed a 6 × 4 cm predominantly left sided thyroid mass that was confirmed on imaging as well. Thyroid function tests were within normal limits. Ultrasound-guided fine needle aspiration suggested a follicular neoplasm. Consequently, the patient underwent a left hemi-thyroidectomy. The pathology was reported as being collision tumor with a combination of follicular and papillary carcinoma. A completion thyroidectomy was performed followed by post operative radio-iodine therapy. Collision tumors are rare involving two or more histologically distinct neoplastic morphologies separated by normal tissue in one or more organ systems. This is to our knowledge the first report of a collision tumor of the thyroid involving a follicular and papillary carcinoma.
Keywords: Collision tumor thyroid, Follicular carcinoma thyroid, Papillary carcinoma thyroid
Introduction
The term “collision tumor” refers to the coexistence of two or more histologically distinct neoplastic morphologies separated by normal tissue in one or more organ systems. With regard to the thyroid gland, collision tumors are rare, with most literature describing co-occurring medullary and papillary carcinomas, or metastatic tumors coexisting with papillary carcinoma of the thyroid gland [1–3, 6]. We report a case of a papillary carcinoma and follicular carcinoma in the thyroid.
Case Report
A 62 year old female presented to our service for the evaluation of a thyroid mass that was diagnosed 1 year prior to her visit. Since the time of diagnosis, she reported having increased shortness of breath, symptoms suggestive of mild palpitations, increased sweating, and sleep disturbance which on further investigation were not related to her thyroid gland. A review of all other systems was negative. Her past medical, social, and surgical histories were noncontributory. Clinically, there were no signs of overt thyrotoxicosis. Physical exam revealed a 6 × 4 cm thyroid mass predominantly in the left lobe with no cervical lymphadenopathy. The patient’s thyroid function tests (TSH, T4) were within normal limits. Flexible laryngoscopy confirmed normal vocal cord function. Ultrasound revealed a diffusely nodular thyroid gland, with a 5.7 cm × 3.0 cm predominantly solid nodule in the left thyroid lobe. Fine needle aspiration biopsy was suspicious for follicular neoplasm, and included a differential diagnosis of follicular adenoma, follicular carcinoma, and a follicular variant of papillary carcinoma. After obtaining informed consent, she underwent a left hemi-thyroidectomy. The final pathology report revealed combined follicular and papillary carcinoma (Fig. 1), with the widely invasive follicular component measuring 4.1 cm in greatest dimension (Fig. 2), and the multifocal papillary component measuring 1 cm in greatest dimension (Fig. 3). There was evidence of extensive vascular invasion by the follicular carcinoma component (Fig. 4). There was no evidence of extrathyroidal extension. The patient underwent a completion right hemi-thyroidectomy, which revealed nodular Hashimoto thyroiditis of the right lobe, along with a 3 mm encapsulated nodule that pathology confirmed as being a minimally invasive follicular carcinoma. The patient was subsequently referred for radio-iodine therapy.
Fig. 1.
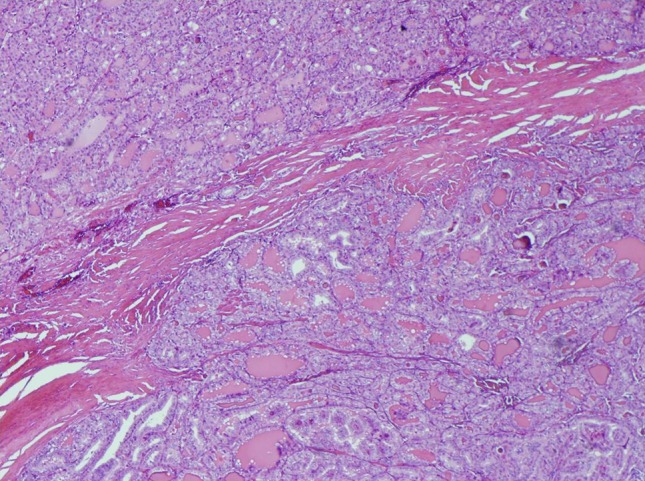
Follicular carcinoma with an area of capsular invasion. The tumor is comprised of small follicles which are seen completely bridging the thick fibrous capsule
Fig. 2.
