Abstract
Background:
Tuberculosis (TB) is one of the main causes of morbidity and mortality in different societies. Understanding factors leading to death following diagnosis of TB is important to predict prognosis in TB patients. The aim of this study was to identify common risk factors associated with death in patients with an in-hospital diagnosis of TB, in a city in Iran with the highest prevalence and incidence of TB in the country.
Materials and Methods:
A retrospective study was conducted at a university-affiliated hospital, Zahedan, in the south-east of Iran, which is a referral center for TB. To identify factors leading to death, medical records of 715 patients ≥15 years old with pulmonary TB from February 2002 to February 2011 have been evaluated. Registered factors included smoking, human immune deficiency virus (HIV) infection, using drugs, lung cancer, drug hepatitis following anti-TB medications, diabetes mellitus, previous TB treatment, anemia; and results of sputum smears. Univariate comparison and multiple logistic regression were performed to identify factors associated with mortality in TB patients.
Results:
Among 715 registered TB patients, 375 (52.5%) patients were male; among those, 334 (53%) were in the alive group and 41 (54%) in the death group. Seventy-five (10.5%) of the total number of TB patients died during TB treatment. The multivariate model showed that anemia (AOR: 19.8, 95% CI: 5.6-35.5), positive sputum smear (AOR: 13.4, 95% CI: 6.8-33.6), smoking (AOR: 12.9, 95% CI: 3.9-27.3), drug hepatitis (AOR: 12.3, 95% CI: 6.7-24.7), diabetes mellitus (AOR: 9.7, 95% CI: 2.9-32.0), drug use (AOR: 7.8, 95% CI: 2.4-25.5), and history of previous TB (AOR: 6.8, 95% CI: 2.2-21.3) were major risk factors for death in TB patients.
Conclusion:
Monitoring co-morbid conditions like diabetes mellitus and anemia are important to reduce death rate in TB patients. Preventive measures for smoking and drug addiction also play an important role to decrease mortality. Follow-up of patients with previous TB treatment is recommended.
Keywords: Tuberculosis, mortality, risk factors
INTRODUCTION
Tuberculosis (TB) is one of the main causes of morbidity and mortality in different societies. In 2010, an estimated 12.0 million people were living with active TB, including 8.8 million new cases, and there were an estimated 1.4 million TB deaths.[1] Identifying risk factors for death following diagnosis of TB is important to predict prognosis in TB patients and planning effective interventions to reduce death rates. Population-based studies have identified a number of risk factors including age, male gender, HIV co-infection, drug resistance, disease severity as factors associated with mortality following a diagnosis of TB.[2,3,4,5,6] A clinical trial during a period of 3 years in the United States and Canada revealed that 6.6% of TB patients died during therapy or follow-up. Those who died were more likely to have malignancy (Adjusted Odds Ratio = AOR 5.3), to be HIV-infected (AOR 3.9), and to be unemployed (AOR 2.0).[7]
Sistan-Balouchestan, the largest province of Iran, is situated in the south-east of Iran and ranks the first among all provinces of the country for TB. The incidence of TB in Iran was estimated 13.7 per 100000 population, but in Zahedan, the center of this big province was 36.6 per 100000 population in the year 2009.[8] Bordering with Afghanistan and Pakistan, which have high incidence and prevalence of TB, makes this part of Iran very critical for this disease as a result of transborder migration.
Therefore, TB is a major public health problem in South-Eastern Iran. However, there is no information on the risk factors associated with death in TB patients in this community. The purpose of this study was to determine common risk factors associated with death in patients with an in-hospital diagnosis of TB.
MATERIALS AND METHODS
Study population and data collection
The study was a retrospective study conducted at a university-affiliated hospital (Boo-Ali Hospital, Zahedan, South-Eastern Iran), which is referral for TB. We analyzed the medical records of 715 patients ≥15 years old with pulmonary TB during a period of 9 years (February 2002 to February 2011). For our study, TB diagnosis was classified as follows: 1-bacteriologically confirmed (smear and/or culture-positive) and 2- bacteriologically not confirmed (smear and/or culture negative). The diagnosis in the latter was made by the combination of clinical manifestations, results of chest X-ray, and the decision by an infectious diseases specialist to start TB treatment.
