Abstract
Sinonasal malignancies are said to be a highly heterogeneous group of cancers, accounting for less than 1 % of all cancers and less than 3 % of all upper aerodigestive tract tumors. Originating from any histologic components of the sinonasal cavity, the histopathology of these tumors is diverse. Accordingly, treatment options vary, surgery being the mainstay in most of them. Recurrence rates differs with each histological type of tumor, dependent on various factors. In this article, we have tried to identify the prevalent characteristics of sinonasal malignancies and to outline the prognostic factors affecting the outcome. It is a retrospective study design with a total number of 102 patients. Patients diagnosed with sinonasal malignancies were included and any patient previously operated outside our institute or having received prior radiation or chemotherapy were excluded. The patients were selected over a period of 10 years, from 2000 to 2010. Data was analyzed using SPSS 17. Majority of the sinonasal tumors were squamous cell carcinomas involving the maxillary sinus. Locoregional recurrence was found to be more frequent in patients with positive neck nodes on final histopathology. Sinonasal malignancies are mostly squamous cell in variety and recurrence of these rare entities is dependent on the histological variety and the presence of positive neck nodes.
Keywords: Sinonasal malignancy, Locoregional recurrence, Squamous cell carcinoma, Positive neck nodes
Malignant lesions involving the sino-nasal tract account for 0.2–0.8 % overall and 3 % of all head and neck malignancies [1]. Approximately 55 % of these lesions are carcinomas with involvement of neck nodes in 7–15 % of the conditions. Treatment involves a wide variety of modalities, including surgery, radiotherapy, and chemotherapy, alone or in combination, however, there is still great controversy about the ideal treatment [1, 2]. In 2003, the American Joint Committee on Cancer (AJCC) published the sixth edition of the sino-nasal tumor staging system [3]. This was in contrast to the fifth-edition staging system of sino-nasal cancer in which the surgically resectable tumors and non-resectable tumors were all grouped together in the T4 stage [4]. As a result it was difficult to evaluate the results of surgery and a newer staging system was introduced.
Despite these improvements, the fact is that there is no widely accepted staging system for tumors of the nasal cavity and ethmoid/sphenoid sinuses. The AJCC tumor stage classification only includes the maxillary sinus [5]. As obvious, this proves difficulties in tumors involving multiple sites in which the primary originating site is difficult to identify.
We analysed retrospectively our 10 years experience of managing sino-nasal tumors, with a series of 63 patients. Our aim was to identify prognostic factors and outcomes in this group of patients.
Objective
To identify the characteristic features of malignant neoplasms of the sinonasal tract and the factors affecting the loco-regional recurrence.
Materials and Methods
The study was performed via a retrospective chart review over a period of ten years, from 2000 to 2010, at the Aga Khan University Hospital, Department of Otolaryngology-Head and Neck Surgery. One hundred and nine patients were included in the study. Malignancies arising from the nasopharynx or previously treated outside the institute were excluded. Patients lost to follow up and with incomplete documentation were also excluded. Patients operated less than 6 months before the final data collection were not included. Hence, final sample size was one hundred and two.
Patients were followed up at monthly intervals in the first year and then at 2–3 month intervals for the next 2 years. Follow up was counted from the date of the first follow up till the last or death. Data was collected up to March 2012.
Analysis
Using Chi Square test, the p value for loco-regional recurrence rate was calculated with respect to nodal status, tumor site, size, stage and histology of tumor. Frequencies were also calculated for descriptive data. Data was analysed using SPSS 17.
Results
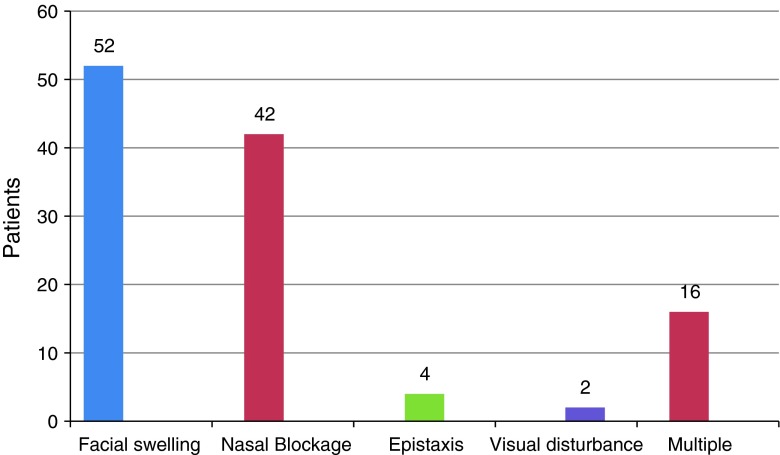
Seventy of the patients were males, the remaining females. The age ranged from 23 to 88 years with a mean age of 50 years. The most frequent presenting symptom was facial swelling, present in 52 (51 %) patients, followed by nasal blockage in 42 (41 %), epistaxis in eight and visual disturbances in two patient respectively. Around sixteen patients (15 %) had more than one presenting symptom (Fig. 1).
