Abstract
The objective of this study was to assess the versatility of pectoralis major myocutaneous (PMMC) flap in the reconstruction of diverse surgical defects following resection of various head and neck malignancies. We performed retrospective analysis of patients in whom PMMC was used to reconstruct head and neck surgical defects during May 2006 to December 2010. The study was carried out at KLES Dr. Prabhakar kore Hospital & M.R.C, Belgaum and involved 95 patients. The patients were grouped depending on the site of defect reconstructed and were analyzed in detail. Of the 95 patients, between the age group 38 and 62 years, 69 patients were males while 26 patients were females. PMMC was used to reconstruct 59 cases of oral mucosal defect, ten cases of skin defect and 18 cases of simultaneous oral mucosal and outer skin defect. PMMC was also used in two cases of laryngopharyngeal defects and six cases with floor of mouth and tongue defects. No failures were noted in the study during the follow up period. Despite worldwide emphasis on free flaps as gold standard in the reconstruction of tissue defects, institutions in developing countries where financial constraints are encountered or as salvage procedure for free flap failure, PMMC due to its versatility is still considered the workhorse for reconstruction of moderate to large sized head and neck defects.
Keywords: Pectoralis major, Flap, Reconstruction, Head and neck cancer
Introduction
Contemporary management of head and neck malignancy is a cumulative effort of new oncologic and reconstructive techniques. Since 1940, with the advent of newer techniques of radical surgery and in-continuity neck dissection, patient survival and functional rehabilitation have significantly improved [1]. The development of reconstructive techniques further revolutionized the success of head and neck surgery. Unfortunately it took over three decades for the concept of reconstruction to come into the picture. It was in the late 1970s and early 1980s that pedicled pectoralis major myocutaneous (PMMC) flap was popularized and became the predominant method used in the reconstruction of head and neck [1]. Since then several other regional flaps viz. latissimus dorsi, trapezius, sternomastoid, platysma have evolved but PMMC has stood the test of time and is still considered the workhorse [2] of head and neck reconstruction.
Reconstruction after ablative head and neck surgery often presents challenging complex 3-dimensional defects. These defects can have dramatic effect on the function and cosmesis which in turn may significantly impact the patient’s quality of life. Moreover with the aggressive protocols of today’s chemo and radiotherapy, the need to bring an oxygenated tissue with good blood supply to the surgical defect is of paramount importance. Ever since its introduction by Ariyan [3] in 1979, PMMC flap has become the most frequently used regional flap and has significantly improved the safety and functional outcome of head and neck surgery. The distinct advantage of PMMC lies in the fact that it is reliable, easy to harvest, can be raised in a short time, has minimal donor site morbidity, plenty of bulk, can be combined with other flaps such as free flap and can be used for single stage reconstruction of inner mucosal and/or outer skin defects in head and neck region and is within the realms of head and neck oncosurgeon.
In this article, we have described our 4 years experience using the PMMC flap in soft tissue head and neck reconstruction. We report the reliability and versatility of this flap, showing its high effectiveness in meeting our surgical needs.
Materials and Methods
We retrospectively reviewed 95 cases of soft tissue head and neck reconstruction with the PMMC flap. All operations were performed at our institution by the same surgeon from May 2006 to December 2010. Patients in whom the surgical defect was closed primarily or using other flaps were excluded from the study. Following the tumour excision, the exact size of the defect was noted and the appropriate sized PMMC flap was used to reconstruct the defect. The PMMC flap was harvested in the usual standard fashion. The patients were grouped separately depending on the site of defect reconstructed pertaining to the head and neck region. Follow-up ranged from 1 to 4 years. The site of the defect reconstructed, the size of the flap harvested and outcome were analyzed in detail.
Results
Of the 95 patients, between the age group 38 and 62 years, 69 patients were males while 26 patients were females. PMMC was used to reconstruct only the oral mucosal defect in 59 patients (Fig. 1), oral mucosa along with outer skin defect in 18 patients, skin defect only in 10 cases (Fig. 2), floor of mouth or tongue defects in six cases and in two cases of laryngopharyngeal defects (Fig. 3; Table 1). Skin paddle size ranged from 9 to 15 cm in length and from 6 to 12 cm in width. In all cases the chest was closed primarily. The overall flap survival rate was 100 %. The complications noted in the study were grouped under two headings namely complications noted at the donor site and those noted at the recipient site. The complications encountered at the recipient site were collection of serous fluid between flap and overlying skin in eight cases and flap edge necrosis in three cases. The only complication encountered at the donor site was suture line dehiscence in one case. All the complications were successfully managed conservatively (Table 2).
Fig. 1.

PMMC flap used for reconstruction of oral mucosal lining (published with the patient’s consent)
Fig. 2.

