Abstract
Soft tissue sarcomas of head and neck region, account for 4–15% of all soft tissue sarcomas and less than 1% of all neoplasms in this region. Leiomyosarcoma is malignant tumor of smooth muscle which accounts for only 4% of head and neck sarcomas. The tumor is commonly encountered as a slow growing, discrete firm, and non-ulcerated painless mass. The physical appearance of these tumors can be deceptively benign and can be mistaken for non-malignant conditions. An early diagnosis and aggressive initial treatment remains the mainstay of therapy for a good prognosis. We are presenting eight cases of primary leiomyosarcoma of head and neck region with review of literature and highlight the need for early prudent diagnosis and treatment.
Keywords: Head and neck soft tissue sarcoma, Leiomyosarcoma, Maxilla, Mandible, Larynx, Buccal mucosa
Introduction
Soft tissue sarcomas of the head and neck are rare tumors and account for less than 10% of all soft tissue sarcomas and less than 1% of all neoplasm of this region [1]. Leiomyosarcoma is the malignant smooth muscle tumor accounting for only 4% the head and neck sarcomas. Only 41 cases of leiomyosarcoma of the head and neck structures have been reported in English literature [2–4].
Zieler [5] is credited with the first report of leiomyosarcoma. Diss and Levy [6] reported case of leiomyosarcoma arising from old lupus vulgaris scars on the cheek. Geever is credited with the first report in the English literature, a 34-year-old man with leiomyosarcoma of the retromolar region [7]. In one of the largest series of head and neck sarcomas including 352 patients, Freedman et al. [8] reported only 4 (1.1%) cases of leiomyosarcoma located at the neck region. This article presents eight cases of leiomyosarcoma in head neck region and highlights the need for early prudent diagnosis and treatment, without which may lead to a very poor outcome.
Materials and Methods
During the period of 1996–2009 the Department of Otolaryngology and Head and Neck Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India have treated eight cases of Leiomyosarcomas of head and neck, records were analysed retrospectively. Slides were assessed in all cases for the following features: tumour depth, presence of circumscribed versus infiltrative tumour borders, mitotic counts per 10 high power fields (HPF; five sets counted), necrosis, nuclear pleomorphism, vascular invasion, and the presence and nature of inflammatory components and correlated with tumor grade which was assessed using the NCI system [9]. Immunohistochemistry was performed for smooth muscle actin, muscle-specific actin, desmin, cytokeratin, S-100 protein. Survival was assessed with Kaplan–Meier method.
Case Summary
Eight cases were seen and treated during the period between 1996 and 2009 in the Department of Otolaryngology and Head and Neck Surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India. Age of cases was ranging from 12 to 55 years. Male:Female was 3:1. Right:Left was 5:3. The duration of symptoms at time presentation was ranging from 4 to 7 months. Most common presenting symptom was painless swelling whereas epistaxis and hoarseness of voice was present in one case. Among eight cases of leiomyosarcoma two cases had tumor of parapharyngeal space, two cases of buccal mucosa, one case of maxilla, one case of larynx, one case of mandible and one case involving tongue. All cases underwent surgical excision after routine investigations, histopathological and radiological work up (Figs. 1, 2, 3). One case underwent chemotherapy, two cases had radiotherapy and two cases underwent both chemo and radiotherapy following surgery. Cisplatin in 4–5 cycles was used in all cases as chemotherapeutic agent. In histopathologic examination number of mitotic figures seen per 10 HPF was ranging from 1 to 30 (Fig. 4). In immunohistochemical study five tumors were positive for Muscle specific actin, four for Desmin and seven for Smooth muscle actin (Fig. 5). 1, 4 and 3 cases were falling in NCI grade I, II and III respectively. All cases were regularly followed up except one patient who lost follow up after surgical excision. The duration of follow up was ranging from 6 months to 5 years. Three patients had local recurrence and distant metastasis in lung died within 3 years of diagnosis. One patient underwent two revision surgeries for excision of recurrence on first occasion and recurrence on second occasion, patient is still under regular follow up for last 6 months and is free of tumor. Two patients were free of disease after 5 years of follow up, whereas one patient was free of recurrence for follow up of 16 months but later lost follow up.
Fig. 1.

Contrast computerized tomography, axial section showing heterogeneous mass in prestyloid compartment of left parapharyngeal space displacing vessels in posterolateral
Fig. 2.