Fig. 1.
Presenting symptoms
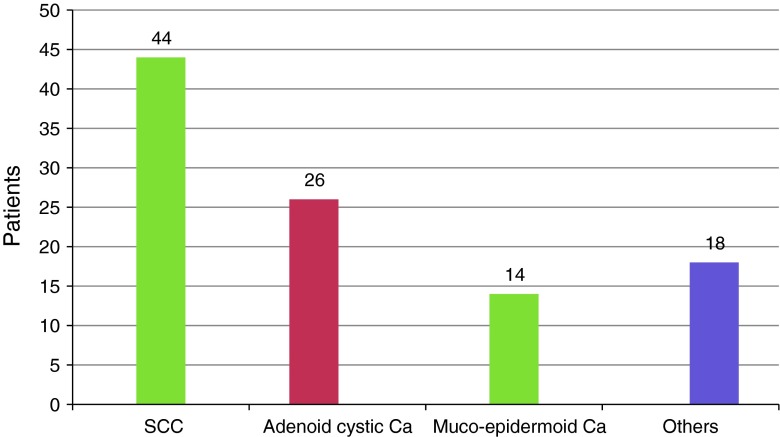
Interestingly the right side was the more frequent side involved with a total of 56 patients (55 %). Within the sinonasal cavity, the maxillary sinus remained the most frequent site to be effected. Sixty patients (59 %) had tumor of the maxillary sinus, twenty (19.6 %) within the nasal cavity and four (4 %) in the ethmoids. Eighteen patients (17.6 %) had tumor involving multiple sites. Squamous cell carcinoma was present in forty four patients (44 %), adenoid cystic carcinoma in 26 (25 %), mucoepidermoid carcinoma in fourteen (15 %) and eighteen had various other malignancies (Fig. 2). The malignancies were classified according to the AJCC classification. Stage I was present in sixteen (15.6 %) patients, stage II in 58 (57 %), stage III in eight (8 %)and stage IV in twenty (19.6 %) individuals. About 50 patients were treated with surgery, 38 individuals were managed by surgery followed by radiation and fourteen underwent surgery followed by chemoradiation. Based on clinical and radiological examination, twenty patients underwent neck dissection.
Fig. 2.
Histopathology of malignancy
The minimum follow up period was about 12 months, with a loco-regional recurrence rate of 39 % (20 patients). Fourteen out of twenty patients, who had undergone neck dissection, had positive neck nodes on final histopathology report.
Ten of the patients with histologically positive neck nodes had recurrence, which was statistically significant (p value 0.04). Additionally, tumor histology had a significant association with the recurrence of disease, with a p value of 0.023. Variables like tumor site, stage and size did not show any significant association with loco-regional recurrence (Table 1).
Table 1.
Association with recurrence
| Recurrence (n = 40) | p value | ||
|---|---|---|---|
| Yes | No | ||
| Neck nodes | 10 | 4 | 0.04 |
| Tumor histology | |||
| Squamous cell carcinoma | 16 | 28 | 0.023 |
| Adenoid cystic carcinoma | 8 | 18 | |
| Mucoepidermoid carcinoma | 10 | 14 | |
| Others | 6 | 12 | |
| Tumor site | |||
| Maxillary sinus | 24 | 34 | 0.82 |
| Ethmoids | 3 | 1 | |
| Nasal cavity | 4 | 16 | |
| Others | 9 | 9 | |
| Tumor size | |||
| Less than 2 cm | 6 | 14 | 0.8 |
| 2–4 cm | 22 | 40 | |
| More than 4 cm | 12 | 8 | |
| Tumor staging | |||
| Stage I | 6 | 10 | 0.6 |
| Stage II | 12 | 46 | |
| Stage III | 6 | 2 | |
| Stage IV | 16 | 4 | |
Conclusion
Sinonasal malignancies have a loco-regional recurrence rate of 39 %. It was noted that the presence of histologically positive neck nodes and histology of the tumor was significantly associated with disease recurrence.