Clinical photograph showing the neck skin defect reconstructed with PMMC flap (published with the patient’s consent)
Fig. 3.
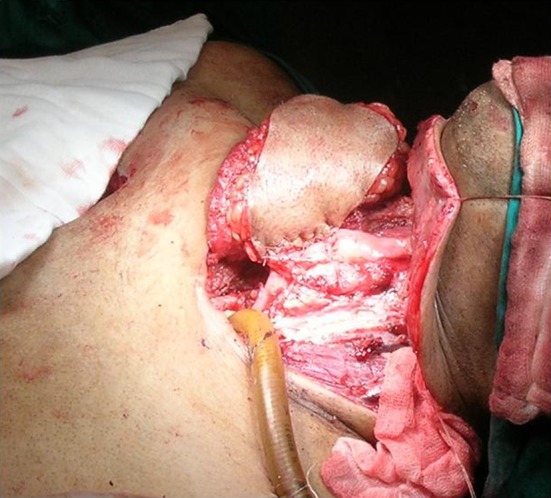
Intraoperative photograph showing PMMC being used for laryngopharyngeal reconstruction (published with the patient’s consent)
Table 1.
| Site of defect reconstructed | No. of cases | Percentage |
|---|---|---|
| Oral mucosa | 59 | 62 |
| Oral mucosa along with outer skin | 18 | 19 |
| Neck skin | 10 | 10 |
| Floor of mouth or tongue | 6 | 6 |
| Laryngopharynx | 2 | 2 |
| Total | 95 | 100 |
Table 2.
| Site of complication | Type of complication | No. of cases |
|---|---|---|
| Donor | Collection of serous fluid | 8 |
| Flap edge necrosis | 3 | |
| Recipient | Suture line dehiscence | 1 |
Discussion
The primary aim of head and neck cancer surgery is to provide a cure or significant palliation with a dire attempt to restore the patient to the pre-morbid level of functioning and quality of life with the best reconstruction possible [1]. One principle which needs to be kept in mind is that no reconstruction procedure at any cost should compromise on adequate tumor resection [1]. While an oncosurgeon plans for reconstruction less priority is usually given to the aesthetic rehabilitation but certain safety factors should be kept in mind. In this context it is essential to prevent life threatening complications like carotid blowout in patients planned for radiotherapy, improper healing due to less vascularity at the site of reconstruction or dysfunction of the organ that has undergone surgery.
Currently the options for all head and neck defect reconstruction can broadly be classified as [1]; primary closure, healing by secondary intention, skin graft, local flap, regional flap and free flap. Small defect with adequate lax tissue can be closed primarily. However larger defects need to be closed by skin graft, local, regional or free flap depending on the structure which requires to be reconstructed.
In about 90 % of the cases head and neck oncosurgeon would do away with pectoralis major or latissimus dorsi myocutaneous flap [4]. However recently the microvascular free flaps are considered the gold standard method for reconstruction of major defect following head and neck cancer surgery [5]. The advantages of free flaps are that they can reconstruct larger head and neck three-dimensional defects with limited donor site morbidity and complications. Further it gives a better functional and aesthetic outcome as compared to regional pedicled flaps. However, free flaps require specialized surgical skills, special and costly instruments and rigorous postoperative monitoring. These factors are usually not available in most head and neck centers especially in the developing countries. Also the fact that it is an expensive procedure adds to the problem.
The PMMC flap has been considered a remarkable step in the history of head and neck reconstruction since its description by Ariyan’s in 1979. The unique anatomy [6, 7] of the pectoralis major muscle makes it the most preferred muscle for head and neck reconstruction. The advantages [6, 8, 9] of PMMC which still make it the preferred choice even today are that the vascular supply of this muscle is very constant and it is covered by small amount of soft tissue and is situated clearly along definite tissue planes making its isolation relatively easy. The pectoralis muscle is well vascularized and has abundant perforators to supply the overlying skin hence it can survive under suboptimal conditions even when transferred to an infected bed. PMMC is a very reliable flap with failure rate of less than 1% and is in close proximity to the head and neck region. The flap can provide a large bulk of well vascularized tissue to cover skin and/or mucosal defects of neck and midface up to the level of tragus. In addition, the low morbidity to the donor site, execution as a single stage procedure without changing the patient’s position has resulted in the broad acceptance of this flap by head and neck reconstructive surgeons. The PMMC flap can also be performed in association with other flaps like the free flaps, deltopectoral and contralateral PMMC flap usually to offer a soft tissue component to a large reconstruction, to protect major vessels namely the carotid artery at risk of radiation induced blow out. Also it can be used as a salvage procedure after the necrosis of microvascularized flaps and in cases where contraindication to free flaps exists, such as medical conditions that make the patient unable to withstand long surgical procedure or inadequate recipient vessels in the neck of patients who previously underwent high-dose radiotherapy. Further advantages of PMMC are that it is easy to elevate and its arc of rotation is adequate for most oropharyngeal and facial defects.