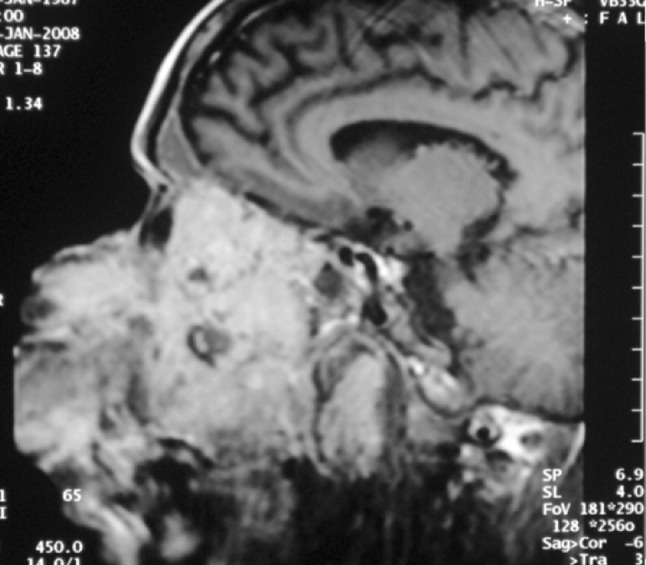
MRI showed homogenous soft tissue mass extending from subcutaneous tissue on left side of face to left infratemporal fossa, inferiorly oral cavity with destruction of hard palate and superiorly involving left orbit with destruction of medial and inferior wall with ill defined fat planes. It was hypointense on T1 and hyperintense on T2 and showed moderate contrast enhancement
Fig. 3.
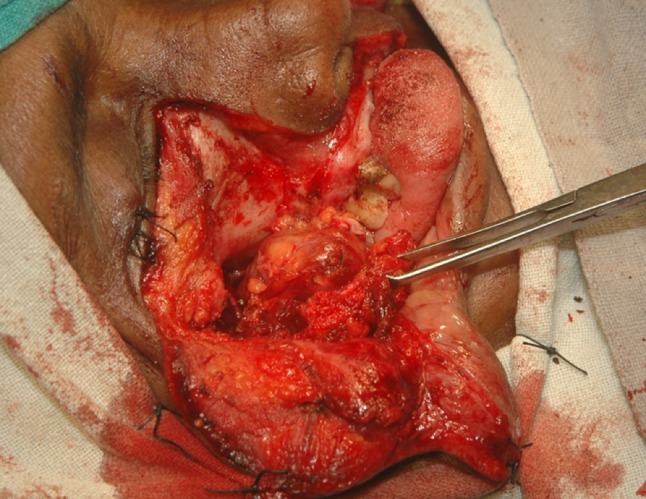
Intra operative photograph during third surgery for recurrence of tumor
Fig. 4.
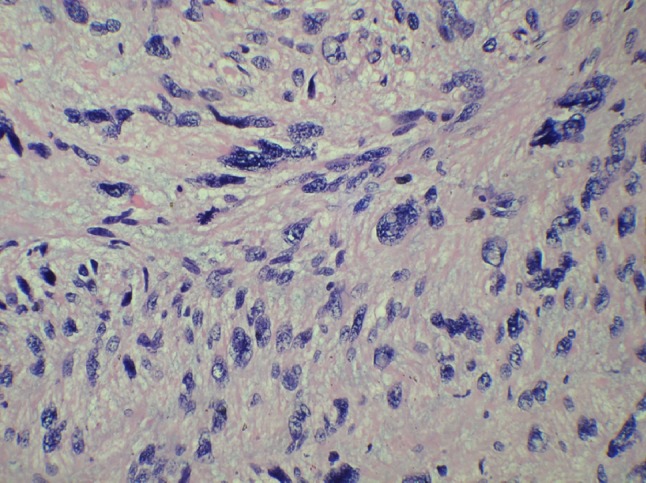
Spindle shaped tumor cell showing marked atypia and mitosis (H&E stain 40×)
Fig. 5.
