Abstract
Cervical thymic cysts are rare lesions often misdiagnosed clinically as branchial cyst. Here we report a rare case of multiloculated thymic cyst in a young 8 year old male child on the left side of the neck. Histopathology of the excised cyst revealed mural nodules of thymic tissue with prominent Hassal’s corpuscles associated with multiloculated cyst. This case is presented here for its rarity. It should be included in the differential diagnosis of neck masses in children.
Keywords: Thymic cyst, Ectopic tissue, Thymus gland, Hassal’s corpuscle
Introduction
Thymus gland is derived mostly from the third pharyngeal pouch. During embryogenesis, the primordial thymic tissue descends down into the mediastinum, initially connected to the pharynx by hollow structures named thymopharyngeal ducts [1]. During its path of descent, remnants of thymic tissue may be left behind leading to the formation of a cyst. Cervical thymic cyst is rare [2] and mostly unilocular [3]. Thymic cysts account for 0.3% of pediatric congenital cervical cysts.
Case Report
An 8 year old male child presented with a swelling in the upper cervical region on the left side of neck for 6 months. The swelling was soft to cystic in consistency and was situated in the carotid triangle. It was fluctuant with diffuse borders and smooth external Surface. Clinically, the lesion was diagnosed as branchial cyst and FNAC report came as ‘Benign Retention Cyst’.
Ultrasound examination showed a cystic mass measuring 3.7 × 2.5 × 2.4 cm in its greatest dimension (Fig. 1).During surgical excision, it was found to be deep to the sternocleidomastoid and was in close relation with the carotid sheath. The excised specimen was a pale brown cystic mass; its cut surface displayed multiple locules between 0.3 × 1 cm diameters with pale brown serous fluid, separated by fine transparent pale septae with tiny greyish white nodules (Figs. 2, 3). On microscopic examination, the thymic tissue with lobules of lymphoid follicles with germinal centres and large keratinous to amorphous appearing Hassal’s corpuscles were present (Fig. 4).
Fig. 1.
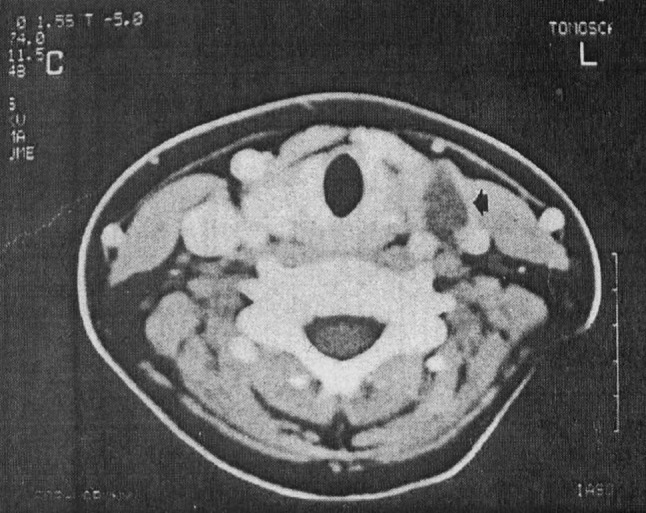
CT scan showing a mass in front of the left common carotid artery and Jugular Vein, medial to the Sternoclediomastoid muscle (arrow head)
Fig. 2.

Intra operative picture of thymic cyst
Fig. 3.

Cut section of the specimen showing brownish multilocutaed cyst with thin septae
Fig. 4.
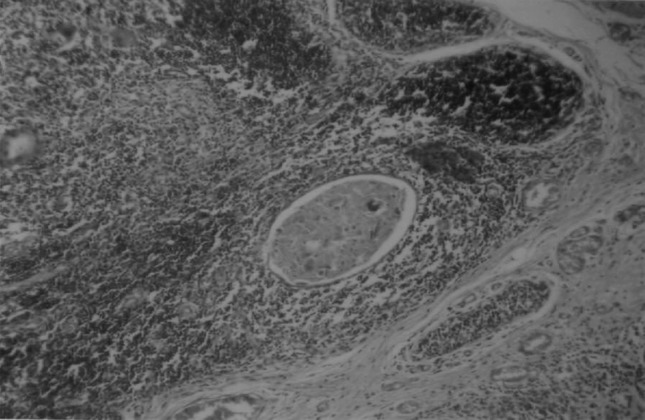
Microphotograph showing degenerating Hassal’s corpuscle within thymic lymphoid tissue
Discussion
Cervical thymic cysts are uncommon lesions found more on the left side of the neck with a slight male preponderance [4]. They manifest usually during the first decade of life, as a slow growing painless mass in the region between the angles of the mandible to sternum, in the vicinity of the carotid sheath, located along the path of descent of embryonic tissue [1].