Registered factors included smoking (more than 10 cigarettes/day), human immune deficiency virus (HIV) infection, using drugs (opium is the most common drug used in this part of Iran), lung cancer, drug hepatitis following anti-TB medications, diabetes mellitus, previous TB treatment, anemia, and results of sputum smears. Hepatitis during anti-tuberculous treatment was defined as an increase in serum transaminase level of >3 times the upper limit of normal (ULN) with symptoms, or an increase in serum transaminase level of >5 times ULN without symptoms.[9] Patients with diabetes mellitus were categorized as registering two fasting blood sugar more than 126 mg/dl, and anemia was defined as hemoglobulin level below 10 g/dl. Human immuno-deficiency virus (HIV) infection was not prevalent in this part of Iran,[8] so HIV tests have been performed just in TB patients with risk factors for the disease. Therefore, 271 (38%) of patients who had risk factors for HIV infection were tested for this disease.
Statistical analysis
The χ2 test or Fisher's exact test have been performed to compare categorical variables, and Student's t-test has been performed to compare age as a continuous variable. All analyzes have been performed using SPSS version 17.0, and results with P < 0.05 have been considered statistically significant. To identify the risk factors associated with mortality, we compared variables between TB patients who died and those who survived through univariate analysis. Afterward variables with P < 0.05 have been entered into multilogistic regression analysis with the forward elimination method, and adjusted odds ratio (AOR) and 95% confidence interval (CI) were determined for them. The Ethics Committees of the Zahedan University of Medical Sciences in Iran approved the study protocol.
RESULTS
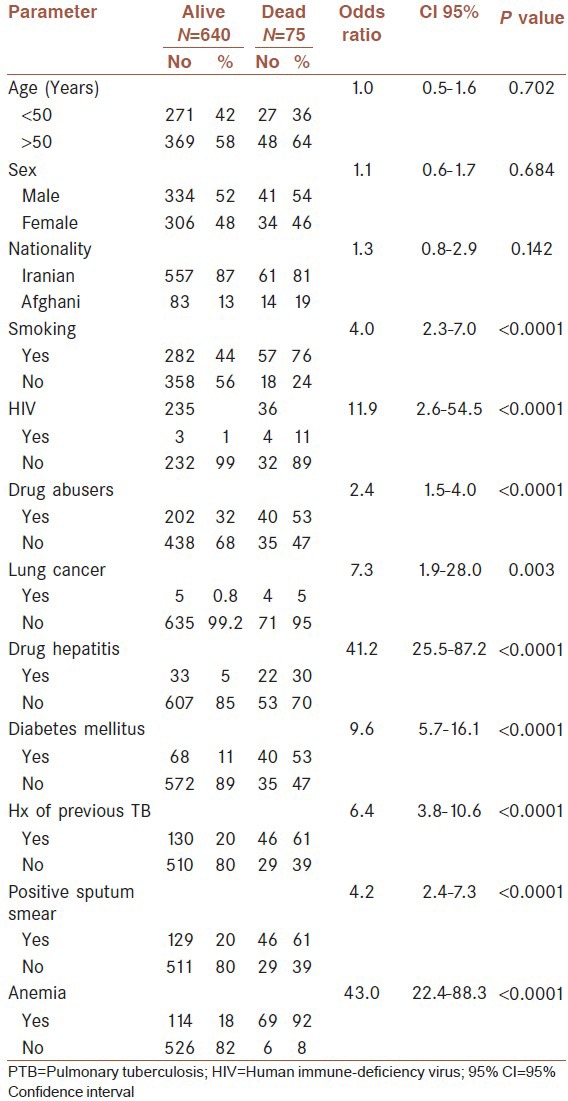