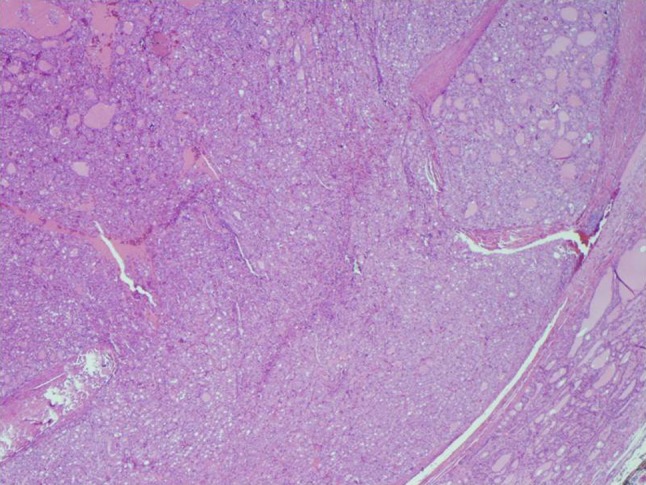
Vascular invasion by the follicular carcinoma. A tumor plug is present within a vascular lumen surrounded by endothelium
Fig. 3.
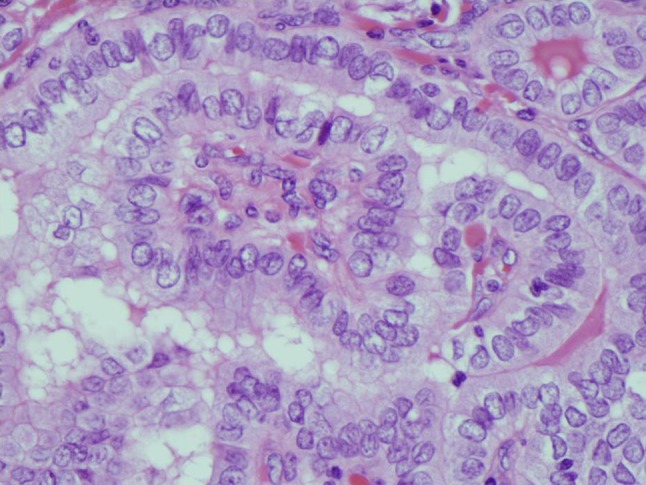
Papillary carcinoma characterized by enlarged ovoid nuclei with frequent nuclear grooves and small distinct nucleoli. The chromatin is powdery and focally shows optical clearing. There is nuclear crowding and overlap. Small papillae are present
Fig. 4.