Discussion
Sinonasal malignancies are a highly diverse group of cancers, accounting for 0.2–0.8 % of all cancers and less than 3 % of all upper-aero digestive tract tumors. These lesions may arise from various histologic components of the sino-nasal tract, such as the Schneiderian mucosa, minor salivary glands, neural tissue, and lymphatics, all of which give rise to a heterogeneous group of disease [6]. Majority of these tumors (60 %) arise from the maxillary sinus, with 20 % arising from the nasal cavity, 5 % from the ethmoid sinuses, and 3 % from the sphenoid and frontal sinuses [2, 7]. Squamous cell carcinoma followed by salivary gland tumors is the most frequent neoplasm encountered (55 %), followed by non-epithelial tumors (20 %) and glandular tumors (15 %) [8, 9].
The use of Ohngren’s line, which is an imaginary plane from the medial canthus of the eye to the angle of the mandible, is adopted by some. It basically separates the para-nasal sinuses into anterior inferior (infrastructure) and superior posterior (suprastructure) sites. Infrastructure carcinomas are associated with a good prognosis, whereas carcinomas of the suprastructure are associated with a poor prognosis because of ready spread of these tumors to the eye, skull base, pterygoids, and infratemporal fossa [8].
Apart from all these, the AJCC proposed a new staging system. Literature supported that the fifth edition of the AJCC staging system was inappropriate for presuming the prognosis of the disease when compared with the 1997 Union Internationale Contre de Cancer (UICC)-AICC staging system. These factors were taken into consideration when proposing a revised sixth edition [10].
Majority of cases present at an advanced stage of disease, with a massive tumor size and invading surrounding bony structures and sinuses, leading to a high frequency of local failure and poor outcome [11] (Fig. 3). One of the major factors responsible for this is that there is considerable variation in symptoms ranging from nasal airway obstruction, facial pain, pressure and epistaxis. These presenting features can be frequently mistaken for sinusitis or upper respiratory tract infections leading to delayed intervention. Additionally, secondary infection is common resulting in a muco-purulent discharge. Advanced staged disease presents with proptosis, diplopia, cerebrospinal fluid leak and epiphora due to invasion intracranially or the orbit.
Fig. 3.
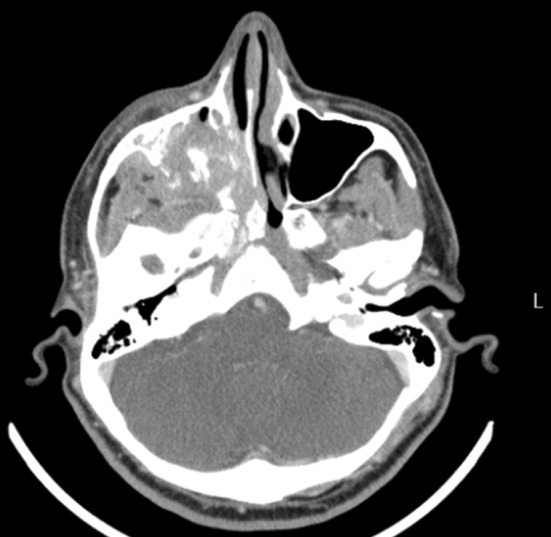
Malignant neoplasm involving right maxilla with extension into the infra-temporal fossa
Squamous cell carcinoma is the most common histology encountered in literature [12]. This finding is apparent in our study as well. Histological status has led to variations in survival rates and recurrences. Literature states that in comparison of epithelial versus non-epithelial tumors, the local control rate and disease free survival rate is lower for epithelial tumors [13]. The 5 year survival rate for adenocarcinomas and adenoid cystic carcinomas range between 40 and 60 % whereas for squamous cell carcinomas have a 5 year survival of 25–50 % [14].
For squamous cell carcinoma, the recurrence rate is reported around 56 % with a poor prognosis in case of extension into the surrounding structures [15]. Our findings showed that squamous cell carcinomas had more common recurrences with respect to other tumors of the sinonasal tract (40 %). Interestingly, most of the Stage III and Stage IV diseases were of squamous cell histology involving surrounding structures.
Studies have investigated over time, various potential prognostic factors affecting local and distant recurrences. These maybe advanced stage of disease, non-surgical treatment, aggressive histologic type, and intracranial extension. In our study, histological status and positive neck nodes were found to be independent prognostic factors affecting recurrence.
Where the nodal status is concerned, there is low propensity of cervical lymph node involvement in malignant neoplasms of the sinonasal tract. Despite that studies have favored performing an elective neck dissection in locally advanced diseases or with an un-favored histology. The incidence of regional metastasis in the past has led to the conservative management of N0 necks [16]. On the contrary, Scurry et al. in their study supported the role of treating an N0 neck for squamous cell carcinomas. They stated the recurrence rate around 18.1 % [17].