A total of 715 TB patients were registered at Boo-Ali Hospital, a referral center for TB patients, during February 2002 to February 2011. Three hundred and seventy-five (52.5%) patients were male, and among those, 334 (53%) were in the alive group and 41 (54%) in the death group. The male mean age ± standard deviation was 53.6 ± 18.5 years (15-98 years old) for the alive group and 58.2 ± 14.3 years (range 15-87 years old) for the death group. Seventy-five (10.5%) of the total number of TB patients died during TB treatment. The baseline demographics and common risk factors in both alive and dead individuals are shown in Table 1. In bivariate analysis, mortality was independently associated with anemia (OR: 43.0, 95% CI: 22.4-88.3, P < 0.0001), drug hepatitis (OR: 41.2, 95% CI: 25.5-87.2, P < 0.0001), HIV co-infection (OR: 11.9, 95% CI: 2.6-54.5, P < 0.0001), diabetes mellitus (OR: 9.6, 95% CI: 5.7-16.1, P < 0.0001), lung cancer (OR: 7.3, 95% CI: 1.9-28.0, P = 0.003), previous TB treatment (OR: 6.4, 95% CI: 3.8-10.6, P < 0.0001), positive sputum smear (OR: 4.2, 95% CI: 2.4-7.3, P < 0.0001), tobacco smoking (OR: 4.0, 95% CI: 2.3-7.0, P < 0.0001), and drug use (OR: 2.4, 95% CI: 1.5-4.0, P <=0.0001).
Table 1.
Characteristics of demographic and risk factors in pulmonary tuberculosis patients who died and those who survived during TB treatment
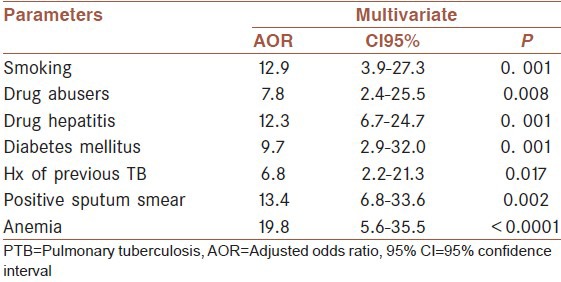
The multivariate model showed that anemia (AOR: 19.8, 95% CI: 5.6-35.5), positive sputum smear (AOR: 13.4, 95% CI: 6.8-33.6); smoking (AOR: 12.9, 95% CI: 3.9-27.3), drug hepatitis (AOR: 12.3, 95% CI: 6.7-24.7), diabetes mellitus (AOR: 9.7, 95% CI: 2.9-32.0), drug use (AOR: 7.8, 95% CI: 2.4-25.5), and history of previous TB (AOR: 6.8, 95% CI: 2.2-21.3) were major risk factors for death in TB patients [Table 2].
Table 2.
Comparison of risk factors in PTB patients who died and those who survived by multivariate analysis
DISCUSSION
Smoking, hepatitis following anti-TB treatment, diabetes mellitus, previous TB treatment, anemia, and drug abuse were predictors of TB mortality in the South-Eastern Iran. Such findings suggest that it is important for TB programs to identify high-risk groups for TB-associated decease and finally develop relevant interventions for improvement of treatment outcome.