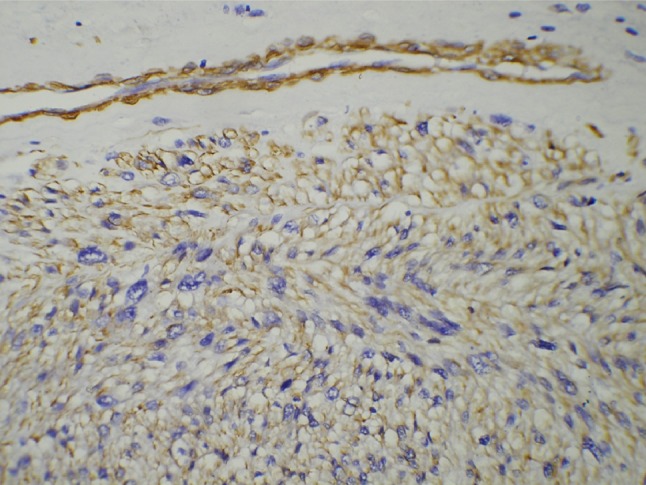
Immunohistochemical stain for SMA showing positivity in the tumor cells (20×)
Discussion
Leiomyosarcoma is the malignant smooth muscle tumor accounting for only 4% of the head and neck sarcomas. This reflects the paucity of smooth muscle found in this region. Smooth muscle is derived from primitive mesenchyme and is found mainly in blood vessels, erector pile musculature of skin, circumvallate papilla, primitive mesenchyme and myoepithelial cells of salivary glands. Aberrant mesenchymal differentiation and metastasis are the other possible modes of origin [10]. The majority of leiomyosarcoma of the head and neck arise in the oral cavity, superficial soft tissues like scalp, paranasal sinuses and jaws [11].
Out of total 41 cases reported, 28 patients were males and 13 were females. The average age was 45 years. Youngest reported case is a 1 year old and the oldest 88 years [12]. Higher incidence is supposed to occur among the middle age or elderly [13]. A bimodal tendency exists with 40% of cases recorded in patients 1–29 years old and 40% occurring in patients 51–67 years of age. Six cases occurred in children. The age of occurrence in our study group ranged from 12 to 55 years. The various sites involved were scalp/soft tissues (11); hypopharynx (3); nose (3); tongue (3); trachea (3); floor of mouth (3); gingiva (2); neck veins (2); and soft palate (2), maxilla (2), parapharyngeal space (2). Single case reports have also been identified in the lips, trachea, thyroid, external auditory canal, larynx, hard palate. The most common intraoral site is tongue [2].
Presenting signs and symptoms are nonspecific and usually referable to the location where they arise. Epistaxis, dysphagia, hoarseness, fever, stridor, and cough have been reported depending upon the site of the lesion. Pain and tenderness is rare in leiomyosarcoma whereas they are more prominent features of leiomyomas. Most commonly encountered is a slowly enlarging, discrete, firm, nonulcerated painless mass [2]. The lesion is submucosal or subcutaneous, reflecting its mesenchymal origin. Grossly, the lesions are smooth, firm and discretely circumscribed. Larger lesions may show focal areas of hemorrhage and necrosis. Based on a large review of leiomyosarcoma of the superficial soft tissues, the lesions of soft tissue origin 2.5 cm or larger are more likely malignant [14].
The differential diagnosis of this rare tumor may be problematic. The physical appearance can be deceptively benign and may be mistaken for non-malignant conditions [15]. Therefore, the diagnosis was supported by immunohistochemical and ultrastructural investigations. Histologically, the tumor is characterized by prominent interlacing bundles and fascicles of elongated “cigar-shaped” blunt-ended nuclei, prominent nucleoli and abundant eosinophilic cytoplasm spindle cells [16]. Tumors which exhibit one mitotic figure per five HPFs are considered malignant. Immunohistochemical identification of desmin, vimentin, actin and myoglobin are helpful in diagnosis [17]. Reticulin stains may be positive, depending on the degree of reticulin present. Desmin has variable results, with an inverse relationship to the vascularity of the tumor. Some leiomyosarcoma may express cytokeratin [18], the presence of which can confound accurate diagnosis. Electron microscopy will demonstrate intracytoplasmic microfilament bundles with numerous cytoplasmic dense bodies, micropinocytotic vesicles and a partly discontinuous basal lamina.