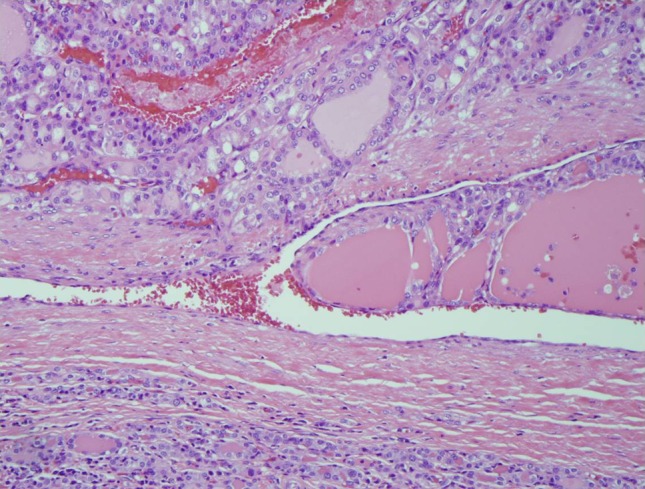
The follicular carcinoma and papillary carcinoma closely approximate each other, only separated by a thin layer of fibrous tissue
Discussion
Papillary carcinomas are the most common malignancy of the thyroid, accounting for 60–65% of thyroid cancer [2]. Follicular carcinoma of the thyroid is the second most common type of malignancy affecting the thyroid, comprising about 15% of cases. Both types show peak onset from the fourth through seventh decades of life, with incidence in females outnumbering males 3:1 [4]. While both types are considered to be relatively quiescent, papillary carcinoma shows a predilection for lymphatic metastasis, while follicular carcinoma tends to metastasize hematogenously [5]. This is the first report of these two separate pathologies occurring simultaneously but independently as a collision phenomenon within the thyroid gland. This presentation increases the potential risk to the patient for both lymphatic and hematogenous metastasis from these individual pathologies. Although, this presentation involved two well differentiated tumors with good prognosis, the presence of two primary cancers should heighten the suspicion for an aggressive potential and increased risk of recurrence.
Collision tumors of the thyroid gland are rare. Consequently, there is a paucity of reported literature on these tumors to date. With regard to the thyroid gland, there have been 19 cases involving a combination of medullary and papillary carcinoma [6]. There have also been several reports of metastatic lesions appearing in conjunction with papillary carcinoma [1–3]. One case report has documented a collision tumor of primary squamous cell carcinoma and papillary carcinoma of the thyroid [7]. Greater understanding of the various combinations of pathologies and their impact on prognosis, treatment, and potential for recurrence can only be achieved by diligent reporting of this rare phenomenon and maintaining follow up data on these patients.
Acknowledgments
Conflict of interest
None.
References
- 1.Brandwein-Gensler M, Urken M, Wang B. Collision tumor of the thyroid: a case report of metastatic liposarcoma plus papillary thyroid carcinoma. Head Neck. 2004;26:637–641. doi: 10.1002/hed.20024. [DOI] [PubMed] [Google Scholar]
- 2.Fortson JK, Durden FL, Jr, Patel V, Darkeh A. The coexistence of anaplastic and papillary carcinomas of the thyroid: a case presentation and literature review. Am Surg. 2004;70:1116–1119. [PubMed] [Google Scholar]
- 3.Jacobson AS, Wenig BM, Urken ML. Collision tumor of the thyroid and larynx: a patient with papillary thyroid carcinoma colliding with laryngeal squamous cell carcinoma. Thyroid. 2008;18:1325–1328. doi: 10.1089/thy.2008.0280. [DOI] [PubMed] [Google Scholar]
- 4.Kilfoy BA, Devesa SS, Ward MH, Zhang Y, et al. Gender is an age-specific effect modifier for papillary cancers of the thyroid gland. Cancer Epidemiol Biomark Prev. 2009;18(4):1092–1100. doi: 10.1158/1055-9965.EPI-08-0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin X, Zhu B, Liu Y, Silverman JF. Follicular thyroid carcinoma invades venous rather than lymphatic vessels. Diagn Pathol. 2010;22(5):8. doi: 10.1186/1746-1596-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rossi S, Fugazzola L, De Pasquale L. Medullary and papillary carcinoma of the thyroid gland occurring as a collision tumour: report of three cases with molecular analysis and review of the literature. Endocr Relat Cancer. 2005;12:281–289. doi: 10.1677/erc.1.00901. [DOI] [PubMed] [Google Scholar]
- 7.Walvekar RR, Kane SV, D’Cruz AK. Collision tumor of the thyroid: follicular variant of papillary carcinoma and squamous carcinoma. World J Surg Oncol. 2006;4:65. doi: 10.1186/1477-7819-4-65. [DOI] [PMC free article] [PubMed] [Google Scholar]