Studies evaluating risk factors for death following diagnosis of TB have focused on specific groups including patients co-infected with HIV, prisoners, migrants, and patients with TB forms resistant.[10,11,12,13,14,15]
A systematic review of risk factors for death in adults during and after TB treatment revealed that risk factors for death in settings with high TB incidence were co-infection with HIV, advanced immuno-compromised patients, smear-negative TB, and malnutrition, but in regions of low TB incidence and HIV prevalence, risk factors included non-infectious co-morbidities, sputum smear-positive TB, and alcohol and substance misuse.[2]
In two separate studies in Singapore and Thailand, older age, male sex, Malay and Thai ethnicity were significant risk factors for death in TB patients.[13,14] A population-based study in Washington State also revealed that mortality was independently associated with increasing age, male gender, HIV co-infection, and U.S. birth.[3] Other significant risk factors associated with death in TB patients were bacteriologically confirmed forms, drug resistance, and residence in long-term care facilities.[13]
Previous TB treatment and multiple drug-resistant TB (MDR-TB) are considered significant risk factors for decease. There are reports supporting the idea that failure or relapses were not associated with an increased risk of death.[7,16] In a 13-year experience in China, survival of patients with highly extensive resistance (XDR) TB was shorter for HIV-infected patients and Beijing family strains.[17] Another study in a TB referral hospital in South Korea showed that there was high mortality in non-HIV infected patients with XDR-TB.[16]
According to another survey, age groups of 40 to 60 years and above 60 years were identified as significant risk factors for death. Other independent risk factors associated with poor treatment outcomes in MDR-TB patients were being a migrant, smear-positivity at treatment onset, and not receiving 3 or more potentially effective drugs with hazard ratio (HR) of 1.77, 1.94, and 3.87, respectively.[18] However, independent risk factors associated with poor treatment outcomes in XDR-TB patients were smear-positivity at treatment onset with an HR of 10.42 and not receiving 3 or more potentially effective drugs with HR of 14.90.[7] Therefore, proper treatment with adequate anti-TB drugs are recommended. Other risk factors that prolonged hospital stay and death in TB patients were co-morbid medical conditions like chronic obstructive pulmonary disease, hypertension, and adverse reactions from using anti-tuberculosis drugs.[17,19]
Our study was done retrospectively to find out the common risk factors associated with mortality that was considered one of the limitations of the survey. The data have been extracted from medical records of patients who have been already visited and registered at the hospital, so it may be subjected to selection bias. The other limitation of the survey was the fact that in many TB patients, multiple causes of death may act simultaneously, so the specific cause of death may not be determined accurately. However, we drew several conclusions from this study. First, death due to TB may be attributable to co-morbid conditions like anemia and diabetes mellitus. Therefore, monitoring fasting blood sugar and hemoglobulin in TB patients are necessary to control those co-morbid conditions. Death rate among TB patients is highest in tobacco smokers and drug abusers, so instructive methods may reduce future mortality in those specific populations. Monitoring adverse effects like hepatotoxicity secondary to anti-tuberculosis treatment is also another preventive measure to reduce mortality in TB patients. Previous history of TB and retreatment may suggest resistance to anti-TB medications leading to higher death rate in that population.
ACKNOWLEDGMENTS
The authors thank Zahedan Deputy of Research Affairs for funding this project. We also thank all staff at Boo-Ali Hospital for their help during the study period, especially, S Mirfakhrai and B Pour-Afghan for technical support. This article was extracted from the thesis by AAD (registered number 1248) at Zahedan University of Medical Sciences.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.The U.S. Government and Global Tuberculosis Fact sheet. US Global Health Policy. 2012. [Last accessed on 2012 Dec 21]. Available from: http://www.kff.org/globalhealth/upload/7883-05.pdf .