Thirty-four of the 41 reported cases in literature had localized disease. Only three patients had concomitant palpable neck nodes, suggesting a low incidence of lymphatic metastasis. One patient had metastatic disease at the time of presentation. The initial treatment in 80% of the 31 patients was wide local excision. Radical neck dissection was performed in the three patients with palpable disease. Surgical intervention combined with radiation therapy, chemotherapy or both was used in three patients. Nineteen patients survived without evidence of disease for 4 months to 12 years, an average of 48 months. All 19 patients who survived underwent initial wide local excision. Eight patients experienced local recurrence. Late regional lymph node metastasis developed in 10% of cases. Distant metastasis developed in seven patients (20%). The usual route of metastatic spread for leiomyosarcoma is theorized to be the bloodstream to the lungs. Five had pulmonary metastases, one patient developed subcutaneous infiltration and another had metastatic disease to the lumbar spine. Eight patients developed local recurrence. One patient received radiation therapy alone, and five underwent further surgical resection. Tumor recurred in three patients 3, 4 and 6 years after therapy, suggesting that patients deserve long-term follow-up. Recurrent disease was contained by surgical treatment in one-half of the patients where follow-up was available [2].
Comparing outcome with tumor grade in our series the patient with a grade 1 tumor was disease-free at 3 months. Amongst grade 2 tumors, one was alive with no evidence of disease since 3 years follow up, one had recurrence twice, two lost follow up and amongst grade 3 tumors, one alive with metastatic disease, and two (50%) died of disease.
Amongst head and neck soft tissue sarcoma, leiomyosarcoma has somewhat intermediate prognosis, 5 year survival rate has been reported to range between 61 and 100% [17], and few report to be 48 months. In our series only two patients were alive after follow up of 5 years. Prognosis appears to be related to the site and extent of the primary tumor. Lesions arising from the skin, nasal cavity, and larynx are associated with a better prognosis than lesions in other sites in the head and neck, probably because these sites are more amenable to complete surgical resection.
There are no randomized trials for treatment of head and neck soft tissue sarcomas. Surgical resection is the principal treatment method for the soft tissue sarcoma. Because adjacent pseudocapsule is commonly infiltrated by the tumor cells and satellite lesions are often found at some distance from the main lesion, the margin of the excision should be at least 1 cm in all directions [19]. Because of the proximity of adjacent neurovascular structures or vertebral column, en bloc resection and achieving these margins at all tumor planes is almost impossible in the head and neck region. Neck dissection is usually not essential because of rarity of metastatic lymph node.
The effectiveness of adjuvant radiation in soft tissue sarcomas of extremities has been clearly shown through three prospective randomized trials that have compared surgery alone with surgery and radiation [20–22]. Preoperative or postoperative choice of external-beam irradiation is still a question for soft tissue sarcomas since there is no supportive data. Some of the potential advantages of preoperative external-beam radiation therapy include decreased intraoperative seeding of tumor cells, and tumor shrinkage that might facilitate later surgery [22]. Cheng showed that preoperative radiation was superior to postoperative radiation in terms of local control for patients with tumors greater than 15 cm [23]. However, others have shown no difference [24]. Adjuvant radiotherapy was delivered to the base of the skull where the tumor was microscopically positive. Although recurrence was expected in this site due to poor radio-response rate of the leiomyosarcoma and positive surgical margins, relapse also occurred outside the radiation field where the surgical margins were negative. This evidence emphasizes the role of adjuvant radiotherapy in reducing the risk of recurrence in surgically treated head and neck leiomyosarcoma even without tumor positive margins. Due to this reason, radiation therapy may be necessary after surgery of head and neck sarcomas.
Soft tissue sarcomas of the head and neck are rare tumors. They tend to be intermediate or high grade and aggressive [24]. Considering all this it is vital that the clinician be familiar with this lesion, anticipate the possible presence of this disease and make a prudent diagnosis before the patient’s life is beyond survival as early diagnosis and aggressive initial management remains the mainstay of treatment. Further studies for early diagnosis and evaluation will improve the future management and survival of leiomyosarcoma in the head and neck.
Acknowledgments
Conflict of interest
There is no conflict of interest or financial disclosure to be made.