Contrast enhanced CT scans can differentiate thymic cysts from other paediatric neck swellings such as branchial cleft cysts and lymphangiomas; [5] the second branchial cysts are located superficial and lateral to internal jugular vein and common carotid artery and lymphangiomas are found in the posterior triangle of the neck, while thymic cysts are situated in close association with the carotid sheath, between internal jugular vein and carotid vessels [6]. Also thymic cysts tend to be larger extending toward the anterosuperior mediastinum [7].
The cysts are mostly unilocular [4], but in our case it is multilocular. The cyst contents are clear, serous or brownish fluid. Microscopically it contains typical thymic tissue with large degenerating Hassal’s corpuscles and cysts lined by single or multilayered epithelium. The parathyroid gland may be found in the periphery of the cyst, indicative of the common embryonic origin from the third branchial pouch [8].
The origin of cervical thymic cysts has been attributed to two different theories. The unilocular cysts are thought to be due to the persistence of the thymopharyngeal duct while the multilocular cysts result from cystic degeneration of thymic Hassal’s corpuscles [4, 9].
Surgical removal is the treatment of choice. It is imperative that the existence of mediastinal thymus is confirmed before excision of the cervical thymic tissue, in order to prevent impairment of immune status in later life [10]. MRI and FNAC may be performed to confirm the presence of mediastinal thymus and in the absence of which surgical removal should be deferred [6]. Complications like recurrence, myasthenia gravis, and malignant transformations are rare.
References
- 1.Verbin RS, Barnes L. Cysts and cyst-like lesions of the oral cavity. Jaws and neck. Surgical pathology of the head and neck. 2. Switzerland: Marcel Dekker AG; 2001. [Google Scholar]
- 2.Nguyen Q, de Tar M, Wells W, Crockett D. Cervical thymic cyst: case reports and review of the literature. Laryngoscope. 1996;106:247–252. doi: 10.1097/00005537-199603000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Hsieh YY, Hsueh S, Hsueh C, Lin JN, Luo CC, Lai JY, et al. Pathological analysis of congenital cervical cysts in children: 20 years of experience at Chang Gung Memorial Hospital. Chang Gung Med J. 2003;26:107–113. [PubMed] [Google Scholar]
- 4.Georgios T, Dionisios L, Stamatia V, Georgios A, Georgios D, Tsikou-Papafragou A. Ectopic thymic cyst in neck. J Larygol Otol. 2000;114:318–320. doi: 10.1258/0022215001905472. [DOI] [PubMed] [Google Scholar]
- 5.Koeller KK, Alamo L, Adair CF, Smirniotopoulos JG. Congenital cystic masses of the neck: radiologic, pathologic correlation. Radiographics. 1999;19:121–146. doi: 10.1148/radiographics.19.1.g99ja06121. [DOI] [PubMed] [Google Scholar]
- 6.Kaufman MR, Smith S, Rothschild MA, Som P. Thymopharyngeal duct cyst. Arch Otolaryngol Head Neck Surg. 2001;127:1357–1360. doi: 10.1001/archotol.127.11.1357. [DOI] [PubMed] [Google Scholar]
- 7.Daga BV, Chaudhary VA, Dhamangaokar VB. Case report: CT diagnosis of thymic remnant cyst/thymopharyngeal duct cyst. Indian Radiol Imaging. 2009;19:293–295. doi: 10.4103/0971-3026.57211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yahya D, Abbas B, Perikala VK. Aberrant thymus and parathyroid gland presenting as a recurrent lateral neck mass: a case report. Ear Nose Throat J. 2006;85:452–453. [PubMed] [Google Scholar]
- 9.Cigliano B, Baltogiannis N, De Marco M, et al. Cervical thymic cysts. Pediatr Surg Int. 2007;12:1219–1225. doi: 10.1007/s00383-006-1822-5. [DOI] [PubMed] [Google Scholar]
- 10.Brearley S, Gentle TA, Baynham MI, Roberts KD, Abrams LD, Thompson RA. Immunodeficiency following neonatal thymectomy in man. Clin Exp Immunol. 1987;70:322–327. [PMC free article] [PubMed] [Google Scholar]