- 2.Waitt CJ, Squire SB. A systematic review of risk factors for death in adults during and after tuberculosis treatment. Int J Tuberc Lung Dis. 2011;15:871–85. doi: 10.5588/ijtld.10.0352. [DOI] [PubMed] [Google Scholar]
- 3.Horne DJ, Hubbard R, Narita M, Exarchos A, Park DR, Goss CH. Factors associated with mortality in patients with Tuberculosis. BMC Infect Dis. 2010. [Last accessed on 2012 May 25]. pp. 10–258. Available from: http://www.biomedcentral.com/1471-2334/10/258 . [DOI] [PMC free article] [PubMed]
- 4.Khan K, Campbell A, Wallington T, Gardam M. The impact of physician training and experience on the survival of patients with active tuberculosis. CMAJ. 2006;175:749–53. doi: 10.1503/cmaj.060124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pablos-Mendez A, Sterling TR, Frieden TR. The relationship between delayed or incomplete treatment and all-cause mortality in patients with tuberculosis. JAMA. 1996;276:1223–8. doi: 10.1001/jama.1996.03540150025026. [DOI] [PubMed] [Google Scholar]
- 6.Anyama N, Bracebridge S, Black C, Niggebrugge A, Griffin SJ. What happens to people diagnosed with tuberculosis? A population-based cohort. Epidemiol Infect. 2007;135:1069–76. doi: 10.1017/S0950268807007996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sterling TR, Zhao Z, Khan A, Chaisson RE, Schluger N, Mangura B, et al. Mortality in a large tuberculosis treatment trial: Modifiable and non-modifiable risk factors. Int J Tuberc Lung Dis. 2006;10:542–9. [PubMed] [Google Scholar]
- 8.Regional Health Center, Zahedan University of Medical Sciences. Iran: CDC; 2009. CDC. Reported tuberculosis in Sistan and Baluchestan. [Google Scholar]
- 9.Wang JY, Liu CH, Hu FC, Chang HC, Liu JL, Chen JM, et al. Risk factors of hepatitis during anti-tuberculous treatment and implications of hepatitis virus load. J Infect. 2011;62:448–55. doi: 10.1016/j.jinf.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Marks SM, Magee E, Robison V. Patients diagnosed with tuberculosis at death or who died during therapy: Association with the human immunodeficiency virus. Int J Tuberc Lung Dis. 2011;15:465–70. doi: 10.5588/ijtld.10.0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balabanova Y, Nikolayevskyy V, Ignatyeva O, Kontsevaya I, Rutterford CM, Shakhmistova A, et al. Survival of civilian and prisoner drug-sensitive, multi- and extensive drug- resistant tuberculosis cohorts prospectively followed in Russia. PLoS One. 2011;6:e20531. doi: 10.1371/journal.pone.0020531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tafuri S, Martinelli D, Melpignano L, de Palma M, Quarto M, Prato R, et al. Tuberculosis screening in migrant reception centers: Results of a 2009 Italian survey. Am J Infect Control. 2011;39:495–9. doi: 10.1016/j.ajic.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 13.Low S, Ang LW, Cutter J, James L, Chee CB, Wang YT, et al. Mortality among tuberculosis patients on treatment in Singapore. Int J Tuberc Lung Dis. 2009;13:328–34. [PubMed] [Google Scholar]
- 14.Amnuaiphon W, Anuwatnonthakate A, Nuyongphak P, Sinthuwatanawibool C, Rujiwongsakorn S, Nakara P, et al. Factors associated with death among HIV-uninfected TB patients in Thailand, 2004-2006. Trop Med Int Health. 2009;14:1338–46. doi: 10.1111/j.1365-3156.2009.02376.x. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen LT, Hamilton CD, Xia Q, Stout JE. Mortality before or during treatment among tuberculosis patients in North Carolina, 1993-2003. Int J Tuberc Lung Dis. 2011;15:257–62,. [PMC free article] [PubMed] [Google Scholar]
- 16.Jeon DS, Kim DH, Kang HS, Hwang SH, Min JH, Kim JH, et al. Survival and predictors of outcomes in non-HIV-infected patients with extensively drug-resistant tuberculosis. Int J Tuberc Lung Dis. 2009;13:594–600. [PubMed] [Google Scholar]
- 17.Liu CH, Li L, Chen Z, Wang Q, Hu YL, Zhu B, et al. Characteristics and treatment outcomes of patients with MDR and XDR tuberculosis in a TB referral hospital in Beijing: A 13-year experience. PLoS One. 2011;6:e19399. doi: 10.1371/journal.pone.0019399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pardeshi G. Survival analysis and risk factors for death in tuberculosis patients on directly observed treatment-short course. Indian J Med Sci. 2009;63:180–6. [PubMed] [Google Scholar]
- 19.Vilariça AS, Diogo N, André M, Pina J. Adverse reactions to antituberculosis drugs in in-hospital patients: Severity and risk factors. Rev Port Pneumol. 2010;16:431–51. doi: 10.1016/s0873-2159(15)30040-4. [DOI] [PubMed] [Google Scholar]