In early tumors the nodal metastasis is rare. Presence of positive neck nodes in our study, proved to be an important factor related to recurrence of disease.
Local recurrence is the dominant failure and leading cause of mortality in patients with malignant neoplasms of the sino-nasal tract in almost all reported studies [18, 19]. Distant metastasis occurs in less than 2 % of all case [17, 19]. On the contrary, distant failure alone or with local recurrence is more frequent and consists of 8–20 % of all recurrent diseases [20].
The treatment plan is mainly surgical resection but the close proximity of these malignancies to vital structures (orbit or brain) complicates the decision and therefore difficult to manage recurrent or residual disease. These tumors remain quite challenging to manage and, therefore, a multidisciplinary approach cannot be over-emphasized. Loco-regional treatment requires radiation along with surgery [21– 23]. Also presence of an advanced T classification, bone or neural invasion, intracranial extension, dural or brain involvement, or positive margins require adjuvant radiation as part of a treatment modality [24]. Depending upon the histology and stage of disease, neoadjuvant or post-operative chemotherapy may be added [25, 26].
Conclusion
Sinonasal malignancies is a diverse group of cancers with a variation in its presentation, histology, local and distant spread and recurrence rates. Frequency of recurrences is more in squamous cell carcinomas with presence of positive neck nodes being an important prognostic factor.
Contributor Information
Maliha Kazi, Phone: +92-333-3009737, Email: maliha_kazi@hotmail.com.
Sohail Awan, Email: sohail.awan@aku.edu.
Montasir Junaid, Email: doc_montsj@yahoo.com.
Sadaf Qadeer, Email: sadaf.qadeer@aku.edu.
Nabeel Humayun Hassan, Email: nabeel.hassan@aku.edu.
References
- 1.Turner JH, Reh DD. Incidence and survival in patients with sinonasal cancer: a historical analysis of population-based data. Head Neck. 2012;34:877–885. doi: 10.1002/hed.21830. [DOI] [PubMed] [Google Scholar]
- 2.Blanch JL, Ruiz AM, Alos L, Coderch JT, Sprekelsen MB. Treatment Of 125 sinonasal tumors: prognostic factors, outcome, and follow-up. Otolaryngol Head Neck Surg. 2004;131:973–976. doi: 10.1016/j.otohns.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 3.AJCC Cancer Staging Manual. 6. New York: Springer; 2003. [Google Scholar]
- 4.Mattavelli CG, Pizzi N, Podrecca S, Valentini V. Malignant maxillary tumors involving the pterygo-maxillary and infratemporal fossae: a series of 65 patients and a comparison of the 1997 and 1977 UICC-AJCC staging systems. Acta Otorhinolaryngol Ital. 2000;20:100–105. [PubMed] [Google Scholar]
- 5.Parsons JT, Mendenhall WM, Mancuso AA, et al. Malignant tumors of the nasal cavity and ethmoid and sphenoid sinuses. Int J Radiot Oncol Biol Phys. 1998;14:11–22. doi: 10.1016/0360-3016(88)90044-2. [DOI] [PubMed] [Google Scholar]
- 6.Lango MN, Topham NS, Perlis CS, et al. Surgery in the multimodality treatment of sinonasal malignancies. Curr Probl Cancer. 2010;34:304–321. doi: 10.1016/j.currproblcancer.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Blanco AI, et al. Carcinoma of paranasal sinuses: long-term outcomes with radiotherapy. Int J Radiat Oncol Biol Phys. 2004;59:51–58. doi: 10.1016/j.ijrobp.2003.09.101. [DOI] [PubMed] [Google Scholar]
- 8.Pilch BZ, Bouquot J, Thompson LDR. Squamous cell carcinoma. In: Barnes L, Eveson JW, Reichart P, Sidransky D, editors. Pathology and genetics of head and neck tumours. (World Health Organization classification of tumours) Lyon: IARC Press; 2005. pp. 15–17. [Google Scholar]
- 9.Götte K, Hörmann K. Sinonasal malignancy: what’s new? ORL. 2004;66:85–97. doi: 10.1159/000077801. [DOI] [PubMed] [Google Scholar]
- 10.Khademi B, Moradi A, Hoseini S. Malignant neoplasms of the sinonasal tract: report of 71 patients and literature review and analysis. Oral Maxillofac Surg. 2009;13:191–199. doi: 10.1007/s10006-009-0170-8. [DOI] [PubMed] [Google Scholar]