However there are several disadvantages [8, 9]. It reduces the vital capacity of the lung postoperatively and donor site defect can be cosmetically unacceptable as there is distortion of symmetry especially in female patients. The flap can be too bulky at times for the proposed reconstruction especially when used as the bipedal flap (Fig. 4). Moreover it cannot be used for defects above the level of external auditory canal and beyond the contralateral anterior axillary line as it is limited by its arc of rotation. The defect at the donor site can lead to impairment of shoulder function occasionally and in males, hirsute chest skin placed intra-orally can be bothersome and the distal skin on the flap is not considered to be reliable. The PMMC flap is relatively immobile and occasionally the flap can dangerously conceal recurrences, making follow-up difficult.
Fig. 4.

Clinical photograph showing the outer skin paddle of bipedal PMMC flap. (published with the patient’s consent)
PMMC can be used for reconstruction [8–10] of various defects in the head and neck region such as intra-oral mucosal lining defects, full thickness defect of oral cavity that is mucosal lining with outside skin defects of cheek, tongue and floor of mouth defects. PMMC can be used for reconstruction following neck dissection involving the excision of skin over the neck for covering carotid vessel to prevent carotid blowout in patients who are post-radiotherapy or patients planned for radiotherapy. There is substantial evidence in the literature especially by Gardiner et al., Coleman, Prince et al., Goldstein et al. and Joesp et al., where PMMC has been used for secondary coverage of necrotic neck wound [11–13]. Leemans et al. [14] in 1995 have reported the use of pectoralis major myofascial flap with split thickness skin graft for carotid exposure or imminent wound breakdown with better results. PMMC can also be used for reconstruction of skin and soft tissue defect over lower part of face and for reconstruction of laryngopharyngeal or esophageal defects. In patients undergoing total laryngectomy following post-radiation failure only the pectoralis major muscle flap can be used to cover the laryngopharyngeal closure so as to prevent salivary leak. Su et al. [15] have described the successful use of PMMC for near-total laryngopharyngectomy for advanced carcinoma hypopharynx. Sopriano [16] in 2002 and later Jegoux et al.[17] in 2007 reported the use of “U” or “horseshoe shaped” PMMC flap for hypopharyngeal reconstruction. Zou et al. [18] have also reported the successful use of PMMC for salvage reconstruction of extensive recurrent oral cancer. Parker et al. [19] reported significant functional improvement with PMMC reconstruction for oral and oropharyngeal resection.
The pectoralis major myocutaneous flap over a period of time has undergone several modifications. One variant is the bipedal flap especially useful for full thickness defect of cheek [20] but complication rates are slightly higher [21] as compared to the single paddled flap. Other modified [6] forms are costomyocutaneous flap, osteomyocutaneous flap, pedicled pectoralis flap under the clavicle, reverse/turnover flap, sensory flap and multiple skin island flap. These modifications have further enhanced the versatility of PMMC.
Conclusion
The current emphasis in tissue replacement has shifted to microvascular free-tissue transfer. However the pectoralis major myocutaneous flap is still an acceptable alternative as it is economical, has reliable vascular supply, especially where bulk is needed and can be done by the primary surgeon himself without any special instrumentation. Most importantly the versatility of the flap makes it suitable for the reconstruction of various types of head and neck defects. Hence it continues to be one of the most widely used flaps in head and neck reconstruction. Thus we conclude that in institutions of developing countries where financial constraints are encountered or as salvage procedure for free flap failure, the PMMC flap still remains a valuable resource in the armamentarium of reconstructive head and neck surgery.
Conflict of interest
None.