References
- 1.Eeles RA, et al. Head and neck sarcomas: prognostic factors and implications for treatment. Br J Cancer. 1993;68:201–207. doi: 10.1038/bjc.1993.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salzer AT. Leiomyosarcoma of head and neck. Houston: Baylor College of medicine; 1993. [Google Scholar]
- 3.Sharma R, et al. Oropharyngeal leiomyosarcoma. Ind J Otolaryngol Head Neck Surg. 2004;56(3):230–232. doi: 10.1007/BF02974360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akcam T, et al. Leiomyosarcoma of head and neck—report of two cases and review of literature. Auris Nasus Larynx. 2005;32:209–212. doi: 10.1016/j.anl.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Zieler G. Uberein malignes myome der haut. Virch Dtsch Pathol Ges. 1908;12:142. [Google Scholar]
- 6.Diss A, Levy G. Leiomyosarcome developpe sur ancien lupus tuberculeux la face. Bull Soc Dermatol Syphilol. 1924;31:108. [Google Scholar]
- 7.Geever EF, Ackerman LV, Dublin WB, Stout AP. Leiomyosarcoma of the buccal region. Cancer Semin. 1949;6:15. [Google Scholar]
- 8.Freedman AM, Reiman HM, Woods JE. Soft-tissue sarcomas of the head and neck. Am J Surg. 1989;158:367–372. doi: 10.1016/0002-9610(89)90135-9. [DOI] [PubMed] [Google Scholar]
- 9.Guillou L, Coindre JM, Bonichon F, et al. Comparative study of the National Cancer Institute and French Federation of Cancer Centers Sarcoma Group grading systems in a population of 410 adult patients with soft tissue sarcoma. J Clin Oncol. 1997;15:350–362. doi: 10.1200/JCO.1997.15.1.350. [DOI] [PubMed] [Google Scholar]
- 10.Chen JM, Novick WH, Logan CA. Leiomyosarcoma of the larynx. J Otolaryngol. 1991;20:345–348. [PubMed] [Google Scholar]
- 11.Marioni G, et al. Laryngeal leiomyosarcoma. J Laryngol Otol. 2000;114:398–401. doi: 10.1258/0022215001905698. [DOI] [PubMed] [Google Scholar]
- 12.Krishnan V, Miyaji C, Mainous E. Leiomyosarcoma of the mandible: case report. J Oral Maxillofac Surg. 1991;49:652–655. doi: 10.1016/0278-2391(91)90350-U. [DOI] [PubMed] [Google Scholar]
- 13.Neville BW (2009) Oral and maxillofacial pathology, 3rd edn. Saunders/Elsevier, St. Louis
- 14.Stout AP, Hill WT. Leiomyosarcoma of superficial soft tissues. Cancer. 1958;11:844–854. doi: 10.1002/1097-0142(195807/08)11:4<844::AID-CNCR2820110425>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 15.Valeriani M, et al. Recurrent cutaneous leiomyosarcoma. J Exp Clin Cancer Res. 1998;17:83–85. [PubMed] [Google Scholar]
- 16.Chae SW, et al. Leiomyosarcoma of the larynx. J Otolaryngol. 1999;28:293–295. [PubMed] [Google Scholar]
- 17.Snowden RT, Osborn FD, Wong FS, Sebelik ME. Ear Nose Throat J. 2001;80(7):449–453. [PubMed] [Google Scholar]
- 18.Miettinen M. Immunoreactivity for cytokeratin and epithelial membrane antigen in leiomyosarcoma. Arch Pathol Lab Med. 1988;112:637–640. [PubMed] [Google Scholar]
- 19.Eilber FR, Eckardt J. Surgical management of soft tissue sarcomas. Semin Oncol. 1997;24:526–533. [PubMed] [Google Scholar]
- 20.Pisters PW, et al. Long term results of a prospective randomized trial of adjuvant brachytherapy in soft tissue sarcoma. J Clin Oncol. 1996;14:859–868. doi: 10.1200/JCO.1996.14.3.859. [DOI] [PubMed] [Google Scholar]
- 21.Yang JC, et al. Randomized prospective study of the benefit of adjuvant radiation therapy in the treatment of soft tissue sarcomas of the extremity. J Clin Oncol. 1998;16:197–203. doi: 10.1200/JCO.1998.16.1.197. [DOI] [PubMed] [Google Scholar]
- 22.Suit HD, et al. Treatment of the patient with stage M0 soft tissue sarcoma. J Clin Oncol. 1988;6:854–862. doi: 10.1200/JCO.1988.6.5.854. [DOI] [PubMed] [Google Scholar]
- 23.Cheng E, Dusenbery K, Winters M, Thompson R. Soft tissue sarcomas: preoperative versus postoperative radiotherapy. J Surg Oncol. 1996;61:90–99. doi: 10.1002/(SICI)1096-9098(199602)61:2<90::AID-JSO2>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 24.Wanebo HJ, Koness RJ, MacFarlane JK, Eiber FR, Byers RM, Elias EG, et al. Head and neck sarcoma: report of the Head and Neck Sarcoma Registry. Society of Head and Neck Surgeons Committee on Research. Head Neck. 1992;14:1–7. doi: 10.1002/hed.2880140102. [DOI] [PubMed] [Google Scholar]