- 11.Bhattacharyya N. Survival and staging characteristics for non-squamous cell malignancies of the maxillary sinus. Arch Otolaryngol Head Neck Surg. 2003;129:334–337. doi: 10.1001/archotol.129.3.334. [DOI] [PubMed] [Google Scholar]
- 12.Cabrerizo JRG, García AS, Gil JRM. Revision of carcinomas in paranasal sinus. Acta Otorrinolaringol Esp. 2007;58:266–275. doi: 10.1016/S0001-6519(07)74925-7. [DOI] [PubMed] [Google Scholar]
- 13.AJCC Cancer Staging Manual. 7. New York: Springer; 2010. [Google Scholar]
- 14.Bridger GP, Kwok B, Baldwin M, Williams JR, Smee RI. Craniofacial resection for paranasal sinus cancer. Head Neck. 2000;22:772–780. doi: 10.1002/1097-0347(200012)22:8<772::AID-HED5>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 15.Fornelli RA, Fedok FG, Wilson EP, Rodman SM. Squamous cell carcinoma of the anterior nasal cavity: a dual institution review. Otolaryngol Head Neck Surg. 2000;123:207–210. doi: 10.1067/mhn.2000.107450. [DOI] [PubMed] [Google Scholar]
- 16.Resto VA, Deschler DG. Sinonasal malignancies. Otolaryngol Clin North Am. 2004;37:473–487. doi: 10.1016/S0030-6665(03)00159-2. [DOI] [PubMed] [Google Scholar]
- 17.Scurry WC, Jr, Goldenberg D, Chee MY, Lengerich EJ, Liu Y, Fedok FG. Regional recurrence of squamous cell carcinoma of the nasal cavity: a systematic review and meta-analysis. Arch Otolaryngol Head Neck Surg. 2007;133:796–800. doi: 10.1001/archotol.133.8.796. [DOI] [PubMed] [Google Scholar]
- 18.Patel SG, Shah JP. TNM staging of cancers of the head and neck: striving for uniformity among diversity. CA Cancer J Clin. 2005;55:242–258. doi: 10.3322/canjclin.55.4.242. [DOI] [PubMed] [Google Scholar]
- 19.Cabrerizo JRG, OrusDotu C, Gili JRM, FabraLlopis JM, Vintro XL, Beltran DJJ. Epidemiologic analysis of 72 carcinomas of the nasal cavity and paranasal sinuses. Acta Otorrinolaringol Esp. 2006;57:359–363. doi: 10.1016/S0001-6519(06)78728-3. [DOI] [PubMed] [Google Scholar]
- 20.Guntinas-Lichius O, Kreppel MP, Stuetzer H, Semrau R, Eckel HE, Mueller RP. Single modality and multimodality treatment of nasal and paranasal sinuses cancer: a single institution experience of 229 patients. Eur J Surg Oncol. 2007;33:222–228. doi: 10.1016/j.ejso.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 21.Calderon-Garciduenas L, et al. Malignant neoplasms of the nasal cavity and paranasal sinuses: a series of 256 patients in Mexico City and Monterrey. Is air pollution the missing link? Otolaryngol Head Neck Surg. 2000;122:499–508. doi: 10.1067/mhn.2000.103080. [DOI] [PubMed] [Google Scholar]
- 22.Bristol IJ, et al. Postoperative radiotherapy for maxillary sinus cancer: long-term outcomes and toxicities of treatment. Int J Radiat Oncol Biol Phys. 2007;68:719–730. doi: 10.1016/j.ijrobp.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 23.Cantu G, et al. Lymph node metastases in malignant tumors of the paranasal sinuses: prognostic value and treatment. Arch Otolaryngol Head Neck Surg. 2008;134:170–177. doi: 10.1001/archoto.2007.30. [DOI] [PubMed] [Google Scholar]
- 24.Dulguerov P, Jacobsen M, Allal A, Lehman W, Calcaterra T. Nasal and paranasal sinus carcinoma: how can we continue to make progress? Curr Opin Otolaryngol Head Neck Surg. 2006;14:67–72. doi: 10.1097/01.moo.0000193177.62074.fd. [DOI] [PubMed] [Google Scholar]
- 25.Dulguerov P, Allal AS, Chen AM, et al. Carcinomas of the paranasal sinuses and nasal cavity treated with radiotherapy at a single institution over five decades: are we making improvement? Int J Radiat Oncol Biol Phys. 2007;69:141–147. doi: 10.1016/j.ijrobp.2007.02.031. [DOI] [PubMed] [Google Scholar]
- 26.Dirix P, et al. Malignancies of the nasal cavity and paranasal sinuses: long-term outcome with conventional or threedimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2007;69:1042–1050. doi: 10.1016/j.ijrobp.2007.04.044. [DOI] [PubMed] [Google Scholar]