References
- 1.Sloan SH, Blackwell KE, Harris JR, Genden EM, Urken ML. Reconstruction of major defects in the head and neck following cancer surgery. In: Myers EN, editor. Cancer of the head and neck. Amsterdam: Elsevier; 2003. [Google Scholar]
- 2.Magee WP, McCaw JB, Horton CE. Pectoralis ‘paddle’ myocutaneous flaps: the workhorse of head and neck reconstruction. Am J Surg. 1980;140:507–513. doi: 10.1016/0002-9610(80)90201-9. [DOI] [PubMed] [Google Scholar]
- 3.Aryan S. The pectoralis major myocutaneous flap. Plast Reconstr Surg. 1979;63:73–78. doi: 10.1097/00006534-197901000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Watkinson JC, Gaze MN, Wilson JA (2000) Reconstruction. Stell and Maran’s head and neck surgery. In: Watkinson JC (ed) Hodder Arnold, London
- 5.Schusterman MA, Miller MJ, Reece GP, Kroll SS, Marchi M, Goepfert H. A single center’s experience with 308 free flaps for repair of head and neck cancer defects. Plast Reconstr Surg. 1994;93:472–478. [PubMed] [Google Scholar]
- 6.Wei WI, Chan YW. Pectoralis major flap. In: Wei FC, Mardini S, editors. Flaps and reconstructive surgeries. Amsterdam: Elsevier; 2009. [Google Scholar]
- 7.Manders EK. Regional pedicle flap. In: Myers EN, editor. Operative otolaryngology head and neck surgery. Amsterdam: Elsevier; 2008. [Google Scholar]
- 8.Vartanian JG, Carvalho AL, Carvlho SM, Mizobe L, Magrin J, Kowalski LP. Pectoralis major and other myofascial/myocutaneous flaps in head and neck cancer reconstruction: experience with 437 cases at a single institution. Head Neck. 2004;26:1018–1023. doi: 10.1002/hed.20101. [DOI] [PubMed] [Google Scholar]
- 9.Milenovic A, Virag M, Uglesic V, Aljinovic-Ratkovic N. The pectoralis major flap in head and neck reconstruction: first 500 patients. J Craniomaxillofac Surg. 2006;34:340–343. doi: 10.1016/j.jcms.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Baek SM, Lawson W, Biller HF (1982) An analysis of 133 pectoralis major myocutaneous flaps. Plast Reconstr Surg 69:460–469 [DOI] [PubMed]
- 11.Gardiner LJ, Ariyan S, Pillsbury HC. Myocutaneous flaps for challenging problems in head and neck reconstruction. Arch of Otolaryngol Head Neck Surg. 1983;109:396–399. doi: 10.1001/archotol.1983.00800200042011. [DOI] [PubMed] [Google Scholar]
- 12.Coleman JJ. Treatment of the ruptured or exposed carotid artery. South Med J. 1985;78:262–267. doi: 10.1097/00007611-198503000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Price JC, Davis RK, Koltai PJ. The pectoralis major myocutaneous flap for salvage of necrotic wounds. Laryngoscope. 1985;95:146–150. doi: 10.1288/00005537-198502000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Leemans CR, Balm AJ, Gregor RT, Hilgers FJ. Management of carotid artery exposure with pectoralis major myofascial flap transfer and split-thickness skin coverage. J Laryngol Otol. 1995;109:1176–1180. doi: 10.1017/S0022215100132360. [DOI] [PubMed] [Google Scholar]
- 15.Su CY, Hwang CF. Near-total laryngopharyngectomy with pectoralis major myocutaneous flap in advanced pyriform carcinoma. J Laryngol Otol. 1993;107:817–820. doi: 10.1017/S0022215100124508. [DOI] [PubMed] [Google Scholar]
- 16.Spriano G, Pellini R, Roselli R. Pectoralis major myocutaneous flap for hypopharyngeal reconstruction. Plast Reconstr Surg. 2002;110:1408–1416. doi: 10.1097/00006534-200211000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Jegoux F, Ferron C, Malard O, Espitalier F, Beauvillain de montreuil C (2007) Reconstruction of circumferential pharyngolaryngectomy using a ‘horseshoe-shaped’ pectoralis major myocutaneous flap. J Laryngol Otol 121:483–488 [DOI] [PubMed]
- 18.Zou H, Zhang WF, Han QB, Zhao YF. Reconstruction of extensive recurrent oral cancer defects with the pectoralis major myocutaneous flap. J Oral Maxillofac Surg. 2007;65:1935–1939. doi: 10.1016/j.joms.2006.10.067. [DOI] [PubMed] [Google Scholar]
- 19.Parker DA, Woodhead J, Das Gupta AR. Pectoralis major flaps: functional aspects of the repair of oral and oropharyngeal resections. J Laryngol Otol. 1988;102:509–512. doi: 10.1017/S0022215100105493. [DOI] [PubMed] [Google Scholar]
- 20.Ahmad QG, Navadgi S, Agarwal R, Kanhere H, Shetty KP, Prasad R. Bipaddle pectoralis major myocutaneous flap in reconstructing full thickness defects of cheek a review of 47 cases. J Plast Reconstr Aesthet Surg. 2006;59:166–173. doi: 10.1016/j.bjps.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 21.Chaturvedi P, Pai PS, Pathak KA, Chaukar DA, Deshpande MS, D’cruz AK. Simultaneous reconstruction of large skin and mucosal defect following head and neck surgery with a single skin paddle pectoralis major myocutaneous flap. J Laryngol Otol. 2005;119:303–305. doi: 10.1258/0022215054020511. [DOI] [PubMed] [Google Scholar]


